Abstract
BACKGROUND AND OBJECTIVES:
Sexually transmitted infections (STIs) represent a major global health problem leading to morbidity, mortality and stigma. Prior to this study there was no information on the prevalence and knowledge of STIs in Faisalabad, Pakistan.
DESIGN AND SETTING:
Prospective, cross-sectional study in patients attending STI clinics from July 2006 to September 2009.
PATIENTS AND METHODS:
After obtaining consent, patients completed structured questionnaires used for behavioral surveys. Blood and urethral swabs were collected and tested for syphilis, gonococcus, genital herpes, chlamydia and chancroid.
RESULT:
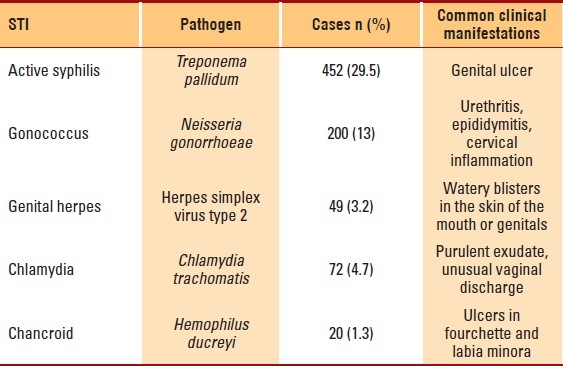
Mean (standard deviation) age of the 1532 participants was 38.9 (9.4) years, including 37.8 (10.2) years for males and 35.5 (6.3) years females. Male gender (n=1276, 83.3%), low socioeconomic class (n=1026, 67.0%) and residence in rural suburbs (n=970, 63.3%) were more common. Most (n=913, 59.6%) were aware of the modes of transmission of STIs and the associated complications, 20% (n=306) were condom users, and 21.2% (n=324) had knowledge of safe sex. Opposite-sex partners were preferred by 972 (63.4%) patients, while 29.9% (n=458) had both homosexual and heterosexual sex partners. Syphilis was present in 29.5% of patients (n=452); gonorrhea, in 13% (n=200), HSV-2, in 3.2% (n=49), chlamydia, in 4.7% (n=72) and chancroid, in 1.3% (n=20).
CONCLUSION:
This report establishes baseline local prevalence rates for STIs. Syphilis emerged as the most prevalent STI in Faisalabad. Population-based studies are required to study the epidemiology of STIs, along with initiation of national health-education campaign.
Not all sexually transmitted infections (STIs) are reproductive tract infections, nor are all reproductive tract infections sexually transmitted. The ‘ST’ in ‘STI’ denotes the manner of transmission of infection, while reproductive tract infection refers to the site of infection. In 1999, 340 million new cases of four curable STIs (gonorrhea, chlamydia, syphilis and trichomoniasis) occurred. These infections represent a major global health problem leading to morbidity, mortality and stigma. Control of STIs has been given priority since the advent of the HIV/ AIDS epidemic, in recognition of their role in facilitating the sexual transmission of HIV. Although the course of many of these STIs is benign even without treatment, some infections may lead to long-term sequelae, including pelvic inflammatory disease, infertility and cervical cancer. Their epidemiological profile varies with geography and depends upon ethnic, demographic, social and economic factors.1–3
Pakistan is the second most populous Muslim-majority country, with an estimated population of 169 639 500 in 2010. Faisalabad, located in the northeast region, was founded in 1892 as an agricultural market and has grown into a large metropolitan city. Also known as “the Manchester of Asia,” Faisalabad is renowned for textiles, engineering, chemicals, food processing, hosiery, printing, publishing, pharmaceuticals and household power loom units.
Religious and social ethics are highly admired and deeply ingrained in the Pakistani society. Many people in Pakistan are severely disadvantaged in terms of income, education, power structure, or gender. Addressing these basic issues of human rights lies at the core of achieving better health outcomes. Certain key features have a direct bearing on Pakistan's health-delivery system: the population size and distribution, the country's geography, the gender ratio and the socioeconomic development of people. The majority of the population, 69%, is rural. Poverty is widespread—31% of Pakistanis subsist on US$1 per day, and 85% earn less than US$2 per day. With only 22% of the population economically active, the proportion of people officially unemployed is currently 20%. All these factors are compounded by cultural practices. Pakistan is a male-dominated society, and prejudice against women is reflected in the higher female mortality rate and low literacy rate. This combination of factors gives rise to strong negative repercussions on health.3–7 Dynamic changes in clinical patterns of STIs must be acknowledged and tracked in populous cities like Faisalabad. The present study assesses the prevalence and knowledge of some common STIs in Faisalabad, Pakistan.
PATIENTS AND METHODS
There was no information on the prevalence of STIs among Faisalabad residents prior to this study. In the general population, sampling was not possible due to social, ethical and religious issues. For this reason, convenience sampling was used. In this cross-sectional observational study, respondents were selected from the Outpatient Departments of the District Head Quarter Hospital and Allied Hospital, Faisalabad, using a multistage systematic sampling method. Multistage sampling involved sample selection over at least three stages. At the first stage, large groups with various infections were selected. At the second stage, a sample with selected STIs was determined; and at the third stage, those who gave consent were included in the study.
Data were collected through behavioral questionnaires (appendix) and biological tests. A pre-coded questionnaire was the survey instrument. Trained investigators pre-tested the validity and reliability of the questionnaire before use. Privacy and confidentiality were maintained for all aspects of the study—history taking, examination and sampling. The Ethical Committee of Punjab Medical College, Faisalabad, reviewed the protocols, gave ethical approval for the study, and its recommendations were included in the study. Before data and sample collection, a workshop was organized to familiarize the study team with standard procedures. Consenting participants were interviewed by a physician trained to make in-person assessment in the following areas: socio-demographic characteristics (age, religion, civil status, education, occupation) and risk factors for STI (current signs of STI, number of marriages and extramarital relationships, symptoms of STI in the past, current symptoms of vaginal/urethral discharge, and medical history). Clinical screening was performed, including a speculum and bimanual examination for signs of STI not noticed by patients.
Appendix 1.
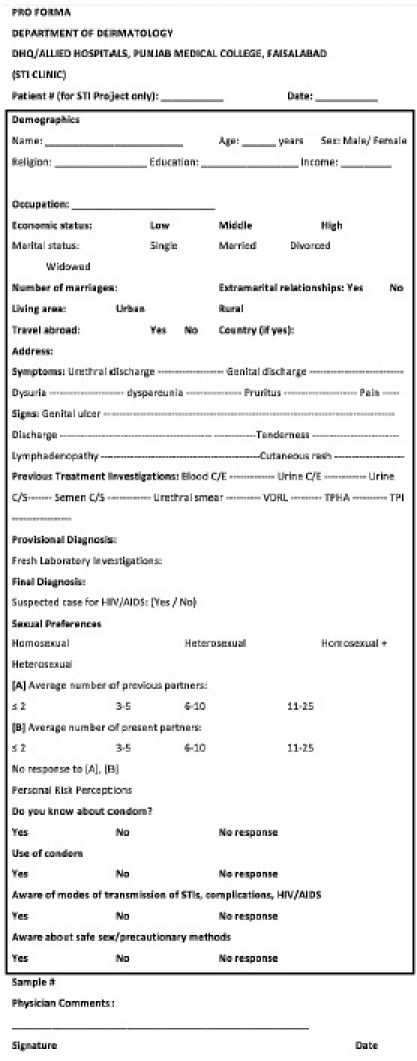
Behavioral Questionnaire
Five common STIs were screened through laboratory assessments: syphilis (Venereal Disease Research Laboratory test [VDRL], Treponema pallidum hemagglutination [TPHA], and rapid plasma reagin [RPR]), gonococcus (positive oxidase reaction, gram-stain, culture in modified Thayer-Martin (MTM) medium, and carbohydrate utilization patterns), genital herpes (immunofluorescent assay, Tzanck test), chlamydia (direct immunofluorescence test), and chancroid (direct immunofluorescence test, culture, coagglutination). Both internal and external quality control mechanisms were ensured. Kits and reagents were purchased from reputable companies, and manufacturers' guidelines were followed for collection, storage and analysis.
RESULTS
Of the 1532 patients who consented to participation, most infections were among people aged 30 to 45 years (Table 1). The mean age of the participants was 38.9 (9.4) years (males, 37.8 [10.18] years; females, 35.5 [6.3] years). Approximately 63.3% of patients (n=970) were from rural suburbs. Male gender (n=1276, 83.3%) and low socioeconomic class (n=1026, 67.0%) were dominant. Most patients (n=1370; 89.4%) were married. About 79% of patients (n=1210) never attended school, while 21% (n=322) had attained primary/high school or higher education. Fifty-five (3.59%) patients were unemployed, 491 (32.0%) were self-employed and 986 (64.4%) were employees.
Table 1.
Sociodemographic and behavioral characteristics of study participants (n= 1532)
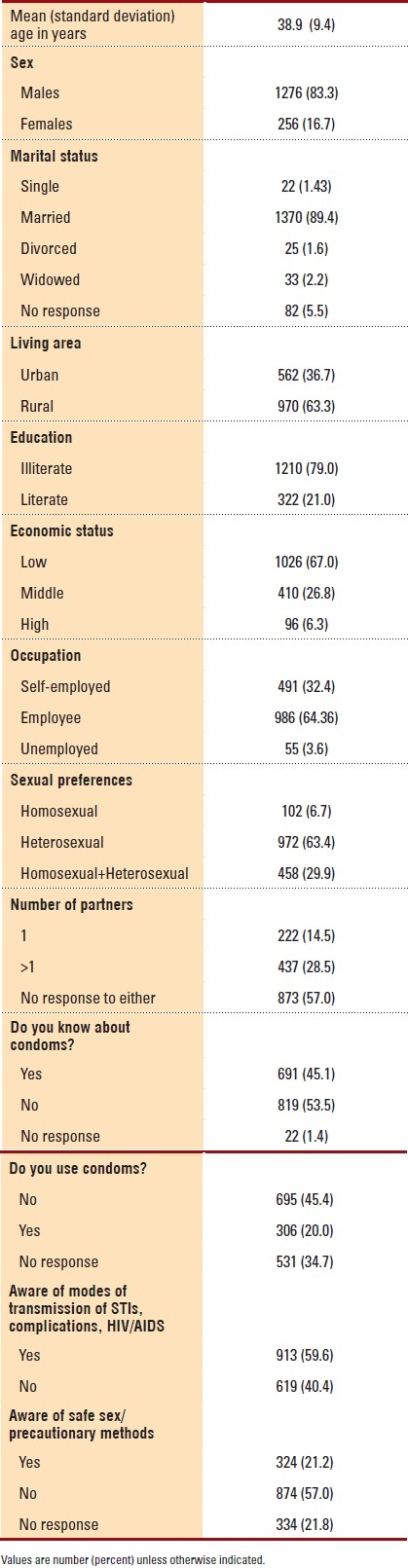
Nine hundred seventy-two (63.4%) patients were heterosexual, while 458 (29.9%) had both same-sex and opposite-sex partners. The majority of patients (57.0%) refused to disclose the number of past or present partners; 28.5% (n=437) reported having two or more partners. Approximately 20% (n=306) were condom users, 45.4% (n=691) had heard of or seen condoms but never used them, and 34.7% (n=531) did not respond to the query. Nearly 60% of patients (n=913) were aware of the modes of transmission of STIs, complications, and HIV/ AIDS; and 324 (21.2%) patients knew about precautionary methods for safe sex.
Four bacterial species—Chlamydia trachomatis, Treponema pallidum, Neisseria gonorrhoeae and Hemophilus ducreyi—and one viral herpes simplex virus, HSV-2, were identified (Table 2). Genital ulcer was the most common presenting complaint (n=452, 29.5%). Painful, tender ulcers (duration of 7 days to 3 weeks) were recurrent and grouped.
Table 2.
Prevalence and clinical presentation of STIs in 1532 participants
DISCUSSION
STIs have a great impact on the health of populations worldwide. STIs may be contracted by people of any age, race or social standing, and their early diagnosis and treatment are necessary to avoid propagation. Sexual education is fundamental to STI prevention.8 Wide disparities and racial gaps in STI rates are evident. Prevalence data are important for the surveillance of STIs. However, no data on STI rate (cases over time) or prevalence assessment was previously available in the study region.
Syphilis emerged as a major STI in Faisalabad. Syphilis, caused by Treponema pallidum, facilitates the transmission of HIV.1,2 We observed a 29.5% prevalence of syphilis, which supports the studies by Basal et al9 and Rehan,10 reporting 32.4% and 31.6% syphilis infection rate, respectively, in the region. In the United States, the rate of syphilis infection was 2.1 cases per 100 000 persons in 1999.11 Syphilis infection has reached alarming rates (13.8%-19.5%) in China.12 In the Peruvian Amazon, it was 6.3%.13 Different studies have reported the prevalence of active syphilis as follows, 9% in Northwestern Tanzania, 1.8% in China, 4% in South Africa and 0.2% in South Korea.14–17 In the rural population of Punjab, India, syphilis was altogether absent.18
The World Health Organization estimates that 92 million Chlamydia trachomatis (CT) infections occurred worldwide in 1999.19 Our estimates of chlamydia prevalence were broadly comparable with those reported in other population-based studies showing prevalence rates ranging from 4.1% to 5.2%.15,20–24 In a population-based study from the Netherlands, CT prevalence was 2.0%.25 Most of the 11.3% of the Barbados population infected with CT urogenital infection were asymptomatic.26 The CT infection rates in Northern Canada, Alaska and Greenland were reported to be 1.69%, 0.72% and 5.54%, respectively.27 Jindal et al18 reported a CT-infection rate of 1% in the rural population of Punjab, India.
Neisseria gonorrhoeae infection is a common bacterial STI.28 The 13% prevalence observed in our study was not comparable to that (27.5%) reported by Rehan.10 A 31.5% prevalence of gonorrhea was observed among STI patients attending hospital in Farwaniya, Kuwait.20 Gonorrhea accounted for 85% and 71% of male urethral discharge presentations in Cape Town and Johannesburg, South Africa, respectively.29 Among men with the complaint of urethral discharge, Neisseria gonorrhoeae was identified in 35% in Karnataka state, South India.30 In contrast, miners in Yunnan, China, had a 0.8% prevalence of Neisseria gonorrhoeae.15 Gesink et al27 summarized published and unpublished rates of gonorrhea infections reported from 2003 through 2006 in Arctic communities. Greenland consistently reported the highest rates of gonorrhea (1.74%); Northern Canada reported a 0.25% rate of gonorrhea infection. The overall prevalence of gonorrhea in the United States was reported to be 0.43%, with substantial racial/ ethnic disparities in the prevalence of gonococcal infections also observed.24
Genital herpes simplex virus type 2 (HSV−2) is an increasingly important cause of genital ulcer disease (GUD).31,32 Our observed 3.2% prevalence of genital herpes was in accordance with the results of the studies by Mir et al33 and García-Corbeira et al.34 The overall HSV-2 seroprevalence in the United States was 21.0% in 1988-1994, 17.0% in 1999-2004,35 and 16.2% in 2005-2008.36 HSV-2 was identified in 85.2% of STI clinic attendees in Delhi, India.37 A cross-sectional study reported an HSV-2 prevalence of 4.8% in Turkey.38 In the 1997-1998 German National Health Survey, the seroprevalence of HSV-2 was 13.3% in Germany, 16.5% in the former East Germany and 12.6% in the former West Germany.39 The prevalence of HSV-2 was 9.6% among miners in China15 and was estimated at 15% in Chennai, India.40 A population-based study demonstrated a 12% prevalence of HSV-2 in Australian adults.41 Among the Korean population attending public health centers, HSV-2 seroprevalence rates for those aged <20, 20-40 and >40 years were 22.6%, 32.7% and 32.3%, respectively.42
During infection, Hemophilus ducreyi thrives in the extracellular environment comprised of antibacterial components, such as phagocytes, of the innate and adaptive immune responses.43 Our observed prevalence of H ducreyi infections (1.4%) was in accordance with that reported in Durban, South Africa (1.2%).44 Five-year (1995-1999) surveillance for STIs in Saudi Arabia indicated a 0.2% prevalence of chancroid.45 Contrary to our findings, H ducreyi occurrence rates of 3% in Paris, 13% in Kuwait and 17.2% in rural Pakistan have been reported.20,46,47
Lack of knowledge and misconceptions in beliefs and attitudes were prominent in our cohort, as reported earlier.47–49 Although relatively fewer numbers of sexual partners per subject were reported in this study, consistent condom use was low. There is an acute need to enhance condom usage and STI-related counseling. In addition, health services need to be modified to ensure early diagnosis and treatment. Pakistan is a Muslim country where lay knowledge regarding STIs is poor. Surveillance arrangements are limited and frequently ignored, with the result that the true incidence of STIs is unknown. Modern diagnostic techniques are not widely deployed, and there is little standardization of medical arrangements.
A major barrier we observed was the difficulty in obtaining STI prevalence data from women. Female participants were shy about pertinent queries. The lower number of female patients in our study can be justified by the fact that the majority of Pakistani women consult gynecologists, family elders, local hakeems, or daies (untrained local women who help in delivering children at home). Family and spousal pressures limit their approach to male physicians. Most female participants were employed in domestic chores and were dependent on men and may have had limited decisive power in their sexual relationships. Another constraint was that sampling was limited to interviewees, who can under-report risk behavior. People also sometimes contact pharmacies or traditional healers instead of health care facilities, and self-medication or alternative therapies may worsen or improve STIs. Many people generally consult local hakeems (homeopathic doctors) and seek medical advice only when pain is intolerable. Therefore, the differences in STI prevalence between this study and other studies may be attributed to the difference in setting, social beliefs and level of awareness about complications between the study populations.
The factors that determine health behaviors in Pakistan may be seen in various physical, socioeconomic, cultural and political contexts. Religious and social ethics discourage open discussion of sexual matters. The low social status of women limits their economic options, and women may exchange sex for money or other forms of support. Poor health services offer little for the prevention and treatment of STIs. Various factors, including proximity, affordability, availability, family pressure and strong community opinion, lead to self-care and consultation with traditional healers, hakeems or even quacks.50 Long-held misconceptions continue to contribute to the national neglect of STI treatment and prevention. Prompt STI detection, prevention and STI-related counseling in STI clinics for vulnerable groups, as well as educational interventions, should be the requisites of public and private health sectors in Pakistan.
REFERENCES
- 1.Shefer T, Strebel A, Wilson T, Shabalala N, Simbayi L, Ratele K, et al. The social construction of sexually transmitted infections (STIs) in South African communities. Qual Health Res. 2002;12:1373–90. doi: 10.1177/1049732302238749. [DOI] [PubMed] [Google Scholar]
- 2.Wasserheit JN. Epidemiologic synergy: Interrelationships between human immunodeficiency virus infection and other sexually transmitted diseases. Sex Transm Dis. 1992;19:61–77. [PubMed] [Google Scholar]
- 3.Ayres RU. London: Earthscan Publications; 1998. Turning point: An end to the growth paradigm; p. 63. [Google Scholar]
- 4.Ministry of Economic Affairs and Statistics. Official Pakistani population clock. [Last accessed on 2010 Feb 11]. Available from: http://www.statpak.gov.pk/depts/pco/.
- 5.Population Census Organization of Pakistan. Population size and growth of major cities, 1998 census. [Last accessed on 2010 Feb 11]. Available from: http://www.statpak.gov.pk/depts/pco/statistics/pop_major_cities/pop_major_cities.html .
- 6.City District Government of Faisalabad. Population. [Last accessed on 2007]. Available from: http://www.faisalabad.gov.pk/statistics.aspx?task=pop .
- 7.Jawad F. Diabetes in Pakistan. Diabetes Voice. 2003;48:12–4. [Google Scholar]
- 8.García Vega EM, Puigvert Viu N. Sexual transmission infections. Rev Enferm. 2010;33:42–6. [PubMed] [Google Scholar]
- 9.Basal KN, Khare KA, Upadhaya PO. Patterns of sexually transmitted diseases in and around Udaipur. Indian J Dermatol Venereol Leprol. 1988;54:90–2. [PubMed] [Google Scholar]
- 10.Rehan N. Profile of men suffering from sexually transmitted infections in Pakistan. J Pak Med Assoc. 2006;56:S60–5. [PubMed] [Google Scholar]
- 11.The national plan to eliminate syphilis from the United States. Atlanta, GA: Centers for Disease Control and Prevention; 1999. US Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for HIV, STD and TB Prevention; pp. 1–84. [Google Scholar]
- 12.Wong SP, Yin YP, Gao X, Wei WH, Shi MQ, Huang PY. Risk of syphilis in STI clinic patients: A cross-sectional study of 11,500 cases in Guangxi, China. Sex Transm Infect. 2007;83:351–6. doi: 10.1136/sti.2007.025015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Zavaleta C, Fernandez C, Konda K, Valcerrama Y, Vermund SH, Gottuzo E. High prevalence of HIV and syphilis in a remote native community of the Peruvian Amazon. Am J Trop Med Hyg. 2007;76:703–5. [PMC free article] [PubMed] [Google Scholar]
- 14.Mosha F, Nicoll A, Barongo L, Borgdorff M, Newell J, Senkoro K, et al. A population-based study of syphilis and sexually transmitted disease syndromes in north-western Tanzania. 1. Prevalence and incidence. Genitourin Med. 1993;69:415–20. doi: 10.1136/sti.69.6.415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Zhang G, Wong M, Yi P, Xu J, Li B, Ding G, et al. HIV-1 and STIs prevalence and risk factors of miners in mining districts of Yunnan, China. J Acquir Immune Defic Syndr. 2010;53:S54–60. doi: 10.1097/QAI.0b013e3181c7d8d2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mhlongo S, Magooa P, Müller EE, Nel N, Radebe F, Wasserman E, et al. Etiology and STI/HIV coinfections among patients with urethral and vaginal discharge syndromes in South Africa. Sex Transm Dis Epub. 2010;37:566–70. doi: 10.1097/OLQ.0b013e3181d877b7. [DOI] [PubMed] [Google Scholar]
- 17.Cho YH, Kim HO, Lee JB, Lee MG. Syphilis prevalence has rapidly decreased in South Korea. Sex Transm Infect. 2003;79:323–4. doi: 10.1136/sti.79.4.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Jindal N, Aggarwal A, Gill P, Sabharwal, Sheevani BB. Community-based study of reproductive tract infections, including sexually transmitted infections, among the rural population of Punjab, India. Indian J Community Med. 2009;34:359–61. doi: 10.4103/0970-0218.58401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Geneva: World Health Organization; 2001. World Health Organization. Global prevalence and incidence of selected curable sexually transmitted diseases: Overview and estimates; p. 50. [Google Scholar]
- 20.Al-Mutairi N, Joshi A, Nour-Eldin O, Sharma AK, El-Adawy I, Rijhwani M. Clinical patterns of sexually transmitted diseases, associated sociodemographic characteristics, and sexual practices in the Farwaniya region of Kuwait. Int J Dermatol. 2007;46:594–9. doi: 10.1111/j.1365-4632.2007.02843.x. [DOI] [PubMed] [Google Scholar]
- 21.Vajdic CM, Middleton M, Bowden FJ, Fairley CK, Kaldor JM. The prevalence of genital Chlamydia trachomatis in Australia 1997-2004: A systematic review. Sex Health. 2005;2:169–83. doi: 10.1071/sh05018. [DOI] [PubMed] [Google Scholar]
- 22.Klavs I, Rodrigues LC, Wellings K, Ke?e D, Hayes R. Prevalence of genital Chlamydia trachomatis infection in the general population of Slovenia: Serious gaps in control. Sex Transm Infect. 2004;80:121–3. doi: 10.1136/sti.2003.005900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Brito de Sá A, Gomes JP, Viegas S, Ferreira MA, Paulino A, Catry MA. Genital infection by Chlamydia trachomatis in Lisbon: Prevalence and risk markers. Fam Pract. 2002;19:362–4. doi: 10.1093/fampra/19.4.362. [DOI] [PubMed] [Google Scholar]
- 24.Miller WC, Ford CA, Morris M, Handcock MS, Schmitz JL, Hobbs MM, et al. Prevalence of chlamydial and gonococcal infections among young adults in the United States. JAMA. 2004;12:2229–36. doi: 10.1001/jama.291.18.2229. [DOI] [PubMed] [Google Scholar]
- 25.Van Bergen J, Götz HM, Richardus JH, Hoebe CJ, Broer J, Coenen AJ. Prevalence of urogenital Chlamydia trachomatis increases significantly with level of urbanisation and suggests targeted screening approaches: Results from the first national population based study in the Netherlands. Sex Transm Infect. 2005;81:17–23. doi: 10.1136/sti.2004.010173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Adams OP, Carter AO, Prussia P, McIntyre G, Branch SL. Risk behaviour, healthcare access and prevalence of infection with Chlamydia trachomatis and Neisseria gonorrhoeae in a population-based sample of adults in Barbados. Sex Transm Infect. 2008;84:192–4. doi: 10.1136/sti.2007.028126. [DOI] [PubMed] [Google Scholar]
- 27.Gesink Law D, Rink E, Mulvad G, Koch A. Sexual health and sexually transmitted infections in the North American Arctic. Emerg Infect Dis. 2008;14:4–9. doi: 10.3201/eid1401.071112. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Furuya R, Tanaka M. Neisseria gonorrhoeae infections. Nippon Rinsho. 2009;67:129–35. [PubMed] [Google Scholar]
- 29.Mhlongo S, Magooa P, Müller EE, Nel N, Radebe F, Wasserman E, et al. Etiology and STI/HIV coinfections among patients with urethral and vaginal discharge syndromes in South Africa. Sex Transm Dis Epub. 2010;37:566–70. doi: 10.1097/OLQ.0b013e3181d877b7. [DOI] [PubMed] [Google Scholar]
- 30.Becker M, Stephen J, Moses S, Washington R, Maclean I, Cheang M, et al. Etiology and determinants of sexually transmitted infections in Karnataka state, south India. Sex Transm Dis. 2010;37:159–64. doi: 10.1097/OLQ.0b013e3181bd1007. [DOI] [PubMed] [Google Scholar]
- 31.Paz-Bailey G, Ramaswamy M, Hawkes SJ, Geretti AM. Herpes simplex virus type 2: Epidemiology and management options in developing countries. Sex Transm Infect. 2007;83:16–22. doi: 10.1136/sti.2006.020966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Nikolic DS, Piguet V. Viral sexually transmitted infections: Prevention, treatments and perspectives. Rev Med Suisse. 2010;28:866–70. [PubMed] [Google Scholar]
- 33.Mir AM, Wajid A, Reichenbach L, Khan M. STI prevalence and associated factors among urban men in Pakistan. Sex Transm Infect. 2009;85:199–200. doi: 10.1136/sti.2008.034165. [DOI] [PubMed] [Google Scholar]
- 34.García-Corbeira P, Dal-Ré R, Aguilar L, Granizo JJ, García-de-Lomas J. Is sexual transmission an important pattern for herpes simplex type 2 virus seroconversion in the Spanish general population? J Med Virol. 1999;59:194–7. doi: 10.1002/(sici)1096-9071(199910)59:2<194::aid-jmv11>3.0.co;2-9. [DOI] [PubMed] [Google Scholar]
- 35.Xu F, Sternberg MR, Kottiri BJ, McQuillan GM, Lee FK, Nahmias AJ, et al. Trends in herpes simplex virus type 1 and type 2 seroprevalence in the United States. JAMA. 2006;296:964–73. doi: 10.1001/jama.296.8.964. [DOI] [PubMed] [Google Scholar]
- 36.Centers for Disease Control and Prevention (CDC). Seroprevalence of herpes simplex virus type 2 among persons aged 14-49 years--United States, 2005-2008. MMWR Morb Mortal Wkly Rep. 2010;23:456–9. [PubMed] [Google Scholar]
- 37.Kaur R, Mittal N, Bhalla P, Reddy BN, Baveja UK. Risk factors of herpes simplex virus type 2 among STD clinic attenders in Delhi, India. J Commun Dis. 2006;38:339–43. [PubMed] [Google Scholar]
- 38.Dolar N, Serdaroglu S, Yilmaz G, Ergin S. Seroprevalence of herpes simplex virus type 1 and type 2 in Turkey. J Eur Acad Dermatol Venereol. 2006;20:1232–6. doi: 10.1111/j.1468-3083.2006.01766.x. [DOI] [PubMed] [Google Scholar]
- 39.Hellenbrand W, Thierfelder W, Müller-Pebody B, Hamouda O, Breuer T. Seroprevalence of herpes simplex virus type 1 (HSV-1) and type 2 (HSV-2) in former East and West Germany, 1997-1998. Eur J Clin Microbiol Infect Dis. 2005;24:131–5. doi: 10.1007/s10096-005-1286-x. [DOI] [PubMed] [Google Scholar]
- 40.Jennings JM, Louis TA, Ellen JM, Srikrishnan AK, Sivaram S, Mayer K, et al. Geographic prevalence and multilevel determination of community-level factors associated with herpes simplex virus type 2 infection in Chennai, India. Am J Epidemiol. 2008;167:1495–503. doi: 10.1093/aje/kwn066. [DOI] [PubMed] [Google Scholar]
- 41.Cunningham AL, Taylor R, Taylor J, Marks C, Shaw J, Mindel A. Prevalence of infection with herpes simplex virus types 1 and 2 in Australia: A nationwide population based survey. Sex Transm Infect. 2006;82:164–8. doi: 10.1136/sti.2005.016899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Shin HS, Park JJ, Chu C, Song HJ, Cho KS, Lee JS, et al. Herpes simplex virus type 2 seroprevalence in Korea: Rapid increase of HSV-2 seroprevalence in the 30s in the southern part. J Korean Med Sci. 2007;22:957–62. doi: 10.3346/jkms.2007.22.6.957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Janowicz DM, Li W, Bauer ME. Host-pathogen interplay of Haemophilus ducreyi. Curr Opin Infect Dis. 2010;23:64–9. doi: 10.1097/QCO.0b013e328334c0cb. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.O′Farrell N, Morison L, Moodley P, Pillay K, Vanmali T, Quigley M, et al. Genital ulcers and concomitant complaints in men attending a sexually transmitted infections clinic: Implications for sexually transmitted infections management. Sex Transm Dis. 2008;35:545–9. doi: 10.1097/OLQ.0b013e31816a4f2e. [DOI] [PubMed] [Google Scholar]
- 45.Madani TA. Sexually transmitted infections in Saudi Arabia. BMC Infect Dis. 2006;6:3. doi: 10.1186/1471-2334-6-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hope-Rapp E, Anyfantakis V, Fouéré S, Bonhomme P, Louison JB, de Marsac TT, et al. Etiology of genital ulcer disease.A prospective study of 278 cases seen in an STD clinic in Paris. Sex Transm Dis. 2010;37:153–8. doi: 10.1097/OLQ.0b013e3181bf5a98. [DOI] [PubMed] [Google Scholar]
- 47.Raheel H, White F, Kadir MM, Fatmi Z. Knowledge and beliefs of adolescents regarding sexually transmitted infections and HIV/AIDS in a rural district in Pakistan. J Pak Med Assoc. 2007;57:8–11. [PubMed] [Google Scholar]
- 48.Mazhar SB, Agha MA, Shaikh MA. Knowledge and misconceptions about sexually transmitted infections in married women-perspective from Islamabad. J Pak Med Assoc. 2006;56:S44–7. [PubMed] [Google Scholar]
- 49.Haque N, Zafar T, Brahmbhatt H, Imam G, ul Hassan S, Strathdee SA. High-risk sexual behaviours among drug users in Pakistan: Implications for prevention of STDs and HIV. Int J STD AIDS. 2004;15:601–7. doi: 10.1258/0956462041724172. [DOI] [PubMed] [Google Scholar]
- 50.Shaikh BT, Hatcher J. Complementary and alternative medicine in Pakistan: Prospects and limitations. Evid Based Complement Alternat Med. 2005;2:139–42. doi: 10.1093/ecam/neh088. [DOI] [PMC free article] [PubMed] [Google Scholar]


