Abstract
BACKGROUND AND OBJECTIVES:
Thyroidectomy is a commonly performed procedure for thyroid problems. Inadvertent removal of the parathyroid glands is one of its recognized complications, which occurs more frequently in certain high-risk patients. The aim of this study was to identify the incidence, risk factors, and clinical relevance of incidental parathyroidectomy during thyroid surgery.
DESIGN AND SETTING:
A retrospective review of thyroid operations performed at a tertiary referral hospital between January 2004 and December 2008.
METHODS:
Pathology reports were reviewed to identify the specimens that included parathyroid tissue and underlying thyroid pathology. Postoperative calcium levels were reviewed in these patients.
RESULTS:
During the study period, 287 thyroidectomies were performed and 47 (16.4%) patients had incidentally removed parathyroid glands. Risk factors for inadvertent parathyroid resection included total thyroidectomy (P=.0001), Hashimoto thyroiditis (P=.004), and extrathyroidal spread (P=.0003). Postoperative hypocalcemia occurred in 18 (38.3%) of the patients in whom the parathyroid gland was removed inadvertently and in 48 (20%) of the rest of the patients (P=.0123).
CONCLUSION:
The incidence of incidental removal of parathyroid tissue during thyroidectomy is 16.4%. Total thyroidectomy, extrathyroidal extension of the tumor, and thyroiditis were found to be the risk factors. Hypocalcemia was significantly higher among patients who had inadvertent parathyroidectomy.
The two most common complications of thyroid resection include recurrent laryngeal nerve injury and hypocalcemia. These and other major complications typically occur in less than 5% of the cases.1,2 In the 21st century, thyroidectomy has become safe and effective with improved outcomes and minimal morbidity.3,4 This is in part due to the awareness of the anatomical relationship of the parathyroid gland to the thyroid, which is important in preventing postoperative hypocalcemia. Nonetheless, the incidence of hypocalcemia following thyroidectomy remains significantly high in the range of 1.6% to 50%, with permanent hypocalcemia occurring in 1.5% to 4% of the cases.5–9 Regardless of surgeon experience, an incidental parathyroid gland features occasionally in the pathology reports of thyroid specimens. The aims of present study are to find out the incidence of the incidental parathyroid excision (IPE) during thyroidectomy and its effects on the postoperative calcium levels and also to evaluate the factors underlying its occurrence.
METHODS
This was a retrospective chart review carried out in patients who underwent thyroid resection at King Khalid University Hospital, Riyadh, between January 2004 and December 2008. The patient records were reviewed, and data on age, sex, preoperative diagnosis, history of previous surgery, and details of operative and postoperative reports were recorded on special data sheets. The thyroid procedures (subtotal and total thyroidectomy together with lobectomy or completion thyroidectomy) were either performed by two surgeons (the authors) who have particular interest and experience in thyroid surgery or by registrars under their close supervision and assistance. Operations that included a simultaneous modified neck dissection or central compartment node dissection were included in the analysis. Procedures for hyperparathyroidism and parathyroid glands intimately involved with tumors were excluded from the study.
Serum calcium levels were measured preoperatively; on the day of surgery; on postoperative days 1 and 2; and 4 to 6 weeks postoperatively in the surgical outpatient clinic. The hypocalcemic patients were followed-up for at least 6 months in the outpatient clinic to determine whether hypocalcemia was transient or permanent. Patients without complications were discharged on postoperative day 1 after ascertaining that their calcium levels were within the normal range.
Pathology reports were reviewed as to the nature of the thyroid disease and specifically for the presence of parathyroid glands, their location (i.e., extracapsular or intrathyroidal), the number removed, their size, and their histological characteristics. Statistical analysis was carried out using the SPSS software package (SPSS, Chicago, IL, USA). The chi-square test and Fisher exact test were used to analyze the association between categorical study variable and IPE (present/absent). For all calculations, P≤.05 was considered statistically significant.
RESULTS
Two hundred and eighty seven patients underwent thyroid resection during the study period. Forty-seven patients (16.4%) were found to have incidentally removed parathyroid glands by reviewing their pathology reports. Patient ages ranged from 14–79 years (mean [standard deviation], 38.5 [13.5] years), but there was no significant difference between the mean age of patients with and without IPE (35 [12] vs. 39 [13] years, P=.119). The majority of patients were women, but gender was not found to be a predictor for incidental removal (P=.128). The thyroid pathology was benign in 164 (57.1%) patients and malignant in 123 (42.9%). The thyroid operations carried out included total thyroidectomy in 121 (42.2%), thyroid lobectomy in 128 (44.6%), subtotal thyroidectomy in 8 (2.8%), and completion thyroidectomy in 30 (10.5%) patients (Table 1).
Table 1.
Demographic, pathological, and operative data of study patients
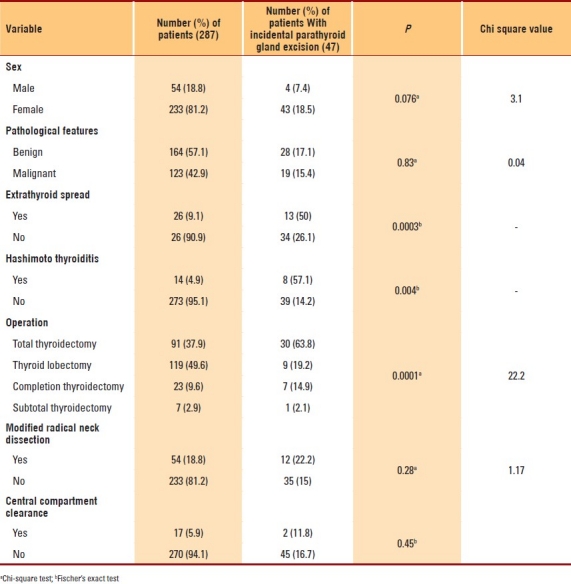
IPE was more common in patients with total thyroidectomy than in those who had undergone lobectomy only (P=.001). Papillary carcinoma was found to be the most common malignancy, while the most common benign pathological abnormality was multinodular goiter (Table 2). Forty-one (87%) of the patients with IPE had only one parathyroid gland excised and 5 patients (10.6%) had two removed. In the remaining patient, three parathyroid glands were recovered from the thyroid specimen. This patient had undergone total thyroidectomy and modified radical neck dissection for papillary carcinoma and was found to have extrathyroidal spread of tumor and a Hashimoto thyroiditis background in the histopathology. Of the 56 parathyroid glands that were removed inadvertently, 29 (51.8%) were extracapsular and 24 (42.9%) were intrathyroidal; details of the remaining three glands were not available. All the incidentally removed parathyroids had normal histology.
Table 2.
Thyroid pathology
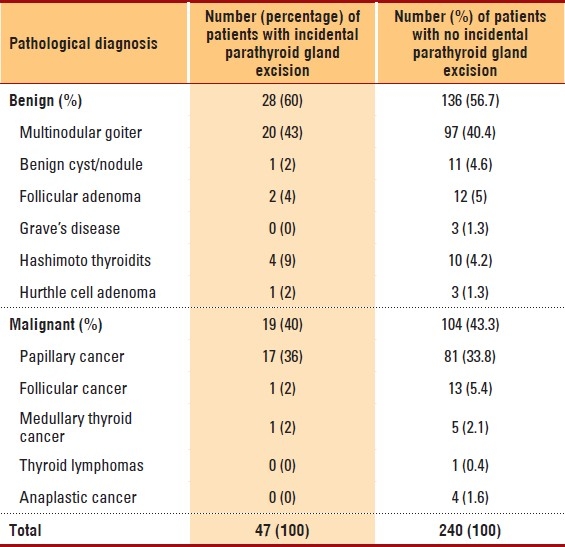
The incidence of biochemical hypocalcemia on the first postoperative day was 23.3%, and hypocalcemia was significantly higher among patients with IPE (38.3%) (18 of 47) than in those without IPE (20%) (48 of 240 patients) (P=.0123). The overall incidence of permanent hypocalcemia was 2.1%. More patients with IPE (4.2%, 2 of 47) developed permanent hypocalcemia than those who did not have IPE (1.7%, 4 of 240), but the difference was not statistically significant (P=.255). The factors assessed for unintentional excision of the parathyroid glands during thyroid surgery are shown in Table 1. Total thyroidectomy, extrathyroidal spread, and thyroiditis were found to be associated with a significantly higher incidence of IPE, according to the chi-square test and Fisher exact test (Table 1).
DISCUSSION
IPE and hypocalcemia are well-recognized complications of thyroid surgery. Theodor Kocher, who reported the first 100 thyroidectomies in 1883, noted the presence of tetany in some cases postoperatively.10 William Halsted (1852–1922) advocated meticulous surgical techniques to prevent damaging the parathyroid glands and, in this way, contributed greatly to the prevention of these serious complications that together with bleeding and laryngeal nerve injury made early thyroid surgery so hazardous.11
The current study is the first in Saudi Arabia as far as we know to examine the incidence of IPE during thyroid surgery. We found the incidence rate of IPE in our patients to be 16.4% and that compares favorably with the rates reported in the literature (5.2%–21.6%).12–16 Strict adherence to anatomical principles and surgical guidelines is vital for minimizing the incidence rate of iatrogenic hypoparathyroidism after thyroidectomy.5,6,17 The operating surgeon should also keep in mind the anatomical variations of the parathyroid glands18,19 to avoid inadvertent injury, devascularization, or resection of the parathyroid parenchyma. There is a wide variability in the number of parathyroid glands, but in most individuals, there are 4, each approximately 6–8 mm in diameter and located extracapsularly on the posterior surface of the thyroid gland. The superior parathyroids are commonly located at the superior pole of the thyroid, while the location of the inferior parathyroids is more variable, and is sometimes intrathymic. However, dissection in the search for all parathyroid glands during thyroid surgery is not advisable and may be hazardous.16
In the present study, risk factors for IPE included total thyroidectomy (P=.0001), Hashimoto thyroiditis (P=.004), and extrathyroid spread (P=.0003) (Table 1). As expected in total thyroidectomy, bilateral dissection increased the risk of parathyroid removal. This may be related to the fact that dissection bilaterally puts all four glands at risk. In addition, in the current study, total thyroidectomy was done mainly for malignant thyroid disease, and malignancy was reported to be a strong predictor of IPE in earlier studies,13,20 though it was not a risk factor in our study (P=.83). In the present as well as earlier studies,13,20,21 total thyroidectomy was found to be a risk factor for IPE. Hashimoto thyroiditis was another risk factor and a predictor of incidental parathyroid removal in our study (P=.004), and this is in line with the earlier reports.22,23 The association between thyroiditis and an increased risk of IPE can be accounted for by the formation of scar tissue as a result of inflammation and by increased bleeding, both of which may cause operative difficulties.
Although extrathyroid extension was not found to be a risk factor in a recent study,24 in the present study, we found it to be another strong predictor of IPE. Extrathyroid extension occurs in malignant lesions, and patients undergoing surgery for thyroid malignancy, particularly with a more aggressive approach, are at a higher risk. In our study, the factors that did not increase the risk for inadvertent parathyroidectomy included age, sex, pathological features (whether benign or malignant), modified radical neck dissection, central compartment clearance, and completion thyroidectomy. In previous studies, female sex16 and younger age20 were found to be the risk factors. In another study,25 male sex was reported as a strong predictor of incidental removal. However, in our series, age and sex were not found to carry any risk for IPE. The association of completion thyroidectomy with IPE has been reported extensively in literature. While Rix and Sinha26 showed a strong statistically significant association, in our study, completion thyroidectomy was not found to be a strong risk factor, despite the surgical difficulties expected with the re-exploration of the neck.
Two recent studies21,22 have reported a significant association between inadvertent parathryoidectomy and neck dissection (central compartment clearance and modified radical neck dissection, respectively). This may be related to the more extensive dissection performed during a similar procedure. In our data, neither central compartment clearance (P=.483) nor modified radical neck dissection (P=.382) were significant predictors for IPE.
In a feasibility study on endoscopic thyroidectomy, Gagner et al27 concluded that there was no significant difference in the rate of IPE between endoscopic and traditional open thyroidectomy. In the current study, about 43% of the incidentally resected parathyroids were intrathyroidal. Intrathyroidal location of parathyroids has been described in about 2% to 5% of autopsy studies,18,28 and incidentally excised parathyroids have been reported to be in an intrathyroid location in up to 40% to 50% of cases.14,21 Thus, incidental parathyroidectomy may occur even in the hands of more experienced thyroid surgeons.
Hypocalcemia is a major concern following thyroid surgery. The incidence of hypocalcemia was significantly higher among our patients with IPE (P≤.05) in the first post-operative day. Although Sasson et al21 and Lin et al22 did not find any association between hypocalcemia and IPE, Sippel et al20 reported that the IPE group had significantly lower postoperative calcium levels, and this is in line with our findings. Injury, devascularization, and unintentional excision of the parathyroids have all been cited as the causes of postoperative hypocalcemia. Although other specific factors have been studied, the cause of postoperative hypocalcemia remains to be multifactorial.29 The overall incidence of permanent hypocalcemia among our patients was 2.1%. Although hypocalcemia reverses spontaneously in most patients, it can remain permanent when caused by an irreversible injury to the parathyroid glands.30–33
In conclusion, unintentional parathyroidectomy during thyroid resection is not uncommon, and it occurred in 16.4% of the cases in this series. Total thyroidectomy, extrathyroid extension of the tumor, and thyroiditis were found to be the risk factors for IPE; however, to date there is no reliable way of predicting in which patients this will happen. Our patients with IPE developed biochemical postoperative hypocalcemia. A significant number of IPE were intrathyroidal (42.9%), and, therefore, this is obviously unavoidable even with changes in the surgical technique.
Acknowledgments
The authors would like to thank and acknowledge Mr. S. Shafi for his support with statistical analysis and Ms. Corazon L. Rivera for her secretarial expertise in typing this manuscript.
REFERENCES
- 1.Udelsman R, Chen H. The current management of thyroid cancer. Adv Surg. 1999;33:1–27. [PubMed] [Google Scholar]
- 2.Bergmaschi R, Becouarn G, Ronceray J, Arnaud JP. Morbidity of thyroid surgery. Am J Surg. 1998;176:71–5. doi: 10.1016/s0002-9610(98)00099-3. [DOI] [PubMed] [Google Scholar]
- 3.Koyuneu A, Dokmetas HS, Turan M, Aydin C, Karadayi K, Budak E, et al. Comparison of different thyroidectomy techniques for benign thyroid disease. Endocr J. 2003;50:723–7. doi: 10.1507/endocrj.50.723. [DOI] [PubMed] [Google Scholar]
- 4.Friguglietti CU, Lin CS, Kulesar MA. Total thyroidectomy for benign thyroid disease. Laryngoscope. 2003;113:1820–6. doi: 10.1097/00005537-200310000-00030. [DOI] [PubMed] [Google Scholar]
- 5.Pattaou F, Combermale F, Fabre S, Carnaille B, Decoulx M, Wemeau JL, et al. Hypocalcemia following thyroid surgery: Incidence and prediction of outcome. World J Surg. 1998;22:718–24. doi: 10.1007/s002689900459. [DOI] [PubMed] [Google Scholar]
- 6.Kupferman ME, Mandel SJ, DiDonato L, Wolf P, Weber RS. Safety of completion thyroidectomy following unilateral lobectomy for well-differentiated thyroid cancer. Laryngoscope. 2002;112:1209–12. doi: 10.1097/00005537-200207000-00013. [DOI] [PubMed] [Google Scholar]
- 7.Shaha AR, Jaffe BM. Parathyroid preservation during thyroidectomy. Am J Otolaryngol. 1998;19:113–7. doi: 10.1016/s0196-0709(98)90106-5. [DOI] [PubMed] [Google Scholar]
- 8.Prim MP, de Diego JL, Hardisson D, Madero R, Gavilan J. Factors related to nerve injury and hypocalcemia in thyroid gland surgery. Otolaryngol Head Neck Surg. 2001;124:111–4. doi: 10.1067/mhn.2001.112305. [DOI] [PubMed] [Google Scholar]
- 9.Kupferman ME, Mandel SJ, DiDonato L, Wolf P, Weber RS. Safety of completion thyroidectomy following unilateral lobectomy for well-differentiated thyroid cancer. Laryngoscope. 2002;112:1209–12. doi: 10.1097/00005537-200207000-00013. [DOI] [PubMed] [Google Scholar]
- 10.Kocher T. Ueber Kropfexstirpation und ihre folgen. Arch Klin Chir. 1883;29:254–337. [Google Scholar]
- 11.Halsted W, Evans H. The parathyroid glandules, their blood supply, and their preservation in operations upon the thyroid gland. Ann Surg. 1907;46:489–506. doi: 10.1097/00000658-190710000-00001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Page C, Strunski V. Parathyroid risk in total thyroidectomy for bilateral, benign, multinodular goiter: report of 351 surgical cases. J Laryngol Otol. 2007;121:237–41. doi: 10.1017/S0022215106003501. [DOI] [PubMed] [Google Scholar]
- 13.Gourgiotis S, Moustafellos P, Dimopoulos N, Papaxoinis G, Baratsis S, Hadjiyannakis E. Inadvertent parathyroidectomy during thyroid surgery: The incidence of a complication of thyroidectomy. Langenbecks Arch Surg. 2006;391:557–60. doi: 10.1007/s00423-006-0079-8. [DOI] [PubMed] [Google Scholar]
- 14.Lee NJ, Blakey JD, Bhuta S, Calcaterra TC. Unintentional parathyroidectomy during thyroidectomy. Laryngoscope. 1999;109:1238–40. doi: 10.1097/00005537-199908000-00010. [DOI] [PubMed] [Google Scholar]
- 15.Loré JM, Pruet CW. Retrieval of the parathyroid glands during thyroidectomy. Head Neck Surg. 1983;5:268–9. doi: 10.1002/hed.2890050313. [DOI] [PubMed] [Google Scholar]
- 16.Sakorafas GH, Stafyla V, Bramis C, Kotsifopoulos N, Kolettis T, Kassaras G. Incidental parathyroidectomy during thyroid surgery: An underappreciated complication of thyroidectomy. World J Surg. 2005;29:1539–43. doi: 10.1007/s00268-005-0032-y. [DOI] [PubMed] [Google Scholar]
- 17.McHenry CR, Speroff T, Wentworth D, Murphy T. Risk factors for post-thyroidectomy hypocalcemia. Surgery. 1994;116:641–8. [PubMed] [Google Scholar]
- 18.Akerstróm G, Malamaeus J, Bergstrom R. Surgical anatomy of human parathyroid glands. Surgery. 1984;95:14–21. [PubMed] [Google Scholar]
- 19.Abboud B. Topographic anatomy and arterial vascularization of the parathyroid glands: Practical application. Presse Med. 1996;25:1156–61. [PubMed] [Google Scholar]
- 20.Sippel RS, Ozgul O, Hartig GK, Mack EA, Chen H. Risks and consequences of incidental parathyroidectomy during thyroid resection. ANZ J Surg. 2007;77:33–6. doi: 10.1111/j.1445-2197.2006.03972.x. [DOI] [PubMed] [Google Scholar]
- 21.Sasson AR, Pinpank JF, Jr, Wetherington RW, Hanlon AL, Ridge JA. Incidental parathyroidectomy during thyroid surgery does not cause transient symptomatic hypocalcemia. Arch Otolaryngol Head Neck Surg. 2001;127:304–8. doi: 10.1001/archotol.127.3.304. [DOI] [PubMed] [Google Scholar]
- 22.Lin DT, Patel SG, Shaha AR, Singh B, Shah JP. Incidence of inadvertent parathyroid removal during thyroidectomy. Laryngoscope. 2002;112:608–11. doi: 10.1097/00005537-200204000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Abboud B, Sleilaty G, Braidy C, Zeineddine S, Ghorra C, Abadjian G, et al. Careful examination of thyroid specimen intraoperatively to reduce incidence of inadvertent parathyroidectomy during thyroid surgery. Arch Otolaryngol Head Neck Surg. 2007;133:1105–10. doi: 10.1001/archotol.133.11.1105. [DOI] [PubMed] [Google Scholar]
- 24.Rajinikanth J, Paul MJ, Deepak T, Abraham DT, Ben Selvan CK, Nair A. Surgical audit of inadvertent parathyroidectomy during total thyroidectomy: Incidence, risk factors, and outcome. Medscape J Med. 2009;11:29. [PMC free article] [PubMed] [Google Scholar]
- 25.Manouras A, Markogiannakis H, Lagoudianakis E, Antonakis P, Genetzakis M, Papadima A, et al. Unintentional parathyroidectomy during total thyroidectomy. Head Neck. 2008;30:497–502. doi: 10.1002/hed.20728. [DOI] [PubMed] [Google Scholar]
- 26.Rix TE, Sinha P. Inadvertent parathyroid excision during thyroid surgery. Surgeon. 2006;4:339–42. doi: 10.1016/s1479-666x(06)80108-3. [DOI] [PubMed] [Google Scholar]
- 27.Gagner M, Inabnet BW, Biertho L. Endoscopic thyroidectomy for solitary nodules: A feasibility study. Ann Chir. 2003;128:696–701. doi: 10.1016/j.anchir.2003.10.016. [DOI] [PubMed] [Google Scholar]
- 28.Akerström G, Rudberg C, Grimelius L, Johansson H, Lundström B, Rastad J. Causes of failed primary exploration and technical aspects of re-operation in primary hyperthyroidism. World J Surg. 1992;16:562–8. doi: 10.1007/BF02067321. [DOI] [PubMed] [Google Scholar]
- 29.Demeester-Mirkine N, Hooghe L, Van Geertruyden J, De Maertelaer V. Hypocalcemia after thyroidectomy. Arch Surg. 1992;127:854–8. doi: 10.1001/archsurg.1992.01420070118021. [DOI] [PubMed] [Google Scholar]
- 30.Schawrtz AE, Friedman EW. Preservation of the parathyroid glands in total thyroidectomy. Surg Gynecol Obstet. 1987;165:327–32. [PubMed] [Google Scholar]
- 31.Thompson NW, Reeve T. Complications of thyroid surgery: How to avoid them, how to manage them, and observations on their possible effect on the whole patient. World J Surg. 2000;24:971–5. doi: 10.1007/s002680010160. [DOI] [PubMed] [Google Scholar]
- 32.Thomusch O, Mchens A, Sekulla C, Ukkat J, Lippert H, Gastinger I, et al. Multivariate analysis of risk factors for postoperative complications in benign goiter surgery: Prospective multicenter study in Germany. World J Surg. 2000;24:1335–42. doi: 10.1007/s002680010221. [DOI] [PubMed] [Google Scholar]
- 33.Bellamy RJ, Kendall-Taylor P. Unrecognized hypocalcemia diagnosed 36 years after thyroidectomy. J R Soc Med. 1985;88:690–1. doi: 10.1177/014107689508801210. [DOI] [PMC free article] [PubMed] [Google Scholar]


