Abstract
Percutaneous vertebroplasty, among various other options, has become a mainstay in the management of osteoporotic and malignant vertebral fractures. The purpose of this article is to describe complications arising from the procedure, which can be classified as mild, which may include a temporary increase in pain and transient hypotension; moderate, including infection and extravasation of cement into the foraminal, epidural or dural space; and severe such as cement leakage in the paravertebral veins, leading to pulmonary embolism, cardiac perforation, cerebral embolism or even death. Vertebroplasty is not a procedure without complications. The article defines them and describes methods to minimize them.
Percutaneous vertebroplasty, among various other options, has become a mainstay in the management of osteoporotic and malignant vertebral fractures. When vertebroplasty is performed, careful attention to the anatomic structures is of utmost importance. Mild complications include temporary pain after the procedure and cement leakage in the intervertebral disc space and into paravertebral soft tissues. Moderate complications include infection and cement leak into the epidural space. Severe complications include leak into the paravertebral veins, leading to pulmonary embolism, cerebral embolism or cardiac perforation. The complications of vertebroplasty can be classified as follows: mild, moderate and severe.
Mild complications
The following are considered mild complications: a temporary increase in pain after the procedure; transient arterial hypotension; cement leakage into the intervertebral disc space, of little or no clinical consequence, or into the paravertebral soft tissues; and an increased risk for new fractures.
Temporary increase in pain following vertebroplasty is infrequently encountered. It is a consequence of inflammatory reaction due to heat generated by polymerization of methyl methacrylate.1 Although it rarely lasts for more than a few hours, it can be easily managed with analgesics (steroidal or nonsteroidal).
Transient arterial hypotension is a rare complication2 that can be induced by polymethyl methacrylate injection during percutaneous vertebroplasty; and although there is no clear explanation of the mechanism, it responds well to supportive measures and is self-limited.
Cement leakage into the disc during vertebroplasty (Figure 1), although of no definite clinical consequence, has a theoretical increase in the risk of subsequent fractures of adjacent vertebral bodies3 ; therefore, it is advised to place the needle laterally and far from the center of the vertebra in a centrally located fracture,3,4 and to adjust the cement consistency so that the cement is more viscous, making it less prone to leak.5 Furthermore, adjusting to smaller volumes of cement may also decrease the risk of leakage (and probably still provide sufficient stability and pain relief6 ; in addition, cessation of injection immediately when disc leakage occurs may be of benefit.7 Cement leakage into the paravertebral soft tissues occurs in 6% to 52% of cases8 and is usually of no clinical significance, with rare reports of peripheral neuropathy (Figures 2a, b). A substantial number of patients with osteoporosis develop new fractures after the procedure; two-thirds of these new fractures occur in a vertebra adjacent to those previously treated (Figure 3).9
Figure 1.

Lateral fluoroscopic view in a 49-year-old man with osteoporotic fracture of L3. Needle is in the anterior aspect of the vertebral body with cement extravasating into the L2/3 disc space (arrow).
Figure 2.
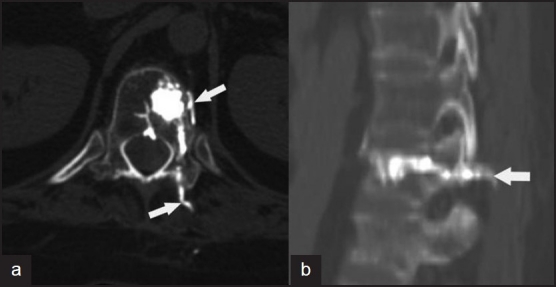
(a) Axial CT scan of a 19-year-old female with heavy steroid use for Wegner granulomatosis, 30 minutes post-vertebroplasty, showing cement leak into the paravertebral soft tissues (arrows) and muscles. (b) Sagittal reformat CT scan in the same patient; arrow shows the extent of the leak.
Figure 3.
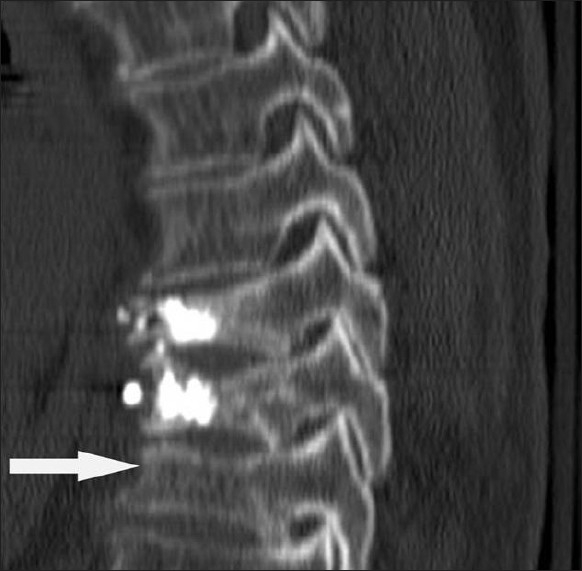
Coronal reformat CT shows a new fracture of T11 (arrow) in a 66-year-old osteoporotic woman who had undergone percutaneous vertebroplasty of T9 and T10 3 months ago, presenting with new severe back pain.
Moderate complications
These include infection, cement leak into the epidural/ foraminal space and misplaced needle in the tract.
Infection is a risk in any percutaneous procedure. It is a complication that can be eliminated or minimized. Possible results of infection are discitis, osteomyelitis; or even an epidural infection10 can occur and can be catastrophic with surgery required to remove the cement which serves as a nidus for infection.11
Extravasation of cement into the epidural (Figure 4) or foraminal space (Figure 5) is a rare complication. Most cases are clinically silent if not for post-procedure CT. The prevalence may be as high as 40%.8,12–14 Chiras et al15 reported paraplegia due to cement-related spinal cord compression to occur in only 0.4% of patients. Needle traversing of the lamina instead of the pedicle can occur, especially in the thoracic vertebra, where the pedicle is smaller, and can lead to catastrophic complications (Figure 6).
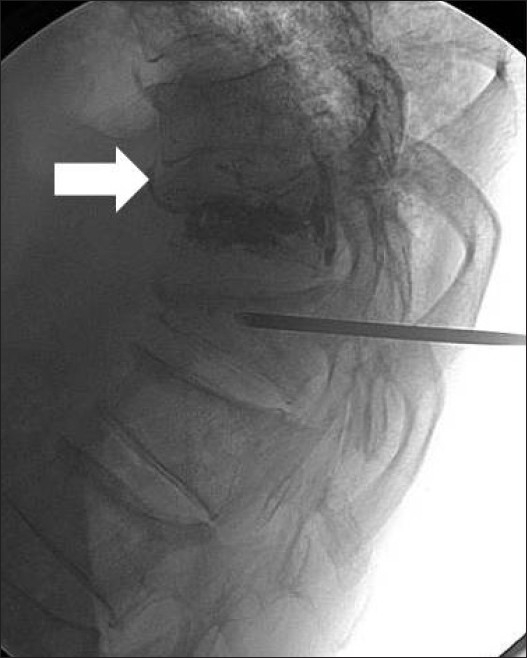
Figure 4.
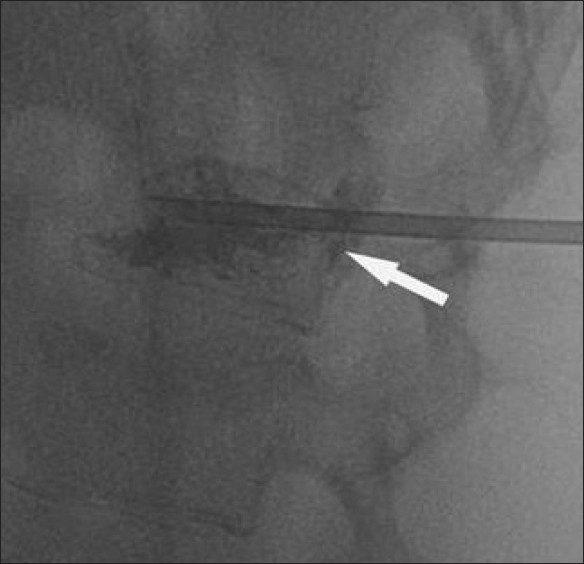
Lateral fluoroscopic image during placement of an osteoplasty needle for vertebroplasty of T11 in a 49-year-old osteoporotic man. Arrow shows an epidural leak.
Figure 5.
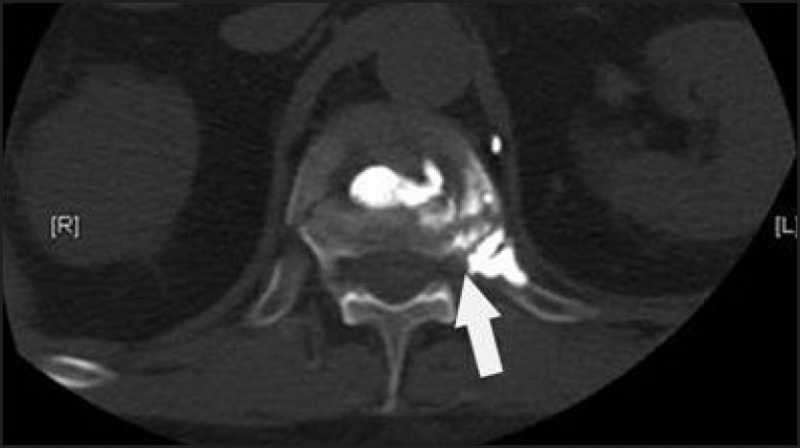
CT scan of the thoracolumbar spine post-vertebroplasty. Arrow points to the foraminal leak.
Figure 6.
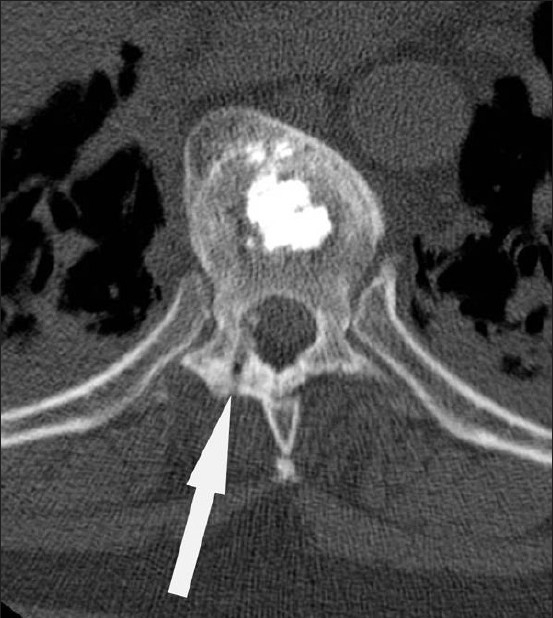
CT scan of the thoracic spine in a 79-year-old woman who underwent vertebroplasty of T11. Arrow points to lamina puncture instead of pedicle in this post-procedure CT.
Severe complications
Severe complications are usually related to cement leakage into the paravertebral veins leading to pulmonary embolism, cardiac perforation, cerebral embolism and even death. Paravertebral venous leak can be due to a combination of highly vascular lesions and liquid consistency of the cement. This leak may also produce radicular pain (Figure 7). Pulmonary cement embolism (Figure 8) is a rare complication of vertebroplasty.16 It can be asymptomatic and is reported to occur in up to 4.6% of the cases and is directly related to the frequency of paravertebral venous leak, but not to the number of vertebral bodies treated.17 If symptomatic, then classical findings of chest discomfort, hypotension, dyspnea would be observed.18 Onset can be immediate or delayed and ultimately can lead to death.19 It is managed with oxygen inhalation; short-term anticoagulation therapy; IV steroid therapy; or in severe cases, IV steroid therapy with catheter-aided interventional techniques.19–21
Figure 7.
Lateral fluoroscopic view in a 77-year-old osteoporotic woman who suffered a fracture of T11 and T12, with arrow pointing to a paravertebral venous leak.
Figure 8.
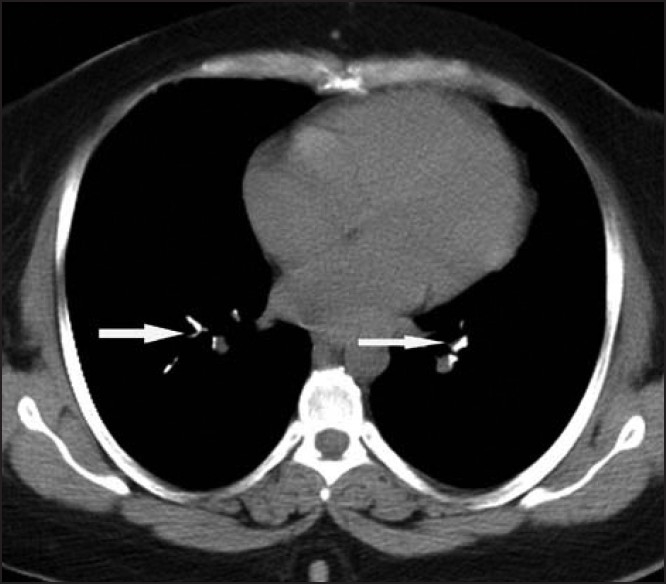
Non-enhanced CT scan of chest done in a 45-year-old woman who underwent vertebroplasty of L4 the previous day. She was complaining of chest pain and dyspnea. Arrow points to a pulmonary cement embolus.
Cardiac perforation is an extremely rare complication of vertebroplasty, with only one case report in the literature, and is potentially fatal and a cause of hemopericardium and tamponade.22 Cerebral embolus has been reported to occur and is attributed to fat emboli from raised intramedullary pressure during cementation.23 When systemic embolus is seen, it is attributed to paradoxical cerebral arterial embolization of cement via a patent foramen ovale.24 Sudden cardiovascular collapse and death during this procedure have been reported. Autopsy results demonstrate fat, bone spicules, and polymethyl methacrylate in the lungs.25
Techniques to minimize complications
Techniques include (a) choosing a transpedicular route in the lumbar spine and choosing the costovertebral junction in the thoracic spine, (b) avoiding a cortical breach whenever possible, (c) optimizing opacification of cement by following the manufacturer recommendations and by not altering recommended proportions of powder polymer and liquid polymer, and (d) defining optimal cement viscosity before injection. If cement leakage occurs, cessation of the procedure is recommended.26
REFERENCES
- 1.Cotten A, Boutry N, Cortet B, Assaker R, Demondion X, Leblond D, et al. Percutanous Vertebroplasty: State of art. RadioGraphics. 1998;18:311–20. doi: 10.1148/radiographics.18.2.9536480. [DOI] [PubMed] [Google Scholar]
- 2.Vasconcelos C, Gailloud P, Martin JB, Murphy KJ. Transient arterial hypotension induced by polymethylmethacrylate Injection during percutanous vertebroplasty. J Vascu Interv Radiol. 2001;12:1001–2. doi: 10.1016/s1051-0443(07)61584-x. [DOI] [PubMed] [Google Scholar]
- 3.Lin EP, Ekholm S, Hiwatashi A, Westesson PL. Vertebroplasty: Cement leakage into the disc increases the risk of new fracture of adjacent vertebral body. AJNR Am J Neuroradiol. 2004;25:175–80. [PMC free article] [PubMed] [Google Scholar]
- 4.Peh WC, Gilula LA, Peck DD. Percutaneous vertebroplasty for severe osteoporotic vertebral body compression fractures. Radiology. 2002;223:121–6. doi: 10.1148/radiol.2231010234. [DOI] [PubMed] [Google Scholar]
- 5.Gilula L. Is insufficient use of polymethylmethacrylate a cause for vertebroplasty failure necessitating repeat vertebroplasty? AJNR Am J Neuroradiol. 2003;24:2120–2. [PMC free article] [PubMed] [Google Scholar]
- 6.Ryu KS, Park CK, Kim MC, Kang JK. Dose-dependent epidural leakage of polymethylmethacrylate after percutaneous vertebroplasty in patients with osteoporotic vertebral compression fractures. J Neurosurg. 2002;96:56–61. doi: 10.3171/spi.2002.96.1.0056. [DOI] [PubMed] [Google Scholar]
- 7.Jensen ME, Evans AJ, Mathis JM, Kallmes DF, Cloft HJ, Dion JE. Percutaneous polymethylmethacrylate vertebroplasty in the treatment of osteoporotic vertebral body compression fractures: Technical aspects. AJNR Am J Neuroradiol. 1997;18:1897–904. [PMC free article] [PubMed] [Google Scholar]
- 8.Laredo JD, Hamze B. Complications of vertebroplasty and their prevention. Semin Ultrasound CT MR. 2005;26:65–80. doi: 10.1053/j.sult.2005.02.003. [DOI] [PubMed] [Google Scholar]
- 9.Uppin AA, Hirsch JA, Centenera LV, Pfiefer BA, Pazianos AG, Choi IS. Occurrence of new vertebral body fracture after percutaneous vertebroplasty in patients with osteoporosis. Radiology. 2003;226:119–24. doi: 10.1148/radiol.2261011911. [DOI] [PubMed] [Google Scholar]
- 10.Chiras J, Deramond H. Complications desvertbroplasties. In: Saillant G, Laville C, editors. Echecs CT complications de Ia chirurgie du rachis: Chirurgie de reprise. Paris France: Sauramps Medical; 1995. pp. 149–53. [Google Scholar]
- 11.Yu SW, Chen WJ, Lin WC, Chen YJ, Tu YK. Serious pyogenic spondylitis following vertebroplasty- a case report. Spine. 2004;29:E209–11. doi: 10.1097/00007632-200405150-00023. [DOI] [PubMed] [Google Scholar]
- 12.Cotten A, Dewatre F, Cortet B, Assaker R, Leblond D, Duquesnoy B, et al. Percutanous vertebroplasty for osteolytic metastasis and myeloma. Radiology. 1996;200:525–30. doi: 10.1148/radiology.200.2.8685351. [DOI] [PubMed] [Google Scholar]
- 13.Ratliff J, Nguyen T, Heiss J. Root and spinal cord compression from methylmethacrylate vertebroplasty. Spine. 2001;26:E300–2. doi: 10.1097/00007632-200107010-00021. [DOI] [PubMed] [Google Scholar]
- 14.Lopes NM, lopes VK. Paraplegia complicating percutanous vertebroplasty for osteoporotic vertebral fracture: Case report. Arq Neuropsiquiatr. 2004;62:879. doi: 10.1590/s0004-282x2004000500027. [DOI] [PubMed] [Google Scholar]
- 15.Chiras J, Depriester C, Weill A, Sola-Martinez MT, Deramond H. Percutanous vertebroplasty surgey; techniques and indications. J Neuroradiol. 1997;24:45–59. [PubMed] [Google Scholar]
- 16.Jang JS, Lee SH, Jung SK. Pulmonary embolism of polymethylmethacrylate after percutaneous vertebroplasty: A report of three cases. Spine. 2002;27:E416–8. doi: 10.1097/00007632-200210010-00021. [DOI] [PubMed] [Google Scholar]
- 17.Choe DH, Marom EM, Ahrar K, Truong MT, Madewell JE. Pulmonary embolism of polymethyl methacrylate during percutaneous vertebroplasty and kyphoplasty. AJR Am J Roentgenol. 2004;183:1097–102. doi: 10.2214/ajr.183.4.1831097. [DOI] [PubMed] [Google Scholar]
- 18.Syed MI, Jan S, Patel NA, Shaikh A, Marsh RA, Stewart RV. Fatal fat embolism after vertebroplasty: Identification of the high-risk patient. AJNR AM J Neuroradiol. 2006;27:343–5. [PMC free article] [PubMed] [Google Scholar]
- 19.Yoo KH, Jeong SW, Yoon W. Acute respiratory distress syndrome associated with pulmonary cement embolism following percutaneous vertebroplasty with polymethylmethacrylate. Spine. 2004;29:E294–7. doi: 10.1097/01.brs.0000131211.87594.b0. [DOI] [PubMed] [Google Scholar]
- 20.Jang JS, Lee SH, Jung SK. Pulmonary embolism of polymethylmethacrylate after percutaneous vertebroplasty: A report of three cases. Spine. 2002;27:E416–8. doi: 10.1097/00007632-200210010-00021. [DOI] [PubMed] [Google Scholar]
- 21.Yoo KY, Jeong SW, Yoon W, Lee J. Acute respiratory distress syndrome associated with pulmonary cement embolism following percutaneous vertebroplasty with polymethylmethacrylate. Spine. 2004;29:E294–7. doi: 10.1097/01.brs.0000131211.87594.b0. [DOI] [PubMed] [Google Scholar]
- 22.Kim SY, Seo JB, Do KH, Lee JS, Song KS, Lim TH. Cardiac perforation caused by acrylic cement: A rare complication of percutaneous vertebroplasty. Am J Roentgenol. 2005;185:1245–7. doi: 10.2214/AJR.04.1443. [DOI] [PubMed] [Google Scholar]
- 23.Edmonds CR, Barbut D, Hager D, Sharrock NE. Intraoperative cerebral arterial embolization during total hip arthroplasty. Anesthesiology. 2000;93:315–8. doi: 10.1097/00000542-200008000-00006. [DOI] [PubMed] [Google Scholar]
- 24.Christie J, Burnett R, Potts HR, Pell AC. Echocardiography of transatrial embolism during cemented and uncemented hemiarthroplasty of the hip. J Bone Joint Surg Br. 1994;76:409–12. [PubMed] [Google Scholar]
- 25.Childers JC., Jr Cardiovascular Collapse and Death during Vertebroplasty [letter] Radiology. 2003;228:902–3. doi: 10.1148/radiol.2283030235. [DOI] [PubMed] [Google Scholar]
- 26.Heran MK, Legiehn GM, Munk PL. Current concepts and techniques in percutanous vertebroplasty. Orthop Clin North Am. 2006;37:409–34. doi: 10.1016/j.ocl.2006.05.001. [DOI] [PubMed] [Google Scholar]


