Abstract
The purpose of the study is to assess frequency and determinants of discussions between HIV-infected women and their HIV providers about childbearing plans, and to identify unmet need for reproductive counseling. We conducted a cross-sectional, audio computer-assisted self-interview (ACASI) among 181 predominately African American HIV-infected women of reproductive age receiving HIV clinical care in two urban health clinics. We used descriptive statistics to identify unmet need for reproductive counseling by determining the proportion of women who want to, but have not, discussed future reproductive plans with their primary HIV care provider. Multivariate analysis determined which factors were associated with general and personalized discussions about pregnancy. Of the 181 women interviewed, 67% reported a general discussion about pregnancy and HIV while 31% reported a personalized discussion about future childbearing plans with their provider. Of the personalized discussions, 64% were patient initiated. Unmet reproductive counseling needs were higher for personalized discussions about future pregnancies (56%) than general discussions about HIV and pregnancy (23%). Younger age was the most powerful determinant of provider communication about pregnancy. A significant proportion of HIV-infected women want to talk about reproductive plans with their HIV provider; however, many have not. HIV care providers and gynecologists can address this unmet communication need by discussing reproductive plans with all women of childbearing age so that preconception counseling can be provided when appropriate. Providers will miss opportunities to help women safely plan pregnancy if they only discuss reproductive plans with younger patients.
Introduction
In the context of HIV clinical care, open discussion regarding sexual health and reproductive plans have become increasingly relevant as the number of HIV-infected women of reproductive age increases.1 Preconception care across the reproductive lifespan is a critical component of comprehensive primary care for HIV-infected women.2 Because of the potential to significantly reduce transmission risks to the partner while trying to become pregnant and to the infant during pregnancy and delivery, HIV-infected women have a heightened need for guidance from HIV providers and obstetrician–gynecologists prior to attempting pregnancy.2–6
With advances in prevention and treatment achieved by highly active antiretroviral therapy (HAART), more HIV-infected women are pursuing childbearing.7,8 In countries with widespread access to HAART, including Brazil and South Africa, many HIV-infected women and men express the desire to have children.9–12 When providers are aware of patients' reproductive desires and intentions, they can assist women in obtaining preconception counseling, which for HIV-infected women includes: (1) improving health before conception, (2) identifying risk factors for adverse maternal or fetal outcomes and intervening to optimize outcomes, (3) preventing transmission of HIV to infants as well as sexual partners,2 and (4) ensuring a reliable contraception method until ready to attempt conception and again postpartum. Furthermore, providers can avoid administering potentially teratogenic drugs during pregnancy such as efavirenz-containing regimens,13 and ensure early prenatal care to support healthy pregnancies and adherence to prophylactic and treatment regimens.
Despite the many benefits of discussing childbearing plans with HIV-infected women of reproductive age, these discussions often occur too late, after conception has occurred.14 In a Swiss study, nearly half (47%) of HIV-infected patients felt health care providers would not sufficiently address their concerns regarding relationships, sexuality, and fertility intentions.11 The reality is that there are few available data regarding the occurrence and content of reproductive discussions between HIV-infected women and their providers. This study aims to addresses this gap by assessing: (1) how many HIV-infected women want to discuss childbearing with their providers, (2) how many discussions actually occur, and (3) determinants of these discussions.
Methods
Study sample and procedures
HIV-infected women of reproductive age receiving clinical care from two HIV medical clinics associated with an urban academic medical center were recruited from clinic waiting rooms or referred by providers between August 2007 and April 2008. An anonymous, cross-sectional, audio computer-assisted self-interview (ACASI) survey was used to assess fertility desires and intentions and communication with HIV providers about pregnancy. Participants were between 15 and 44 years of age and current clients of the clinics. Exclusion criteria were current pregnancy and history of hysterectomy. Oral informed consent was provided for participation in the survey and to permit review of medical records. All procedures were approved by the Institutional Review Board. More detailed study procedures are reported elsewhere.15
Measures
The primary outcome variables for this analysis include patient's reports of general and personalized communication about HIV and pregnancy with a primary HIV care provider. General communication about HIV and pregnancy was measured by the question: “Has your HIV doctor spoken with you about issues and concerns related to pregnancy in HIV-infected women?” Personalized communication, specific to the woman's future fertility goals, was measured by the question: “Have you and your HIV doctor spoken about future pregnancies?” The response options for both questions were “yes” or “no.” If a more personalized discussion regarding fertility plans had occurred, participants were asked two follow-up questions. First, “Who initiated the conversation?” with response options of “You brought it up” or “Your HIV doctor brought it up.” Second, “What was discussed?” with respondents selecting any or all of the following response options: “Prevention of mother-to-child transmission (MTCT), medications during pregnancy, challenges becoming pregnant, safe conception and other.”
To identify how many women are interested in discussing childbearing with their HIV provider, women were asked “Do you want to talk with your HIV doctor about pregnancy?” Response options were “yes” or “no.”
To assess fertility desire and intention, respondents were asked two separate questions; “How many children do you want to have in the future?” and “How many children do you expect to have in the future?” Women who reported a number greater than zero were coded as desiring or intending a future child. The distinction between childbearing desires and expectations among people living with HIV was made clear to participants and was previously examined by Chen and colleagues.12
Data analysis
Descriptive statistics were used to determine the proportion of women who want to discuss and have discussed future reproductive plans with their primary HIV care provider (and/or gynecologist). To test associations of demographic, individual, and clinical factors with provider communication we used bivariate logistic regression with dichotomous variables and t tests with continuous variables. We used backward stepwise selection to identify variables significant at p < 0.05 for inclusion in the multivariate models to determine factors associated with both general and personalized provider communication.
Results
Sample characteristics
Study participants (n = 181) were predominately African-American (88%), with a mean age of 32.4 years (Table 1). Thirty-five percent of women were childless and 38% had at least one child since their HIV diagnosis. Among sexually active women, 62% had an HIV-negative sexual partner and 11% did not know their partner's HIV serostatus. Consistent condom use, however, is low (28%), 25% reported using no method to avoid pregnancy or HIV/sexually transmitted infection (STI) transmission, and 22% have had a tubal ligation. History of drug use was reported by 23% of women. Laboratory records were available for over 91% of the sample. Nearly 70% were on HAART, among whom 39% had an undetectable plasma viral load.
Table 1.
Characteristics of HIV-Infected Women Included in the Sample (n = 181)
| Characteristic | n (%) |
|---|---|
| Mean age | 32.4 |
| 15–19 | 27 (15) |
| 20–29 | 38 (21) |
| 30–39 | 66 (36) |
| 40–44 | 50 (28) |
| Race/ethnicity | |
| African American | 159 (88) |
| White | 18 (10) |
| Hispanic | 4 (2) |
| Number of children | |
| 0 | 64 (35) |
| 1 | 26 (15) |
| 2 | 29 (16) |
| ≥3 | 62 (34) |
| Insurance status | |
| Uninsured/unknown | 28 (15.5) |
| Medicaid/Ryan White | 142 (79) |
| Private | 10 (5.5) |
| Sexual orientation | |
| Heterosexual | 158 (87) |
| Bisexual | 19 (10.5) |
| Lesbian | 3 (1.6) |
| HIV risk group | |
| Heterosexual sex | 101 (56) |
| Perinatal transmission | 28 (16) |
| Injection drug use | 21 (12) |
| Unknown | 27 (15) |
| Previous pregnancy with HIV+ status | |
| Yes | 69 (59) |
| No | 48 (41) |
| Relationship status | |
| Married | 23 (13) |
| In committed relationship | 77 (43) |
| Dating, uncommitted relationship | 37 (20) |
| Not in a relationship | 44 (24) |
| HIV status of partnera | |
| Positive | 45 (27) |
| Negative | 103 (62) |
| Unknown | 18 (11) |
| Consistent condom use with primary partner (n = 166) | |
| 100% | 47 (28) |
| 0% | 41 (25) |
| Tubal ligation | |
| Yes | 41 (22) |
| % felt somewhat pressured | 9 (22) |
| % moderately to very unsatisfied | 8 (19) |
| On HAART | |
| Yes | 120 (69) |
| No | 53 (31) |
| Mean CD4 count (n = 173) | 460 |
| <200 | 120 (69) |
| >500 | 53 (31) |
| Mean viral load (n = 165) | 30996 |
| Undetectable <50 | 64 (39) |
| >100,000 | 12 (7) |
| AIDS diagnosisb | |
| Yes | 74 (43) |
| No | 99 (57) |
As reported by participant.
AIDS defined due to an opportunistic infection or ever having a CD4 count <200.
HAART, highly active retroviral therapy.
The majority of women in this sample (59%) want to have a child in the future, of whom 66% intend to have a child. Nearly 60% of women under age 30 intend to have a child in the future, while 28% of women between 30 and 44 years intend to have a child. When examining childless women or those with only one child; 60% of younger and 33% of older women intend to have children.
Communication with HIV provider
Approximately two thirds of women (67%, n = 121), reported ever having a general discussion about issues and concerns related to HIV and pregnancy. Almost half of these women (49%) had also talked with their gynecologist about these issues.
Satisfaction with primary HIV-provider communication was high (80%) and 65% said they would feel somewhat to very comfortable talking to their provider about trying to become pregnant in the future, if they so desired.
Of the total sample, 31% of women reported a personalized discussion with their HIV provider about their own fertility desires and intentions. Among these women, 64% reported initiating the conversation with their provider. Interestingly, these women were 62% less likely to report incongruence between their fertility desires and fertility intentions compared to those who had not had a personalized discussion (odds ratio [OR] 0.38, 95% confidence interval [CI] (0.45–0.97), p = 0.044). Among personalized discussions with providers about pregnancy, the most frequently discussed topics were minimizing the risk of MTCT (61%), HIV prevention for one's partner or safe conception (48%), medications during pregnancy (45%), and challenges with becoming pregnant (32%). Other topics included psychological readiness for motherhood, birth spacing, breastfeeding, and the option to reverse a tubal ligation.
Unmet need for reproductive counseling
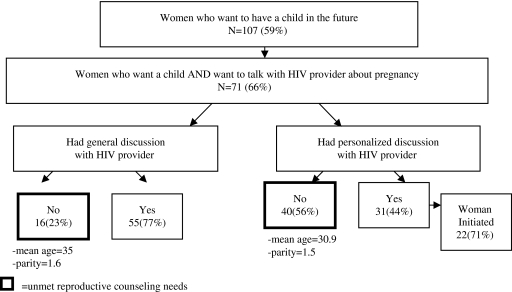
To identify the most imminent unmet need for reproductive counseling, we stratified by fertility desire and desire to talk with a provider about pregnancy (Fig. 1). We included women who had elected sterilization because 32% of women with a tubal ligation reported the desire to talk with their HIV provider about pregnancy. The unmet need for reproductive counseling is defined as the absence of communication about pregnancy and safe conception among women who report both the desire to have a child and the desire to talk with their HIV provider about fertility plans. Nearly 40% of the sample reported the desire for a future child and the desire to talk with their provider; yet 23% of these women have had no communication with their provider about pregnancy and HIV. This unmet need for reproductive counseling is significantly greater for personalized communication about future pregnancies. Unmet need for reproductive counseling rose from 23% for general discussion about HIV and pregnancy to 56% for personalized communication with providers about future pregnancies.
FIG. 1.
Unmet reproductive counseling needs: Women who want to have a child and want to talk with their HIV provider about pregnancy, but have not.
Concerns about infertility and tubal ligations
Some HIV-infected women experience challenges in getting pregnant but nevertheless report the desire to have future biological children. We examine two such groups. First, approximately 14% (n = 25) of HIV-infected women in the sample have tried unsuccessfully to become pregnant for at least 1 year (approximately half trying >2 years), and 76% of these women reported asking their HIV provider or gynecologist for guidance in becoming pregnant. The mean viral load of this subgroup is moderately high at 30,344 copies per milliliter.
Second, 22% (n = 41) of the sample have had a tubal ligation, providing a permanent form of birth control. Nonetheless, 37% of these women reported the desire to have a child and two of these women reported personalized discussions with their HIV providers about reversing their operation in hopes of conceiving a child.
Factors associated with provider communication among HIV-infected women
We used bivariate and multivariate logistic regression to identify factors associated with discussions about pregnancy and future childbearing with HIV care providers (Table 2). We explored this for both general and personalized communication about HIV and pregnancy.
Table 2.
Bivariate and Multivariate Logistic Regression to Identify Associations with Provider Communication about Pregnancy with HIV-Infected Women of Reproductive Age (General and Personalized Communication), n = 181
| |
General communication |
Personalized communication |
||
|---|---|---|---|---|
| OR (95% CI) | AOR (95% CI) | OR (95% CI) | AOR (95%CI) | |
| Age (<30 yrs) | 6.2 (2.7–13.6)a | 5.1 (2.3–11)a | 3.2 (1.6–6.1)b | 2.7 (1.4–5.3)b |
| Provider gender (female) | 2.5 (1.2–4.9)a | 1.07 (0.52–2.2),NS | ||
| Want to discuss pregnancy (yes) | 2.13 (1.1–4.0)c | 2.77 (1.4–5.4)b | 2.3 (1.2–4.6)c | |
| Want to have a child (yes) | 2.4 (1.3–4.5)b | 1.9 (0.98–3.7), | ||
| Parity (0 or 1 child) | 1.46 (0.79–2.7) NS | 1.9 (1.002–3.6)c | ||
| Undetectable VL | 0.87 (0.43–1.7) NS | 0.89 (0.43–1.8) NS | ||
| HAART | 0.98 (0.49–1.9) NS | 0.94 (0.47–1.9) NS | ||
| AIDS diagnosis | 0.44 (0.21–81)b | 0.53(.27–1.1) NS | 0.99 (0.5–1.8) NS | |
| Insurance status public | ||||
| Public assist (ref) | ||||
| Private Insurance | 0.42 (0.31–1.7) NS | 1.8 (0.81–4.2) NS | ||
p < 0.001.
p < 0.01.
p < 0.05.
Multivariate analysis conducted only with significant (<0.05), and marginally significant (<0.10) bivariate variables, controlling for study site. OR, odds ratio; CI, confidence interval; AOR, adjusted odds ratio; VL, viral load; NS, not significant; HAART, highly active antiretroviral therapy.
In bivariate analysis, age was the strongest determinant of communication about pregnancy. Younger women (under age 30) were six times more likely to have general (OR 6.2, 95% CI [2.7–13.6], p < 0.001) and three times more likely to have personalized (OR 3.2, 95% CI [1.6–6.1], p = 0.001) discussions about pregnancy than women aged 30 or older. HIV infected women with no or only one child were twice as likely to have a personalized conversation about future pregnancies with their provider compared to those with two or more children (OR 1.9, 95% CI [1.002–3.6], p = 0.049).
Women who expressed interest in talking with their HIV provider about pregnancy were twice as likely to have a general discussion about pregnancy and nearly three times as likely to have a personalized discussion about future childbearing plans (OR 2.13, 95% CI [1.1–4.0], p = 0.02 and OR 2.77, 95% CI [1.4–5.4], p = 0.003, respectively). Likewise, women who want to have a child in the future were also more likely to have had a general and personalized discussion with their HIV provider (OR 2.4, 95% CI [1.3-4.5], p = 0.007) and (OR 1.9, 95% CI [0.98–3.7], p = 0.056), respectively. Women reporting personalized discussions with their HIV provider were nearly three times more likely to report accurate knowledge of MTCT risk with HAART, defined as 1% or 2% (OR 2.8, 95% CI [1.2–6.6], p = 0.013). The association between general discussions about pregnancy and accurate knowledge of MTCT was marginally significant (OR 2.4, 95%CI (.87-4.8), p = 0.08).
Patients with female providers were over twice as likely to report a general discussion of issues with HIV and pregnancy (OR 2.5, 95%CI [1.2–4.9], p = 0.008). Provider gender, however, was not associated with the likelihood of a personalized discussion on the topic. Patients with an AIDS diagnosis were half as likely to have had a general discussion about pregnancy with their provider (OR 0.44, 95% CI (0.23–0.85), p = 0.01).
In the multivariate model for general communication about HIV and pregnancy (Table 2), only patient age retained statistical significance. Younger women were five times more likely to have talked with their provider about pregnancy than women over 30 (adjusted odds ratio [AOR] 5.1, 95% CI [2.3–11], p < 0.001). Likewise, younger age remained significantly associated with personalized communication about future childbearing with younger women nearly three times more likely to have these discussion (AOR 2.7, 95% CI [1.4–5.3], p = 0.004). Women who reported the desire to talk about pregnancy with one's HIV provider were over twice as likely to have had a personalized discussion about future pregnancies than women who did not report this desire (AOR 2.3, 95% CI [1.2–4.6], p = 0.018). We found no interaction effect between patient age and the desire to talk with one's HIV provider about pregnancy. In summary, age (younger than age 30) is the strongest predictor of provider communication (both general and personalized) regarding pregnancy and future reproductive plans.
Discussion
Reproductive counseling among HIV-infected women of childbearing age is not universal. The absence of personalized communication is particularly troubling among women who have pregnancy desires and want to discuss them with their HIV provider, but have not (40/71, 56%). Given the important health-oriented topics covered in the personalized discussions, which are positively associated with accurate knowledge of MTCT risk, the 56% unmet need for personalized reproductive counseling warrants attention to improve women's health, their understanding of transmission risks, and the health of their partners and future children. Given the high level of specialty care provided at the study sites, it is likely these data represent a best case scenario for the integration of reproductive counseling in HIV clinical care.
The multivariate analysis identified younger age as the only significant determinant of a general discussion about HIV and pregnancy. Younger age has been positively associated with fertility intentions in several studies among HIV-infected women,11,12,16–20 and is a logical and obvious cue to prompt provider discussions about reproductive plans. Among this same sample of women, however, young patient age (<30 years) was not significantly associated with fertility intentions after controlling for parity, childbearing motivations, fertility desires, perceived partner desire for a child, knowledge of MTCT, and an AIDS diagnosis (AOR 1.4, p = 0.5).15 The reliance on young age alone to prompt discussions about pregnancy among this population is particularly troubling as 28% of women sampled between 30–44 years both desire and intend to have a child in the future. Neglecting this issue with women in their thirties and forties may result in missed opportunities to prevent HIV transmission and provide adequate support to women.
Younger women (<30 years of age) and those who want to talk with their provider about pregnancy were significantly more likely to have personalized conversations with their provider about pregnancy. This corresponds with our finding that the majority of women who had these discussions (64%), initiated the conversations. Furthermore, these women were 62% less likely to have incongruence between their desires and intentions. These findings suggest two take-away messages. First, women—not providers—are more likely to initiate conversations. Second, women whose desires and intentions match-up are more likely to initiate these conversations. Hence, a major barrier to communication is that providers are not initiating discussions. Furthermore, and perhaps more alarmingly, an ambivalent subset of women are especially vulnerable because they are not initiating a conversation they may need to: (1) prevent unintended pregnancies, (2) protect themselves and others in optimizing conception practices, and (3) learn how to cope with and manage their ambivalence about childbearing.
The proportion of women with viral suppression on HAART in this sample (39%) is lower than the estimated 60–65% among all patients on HAART.21 Significantly higher proportions of viral suppression (73–81%) have been reported among pregnant women who initiated HAART during pregnancy and achieved viral suppression before delivery.22,23 Many of the urban women sampled have characteristics associated with lower viral suppression including a long duration of infection (27% infected ≥15 years), history of drug use24 (23%), adolescence,25 or perinatal infection26 (15% perinatally infected adolescents). Significant disparities in viral suppression are observed among African Americans,27 whom comprise 88% of our sample. Desire for childbearing appears high regardless of viral load. Challenges achieving an undetectable viral load have significant implications for both sexual and perinatal transmission, and thus further indicate the importance of discussing childbearing plans with HIV-infected women of reproductive age and specialized counseling for those considering childbearing.
Implications for research and practice
Providers must feel comfortable discussing fertility plans with all women of reproductive age—from adolescents to women in their forties. Many providers treating women in the general population do not broach sexuality issues because they (1) lack training and skills to deal with human sexuality concerns, (2) may feel personal discomfort with the subject, (3) fear offending the patient, or (4) avoid the topic due to concerns about time constraints.28,29 Although HIV providers are more likely to discuss sexual health with their patients, communication does not appear adequate in light of the needs reported by HIV-infected individuals in this study. Additional training may be required to increase providers' level of comfort discussing childbearing options and providing referrals for more specialized preconception counseling as appropriate. Otherwise, reproductive counseling may be contingent on the provider's level of comfort and interest in discussing the topic with patients, or an individual's initiative to inquire about the topic.
Given the stigma HIV-infected women may experience when considering childbearing,30 they may have a heightened fear of disapproval from their HIV provider. As a result these women may hesitate or avoid discussing their desire for childbearing, and may rely on the provider to initiate the conversation. If communication is not initiated by the provider, it may only occur after pregnancy. Further, discussions about reproductive options should be customized as women who have already chosen sterilization and are happy with their decision will not benefit from extensive discussion. Barriers to the best practice of universal reproductive counseling within HIV clinical care settings should be identified by future studies that include providers.
One of the potential barriers in routine discussion of childbearing plans is provider discomfort in the setting of a serodiscordant relationship. Assisted reproductive technologies can facilitate safe conception among HIV serodiscordant couples avoiding risk to uninfected partners.3–6 Nonetheless, the options are very expensive and rarely covered by health insurance, putting them beyond reach of most people living with HIV. Although larger studies are needed, there is compelling evidence from Barreiro and colleagues5,6 that natural conception can be considered a possible alternative for HIV serodiscordant couples, as long as: (1) complete suppression of viremia with HAART is achieved in the infected partner, (2) any STIs are treated and resolved, (3) the fertility potential of each partner has been confirmed, and (4) couples receive expert reproductive counseling prior to any attempt at conception. When the woman is HIV positive but the male partner is HIV negative, home insemination for transfer of semen can easily be learned and is effective in preventing exposure to infected secretions while attempting to conceive (J. Anderson, personal communication, May 2009). Among HIV-infected women in our study, 73% reported having a partner with a seronegative or unknown status. It is critical that providers play a role in guiding serodiscordant couples through the process to minimize risk to the uninfected partner.
It is unknown what proportion of HIV-infected women of reproductive age are aware of their options to reduce transmission to an uninfected partner. In-depth qualitative interviews with nine HIV-infected women found there was insufficient knowledge of how to reduce partner transmission risk in relation to childbearing.31 HIV providers and obstetrician-gynecologists are likely the most accessible and accurate source for reproductive counseling to impart this knowledge. Women who express a desire for a future pregnancy, those who are not trying to conceive but are not using appropriate contraception consistently, or who express uncertainty about reproductive plans can all benefit from preconception counseling.32
Data documenting women's current awareness of preconception counseling, the potential demand for such services, and perceived barriers to utilization will inform programmatic efforts to reach women with such services. Additionally, more specificity regarding how discussions concerning pregnancy are initiated, if they occur on more than one occasion, and more detailed reporting of the content covered is needed in future research to identify gaps in provider communication.
Limitations
Because of our cross-sectional study design we could not determine who is prompting the general discussion about pregnancy and HIV. The follow-up question regarding who initiated the conversation was only asked about the personalized discussion about future childbearing. It is therefore uncertain if it is the woman's desire to discuss fertility that prompts her to raise the topic with the provider, or if her desire to discuss fertility is apparent in subtle ways that motivate the provider to initiate the discussion of childbearing. Or, it could reflect the provider characteristic of being thorough in discussing fertility plans with all female patients of reproductive age.
This study relied on patient reports of discussions about pregnancy, as providers were not included in the study. It is possible that more discussion about pregnancy occurred than was recalled by female participants.
The generalizability of these findings is limited due to convenience sampling and the potential for selection bias. This study was conducted at a teaching hospital where practitioners are expected and encouraged to apply best practices. Both study sites had specialized HIV providers in a city with one of the highest HIV prevalence rates in the country. It is likely that provider communication about HIV and pregnancy in this study occur more frequently than in other areas where HIV is less prevalent. Furthermore, perceived stigma from health care providers may be lower in these clinics with dedicated HIV care teams compared to areas of the country with fewer HIV-infected people and less comprehensive services. Hence, these findings most likely underestimate the unmet need for reproductive counseling among HIV-infected women.
These findings highlight provider communication about childbearing among a predominately African-American, lower socioeconomic, urban population of women living with HIV who receive clinic-based care. Our study sample reflects the group of women most affected by HIV in the United States, and contributes to the literature on provider communication about childbearing among HIV-infected women for which few data exist.
Furthermore, the findings suggest those providing care to HIV-infected women of reproductive age can improve their efforts to comprehensively discuss issues related to HIV and pregnancy, including personalized and sensitive inquiry about women's immediate and long-term fertility desires and intentions. Universal communication about future reproductive desires and intentions can reduce missed opportunities to offer guidance to those with childbearing interests, help reduce stigma by normalizing childbearing among women living with HIV, and assist women to avoid unintended pregnancies.
Acknowledgments
We are grateful to the Women's HIV Program for providing funds for participant remuneration, and acknowledge Rosemary Ramroop, Jennifer Gaver, and Angela Williams for their valuable assistance with participant recruitment. We sincerely thank the adolescent and adult women who participated in this study.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Centers for Disease Control and Prevention. Fact sheet: Estimates of new HIV infections in the United States. 2008. www.cdc.gov/hiv/topics/surveillance/resources/factsheets/incidence.htm. [Dec 12;2008 ]. www.cdc.gov/hiv/topics/surveillance/resources/factsheets/incidence.htm
- 2.Aaron EZ. Criniti SM. Preconception health care for HIV-infected women. Top HIV Med. 2007;15:137–141. [PubMed] [Google Scholar]
- 3.Semprini AE. Hollander LH. Vucetich A. Gilling-Smith C. Infertility treatment for HIV-positive women. Womens Health. 2008;4:369–382. doi: 10.2217/17455057.4.4.369. [DOI] [PubMed] [Google Scholar]
- 4.Barreiro P. del Romero J. Leal M. Hernando V. Asencio R. de Mendoza C. (2006). Natural pregnancies in HIV-serodiscordant couples receiving successful antiretroviral therapy. J Acquir Immune Defic Syndr. 2006;43:324–326. doi: 10.1097/01.qai.0000243091.40490.fd. [DOI] [PubMed] [Google Scholar]
- 5.Barreiro P. Duerr A. Beckerman K. Soriano V. Reproductive options for HIV-serodiscordant couples. AIDS Rev. 2007;8:158–170. [PubMed] [Google Scholar]
- 6.Barreiro P. Castilla JA. Labarga P. Soriano V. Is natural conception a valid option for HIV-serodiscordant couples? Hum Reprod. 2007;22:2353–2358. doi: 10.1093/humrep/dem226. [DOI] [PubMed] [Google Scholar]
- 7.Klein J. Pena JE. Thornton MH. Sauer MV. Understanding the motivations, concerns, and desires of human immunodeficiency virus 1-serodiscordant couples wishing to have children through assisted reproduction. Obstet Gynecol. 2003;101(5 Pt 1):987–994. doi: 10.1016/s0029-7844(03)00012-7. [DOI] [PubMed] [Google Scholar]
- 8.Sharma A. Feldman JG. Golub ET, et al. Live birth patterns among human immunodeficiency virus-infected women before and after the availability of highly active antiretroviral therapy. Am J Obstet Gynecol. 2007;196:541.e1–541.e6. doi: 10.1016/j.ajog.2007.01.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Myer L. Morroni C. Rebe K. Prevalence and determinants of fertility intentions of HIV-infected women and men receiving antiretroviral therapy in South Africa. AIDS Patient Care STDS. 2007;21:278–285. doi: 10.1089/apc.2006.0108. [DOI] [PubMed] [Google Scholar]
- 10.Nóbrega AA. Oliveira FA. Galvão MT, et al. Desire for a child among women living with HIV/AIDS in northeast Brazil. AIDS Patient Care STDs. 2007;21:261–267. doi: 10.1089/apc.2006.0116. [DOI] [PubMed] [Google Scholar]
- 11.Panozzo L. Battegay M. Friedl A. Vernazza PL. Swiss Cohort Study. High risk behaviour and fertility desires among heterosexual HIV-positive patients with a serodiscordant partner—Two challenging issues. Swiss Med Wkly. 2003;133:124–127. doi: 10.4414/smw.2003.10124. [DOI] [PubMed] [Google Scholar]
- 12.Chen JL. Philips KA. Kanouse DE. Collins RL. Miu A. Fertility desires and intentions of HIV-positive men and women. Fam Plann Perspect. 2001;33:144–152, 165. [PubMed] [Google Scholar]
- 13.U.S. Public Health Service Task Force. Recommendations for use of antiretroviral drugs in pregnant HIV-infected women for maternal health and interventions to reduce perinatal HIV transmission in the United States. 2005. 2005. http://aidsinfo.nih.gov. [Mar 17;2010 ]. http://aidsinfo.nih.gov Updated July, 2008.
- 14.Bridge D. Hodder A. Squires K, et al. Clinicians fail to routinely provide reproductive counseling to HIV-infected women in the United States [Abstract TUPE0911]; Presented at the XVII International AIDS Conference; Mexico City, Mexico. Aug 3–8;2008 . [Google Scholar]
- 15.Finocchario-Kessler S. Sweat M. Dariotis J, et al. Understanding high fertility desires and intentions among a sample of urban women living with HIV in the United States. AIDS Behav. 2009 Nov 12; doi: 10.1007/S10461-009-9637-8. [E-pub ahead of print] [DOI] [PubMed] [Google Scholar]
- 16.Sowell RL. Murdaugh CL. Addy CL. Moneyham L. Tavokoli A. Factors influencing intent to get pregnant in HIV-infected women living in the southern USA. AIDS Care. 2002;14:181–191. doi: 10.1080/09540120220104695. [DOI] [PubMed] [Google Scholar]
- 17.Stanwood NL. Cohn SE. Heiser JR. Pugliese M. Contraception and fertility plans in a cohort of HIV-positive women in care. Contraception. 2007;75:294–298. doi: 10.1016/j.contraception.2006.12.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Craft SM. Delaney RO. Bautista DT. Serovich JM. Pregnancy decisions among women with HIV. AIDS Behav. 2007;11:927–935. doi: 10.1007/s10461-007-9219-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Richter DL. Sowell RL. Pluto DM. Factors affecting reproductive decisions of African American women living with HIV. Women Health. 2002;36:81–96. doi: 10.1300/J013v36n01_06. [DOI] [PubMed] [Google Scholar]
- 20.Kirshenbaum SB. Hirky AE. Correale J, et al. “Throwing the dice”: Pregnancy decision-making among HIV-positive women in four U.S. cities. Perspect Sex Reprod Health. 2004;36:106–113. doi: 10.1363/psrh.36.106.04. [DOI] [PubMed] [Google Scholar]
- 21.AIDS Alert. Full viral suppression newest trend seen in the “post-HAART” era. 2008. www.geneticimmunity.com/doc/042130-Dermavir-AIDSAlert.pdf. [Jan 3;2010 ]. www.geneticimmunity.com/doc/042130-Dermavir-AIDSAlert.pdf [PubMed]
- 22.Patel D. Cortina-Borja M. Thorne C. Newell ML. European Collaborative Study. Time to undetectable viral load after highly active antiretroviral therapy initiation among HIV-infected pregnant women. Clin Infect Dis. 2007;15(44):1647–1656. doi: 10.1086/518284. [DOI] [PubMed] [Google Scholar]
- 23.Baroncelli S. Tamburrini E. Ravizza M. Antiretroviral treatment in pregnancy: A six-year perspective on recent trends in prescription patterns, viral load suppression, and pregnancy outcomes. AIDS Patient Care STDs. 2009;23:513–520. doi: 10.1089/apc.2008.0263. [DOI] [PubMed] [Google Scholar]
- 24.Cofrancesco J. Scherzer R. Tien P, et al. Illicit drug use and HIV treatment outcomes in a US cohort. AIDS. 2008;22:357–365. doi: 10.1097/QAD.0b013e3282f3cc21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Flynn P. Rudy B. Lindsey J, et al. Long-term observation of adolescents initiating HAART therapy: Three-year follow-up. AIDS Res Hum Retroviruses. 2007;23:1208–12014. doi: 10.1089/aid.2006.0290. [DOI] [PubMed] [Google Scholar]
- 26.Rutstein R. Gebo K. Flynn P, et al. Immunologic function and virologic suppression among children with perinatally acquired HIV Infection on highly active antiretroviral therapy. Med Care. 2005;43(9 Suppl):III15–22. doi: 10.1097/01.mlr.0000175636.34524.b9. [DOI] [PubMed] [Google Scholar]
- 27.Weintrob A. Grandits G. Agan B, et al. (2009). Virologic response differences between African Americans and European Americans initiating highly active antiretroviral therapy with equal access to care. J Acquire Immune Defic Syndr. 2009;52:574–580. doi: 10.1097/QAI.0b013e3181b98537. [DOI] [PubMed] [Google Scholar]
- 28.Berman L. Berman J. Felder S, et al. Seeking help for sexual function complaints: What gynecologists need to know about the female patient's experience. Fertil Steril. 2003;79:572–576. doi: 10.1016/s0015-0282(02)04695-2. [DOI] [PubMed] [Google Scholar]
- 29.Kingsberg S. Just ask! Talking to patients about sexual function. Sex Reprod Menopause. 2004;2:199–203. [Google Scholar]
- 30.Squires K. Bridge DA. Aberg J. Social stigma of pregnant HIV-infected women in the US [Abstract TUPE0908]; Presented at the XVII International AIDS Conference; Mexico City, Mexico. Aug 3–8;2008 . [Google Scholar]
- 31.Sanders LB. Women's voices: The lived experience of pregnancy and motherhood after diagnosis with HIV. J Assoc Nurses AIDS Care. 2008;19:47–57. doi: 10.1016/j.jana.2007.10.002. [DOI] [PubMed] [Google Scholar]
- 32.Lampe MA. Human immunodeficiency virus-1 and preconception care. Matern Child Health J. 2006;10(5 Suppl):S193–195. doi: 10.1007/s10995-006-0131-x. [DOI] [PMC free article] [PubMed] [Google Scholar]