Abstract
Objective
To examine the roles of lifetime abuse-related injury, posttraumatic stress disorder (PTSD) symptom severity, and depressive symptom severity in mediating the effects of severity of assaultive intimate partner violence (IPV), psychological IPV, and child abuse on chronic pain severity in women survivors of IPV.
Methods
Structural equation modeling of data from a community sample of 309 women survivors of IPV was used to test partial and full theoretical models of the relationships among the variables of interest.
Results
The full model had good fit and accounted for 40.2% of the variance in chronic pain severity. Abuse-related injury, PTSD symptom severity, and depressive symptom severity significantly mediated the relationship between child abuse severity and chronic pain severity, but only abuse-related injury significantly mediated the relationship between assaultive IPV severity and chronic pain severity. Psychological IPV severity was the only abuse variable with significant direct effects on chronic pain severity but had no significant indirect effects.
Conclusions
These findings can inform clinical care of women with chronic pain in all areas of healthcare delivery by reinforcing the importance of assessing for a history of child abuse and IPV. Moreover, they highlight the relevance of routinely assessing for abuse-related injury and PTSD and depressive symptom severity when working with women who report chronic pain.
Introduction
Intimate partner violence (IPV) is a pattern of physical, sexual, or emotional violence by an intimate partner in the context of coercive control.1 Chronic pain has been established as a health consequence of IPV in controlled studies2–4 and in both population-based and clinical samples.5–8 Despite extensive literature demonstrating that child and adult abuse experiences, abuse-related injury, depressive symptoms, and posttraumatic stress disorder (PTSD) influence the severity of chronic pain separately,9–13 how these factors together influence chronic pain severity in abused women has seldom been studied.
Chronic pain in abused women stems in part from a complex biopsychosocial stress response to abuse-related physical or psychosocial trauma in childhood and adulthood.14,15 Trauma is defined as extreme stress associated with such events as military combat, physical and sexual assault, or natural disasters.16 Chronic pain may result from neuropathic changes associated with abuse-related injuries17 and endocrine and immune system changes associated with psychological responses to trauma, such as PTSD.12,18 PTSD has been identified as a mediator of the relationship between trauma and physical health outcomes.18 In a recent review of studies of immune function in PTSD, an excess of inflammatory immune activity similar to that associated with chronic pain was identified.19 Intensity, distress, and disability are greater in persons with chronic pain who also have PTSD.20 According to a meta-analysis, the mean prevalence of PTSD in women with a history of IPV is 63.8%.21 There is empirical support that PTSD mediates the relationships both between IPV and proinflammatory cytokines12 and between violence and physical health symptoms, particularly chronic pain.9
Development of posttrauma PTSD symptoms may be linked to changes in the neuroendocrine and immune systems that took place in response to trauma early in life, such as child abuse.22 Among women who had experienced both child and adult physical or sexual abuse, Kimmerling et al.23 found that the risk of experiencing PTSD was more than double that of women who had experienced only child or adult victimization. In an earlier analysis, we found that PTSD symptom severity and lifetime abuse-related injury were each significant mediators of the relationships between both assaultive IPV and child abuse severity and chronic pain severity in women survivors of IPV.24
Depressive symptoms may also be an important link between lifetime trauma and physical health outcomes.25 In meta-analyses, depression has been estimated to affect as many as 47.6% of abused women21 and to be moderately associated with physical partner assault.26 Depression is also associated with child abuse.27 Exposure to both child abuse and IPV increases the risk of depressive symptoms.28 The comorbidity of depression with PTSD29 and chronic pain30 has been established. Approximately 50% of women with histories of IPV were found to have comorbid PTSD and depression.31,32 In a longitudinal study following women who left shelters, physical health outcomes (including pain) of recent IPV were mediated by depression and anxiety but not by abuse-related injury.33 Yet in a community sample of women, half of whom had experienced partner abuse in the previous 6 months, recent injury, stress, and depression all had significant mediating effects on health outcomes of abuse, with those of injury being smaller.34 After exposure to trauma, young adults who developed PTSD were more likely than those who did not to develop major depression, suggesting that the depressive effects of traumatic events are not independent of PTSD-inducing effects.35 In women who had been sexually assaulted, symptoms of depression and PTSD each accounted for unique variance in self-reported health symptoms (including pain), whereas assault-related injury did not.36 In a community sample of abused women who had been out of the relationship at least 1 year, depressive symptoms, current employment status, and length of time in an abusive relationship predicted moderate to severe chronic pain, whereas PTSD, abuse-related injury, and threats of physical violence in the last year in the relationship did not.37
In spite of such research, no studies have explored how depression, PTSD, and abuse-related injury together might mediate the relationships between past child and adult abuse and chronic pain in women. Building on our previous analysis of the mediating effects of abuse-related injury and PTSD symptoms,24 we tested a theoretical model (Fig. 1) to examine the roles of lifetime abuse-related injury, PTSD symptom severity, and depressive symptom severity in mediating the effects of assaultive IPV severity, psychological IPV severity, and child abuse severity on chronic pain severity in women survivors of IPV.
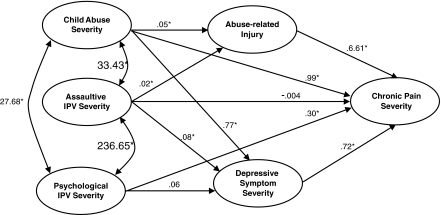
FIG. 1.
Partial model with nonstandardized coefficients. IPV, intimate partner violence. *p < 0.05.
Materials and Methods
A community sample of 309 adult, English-speaking women from three Canadian provinces who met the inclusion criteria of having (1) left an abusive partner (index partner) at least 3 months but no more than 3 years previously and (2) screened positive on the modified Abuse Assessment Screen38 was recruited primarily through community advertising using posters and newspapers, after ethical approval from relevant Research Ethics Boards. Between June 2004 and January 2006, baseline data for an ongoing longitudinal study of patterns of women's health in the early years after leaving an abusive male partner were collected using standardized self-report measures, biophysical tests, and survey questions in two sessions in a private location of the participant's choice.39 After receiving informed consent, interviewers collected data about women's resources, service use, and demographic characteristics; approximately 2 weeks later, a Registered Nurse collected an abuse history and conducted a health assessment. Data were recorded using computer-assisted data entry. Women received a participation fee of $30 and reimbursement for child care and transportation costs. A rigorous safety protocol was followed in all interactions to protect both participants and data collectors. Using this baseline data, we tested the proposed theoretical model using structural equation modelling (SEM).
Measures
Child abuse severity was measured with the emotional, physical, and sexual abuse scales from the Childhood Trauma Questionnaire (CTQ).40 For each of the five items on each scale, participants were asked to rate the frequency of a particular childhood event on a 5-point Likert scale (1 = never true, 3 = sometimes, 5 = very often true). Scores for each scale were calculated by summing the corresponding item scores (range 5–25), with higher scores indicating a greater severity of maltreatment. This scale has established reliability and validity among adolescent psychiatric inpatients and women exposed to IPV.2,41 In this study, Cronbach's alpha reliability coefficient was 0.90 for emotional abuse, 0.89 for physical abuse, and 0.96 for sexual abuse.
Assaultive IPV severity from the index partner was measured using the Physical Abuse total score of the Index of Spouse Abuse (ISA) scale.42 Participants were asked to rate the frequency of specific abusive acts directed toward them by their ex-partners on a scale of 0 (never) to 4 (very frequently) on 11 items related to physical and sexual abuse. Individual items were weighted for severity and summed for a possible range of 0–100. Reliability and validity for the ISA are well established.43 Internal consistency of the Physical Abuse items in this study was 0.84. Psychological IPV severity was measured using the Non-physical Abuse total score of the ISA that consists of 19 items related to nonphysical abuse. Internal consistency of the Non-physical Abuse items of the ISA in this study was 0.83.
Lifetime abuse-related injury was measured using self-report of lifetime frequency of abuse-related injuries that resulted in (1) hospitalization, (2) a visit to the emergency room, (3) broken bones, or (4) head injury with loss of consciousness.24 Because of skewed distributions, scores were recoded on a scale of 1–4, where 1 reflects no injury and 2, 3, and 4 reflect increasing frequency of injury.
PTSD symptom severity was measured by the total scores for each of three symptom subscales (hypervigilance, intrusion, avoidance/numbing) on the Davidson Trauma Scale (DTS).44.45 Women who reported having experienced a traumatic event were asked to rate the symptoms of PTSD experienced in the past week on 4-point scales for frequency (not at all to every day) and severity (not at all distressing to extremely distressing). Total subscale scores were calculated by summing the frequency and severity responses to applicable items. Scores ranged from 0 to 56 for avoidance/numbing and 0 to 40 for both intrusion and hypervigilance. The DTS has been shown to have validity, good internal consistency, and test-retest reliability in a variety of trauma populations,46 and the subscales have good internal consistency.47 In this study, Cronbach's alpha was 0.90 for intrusion, 0.91 for avoidance, and 0.89 for hyperarousal.
The 20-item Center for Epidemiologic Studies-Depression (CES-D) scale was used to measure depressive symptom severity.48 The CES-D has established reliability and validity with general populations and with abused women.48,49 Women were asked to rate symptom frequency in the past week on a 4-point scale from rarely to most of the time. Summed total scores range from 0 to 60, with higher scores reflecting more symptoms of depression. In this study, the Cronbach's alpha was 0.93.
The total scores of the Pain Intensity and Pain Disability scales along with the number of disability days in the past 6 months from the Chronic Pain Grade (CPG) scale were used to measure chronic pain severity.50 Participants rated their current pain intensity as well as worst pain intensity and average pain intensity in the past 6 months using three separate scales from 0 (no pain) to 10 (pain as bad as it could be). The Pain Intensity score (0–100) was derived by multiplying the mean of the three intensity items by 10. Pain Disability in the past 6 months was similarly calculated from three items (0–10) measuring pain-related interference with daily activities; change in ability to take part in recreational, social, and family activities; and change in ability to work, including housework. Disability days were determined by a single question asking how many days had been lost from usual activities (work, school, or housework) because of the pain in the past 6 months. Reliability and validity of the CPG scale have been confirmed in both community and clinical samples of adults.51–53 In this study, internal consistency of the Pain Intensity and Pain Disability scores were 0.84 and 0.93, respectively.
Analysis
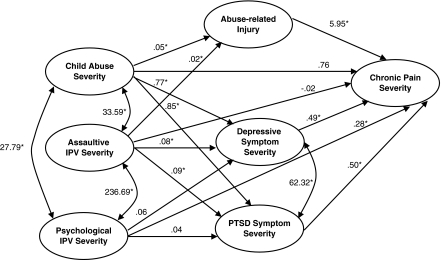
In SEM, the structural model is based on predetermined theoretical relationships and includes observed variables and latent variables, which are inferred constructs from the selected observed variables.54 SEM estimates the relationships between the observed variables and the latent variables and, at the same time, the direct and indirect effects among the latent variables. Because SEM incorporates measurement error, estimates of relationships between latent variables are more accurate than those achieved through other techniques. In order to have a clear understanding of the effects of the three mediating variables (PTSD symptom severity, depressive symptom severity, and lifetime abuse-related injury) in our theoretical model, we built on our previous test of PTSD symptom severity and lifetime abuse-related injury as mediators of the relationships between abuse severity and chronic pain severity using the current dataset.24 In the current analysis, we first tested a partial theoretical model with only depressive symptom severity and lifetime abuse-related injury as mediators (Fig. 1). Then, we tested our full model with PTSD symptom severity, depressive symptom severity, and lifetime abuse-related injury as mediators (Fig. 2). In both models, child abuse severity, assaultive IPV severity, and psychological IPV severity were allowed to intercorrelate freely. In the full model, PTSD symptom severity and depressive symptom severity were also allowed to intercorrelate freely. In both models, we controlled for age by including self-reported age as a manifest variable; the association between age and chronic pain severity is well documented.55 The significance level for all analyses was p < 0.05.
FIG. 2.
Full theoretical model with nonstandardized coefficients. *p < 0.05. PTSD, posttraumatic stress disorder.
Descriptive statistics of the observed variables showed no violations of the normal distribution assumptions and no outliers. Multicollinearity was not suggested by bivariate correlations among observed variables (Table 1). The maximum likelihood (ML) estimation technique using Mplus© was used for data analysis. Similarities between bootstrapped estimates of the standard errors and those obtained by the ML model indicated that assumptions of normal distribution were met by the ML model. A metric from one of the indicators (the reference indicator) was assigned to each of the latent variables. Missing data were handled by first estimating the proposed model using a listwise deletion method and then reestimating using a full-information, maximum-likelihood (FIML) technique. These two estimation approaches yielded almost identical estimates in both magnitude of effects and level of significance; therefore, in order to use the full sample, the results of the FIML are reported.
Table 1.
Pearson's Correlations Among Measured Variables
| 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | 13. | 14. | 15. | 16. | 17. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. CTQ_Emotional | 1.00 | ||||||||||||||||
| 2. CTQ_Physical | 0.65 | 1.00 | |||||||||||||||
| 3. CTQ_Sexual | 0.48 | 0.44 | 1.00 | ||||||||||||||
| 4. ISA_Physical | 0.23 | 0.17 | 0.19 | 1.00 | |||||||||||||
| 5. ISA_NonPhysical | 0.25 | 0.20 | 0.20 | 0.57 | 1.00 | ||||||||||||
| 6. Hospitalized | 0.26 | 0.28 | 0.31 | 0.27 | 0.08 | 1.00 | |||||||||||
| 7. Emergency | 0.33 | 0.30 | 0.32 | 0.43 | 0.18 | 0.64 | 1.00 | ||||||||||
| 8. Broken Bones | 0.14 | 0.18 | 0.11 | 0.37 | 0.16 | 0.54 | 0.59 | 1.00 | |||||||||
| 9. Head Injury | 0.17 | 0.22 | 0.23 | 0.39 | 0.17 | 0.51 | 0.57 | 0.56 | 1.00 | ||||||||
| 10. DTS_Avoidance | 0.34 | 0.25 | 0.22 | 0.24 | 0.20 | 0.19 | 0.26 | 0.18 | 0.16 | 1.00 | |||||||
| 11. DTS_Hyperarousal | 0.32 | 0.24 | 0.21 | 0.27 | 0.24 | 0.12 | 0.26 | 0.18 | 0.10 | 0.75 | 1.00 | ||||||
| 12. DTS_Intrusion | 0.36 | 0.29 | 0.18 | 0.28 | 0.22 | 0.22 | 0.28 | 0.11 | 0.19 | 0.64 | 0.60 | 1.00 | |||||
| 13. CES-D | 0.35 | 0.26 | 0.20 | 0.27 | 0.25 | 0.12 | 0.19 | 0.14 | 0.11 | 0.51 | 0.56 | 0.39 | 1.00 | ||||
| 14. CPG_Pain Disability | 0.36 | 0.30 | 0.21 | 0.26 | 0.30 | 0.20 | 0.31 | 0.23 | 0.15 | 0.34 | 0.36 | 0.38 | 0.43 | 1.00 | |||
| 15. CPG_Pain Intensity | 0.30 | 0.30 | 0.23 | 0.32 | 0.31 | 0.22 | 0.29 | 0.22 | 0.23 | 0.35 | 0.38 | 0.38 | 0.40 | 0.71 | 1.00 | ||
| 16. CPG_Days Lost | 0.21 | 0.13 | 0.06 | 0.15 | 0.19 | 0.17 | 0.21 | 0.13 | 0.08 | 0.27 | 0.30 | 0.37 | 0.25 | 0.60 | 0.49 | 1.00 | |
| 17. Age | 0.02 | 0.02 | 0.03 | −0.20 | −0.14 | −0.03 | −0.06 | 0.00 | −0.10 | −0.031 | −0.02 | 0.064 | −0.02 | 0.07 | −0.01 | 0.13 | 1.00 |
CES-D, Center for Epidemiologic Studies–Depression; CPG, Chronic Pain Grade; CTQ, Childhood Trauma Questionnaire; DTS, Davidson Trauma Scale; ISA, Index of Spouse Abuse.
Results
The 309 women ranged in age from 19 to 63 years (mean = 39.4, standard deviation [SD] = 9.8), had 6–22 years of education (mean = 13.4, SD = 2.6), and had been living separately from their abusive partners for 3–40 months (mean = 20, SD = 10.2). More than half (57%) had dependent children. Annual incomes in Canadian dollars ranged from 0 to $95,000 (mean = $20,391, SD = $17,145). Of the 309 women, 45.1% were employed, 31.4% were on social assistance, and 10.4% received a disability pension. The majority of the participants were Caucasian, with only 16.8% of women self-identifying as belonging to a visible minority and 7.4% as Aboriginal.
The correlation matrix for relationships among the observed variables is reported in Table 1. Descriptive statistics for each observed variable and factor loadings for latent variables for both the partial model and the full model are reported in Table 2. For all observed variables, factor loadings were statistically significant and of ample magnitudes (0.59–0.91). For both the partial and full hypothesized models, the goodness of fit indices met the criteria for indicating a good fit between the data and the model, except for the chi-square statistic, which was significant (Table 3).54 There were no significant modification indices; thus, the models were retained. To permit comparisons across models, the nonstandardized coefficients (B) are included in Figure 1 for the full model and in Figure 2 for the partial model. To permit comparisons within the models, the standardized coefficients (β) for both models are reported in Table 4.
Table 2.
Latent Variables, Observed Variables, Descriptive Statistics, and Factor Loadings (n = 309)
| |
|
|
Descriptive statistics |
Factor loadings |
|
|---|---|---|---|---|---|
| Latent variables | Observed variables | n | Mean (SD), range | Partial model | Full model |
| Child abuse severity | CTQ Emotional total score | 304 | 14.80 (6.31), 5–25 | 0.85 | 0.85 |
| CTQ Physical total score | 304 | 10.05 (5.73), 5–25 | 0.76 | 0.76 | |
| CTQ Sexual | 304 | 11.88 (7.20), 5–25 | 0.58 | 0.58 | |
| Assaultive IPV severity | ISA Physical total score | 303 | 48.58 (23.47), 7.18–100 | 1.00 | 1.00 |
| Psychological Abuse severity | ISA Non-Physical total score | 290 | 65.3 (18.63), 18.54–100 | 1.00 | 1.00 |
| Lifetime Abuse-Related Injury | Hospitalized total score | 306 | 0.54 (1.14), 0–4 | 0.74 | 0.74 |
| Emergency Room Visits total score | 306 | 1.08 (1.43), 0–4 | 0.84 | 0.84 | |
| Broken Bones total score | 304 | 0.43 (1.02), 0–4 | 0.73 | 0.73 | |
| Head Injury total score | 304 | 0.64 (1.21), 0–4 | 0.70 | 0.70 | |
| PTSD symptom severity | DTS Avoidance total score | 285 | 17.71 (13.83), 0–56 | 0.87 | |
| DTS Hyperarousal total score | 286 | 16.94 (10.85), 0–40 | 0.86 | ||
| DTS Intrusion total score | 285 | 13.07 (10.07), 0–40 | 0.72 | ||
| Depressive symptom severity | CES-D total score | 309 | 25.23 (13.03), 0–54.74 | 1.00 | 1.00 |
| Chronic Pain severity | CPG Pain Disability total score | 303 | 37.28 (32.11), 0–100 | 0.91 | 0.90 |
| CPG Pain Intensity total score | 303 | 49.01 (25.84), 0–100 | 0.78 | 0.79 | |
| CPG days lost from usual activities due to pain past 6 months | 292 | 23.92 (44.66), 0–180 | 0.64 | 0.65 | |
Table 3.
Goodness of Fit Indices
| Critical value | Partial model | Full model | |
|---|---|---|---|
| Comparative fit index | ≥0.90 | 0.97 | 0.97 |
| Root mean square of approximation | <0.05 | 0.047 | 0.048 |
| Tucker-Lewis index | ≥0.95 | 0.96 | 0.95 |
| Chi-square test of model fit | p ≥ 0.05 | 103.56 (df = 62), p = 0.0007 | 167.87 (df = 98), p < 0.001 |
Table 4.
Standardized Coefficients for Partial and Full Tested Model
| |
Causal effects partial model |
Causal effects full model |
||||
|---|---|---|---|---|---|---|
| Outcome and determinants | Direct | Indirect | Total | Direct | Indirect | Total |
| PTSD symptom severity | (R2 = 0.238) | |||||
| Child Abuse severity | 0.38* | |||||
| Psychological IPV severity | 0.06 | |||||
| Assaultive IPV severity | 0.18* | |||||
| Depression symptom severity | (R2 = 0.179) | (R2 = 0.179) | ||||
| Child Abuse severity | 0.32* | 0.32* | ||||
| Psychological IPV severity | 0.09 | 0.09 | ||||
| Assaultive IPV severity | 0.14* | 0.14* | ||||
| Abuse-related injury | (R2 = 0.321) | (R2 = 0.324) | ||||
| Child Abuse severity | 0.30* | 0.31* | ||||
| Assaultive IPV severity | 0.41* | 0.41* | ||||
| Chronic pain severity | (R2 = 0.377) | (R2 = 0.402) | ||||
| PTSD Symptom severity | 0.21* | |||||
| Depression Symptom severity | 0.32* | 0.22* | ||||
| Abuse-related injury | 0.19* | 0.17* | ||||
| Child Abuse severity | 0.18* | 0.34* | 0.14 | 0.08* (PTSD) | 0.34* | |
| 0.06* (Injury) | 0.05* (Injury) | |||||
| 0.10* (Depression) | 0.07* (Depression) | |||||
| Psychological IPV severity | 0.19* | 0.22* | 0.18* | 0.01 (PTSD) | 0.21* | |
| 0.03 (Depression) | 0.02 (Depression) | |||||
| Assaultive IPV severity | −0.003 | 0.12 | −0.02 | 0.04 (PTSD) | 0.12 | |
| 0.08* (Injury) | 0.07* (Injury) | |||||
| 0.05* (Depression) | 0.03 (Depression) | |||||
Significance level p < 0.05.
Partial model
The partial model, in which depressive symptom severity and lifetime abuse-related injury were tested as mediators of the relationship between abuse severity and chronic pain severity, accounted for 37.7 % of variance in chronic pain severity. Child abuse severity, assaultive IPV severity, and psychological IPV severity together accounted for 17.9% of variance in depressive symptom severity and 32.1% of variance in lifetime abuse-related injury. The correlation of child abuse severity with psychological IPV severity was r = 0.28 (p < 0.001), and with assaultive IPV severity was r = 0.27 (p < 0.001). The correlation between psychological IPV severity and assaultive IPV severity was r = 0.56 (p < 0.001). Depressive symptom severity was a significant mediator of the effects of both child abuse severity (β = 0.10) and assaultive IPV (β = 0.05) on chronic pain severity. Similarly, lifetime abuse-related injury was a significant mediator of the effects of both child abuse severity (β = 0.06) and assaultive IPV (β = 0.08) on chronic pain severity. Depressive symptom severity (β = 0.03) was not a significant mediator of the effect of psychological IPV severity in the partial model. Among the past abuse severity variables, psychological IPV severity (β = 0.19) had the largest significant direct effect on chronic pain severity, followed by child abuse severity (β = 0.18); the direct effect of assaultive IPV severity (β = −0.003) on chronic pain severity was not significant. The significant direct effect of depressive symptom severity on chronic pain severity (β = 0.32) was one and half times the magnitude of that of lifetime abuse-related injury (β = 0.19) when abuse severity was controlled.
Full model
The full model, which included lifetime abuse-related injury, depressive symptom severity, and PTSD symptom severity as mediators of abuse severity, accounted for 23.8% of the variance in PTSD symptom severity, and 40.2% of the variance in chronic pain severity. The percent of variance accounted for in lifetime abuse-related injury and depressive symptom severity and the correlations between the abuse severity variables were the same as those reported for the partial model. The correlation between PTSD symptom severity and depressive symptom severity was r = 0.51 (p < 0.001).
PTSD symptom severity was a significant mediator only of the effect of child abuse severity (β = 0.08) on chronic pain severity. Similarly, depressive symptom severity (β = 0.07) had a significant mediating effect only on the relationship between child abuse severity and chronic pain severity. However, abuse-related injury was a significant mediator for the relationships of both child abuse severity (β = 0.05) and assaultive IPV severity (β = 0.07) with chronic pain severity. The significant direct effects of the PTSD symptom severity (β = 0.21) and depressive symptom severity (β = 0.22) on chronic pain severity were of almost equal magnitude, whereas those of lifetime abuse-related injury (β = 0.17) were slightly less. Among the past abuse severity variables, psychological IPV severity had the only significant direct effect on chronic pain severity (β = 0.18).
Comparisons between full and partial models
In comparison to the partial model, the addition of PTSD as a mediating variable in the full model reduced the significant direct effects of depressive symptom severity from B = 0.72 to B = 0.49 and of lifetime abuse-related injury from B = 6.61 to B = 5.95 (Figs. 1 and 2). Additionally, the significant mediating effect of assaultive IPV severity on chronic pain severity through depressive symptom severity (B = 0.06) in the partial model became insignificant in the full model (B = 0.04). With respect to child abuse severity, the significant mediating effect through depressive symptom severity was reduced from B = 0.56 in the partial model to B = 0.38 in the full model. The magnitudes of the significant mediating effects through lifetime abuse-related injury were similar in both the partial and full models for both child abuse severity (B = 0.32 vs. B = 0.29) and assaultive IPV severity (B = 0.10 vs. B = 0.09). The direct effect of child abuse severity on chronic pain severity was significant in the partial model (B = 0.99, p = 0.011) but insignificant in the full model (B = 0.76, p = 0.053). The magnitude of the significant direct effect of psychological IPV severity was similar in both models.
Discussion
Understanding the relationships among chronic pain, abuse, depression, and PTSD has important implications not only for women with known IPV but also for women with chronic pain, depression, or PTSD whether they are seen in a primary care, emergency, or mental health setting. Assessment for lifetime abuse, particularly IPV and child abuse, is essential. Specifically, clinicians must base practice on an understanding of the relationships among the forms and severity of abuse and chronic pain. In this study, only psychological abuse severity, not assaultive IPV severity, had significant direct effects on chronic pain severity, a finding that supports earlier epidemiological findings of increased odds for chronic pain among women who had experienced psychological abuse3 and challenges the emphasis on physical injury that often dominates clinical understanding of IPV. Our findings are particularly noteworthy given that we considered the mediating effects of mental health and injury in our analytic model. They highlight the importance of clinicians recognizing that women who have experienced coercion, control, and intimidation from their partners, even if there is no physical assault, may be at risk for chronic pain and of inquiring routinely about all forms of abuse.
Our findings also draw attention to the importance of timely and effective assessment and management of abuse-related injury in children and adults to prevent long-term chronic pain. In our analysis, both child abuse severity and assaultive IPV severity were found to affect chronic pain severity indirectly through lifetime abuse-related injury, with the significant direct effects of child abuse severity on lifetime abuse-related injury being only a little less than those of assaultive IPV. Injuries sustained in childhood abuse as well adulthood may lead to neuropathic changes in pain pathways associated with chronic pain if the pain is not managed well56; hence, the sequelae of childhood injuries may persist into adulthood. Our finding that the significant direct effect of child abuse severity on chronic pain severity became insignificant in the full model may be related to sample size, and further research is required to explore this relationship. In the Adverse Childhood Events (ACE) study, Felitti et al.57 found profound lasting effects of child abuse on adult health but did not explore the pathways by which these effects are produced, such as through abuse-related injury, PTSD, or depression.
Our findings suggest that assessment and treatment of PTSD and of clinical depression are important in the treatment of chronic pain in women with abuse histories. Additionally, assessment and treatment of chronic pain may be important in the management of depression and PTSD. Current PTSD symptom severity and depression symptom severity were found to be significant mediators of the effects of child abuse severity on chronic pain severity but not of the effects of either assaultive or psychological abuse in the full model. Interestingly, the significant direct effects of child abuse severity on both PTSD symptom severity and depressive symptom severity were about twice the magnitude of those of assaultive IPV severity on these variables. These findings support the argument that an increased inflammatory response in PTSD and in depressive disorders following IPV or other adult traumas may be associated with neuroendocrine changes in response to previous trauma, particularly early in life (such as child abuse).58–63 Whether these changes are associated with exposure to early trauma or to having developed PTSD in response to that earlier trauma requires further research.64 Contrary to findings of other studies that did not consider child abuse severity,65 psychological IPV severity had no significant direct effects on either PTSD or depressive symptom severity. Together, these findings draw attention to the imperatives of including child abuse history in research focusing on the health effects of IPV and of early assessment and intervention in child abuse, aimed toward mitigation of immediate health effects and long-term biophysical changes.
Assessment of lifetime abuse experiences is clearly important. Our work extends the findings of Sutherland et al.34 that injury, stress, and depression are significant mediators of the health outcomes of partner abuse by adding both child abuse severity and PTSD symptom severity to the analysis. Our findings that abuse-related injury, PTSD symptom severity, and depressive symptom severity all mediated the effects of child abuse severity on chronic pain severity but that only abuse-related injury mediated the effects of assaultive IPV on chronic pain severity demonstrate the importance of attending to lifetime abuse in theoretical and clinical studies of the physical health effects of abuse and in clinical practice.
Our findings also suggest that comorbid depressive and PTSD symptoms, as opposed to one or the other, may account for greater chronic pain severity in abused women with histories of child abuse. This finding has important implications for attending to both mental health concerns in women with chronic pain and abuse histories. In our sample, 44.5% of woman abuse survivors had comorbid symptoms consistent with clinical depression and PTSD, 28.2% had symptoms consistent with clinical depression, 23.1% lacked symptoms consistent with either clinical depression or PTSD, and 4.2% had only symptoms consistent with PTSD. Importantly, our findings suggest that although depressive symptom severity and PTSD symptom severity are not conceptually distinct, each accounts for unique variance in chronic pain severity. In our partial model, lifetime abuse-related injury and depressive symptom severity accounted for 37.7% of the variance in chronic pain severity, a similar value to the 37.8% accounted for in our previous analysis of the mediating effects of lifetime abuse-related injury and PTSD symptom severity on chronic pain severity.24 The full model accounted for 40.2% of variance, and the magnitude of the direct effect of depressive symptom severity decreased to a value equivalent to that of PTSD symptom severity. In contrast, Humphreys et al.37 found that only depression, not PTSD, predicted moderate to severe chronic pain in formerly abused women, although child abuse was not included in their logistic regression model. Current understandings of the mechanisms by which abuse affects chronic pain appear to be related, at least in part, by which variables are included in particular studies.
In our sample, 48.7% and 72.8% were above the cutoff scores for PTSD and depression measures, respectively. Interestingly, when asked about diagnoses by health professionals, only 7% of women in our sample reported a diagnosis of PTSD, 31% a diagnosis of depression,66 and 3.6% had both diagnoses. This suggests that, at least in our sample, the comorbidity of PTSD and depression is not being identified by clinicians. This may be related to clinicians not inquiring about past trauma once they have diagnosed depression or women's lack of comfort in reporting abuse experiences. Gill et al.67 observed that if traumatized women who seek help for chronic physical health problems are not assessed and treated for their underlying response to trauma, their physical symptoms are likely to continue. Health problems have been found to be a major interference for women struggling to provide for their families and create new lives after leaving abusive partners.68 Thus, effective treatment of chronic pain and associated mental health problems is critical to helping women move forward.
The analyses have several limitations. Measures of IPV were completed only for the partner from whom the woman had most recently separated and did not take into account lifetime experiences of IPV. Recall bias may be an issue, particularly with respect to questions about child abuse, lifetime abuse-related injury, and chronic pain in the past 6 months. Recall limitations are difficult to overcome with respect to child abuse, as studies based on reported child abuse do not account for experiences of abuse that are not reported formally.69 Our measure of chronic pain was chosen to take into account pain intensity and disability over the previous 6 months because a measure of current pain, although perhaps more accurate, would be unlikely to capture the pattern of pain over time. Another limitation is our reliance on self-report screening measures of both PTSD symptoms and depressive symptoms as opposed to a clinical diagnostic assessment. Further, the DTS does not measure duration of PTSD, which may be a factor in the development of chronic pain. Finally, data were collected concurrently, and the assumption of temporal ordering of variables necessary to determine causation was met for only some variables. Subsequent testing of the model with longitudinal data will provide more definitive support for causation between the latent variables.
Our findings add to the dialogue about the potential long-term impact of abuse survivors' mental health on their physical health while also taking into account the effects of abuse-related injury. Further research is needed to more fully understand the unique effects, as well as the interrelated direct and indirect effects, of depressive and PTSD symptoms on chronic pain in abuse survivors within in the context of cumulative abuse history.
Acknowledgments
This research was funded by the Canadian Institutes of Health Research, New Emerging Team grant 106054 and Institute of Gender and Health Operating grant 15156. We thank the women who took part in the Women's Health Effects Study.
Disclosure Statement
The authors have no conflicts of interest to report.
References
- 1.Tjaden P. Thoennes N. Extent, nature and consequences of intimate partner violence: Findings from the National Violence Against Women Survey. National Institute of Justice and the Centers for Disease Control and Prevention; 2000. [Google Scholar]
- 2.Campbell J. Jones A. Dienemann J, et al. Intimate partner violence and physical health consequences. Arch Intern Med. 2002;162:1157–1163. doi: 10.1001/archinte.162.10.1157. [DOI] [PubMed] [Google Scholar]
- 3.Coker A. Smith P. Bethea L. King M. McKeown R. Physical health consequences of physical and psychological intimate partner violence. Arch Fam Med. 2000;9:451–457. doi: 10.1001/archfami.9.5.451. [DOI] [PubMed] [Google Scholar]
- 4.Kramer A. Lorenzon D. Mueller G. Prevalence of intimate partner violence and health implications for women using emergency departments and primary care clinics. Womens Health Issues. 2004;14:19–29. doi: 10.1016/j.whi.2003.12.002. [DOI] [PubMed] [Google Scholar]
- 5.Jamieson D. Steege J. The association of sexual abuse with pelvic pain complaints in a primary care population. Am J Obstet Gynecol. 1997;177:1408–1412. doi: 10.1016/s0002-9378(97)70083-8. [DOI] [PubMed] [Google Scholar]
- 6.Leserman J. Drossman D. Relationship of abuse history to functional gastrointestinal disorders and symptoms: Some possible mediating factors. Trauma Violence Abuse. 2007;8:331–343. doi: 10.1177/1524838007303240. [DOI] [PubMed] [Google Scholar]
- 7.Leserman J. Drossman D. Zhiming L. Toomey T. Nachman G. Glogan L. Sexual and physical abuse history in gastroenterology practice. Psychosom Med. 1996;58:4–15. doi: 10.1097/00006842-199601000-00002. [DOI] [PubMed] [Google Scholar]
- 8.Walling M. Reiter R. O'Hara M. Milburn A. Lilly G. Vincent S. Abuse history and chronic pain in women: I. Prevalences of sexual and physical abuse. Obstet Gynecol. 1994;84:193–199. [PubMed] [Google Scholar]
- 9.Campbell R. Greeson M. Bybee D. Raja S. The co-occurrence of childhood sexual assault, adult sexual assault, intimate partner violence, and sexual harassment: A mediation model of posttraumatic stress disorder and physical health outcomes. J Consult Clin Psychol. 2008;76:194–207. doi: 10.1037/0022-006X.76.2.194. [DOI] [PubMed] [Google Scholar]
- 10.Coker A. Smith P. Fadden MP. Intimate partner violence and disabilities. J Womens Health. 2005;14:829–838. doi: 10.1089/jwh.2005.14.829. [DOI] [PubMed] [Google Scholar]
- 11.Walsh C. Jamieson E. MacMillan H. Boyle M. Child abuse and chronic pain in a community survey of women. J Interpers Violence. 2007;22:1536–1554. doi: 10.1177/0886260507306484. [DOI] [PubMed] [Google Scholar]
- 12.Woods A. Page G. O'Campo P. Pugh L. Ford D. Campbell J. The mediation effect of posttraumatic stress disorder symptoms on the relationship of intimate partner violence and IFN-γ levels. Am J Community Psychol. 2005;36:159–175. doi: 10.1007/s10464-005-6240-7. [DOI] [PubMed] [Google Scholar]
- 13.Wuest J. Merritt-Gray M. Ford-Gilboe M. Lent B. Varcoe C. Campbell JC. Chronic pain in women survivors of intimate partner violence. J Pain. 2008;9:1049–1057. doi: 10.1016/j.jpain.2008.06.009. [DOI] [PubMed] [Google Scholar]
- 14.Chapman CR. Tuckett R. Song CW. Pain and stress in a systems perspective: Reciprocal neural, endocrine and immune interactions. J Pain. 2008;9:122–145. doi: 10.1016/j.jpain.2007.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Meagher MW. Links between traumatic family violence and chronic pain: Biopsychosocial pathways and treatment implications. In: Kendall-Tackett KA, editor. Health consequences of abuse in the Family. Washington, DC: APA; 2005. pp. 155–177. [Google Scholar]
- 16.Schnurr P. Green B. Understanding relationships among trauma, posttraumatic stress disorder, and health outcomes. In: Schnurr P, editor; Green B, editor. Trauma and health: Physical health consequences of exposure to extreme stress. Washington, DC: APA; 2004. pp. 247–275. [Google Scholar]
- 17.Martelli M. Zaster N. Bender M. Nicholson K. Psychological, neuropsychological, and medical considerations in the assessment and management of pain. J Head Trauma Rehabil. 2004;19:10–28. doi: 10.1097/00001199-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Green B. Kimmerling R. Trauma, posttraumatic stress disorder and health status. In: Schnurr P, editor; Green B, editor. Trauma and health: Physical consequences of exposure to extreme stress. Washington, DC: APA; 2004. pp. 13–37. [Google Scholar]
- 19.Gill J. Saligan L. Wood S. Page G. PTSD associated with an excess of inflammatory immune activities. Perspect Psychiatr Care. 2009;45:262–277. doi: 10.1111/j.1744-6163.2009.00229.x. [DOI] [PubMed] [Google Scholar]
- 20.Otis J. Keane T. Kerns R. An examination of the relationship between chronic pain and posttraumatic stress disorder. J Rehabil Res Dev. 2003;40:397–406. doi: 10.1682/jrrd.2003.09.0397. [DOI] [PubMed] [Google Scholar]
- 21.Golding J. Intimate partner violence as a risk factor for mental disorders: A meta-analysis. J Fam Violence. 1999;14:99–132. [Google Scholar]
- 22.Dallem SJ. Health issues associated with violence against women. In: Kendall-Tackett K, editor. Handbook of women, stress, and trauma. New York: Brunner-Routledge; 2005. pp. 159–180. [Google Scholar]
- 23.Kimmerling R. Alvarez J. Pavao J. Kaminski A. Baumrind N. Epidemiology and consequences of women's revictimization. Women Health Issues. 2007;17:101–106. doi: 10.1016/j.whi.2006.12.002. [DOI] [PubMed] [Google Scholar]
- 24.Wuest J. Ford-Gilboe M. Merritt-Gray M, et al. Abuse-related injury and symptoms of posttraumatic stress disorder as mechanisms of chronic pain in survivors of intimate partner violence. Pain Med. 2009;10:739–747. doi: 10.1111/j.1526-4637.2009.00624.x. [DOI] [PubMed] [Google Scholar]
- 25.Dennis M. Flood A. Reynolds V, et al. Evaluation of lifetime trauma exposure and physical health in women with posttraumatic stress disorder or major depressive disorder. Violence Women. 2009;15:618–627. doi: 10.1177/1077801209331410. [DOI] [PubMed] [Google Scholar]
- 26.Stith SM. Smith DB. Penn CE. Warda D. Tritt D. Intimate partner physical abuse perpetration and victimization risk factors: A meta-analytic review. Aggress Violent Behav. 2004;10:65–98. [Google Scholar]
- 27.Heim C. Newport DJ. Mletzko T. Miller A. Nemeroff C. The link between childhood trauma and depression: Insights from HPA axis studies in humans. Psychoneuroendocrinology. 2008;33:693–710. doi: 10.1016/j.psyneuen.2008.03.008. [DOI] [PubMed] [Google Scholar]
- 28.Fogarty C. Fredman L. Heeren T. Liebschulz J. Synergistic effects of child abuse and intimate partner violence on depressive symptoms in women. Prev Med. 2008;46:463–469. doi: 10.1016/j.ypmed.2007.12.009. [DOI] [PubMed] [Google Scholar]
- 29.O'Campo P. Kub J. Woods A, et al. Depression, PTSD and co-morbidity related to intimate partner violence in civilian and military women. Brief Treat Crisis Intervent. 2006;6:99–110. [Google Scholar]
- 30.Von Korff M. Simon G. The relationship between pain and depression. Br J Psychiatry. 1996;168:101–108. [PubMed] [Google Scholar]
- 31.Kelly U. Symptoms of PTSD and major depression in Latinas who have experienced intimate partner violence. J Ment Health Nurs. 2010;31:119–127. doi: 10.3109/01612840903312020. [DOI] [PubMed] [Google Scholar]
- 32.Nixon R. Resick P. Nishith P. An exploration of comorbid depression among female victims of intimate partner violence with posttraumatic stress disorder. J Affect Disord. 2004;82:315–320. doi: 10.1016/j.jad.2004.01.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sutherland C. Bybee D. Sullivan C. The long term effects of battering on women's health. Womens Health. 1998;4:41–70. [PubMed] [Google Scholar]
- 34.Sutherland C. Bybee D. Sullivan C. Beyond bruises and broken bones: The joint effects of stress and injuries on battered women's health. Am J Community Psychol. 2002;30:609–636. doi: 10.1023/A:1016317130710. [DOI] [PubMed] [Google Scholar]
- 35.Breslau N. Davis GC. Peterson EL. Schultz LR. A second look at comorbidity in victims of trauma: The posttraumatic stress disorder-major depression connection. Biol Psychiatry. 2000;49:902–909. doi: 10.1016/s0006-3223(00)00933-1. [DOI] [PubMed] [Google Scholar]
- 36.Clum GA. Calhoun KS. Kimmerling R. Associations among symptoms of depression and posttraumatic stress disorder and self-reported health in sexually assaulted women. J Nerv Ment Dis. 2000;188:671–678. doi: 10.1097/00005053-200010000-00005. [DOI] [PubMed] [Google Scholar]
- 37.Humphreys J. Cooper B. Miaskowski C. Differences in depression, posttraumatic stress disorder, and lifetime trauma abuse exposure in formerly abused women with mild versus moderate to severe chronic pain. J Interpers Violence Online. 2010 Feb 2; doi: 10.1177/0886260509354882. First published. [DOI] [PubMed] [Google Scholar]
- 38.Parker B. McFarlane J. Nursing assessment of the battered pregnant woman. Am J Matern Child Nurs. 1991;16:161–164. doi: 10.1097/00005721-199105000-00013. [DOI] [PubMed] [Google Scholar]
- 39.Ford-Gilboe M. Wuest J. Varcoe C, et al. Modeling the effects of intimate partner violence and access to resources on women's health in the early years after leaving an abusive partner. Soc Sci Med. 2009;68:1021–1029. doi: 10.1016/j.socscimed.2009.01.003. [DOI] [PubMed] [Google Scholar]
- 40.Bernstein D. Fink L. Childhood Trauma Questionnaire: A retrospective self-report. New York: Psychological Corporation; 1998. [Google Scholar]
- 41.Lang AJ. Stein MB. Kennedy CM. Foy DW. Adult psychopathology and intimate partner violence among survivors of childhood maltreatment. J Interpers Violence. 2004;19:1102–1118. doi: 10.1177/0886260504269090. [DOI] [PubMed] [Google Scholar]
- 42.Hudson W. McIntosh S. The assessment of spouse abuse: Two quantifiable dimensions. J Marriage Fam. 1981;43:873–885. [Google Scholar]
- 43.Campbell D. Campbell J. King C. Parker B. Ryan J. The reliability and factor structure of the index of spouse abuse with African-American battered women. Violence Vict. 1994;9:259–274. [PubMed] [Google Scholar]
- 44.Davidson J. Davidson Trauma Scale (DTS) Toronto, ON: MultiHealth Systems; 1996. [Google Scholar]
- 45.Davidson J. Book S. Colket J, et al. Assessment of a new self-rating scale for post-traumatic stress disorder. Psychol Med. 1997;27:153–160. doi: 10.1017/s0033291796004229. [DOI] [PubMed] [Google Scholar]
- 46.Zlotnick C. Shea T. Rosen K, et al. An affect-mangagement group for women with posttraumatic stress disorder and histories of child sexual abuse. J Trauma Stress. 1997;10:425–436. doi: 10.1023/a:1024841321156. [DOI] [PubMed] [Google Scholar]
- 47.Zlotnick C. Davidson J. Shea T. Pearlstein T. Validation of the Davidson Trauma Scale in a sample of survivors of childhood sexual abuse. J Nerv Ment Dis. 1996;184:255–257. doi: 10.1097/00005053-199604000-00010. [DOI] [PubMed] [Google Scholar]
- 48.Radloff L. The CES-D scale: A self-report depression scale for research in the general population. Appl Psych Meas. 1977;1:385–401. [Google Scholar]
- 49.Jarvis K. Gordon E. Novaco R. Psychological distress of children and mothers in domestic violence emergency shelters. J Fam Violence. 2005;20:390–402. [Google Scholar]
- 50.Von Korff M. Ormel J. Keefe F. Dworkin S. Grading the severity of chronic pain. Pain. 1992;50:133–149. doi: 10.1016/0304-3959(92)90154-4. [DOI] [PubMed] [Google Scholar]
- 51.Mallen C. Peat G. Thomas E. Croft P. Severe disabling chronic pain in young adults: Prevalence from a population based postal survey in North Staffordshire. www.biomedcentral.com/1471-2474/6/42. [Feb 15;2005 ];BMC Musculoskelet Disord. 2005 6:1–9. doi: 10.1186/1471-2474-6-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Plesh O. Crowford P. Gansky S. Chronic pain in a biracial population of young women. Pain. 2002;99:515–523. doi: 10.1016/S0304-3959(02)00262-2. [DOI] [PubMed] [Google Scholar]
- 53.Smith B. Penny K. Purves A, et al. The Chronic Pain Grade questionnaire: Validity and reliability in postal research. Pain. 1997;71:141–147. doi: 10.1016/s0304-3959(97)03347-2. [DOI] [PubMed] [Google Scholar]
- 54.Schumacker R. Lomax R. A beginner's guide to structural equation modeling. 2nd. Mahwah, NJ: Lawrence Erlbaum Associates; 2004. [Google Scholar]
- 55.Verhaak P. Kerssens J. Dekke J. Sorbi M. Bensing J. Prevalence of chronic benign pain disorder among adults: A review of the literature. Pain. 1998;77:231–239. doi: 10.1016/S0304-3959(98)00117-1. [DOI] [PubMed] [Google Scholar]
- 56.Carr D. Goudas L. Acute pain. Lancet. 1999;353:2051–2058. doi: 10.1016/S0140-6736(99)03313-9. [DOI] [PubMed] [Google Scholar]
- 57.Felitti VJ. Anda RF. Nordenberg D, et al. Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study. Am J Prev Med. 1998;14:245–258. doi: 10.1016/s0749-3797(98)00017-8. [DOI] [PubMed] [Google Scholar]
- 58.Yehuda R. Current status of cortisol findings in post-traumatic stress disorder. Psychiatr Clin North Am. 2002;25:341–368. doi: 10.1016/s0193-953x(02)00002-3. [DOI] [PubMed] [Google Scholar]
- 59.Yehuda R. Advances in understanding neuroendocrine alterations in PTSD and their therapeutic implications. Ann NY Acad Sci. 2006;1071:137–166. doi: 10.1196/annals.1364.012. [DOI] [PubMed] [Google Scholar]
- 60.Yehuda R. Halligan S. Golier J. Grossman R. Bierer L. Effects of trauma exposure on the cortisol response to dexamethasone administration in PTSD and major depressive disorder. Psychoneuroendocrinology. 2004;29:389–404. doi: 10.1016/s0306-4530(03)00052-0. [DOI] [PubMed] [Google Scholar]
- 61.Robles T. Glaser R. Kielcolt-Glaser J. Out of balance: A new look at chronic stress, depression and immunity. Current Dir Psychol Sci. 2005;14:111–115. [Google Scholar]
- 62.Meewisse M. Reitsma J. de Vries G. Gersons B. Olff M. Cortisol and post-traumatic stress disorder in adults: Systematic review and meta-analysis. Br J Psychiatry. 2007;191:387–392. doi: 10.1192/bjp.bp.106.024877. [DOI] [PubMed] [Google Scholar]
- 63.Scott-Tilley D. Tilton A. Sandel M. Biologic correlates to the development of post-traumatic stress disorder in female victims of intimate partner violence: Implications for practice. Perspect Psychiatr Care. 2010;46:26–36. doi: 10.1111/j.1744-6163.2009.00235.x. [DOI] [PubMed] [Google Scholar]
- 64.Breslau N. The epidemiology of trauma, PTSD, and other posttrauma disorders. Trauma Violence Abuse. 2009;10:198–210. doi: 10.1177/1524838009334448. [DOI] [PubMed] [Google Scholar]
- 65.Mechanic M. Weaver T. Resick P. Mental health consequences of intimate partner abuse: A multidimensional assessment of four different forms of abuse. Violence Women. 2008;14:634–654. doi: 10.1177/1077801208319283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Wuest J. Merritt-Gray M. Lent B. Varcoe C. Connors A. Ford-Gilboe M. Patterns of medication use among women survivors of intimate partner violence. Can J Public Health. 2007;98:460–464. doi: 10.1007/BF03405439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Gill J. Page G. Sharps P. Campbell JC. Experiences of traumatic events and associations with PTSD and depression development in urban health care-seeking women. J Urban Health. 2008;5:693–706. doi: 10.1007/s11524-008-9290-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wuest J. Ford-Gilboe M. Merritt-Gray M. Berman H. Intrusion: The central problem for family health promotion among children and single mothers after leaving an abusive partner. Qual Health Res. 2003;13:597–622. doi: 10.1177/1049732303013005002. [DOI] [PubMed] [Google Scholar]
- 69.Raphael K. Widom C. Lange G. Childhood victimization and pain in adulthood: A prospective investigation. Pain. 2002;92:283–293. doi: 10.1016/s0304-3959(01)00270-6. [DOI] [PubMed] [Google Scholar]