Abstract
OBJECTIVE
To examine trends in nontraumatic lower-extremity amputations (LEAs) over an 8-year period in patients with and without diabetes in Spain.
RESEARCH DESIGN AND METHODS
We identified all patients who underwent an LEA using national hospital discharge data. Discharges were grouped by diabetes status: type 1 diabetes, type 2 diabetes, and no diabetes. The incidence of discharges attributed to amputations were calculated overall and stratified by diabetes status and year. We calculated length of stay and in-hospital fatality stratified by diabetes status and type of LEA.
RESULTS
From 2001 to 2008, 46,536 minor LEAs and 43,528 major LEAs were performed. In patients with type 1 diabetes, the incidence of minor and major amputations decreased significantly from 2001 to 2008 (0.88–0.43 per 100,000 inhabitants and 0.59–0.22 per 100,000 inhabitants, respectively). In patients with type 2 diabetes, the incidence of minor and major LEAs increased significantly (9.23–10.9 per 100,000 inhabitants and 7.12–7.47 per 100,000 inhabitants). Hospital stay was similar among type 1 diabetic and type 2 diabetic subjects, according to the type of LEA. Only in-hospital mortality for minor LEAs among type 1 diabetic subjects decreased significantly (4.0% in 2001 vs. 1.6% in 2008).
CONCLUSIONS
Our national data show a decrease in the incidence of major and minor LEAs in patients with type 1 diabetes and an increase among patients with type 2 diabetes. Further improvement is necessary in the preventive care and early treatment of patients with diabetes. The management of foot lesions, especially among type 2 diabetic patients, is particularly urgent.
The prevalence of lower-extremity disease, including peripheral arterial disease and peripheral neuropathy, is twice as high in individuals with diabetes as in the general population (1,2). Despite intensive interventions, many of these patients require a lower-extremity amputation (LEA), which has a high social impact and poor clinical prognosis as well as considerable financial implications for health care systems (1). LEA rates are 15–40 times higher in diabetic patients than in nondiabetic patients (3).
The prevalence of diabetes in the Spanish population is ~5–6%, and this figure increases with age (4). This is expected to lead to an increase in the number of amputations (1). However, Krishnan et al. (5) suggested that appropriate multidisciplinary care of patients with diabetes can actually reduce the incidence of LEAs by up to 70%.
Vamos et al. (2) indicated that trends in amputation procedures can help improve our understanding of the burden of diabetes and could be used to inform future health care planning. In Spain, little information is available on the trends and associated outcomes of LEAs (6,7). We used national hospital discharge data to examine trends in the incidence of LEA procedures (major and minor) in patients with type 1 and type 2 diabetes between 2001 and 2008 in Spain. We also analyzed outcomes of discharge, such as length of stay (LOS) and in-hospital mortality.
RESEARCH DESIGN AND METHODS
The Spanish Minimum Basic Data Set (MBDS) was used as the data source. This national hospital database is managed by the Spanish Ministry of Health (8) and includes hospital details, patient data, surgical and obstetric procedures, other procedures, and date and type of discharge. The Spanish Ministry of Health sets standards for registration and performs periodic audits (8).
Diagnoses and surgical procedures were assigned using the ICD-9-CM; all inpatients in the MBDS database had a primary surgical procedure and/or primary diagnosis and up to 20 procedures and/or 14 diagnoses coded at discharge.
Amputations were identified as any procedure code for LEA in any procedure field between 1 January 2001 and 31 December 2008. A minor amputation was defined as any LEA distal to the ankle joint (ICD-9-CM codes 84.10–84.12); a major amputation was defined as any LEA through or proximal to the ankle joint (ICD-9-CM codes 84.13–84.17). All traumatic LEAs, defined by any trauma-related code of the lower extremity in any diagnosis field, were excluded (ICD-9-CM codes 895–897, 905.9, 928–929, and 959). Discharges were grouped by diabetes status as follows: no diabetes, type 1 diabetes (ICD-9-CM codes 250.x1 and 250.x3), and type 2 diabetes (ICD-9-CM codes: 250.x0 and 250.x2). No unique identifiers were available when patient data were obtained; therefore, it was not possible to identify multiple amputations in an individual unless the subsequent amputation occurred during the same hospital stay. For patients with multiple LEAs during their stay, only the highest LEA was used in the data analysis. We calculated LOS and in-hospital fatality stratified by diabetes status and type of LEA.
The incidence of discharges after amputation was calculated overall and by diabetes status for each year. We calculated the yearly age- and sex-specific incidence rates (per 100,000 inhabitants) by dividing the number of cases per year per sex and age-group by the corresponding number of people in that population group, according to the National Institute of Statistics on 31 December of each year (9).
Statistical analyses were performed using Stata version 10.1 (Stata, College Station, TX). A descriptive statistical analysis was performed for all the continuous variables and categories by stratifying LEAs as major or minor. To test the time trend in the incidence of LEA procedures, we fitted separate Poisson regression models for patients with and without diabetes, using year of discharge, sex, and age as independent variables. For in-hospital mortality, logistic regression analyses were performed with mortality as a binary outcome using the same variables. In these models, an interaction term for diabetes and year of discharge was tested and included if P < 0.05.
Data confidentiality was maintained at all times according to Spanish legislation. Patient identifiers were deleted before the database was provided to the authors in order to maintain patient anonymity. It is not possible to identify patients at individual levels, either in this article or in the database. Given the anonymous and mandatory nature of the dataset, the requirement for informed consent was not necessary.
RESULTS
Between 2001 and 2008, 90,064 nontraumatic amputations (46,536 minor and 43,528 major) corresponding to 86,023 discharges were performed in Spain. Simultaneous bilateral procedures were recorded in 4.4% (n = 4,041) of cases. Over the study period, 64.5% of all discharges after a nontraumatic LEA occurred in patients with diabetes, with type 1 diabetic patients accounting for 3.5% and type 2 diabetic patients for 61.0% of discharges.
The mean age of patients who underwent LEAs was (means ± SD) 69.5 ± 14.6 years: patients with type 1 diabetes were aged 62.09 ± 14.9 years; patients with type 2 diabetes were aged 70.7 ± 11.0 years; and patients without diabetes were aged 70.2 ± 11.4 years. A considerable male predominance was observed in LEAs among patients with diabetes, with the male-to-female ratio being >2:1 (type 1 diabetes: 2.23, type 2 diabetes: 2.18, and no diabetes: 2.4). Minor LEAs were more common than major LEAs in patients with diabetes (minor-to-major ratio 1.69 [95% CI 1.61–1.78] for type 1 diabetes and 1.39 [1.37–1.40] for type 2 diabetes).
Minor LEAs
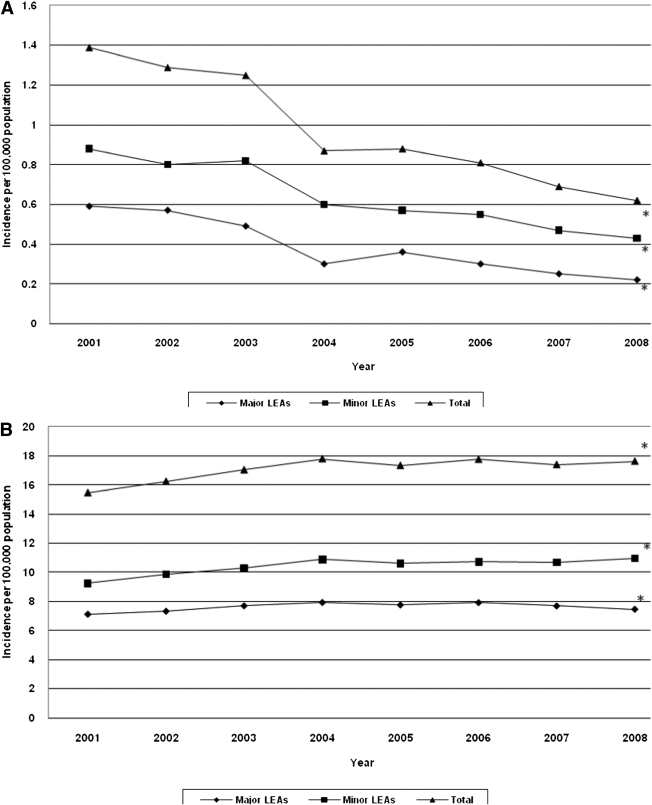
Between 2001 and 2008, the overall number of nontraumatic minor LEAs in Spain increased from 5,327 to 6,378. The incidence of minor amputations in patients with type 1 diabetes decreased significantly from 0.88 (95% CI 0.79–0.98) to 0.43 (0.37–0.50) per 100,000 inhabitants. In patients with type 2 diabetes, the incidence of minor LEAs increased significantly from 9.23 (8.92–9.55) to 10.97 (10.66–11.29) per 100,000 inhabitants during the study period (Fig. 1).
Figure 1.
Changes in minor and major LEA incidence rates in patients with type 1 diabetes expressed per 100,000 inhabitants (A) and in patients with type 2 diabetes expressed per 100,000 inhabitants (B) (Spain, 2001–2008). *P < 0.05 (Poisson regression analysis). Population data were obtained from the Spanish National Institute of Statistics (9). The estimated total population was 40,964,000 in 2001; 41,663,000 in 2002; 42,345,000 in 2003; 43,038,000 in 2004; 43,758,000 in 2005; 44,474,000 in 2006; 45,283,000 in 2007; and 45,828,000 in 2008.
The mean age of patients undergoing a minor amputation was 66.9 ± 14.6 years. No significant change in age was observed during the study period. However, patients with type 2 diabetes were significantly older than those with type 1 diabetes (aged 68.6 vs. 59.8 years; P < 0.05) (Table 1).
Table 1.
Hospital discharges after LEAs in Spain, 2001–2008
| Minor LEAs | Major LEAs | Total* | |
|---|---|---|---|
| Type 1 diabetes†‡ | 59.8 (14.3) | 65.8 (15.0) | 62.0 (14.9) |
| Age (years) (%) | |||
| <44 | 332 (16.6) | 141 (11.9) | 450 (15.0) |
| 45–74 | 1,296 (64.9) | 649 (55.0) | 1,836 (61.0) |
| ≥75 | 368 (18.4) | 391 (33.1) | 724 (24.1) |
| Sex (%) | |||
| Male | 1,455 (72.9) | 744 (63.0) | 2,079 (69.1) |
| Female | 541 (27.1) | 437 (37.0) | 931 (30.9) |
| Type 2 diabetes†‡ | 68.6 (11.5) | 73.6 (10.2) | 70.7 (11.0) |
| Age (years) (%) | |||
| <44 | 699 (2.2) | 203 (0.9) | 873 (1.7) |
| 45–74 | 20,822 (64.7) | 11,088 (47.8) | 30,190 (57.5) |
| ≥75 | 10,664 (33.1) | 11,921 (51.4) | 21,428 (40.8) |
| Sex (%) | |||
| Male | 23,791 (73.9) | 14,312 (61.7) | 36,027 (68.6) |
| Female | 8,394 (26.1) | 8,900 (38.3) | 16,464 (31.4) |
| No diabetes†‡ | 63.9 (20.5) | 71.1 (17.3) | 68.3 (19.0) |
| Age (years) (%) | |||
| <44 | 2,072 (16.8) | 1,727 (9.0) | 3,715 (12.2) |
| 45–74 | 5,682 (46.0) | 7,264 (38.0) | 12,493 (40.9) |
| ≥75 | 4,601 (37.2) | 1,0144 (53.0) | 14,314 (46.9) |
| Sex (%) | 9,220 (74.6) | 13,355 (69.8) | 21,809 (71.5) |
| Male | |||
| Female | 3,135 (25.4) | 5,780 (30.2) | 8,713 (28.5) |
Data are means (SD).
*Not all the denominators add up to the same number because the same patient can undergo multiple amputations.
†Statistically significant differences (P < 0.05) on comparing type 1 diabetes with type 2 diabetes for minor LEAs.
‡Statistically significant differences (P < 0.05) on comparing type 1 diabetes with type 2 diabetes for major LEAs.
LOS was similar among patients undergoing minor LEAs. Multivariate analysis revealed that LOS did not change in patients with type 1 diabetes, type 2 diabetes, or those without diabetes during the study period (Table 2). In-hospital mortality rates for type 1 diabetes–related minor LEAs decreased significantly during the study period (4.0% in 2001 vs. 1.6% in 2008) after adjustment for age, sex, and year. We found no significant change over time for in-hospital mortality rate, type 2 diabetes, or no diabetes (Table 2).
Table 2.
Hospital discharges after minor LEAs in Spain, 2001–2008
| 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | Total | |
|---|---|---|---|---|---|---|---|---|---|
| Type 1 diabetes | |||||||||
| Number of discharges* | 326 | 300 | 313 | 234 | 225 | 222 | 193 | 183 | 1,996 |
| Rate† | 0.88 | 0.8 | 0.82 | 0.6 | 0.57 | 0.55 | 0.47 | 0.43 | NA |
| LOS, median (days) | 18 | 18 | 19 | 15 | 17 | 18 | 16 | 14 | 17 |
| LOS, interquartile range (days) | 3–30 | 3–29 | 3–33 | 3–28 | 3–32 | 4–28 | 3–28 | 2–27 | 3–64 |
| Number of deaths* | 13 | 4 | 8 | 7 | 7 | 6 | 4 | 3 | 52 |
| Percentage of deaths* | 4.0 | 1.3 | 2.6 | 3.0 | 3.1 | 2.7 | 2.1 | 1.6 | 2.6 |
| Type 2 diabetes | |||||||||
| Number of discharges* | 3,320 | 3,615 | 3,843 | 4,141 | 4,118 | 4,243 | 4,333 | 4,572 | 32,185 |
| Rate† | 9.23 | 9.87 | 10.29 | 10.88 | 10.61 | 10.72 | 10.68 | 10.97 | NA |
| LOS, median (days) | 19 | 19 | 20 | 19 | 18 | 18 | 19 | 18 | 19 |
| LOS, interquartile range (days) | 4–64 | 4–66 | 4–66 | 4–64 | 4–64 | 3–60 | 3–64 | 3–63 | 4–64 |
| Number of deaths* | 135 | 148 | 148 | 146 | 156 | 126 | 162 | 161 | 1,182 |
| Percentage of deaths* | 4.1 | 4.1 | 3.9 | 3.5 | 3.8 | 3.0 | 3.7 | 3.5 | 3.7 |
| No diabetes | |||||||||
| Number of discharges* | 1,681 | 1,567 | 1,528 | 1,485 | 1,444 | 1,486 | 1,541 | 1,623 | 12,355 |
| Rate† | 4.67 | 4.29 | 4.09 | 3.89 | 3.73 | 3.76 | 3.79 | 3.89 | NA |
| LOS, median (days) | 19 | 19 | 18 | 17 | 18 | 18 | 18 | 17 | 18 |
| LOS, interquartile range (days) | 2–69 | 2–69 | 2–74 | 2–68 | 2–74 | 2–77 | 2–68 | 2–74 | 2–71 |
| Number of deaths* | 78 | 99 | 98 | 90 | 95 | 71 | 87 | 93 | 711 |
| Percentage of deaths* | 4.6 | 6.3 | 6.4 | 6.1 | 6.6 | 4.8 | 5.6 | 5.7 | 5.8 |
NA, not available.
*Significant association (P < 0.05) for time trend among discharges after minor LEAs.
†Rate changes in minor LEA incidence rates in patients with type 1 diabetes expressed per 100,000 inhabitants; in patients with type 2 diabetes expressed per 100,000 inhabitants; and in patients without diabetes expressed per 100,000 inhabitants (Spain, 2001–2008).
Major LEAs
The number of major nontraumatic amputations increased from 5,211 to 5,474 during the study period. The incidence of major amputations decreased significantly from 0.59 (95% CI 0.51–0.67) to 0.22 (0.17–0.26) per 100,000 inhabitants in patients with type 1 diabetes. However, in patients with type 2 diabetes, the incidence of major LEAs increased significantly from 7.12 (6.84–7.40) to 7.47 (7.21–7.73) (Fig. 1).
The mean age of patients undergoing a major amputation was 72 ± 14 years. There was no significant change in age during the study period. However, patients with type 2 diabetes were significantly older than those with type 1 diabetes (73.6 vs. 65.8 years; P < 0.05) (Table 1).
LOS was similar among patients undergoing major LEAs. Multivariate analysis did not reveal changes in LOS in patients with type 1 diabetes, type 2 diabetes, or those without diabetes during the study period (Table 3). In-hospital mortality rates for type 1 diabetes–related major LEAs did not change (8.3% in 2001 vs. 8.7% in 2008); however, they increased for type 2 diabetes (9.7% in 2001 vs. 10.1% in 2008) and decreased for major LEAs in patients without diabetes (15.1% in 2001 vs. 14.0% in 2008). Logistic regression analysis showed no significant change in hospital mortality rates associated with major LEAs after adjustment for age, sex, and year (Table 3).
Table 3.
Hospital discharges after major LEAs in Spain, 2001–2008
| 2001 | 2002 | 2003 | 2004 | 2005 | 2006 | 2007 | 2008 | Total | |
|---|---|---|---|---|---|---|---|---|---|
| Type 1 diabetes | |||||||||
| Number of discharges* | 216 | 210 | 183 | 117 | 141 | 119 | 103 | 92 | 1,181 |
| Rate† | 0.59 | 0.57 | 0.49 | 0.3 | 0.36 | 0.3 | 0.25 | 0.22 | NA |
| LOS, median (days) | 19 | 17 | 17 | 19 | 17 | 16 | 18 | 19 | 18 |
| LOS, interquartile range (days) | 5–38 | 4–72 | 3–106 | 5–91 | 3–69 | 3–77 | 4–91 | 4–89 | 4–83 |
| Number of deaths | 18 | 17 | 22 | 8 | 12 | 9 | 11 | 8 | 105 |
| Percentage of deaths | 8.3 | 8.1 | 12.0 | 6.8 | 8.5 | 7.6 | 10.7 | 8.7 | 8.8 |
| Type 2 diabetes | |||||||||
| Number of discharges* | 2,484 | 2,624 | 2,822 | 2,970 | 2,974 | 3,113 | 3,112 | 3,113 | 23,212 |
| Rate† | 7.12 | 7.33 | 7.71 | 7.94 | 7.77 | 7.93 | 7.7 | 7.47 | NA |
| LOS, median (days) | 19 | 19 | 19 | 18 | 18 | 18 | 18 | 16 | 18 |
| LOS, interquartile range (days) | 5–66 | 5–69 | 5–68 | 5–63 | 5–69 | 5–64 | 5–68 | 5–66 | 5–66 |
| Number of deaths | 242 | 269 | 310 | 307 | 313 | 299 | 353 | 313 | 2,406 |
| Percentage of deaths | 9.7 | 10.3 | 11.0 | 10.3 | 10.5 | 9.6 | 11.3 | 10.1 | 10.4 |
| No diabetes | |||||||||
| Number of discharges | 2,511 | 2,503 | 2,468 | 2,390 | 2,312 | 2,378 | 2,304 | 2,269 | 19,135 |
| Rate | 7.20 | 7.03 | 6.75 | 6.39 | 6.03 | 6.06 | 5.70 | 5.44 | NA |
| LOS, median (days) | 18 | 17 | 17 | 18 | 18 | 17 | 18 | 19 | 18 |
| LOS, interquartile range (days) | 5–71 | 5–72 | 4–72 | 4–77 | 4–81 | 4–80 | 4–82 | 4–77 | 4–77 |
| Number of deaths | 380 | 341 | 334 | 330 | 323 | 317 | 294 | 318 | 2,637 |
| Percentage of deaths | 15.1 | 13.6 | 13.5 | 13.8 | 14.0 | 13.3 | 12.8 | 14.0 | 13.8 |
NA, not available.
*Significant association (P < 0.05) for time trend among discharges after major LEAs.
†Rate changes in major LEA incidence rates in patients with type 1 diabetes expressed per 100,000 inhabitants; in patients with type 2 diabetes expressed per 100,000 inhabitants; and in patients without diabetes expressed per 100,000 inhabitants (Spain, 2001–2008).
CONCLUSIONS
To our knowledge, this is the first nationwide analysis of the incidence of diabetes-related minor and major LEAs in Spain. Our results reveal a reduction in the overall number of nontraumatic LEAs between 2001 and 2008, with different trends in minor and major LEAs in patients with type 1 diabetes and patients without diabetes. An upward trend was observed in type 2 diabetes–related minor and major LEAs; however, the absolute increase was small.
Previous studies reporting a decrease in the incidence of LEAs in patients with diabetes stated that they were performed by researchers who were highly specialized in diabetic foot care and working in centers with well-established vascular services (5,10). In northern Europe, an increase in the proportion of hospitals with specialist diabetic podiatry services (32–72%) was associated with a drop in the rate of diabetes-related major amputations, from 5.5 to 3.6 per 100,000 people, despite a rise in the prevalence of diabetes (11,12).
In Spain, studies (6,7) from several geographical areas showed decreasing LEA rates in patients with diabetes. Other Spanish regional studies (13,14) indicated that LEA rates in populations with or without diabetes are higher than previously reported; however, national population-based data on trends in LEAs in Spain are lacking.
In 2007, Trautner et al. (15) found a significant reduction in the incidence of LEAs between 1990 and 2005 in diabetic patients, although this remained unchanged in nondiabetic patients. The reduction in relative risk was particularly clear for major amputations. The authors explained their findings by referring to the implementation of intensive diabetic foot care in the study region. This is consistent with our results and with those of studies from other countries where a reduction in the number of LEAs performed on diabetic subjects was observed (16).
The upward trend in LEAs in patients with type 2 diabetes likely reflects a number of factors, such as improved survival of patients, increases in prevalence and incidence, greater awareness of diabetic foot disease, improved specialist services and agreement between the patient and the expert that loss of the limb is (or is not) the best option (2,4,17). Available information shows that the prevalence of type 2 diabetes is rising in Spain; therefore, the increase in LEAs among those with type 2 diabetes is possibly less pronounced than one would surmise from our data (4). Separate data for the incidence of LEAs related to type 1 and type 2 diabetes are rarely documented in population-based studies (2). Ebskov et al. (18) indicated that the overall decrease in major LEA rates was attributable to a decline in the number of patients with type 1 diabetes. In Spain, we cannot conclude that this decrease in LEA rates among type 1 diabetic patients is associated with changes in the prevalence of type 1 diabetes. Zorrilla Torras et al. (19) indicated that incidence data showed no significant changes during 1997–2005 for type 1 diabetes, and other studies (4,19) in Spain reach similar conclusions. We agree with Jonasson et al. (20), who suggested that in Sweden the reduction in the risk of nontraumatic LEAs among patients with type 1 diabetes might be attributed to the introduction of a program for prevention and treatment of ulceration in patients with diabetes. Furthermore, previous studies show that patients with type 1 diabetes are more strictly controlled for risk factors and diabetic foot disease; in contrast, many patients with type 2 diabetes have less aggressive management of risk factors (18).
The proportion of minor and major LEAs was higher in men than in women. This finding is consistent with those of previous studies (2,11). However, the finding is not easily explained. Congdon et al. (21) indicated that although the prevalence of diagnosed diabetes has increased considerably in men, it may not fully explain the increasing male predominance in LEAs.
LOS, which may be regarded as a major determinant of the financial burden of diabetes-related LEAs on society, was found to decrease, although this may reflect general changes in hospital practices and may not necessarily be a consequence of efforts to manage foot disease in patients with diabetes (11). We observed that the median LEA-related LOS was similar for minor and major amputations. One explanation is that in-hospital mortality was ~2.5 times higher for major LEAs than for minor LEAs, thus accounting for the unexpectedly low LOS.
Overall in-hospital mortality rates for LEAs did not change significantly between 2001 and 2008, except for type 1 diabetes–related minor LEAs. The exact reason for this trend is not fully understood. Vamos et al. (2) indicated that patients with type 1 diabetes are more strictly controlled for risk factors and diabetic foot disease. Outcomes such as LOS may have been influenced by covariates other than postoperative complications. In such a scenario, only in-hospital mortality can be used to draw direct conclusions on the complications rate in the current study.
The strength of our study lies in its large sample size and standardized methodology. Nevertheless, it does present a series of limitations. Our data source was the MBDS, an administrative database that contains discharge data for Spanish hospitalizations and uses information the physician has included in the discharge report. Therefore, it does not include all the variables of the clinical history, and clinical factors might have contributed to the variability observed in LOS. Physicians usually only record information on the main diseases (up to 15) and procedures (up to 20). Thus, if the physician considers that a comorbid condition is not related, has not increased LOS, or has complicated the main disease, it will probably not be reflected in the database. Another limitation of this database is its anonymity, which makes it impossible to detect whether the same patient was admitted more than once during the same year.
Nevertheless, this dataset, which was introduced in Spain in 1982, is a mandatory register, and its coverage is estimated to be >95% (8). Furthermore, it provides useful information on hospital management of LEAs, given that it brings together data from all discharges after LEAs, regardless of the characteristics of the attending hospital or the department to which the patient is admitted. Ribera et al. (22) indicated that because the quality of the coding seems to be improving, administrative databases may become more useful, not only in estimating raw rates but in providing characteristics of hospitalization and adjusted mortality rates. As a consequence, more patients with diabetes could be identified. In any case, we believe this would only represent a small effect on amputation rates (22).
The major limitation of our study is that we were unable to calculate diabetes type–specific incidence rates. In Spain no nationwide representative studies with blood glucose measurements or national diabetes prospective registries are available, and, consequently, we do not have denominators to estimate rates for type 1 or 2 diabetes (4). In addition, Jeffcoate et al. (17) indicated that use of the total population is necessary when the prevalence of diabetes is not well documented. Because of the impossibility of screening the whole population for diabetes, concessions had to be made.
Because we cannot distinguish between the two lower extremities, we have to assume that all amputations during one discharge are conducted on the same limb; therefore, we might underestimate the number of LEAs. However, we were able to differentiate between type 1 and type 2 diabetes and we also included a nondiabetic comparator. Although concerns about the accuracy of routinely collected datasets have been raised, these are periodically audited. As a consequence, the quality and validity of our dataset has been assessed and proved useful for health research (22). Despite these limitations, we believe that the MBDS is a valid instrument for conducting epidemiologic studies on chronic diseases. Furthermore, discharge databases have been widely used by other authors to assess outcomes, burdens, and trends in LEA procedures in patients with and without diabetes (2,16,23,24).
In conclusion, our national data show a decrease in the incidence of major and minor LEAs in patients with type 1 diabetes between 2001 and 2008 in Spain. The decrease may be related to more strictly controlled risk factors in these patients. However, the burden of amputations increased in patients with type 2 diabetes, suggesting that diabetic foot care remains suboptimal in Spain. Additional improvements in preventive care and early treatment are necessary for patients with diabetes. The management of foot lesions, especially among patients with type 2 diabetes, is particularly urgent.
Acknowledgments
This study forms part of research funded by the Fondo de Investigaciones Sanitarias (Health Research Fund grant no. PI10/00360), Instituto de Salud Carlos III.
No potential conflicts of interest relevant to this article were reported.
A.L.-d.-A. researched data, contributed to discussion, and wrote, reviewed, and edited the manuscript. M.A.M.-H. and P.C.-G. contributed to discussion and reviewed and edited the manuscript. V.H.-B. researched data and reviewed and edited the manuscript. Á.G.-d.-M. contributed to discussion and reviewed and edited the manuscript. R.J.-G. researched data, contributed to discussion, and wrote, reviewed, and edited the manuscript. All authors reviewed and gave their final approval of the version to be submitted.
The authors thank the Ministry of Health and Social Policy for providing them with the dataset and Alejandro Alvaro (Preventive Medicine and Public Health Teaching and Research Unit, Health Sciences Faculty, Rey Juan Carlos University) for his help in checking the databases.
References
- 1.Boulton AJ, Vileikyte L, Ragnarson-Tennvall G, Apelqvist J. The global burden of diabetic foot disease. Lancet 2005;366:1719–1724 [DOI] [PubMed] [Google Scholar]
- 2.Vamos EP, Bottle A, Majeed A, Millett C. Trends in lower extremity amputations in people with and without diabetes in England, 1996-2005. Diabetes Res Clin Pract 2010;87:275–282 [DOI] [PubMed] [Google Scholar]
- 3.Frykberg RG, Zgonis T, Armstrong DG, et al. ; American College of Foot and Ankle Surgeons Diabetic foot disorders: a clinical practice guideline (2006 revision). J Foot Ankle Surg 2006;45(Suppl.):S1–S66 [DOI] [PubMed] [Google Scholar]
- 4.Ruiz-Ramos M, Escolar-Pujolar A, Mayoral-Sánchez E, Corral-San Laureano F, Fernández-Fernández I. Diabetes mellitus in Spain: death rates, prevalence, impact, costs and inequalities. Gac Sanit 2006;20(Suppl. 1):15–24 [in Spanish] [DOI] [PubMed] [Google Scholar]
- 5.Krishnan S, Nash F, Baker N, Fowler D, Rayman G. Reduction in diabetic amputations over 11 years in a defined U.K. population: benefits of multidisciplinary team work and continuous prospective audit. Diabetes Care 2008;31:99–101 [DOI] [PubMed] [Google Scholar]
- 6.Calle-Pascual AL, Garcia-Torre N, Moraga I, et al. Epidemiology of nontraumatic lower-extremity amputation in area 7, Madrid, between 1989 and 1999: a population-based study. Diabetes Care 2001;24:1686–1689 [DOI] [PubMed] [Google Scholar]
- 7.Almaraz MC, Soriguer F, Zamorano D, et al. Incidence of amputaciones of the lower extremities in the population with diabetes mellitus in Málaga (1996-1997). Aten Primaria 2000;26:677–680 [in Spanish] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Instituto Nacional de Gestión Sanitaria, Ministerio de Sanidad y Consumo. Conjunto Mínimo Básico de Datos, Hospitales del INSALUD [article online], 2001. Available from http://www.ingesa.msc.es/estadEstudios/documPublica/internet/home.htm Accessed 11 April 2011
- 9.Instituto Nacional de Estadística (INE). Population estimates [article online], 2010. Available from http://www.ine.es Accessed 15 September 2010
- 10.Canavan RJ, Unwin NC, Kelly WF, Connolly VM. Diabetes- and nondiabetes-related lower extremity amputation incidence before and after the introduction of better organized diabetes foot care: continuous longitudinal monitoring using a standard method. Diabetes Care 2008;31:459–463 [DOI] [PubMed] [Google Scholar]
- 11.van Houtum WH, Rauwerda JA, Ruwaard D, Schaper NC, Bakker K. Reduction in diabetes-related lower-extremity amputations in the Netherlands: 1991-2000. Diabetes Care 2004;27:1042–1046 [DOI] [PubMed] [Google Scholar]
- 12.Edmonds ME. The diabetic foot, 2003. Diabetes Metab Res Rev 2004;20(Suppl. 1):S9–S12 [DOI] [PubMed] [Google Scholar]
- 13.Aragón-Sánchez J, García-Rojas A, Lázaro-Martínez JL, et al. Epidemiology of diabetes-related lower extremity amputations in Gran Canaria, Canary Islands (Spain). Diabetes Res Clin Pract 2009;86:e6–e8 [DOI] [PubMed] [Google Scholar]
- 14.Rubio JA, Salido C, Albarracín A, Jiménez S, Alvarez J. Incidence of lower extremity amputations in Area 3 of Madrid. Retrospective study during the period 2001-2006. Rev Clin Esp 2010;210:65–69 [in Spanish] [DOI] [PubMed] [Google Scholar]
- 15.Trautner C, Haastert B, Mauckner P, Gätcke LM, Giani G. Reduced incidence of lower-limb amputations in the diabetic population of a German city, 1990-2005: results of the Leverkusen Amputation Reduction Study (LARS). Diabetes Care 2007;30:2633–2637 [DOI] [PubMed] [Google Scholar]
- 16.Icks A, Haastert B, Trautner C, Giani G, Glaeske G, Hoffmann F. Incidence of lower-limb amputations in the diabetic compared to the non-diabetic population: findings from nationwide insurance data, Germany, 2005-2007. Exp Clin Endocrinol Diabetes 2009;117:500–504 [DOI] [PubMed] [Google Scholar]
- 17.Jeffcoate WJ, van Houtum WH. Amputation as a marker of the quality of foot care in diabetes. Diabetologia 2004;47:2051–2058 [DOI] [PubMed] [Google Scholar]
- 18.Ebskov B, Ebskov L. Major lower limb amputation in diabetic patients: development during 1982 to 1993. Diabetologia 1996;39:1607–1610 [DOI] [PubMed] [Google Scholar]
- 19.Zorrilla Torras B, Cantero Real JL, Barrios Castellanos R, Ramírez Fernández J, Argente Oliver J, González Vergaz A; en nombre del Registro de Incidencia de Diabetes Tipo 1 en Menores de 15 años (Consejería de Sanidad, Comunidad de Madrid) Incidence of type 1 diabetes mellitus in children: results from the population registry of the Madrid Region, 1997-2005. Med Clin (Barc) 2009;132:545–548 [in Spanish] [DOI] [PubMed] [Google Scholar]
- 20.Jonasson JM, Ye W, Sparén P, Apelqvist J, Nyrén O, Brismar K. Risks of nontraumatic lower-extremity amputations in patients with type 1 diabetes: a population-based cohort study in Sweden. Diabetes Care 2008;31:1536–1540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Congdon P. Estimating diabetes prevalence by small area in England. J Public Health (Oxf) 2006;28:71–81 [DOI] [PubMed] [Google Scholar]
- 22.Ribera A, Marsal JR, Ferreira-González I, et al. Predicting in-hospital mortality with coronary bypass surgery using hospital discharge data: comparison with a prospective observational study. Rev Esp Cardiol 2008;61:843–852 [PubMed] [Google Scholar]
- 23.Vamos EP, Bottle A, Edmonds ME, Valabhji J, Majeed A, Millett C. Changes in the incidence of lower extremity amputations in individuals with and without diabetes in England between 2004 and 2008. Diabetes Care 2010;33:2592–2597 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Ikonen TS, Sund R, Venermo M, Winell K. Fewer major amputations among individuals with diabetes in Finland in 1997-2007: a population-based study. Diabetes Care 2010;33:2598–2603 [DOI] [PMC free article] [PubMed] [Google Scholar]