Abstract
OBJECTIVE
Type 2 diabetes is associated with increased risks of several types of cancer; however, its relationship to renal cell cancer remains unclear.
RESEARCH DESIGN AND METHODS
A total of 118,177 women aged 30 to 55 years at baseline (1976) were followed up through 2008 in the Nurses’ Health Study. Self-reports of physician-diagnosed diabetes were collected at baseline and updated biennially. Hazard ratios (HRs) were calculated using Cox proportional hazards models with adjustment for age, BMI, hypertension, smoking, and parity.
RESULTS
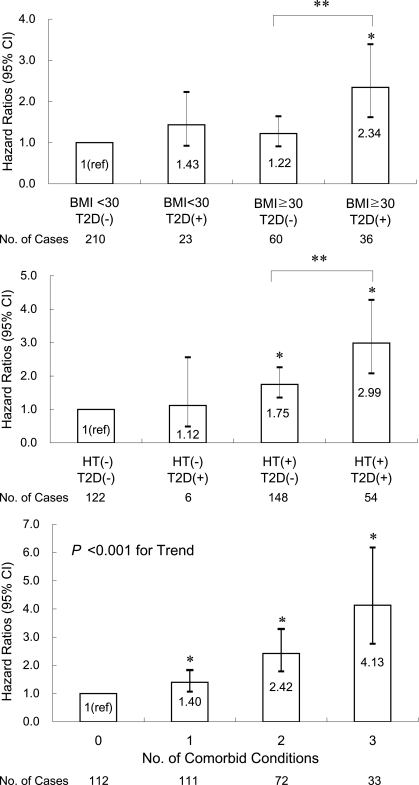
During 32 years of follow-up (3,531,170 person-years), 16,819 cases of type 2 diabetes and 330 cases of pathology-confirmed incident renal cell cancer were documented. After multivariate adjustment, type 2 diabetes was significantly associated with an increased risk of renal cell cancer (HR 1.60 [95% CI 1.19–2.17]). These associations were consistent across different strata of BMI, smoking, and hypertension (Pinteraction ≥ 0.32). The risk of renal cell cancer increased with an increasing number of comorbidities, including obesity, hypertension, and type 2 diabetes (Ptrend < 0.001). When compared with women without any comorbidity, women who had all three conditions had a HR of 4.13 (2.76–6.18) for renal cell cancer.
CONCLUSIONS
Type 2 diabetes is independently associated with an increased risk of renal cell cancer in women. In addition, comorbidity of obesity, hypertension, and type 2 diabetes substantially elevates the risk of renal cell cancer.
The prevalence of type 2 diabetes is increasing worldwide. From 1980 through 2007, the number of Americans with diabetes more than tripled from 5.6 million to 17.4 million (1). Recent epidemiologic evidence suggests that type 2 diabetes is associated with an increased risk of cancer of colon, breast, liver, endometrium, and pancreas (2–5). Possible mechanisms for these associations include hyperinsulinemia, increased IGF-I, hyperglycemia, and inflammatory cytokines in diabetes (2,4,5).
Renal cell cancer accounts for 85% of kidney cancer, which is the 15th most common cancer in the world (6). Renal cell cancer is mainly a disease of high-income countries, and populations in North America and parts of Europe have 10 to 15 times higher prevalence than Asian and African populations (6). Nonetheless, the rates of renal cell cancer are increasing worldwide (6), and this global increase is not fully explained by improvements in detection of tumor (7). The large geographic variation in renal cell cancer rates suggests that westernization may contribute to its etiology. The Western diet and physical inactivity often result in obesity and insulin resistance, consequently leading to metabolic syndrome and type 2 diabetes. Obesity and hypertension are the most established risk factors for renal cell cancer (4,8,9), and both factors are linked to type 2 diabetes through insulin resistance and metabolic syndrome.
Therefore, we hypothesized that type 2 diabetes would be associated with an increased risk of renal cell cancer and interact synergistically with obesity and/or hypertension due to the common underlying mechanism of insulin resistance. Defining this association is important given the rising global epidemic of type 2 diabetes and also, to some extent, renal cell cancer, but evidence from previous studies has been unclear. Most investigations were case-control studies (8,10,11) although a few were prospective (9,12,13). In this study, we prospectively evaluated the association between type 2 diabetes and subsequent renal cell cancer risk in the Nurses’ Health Study.
RESEARCH DESIGN AND METHODS
Study population
The Nurses’ Health Study cohort was established in 1976 when 121,700 female registered nurses aged 30 to 55 years returned a mailed questionnaire about medical history and various risk factors for chronic disease. Follow-up questionnaires were sent every 2 years to update information on lifestyle factors and newly diagnosed diseases. Deaths in the cohort were identified by reports from family members in response to the follow-up questionnaires and from the National Death Index. In this study, women who reported renal cell cancer or any other cancer (except for nonmelanoma skin cancer) before baseline were excluded from analyses. The follow-up rate in this study population was 98%. The Nurses’ Health Study was approved by the institutional review board of Brigham and Women’s Hospital (Boston, MA).
Assessment of diabetes
On the baseline and subsequent biennial questionnaires, we asked the participants if and when they had ever been diagnosed with diabetes by a physician. All women who reported a diagnosis were mailed a supplementary questionnaire requesting additional information on symptoms, diagnostic tests, and treatments. Participants were considered to have type 2 diabetes if they met the National Diabetes Data Group criteria (14), were diagnosed at age 30 years or over, and did not meet the criteria for type 1 (insulin-dependent and ketosis-prone) diabetes. Women whose dates of diagnosis were unknown (n = 113) were excluded from analyses. We included women who had been diagnosed with type 2 diabetes either at baseline or during the follow-up period.
The validity of self-reported diabetes was investigated in a random sample of 62 women in this cohort. The diagnoses of type 2 diabetes were confirmed by medical record review for 98.4% of the women (15). In addition, another substudy assessing the prevalence of undiagnosed diabetes suggested a very low rate (0.5%) of false-negative results (15).
Ascertainment of renal cell cancer
Self-reported information on newly diagnosed kidney cancer was obtained on each biennial questionnaire. Participants (or next of kin on behalf of decedents) who reported a diagnosis of kidney cancer were asked for permission to access medical records. Physicians blinded to participants’ information reviewed medical records. Women whose diagnoses of kidney cancer were not confirmed by pathology reports were excluded from analyses (n = 115). Based on the World Health Organization classification (16), cases of renal cell cancer included clear cell, papillary, chromophobe, collecting duct carcinoma, and renal cell carcinoma unclassified. Renal pelvis or ureter cancer was not included due to a limited number of cases in this cohort.
Assessment of other risk factors
Information on body weight, smoking, history of hypertension, and parity has been updated every 2 years since 1976. BMI (in kg/m2) was calculated using height from 1976 and updated weight. Self-reported and measured weights were highly correlated (r = 0.97) in a validation study (17). For past and current smokers, pack-years of smoking were calculated by multiplying the duration and dose of smoking. Physician-diagnosed hypertension was self-reported, and its reliability was reported by a validation study (18). Parity was updated until 1996, when few childbirths were reported in this cohort. Information on alcohol consumption, fruit and vegetable intake, and physical activity was obtained from 1980.
Statistical analysis
Participants were followed up prospectively for the diagnosis of type 2 diabetes and incident renal cell cancer from 1976 to 2008. Person-years of follow-up were calculated from the date of return of the 1976 questionnaire to the date of renal cell cancer diagnosis, the date of death from any cause, or the end of follow-up (31 May 2008), whichever came first. We entered status of type 2 diabetes in the model as a time-dependent variable allowing the status to change during follow-up upon a new diagnosis. For women who had diabetes at baseline, person-years as diabetic were calculated from the beginning of the study (1976); women who developed diabetes during follow-up contributed person-years as nondiabetic while they were free of diabetes and as diabetic from the dates of diagnosis.
Cox proportional hazards regression models were used to calculate the hazard ratios (HRs) with 95% CIs. The proportionality assumption of Cox models was not violated. To control as finely as possible for confounding by age, calendar time, and any possible two-way interactions between these two time scales, we stratified the analysis jointly by age in months at start of follow-up and calendar year of the current questionnaire cycle. In the multivariate models, we additionally adjusted for potential confounders, including BMI (continuous), smoking status (never, past, current) and pack-years (continuous), history of hypertension (yes, no), and parity (nulliparous, 1–2, 3, 4, ≥5 children). In a secondary analysis beginning at the follow-up from 1980, we tested whether inclusion of additional covariates (race [white, nonwhite], alcohol consumption, fruit and vegetable intake, and physical activity) would alter the results.
Because insulin levels may vary at different stages of diabetes, we evaluated the risk of renal cell cancer depending on time since diagnosis of diabetes. Time since diagnosis was calculated from the date of diabetes diagnosis and categorized into 5-year intervals. Linear trend of renal cell cancer risk was tested among diabetic women using time since diagnosis as a continuous term (in month) in the model.
We conducted stratified analyses by levels of BMI (<30, ≥30 kg/m2), smoking status (never, ever), and history of hypertension (no, yes) because these are known risk factors of renal cell cancer and may be related to type 2 diabetes through insulin resistance and metabolic syndrome. Using the likelihood ratio test, the model including the interaction term for variables of interest was compared with the model with the main effect only. In addition, the combined effects of obesity (BMI ≥30 kg/m2), hypertension, and type 2 diabetes on the risk of renal cell cancer were evaluated. According to the number of combined conditions, participants were categorized into four subgroups (zero, one, two, or three conditions). Linear trend was examined by treating the number of combined conditions as a continuous term.
Finally, we assessed public health burden of prevalent obesity, hypertension, and type 2 diabetes by calculating population-attributable risk proportions.
Statistical tests were performed using SAS statistical software version 9.1 (SAS Institute, Cary, NC). All P values were two-tailed; P < 0.05 was considered statistically significant.
RESULTS
During 32 years of follow-up of 118,177 women (3,531,170 person-years), we documented 16,819 cases of type 2 diabetes (1,638 at baseline and 15,181 during follow-up) and 330 cases of incident renal cell cancer. Table 1 presents characteristics of the study population in 1990 (the midpoint of the follow-up period was chosen to best represent the overall follow-up). Women who reported type 2 diabetes had a substantially higher BMI and history of hypertension compared with nondiabetic women.
Table 1.
Age-standardized characteristics of study participants in 1990*
| Characteristic | No diabetes | Type 2 diabetes |
|---|---|---|
| Women (n) | 107,714 | 6,424 |
| Age, mean (years) | 56.8 | 57.0 |
| Duration of type 2 diabetes, mean (years) | — | 9.3 |
| White (%) | 96.9 | 94.3 |
| BMI, mean (kg/m2) | 25.5 | 30.5 |
| History of hypertension (%) | 28.8 | 63.4 |
| Current smokers (%) | 17.6 | 15.7 |
| Past smokers (%) | 37.9 | 38.7 |
| Pack-years of smoking, mean† | 24.2 | 25.7 |
| Alcohol intake (g/day) | 6.2 | 3.4 |
| Fruit intake (g/day) | 2.2 | 2.3 |
| Vegetable intake (g/day) | 2.8 | 2.8 |
| Physical activity, mean (METs) | 15.4 | 12.2 |
| Parity, mean (no. of children)‡ | 3.0 | 3.0 |
*Except for the data on mean of age, all data shown are age-standardized to the age distribution of study population;
†among current or past smokers only;
‡among parous women only.
Type 2 diabetes was associated with a significantly increased risk of renal cell cancer (Table 2). The age-adjusted HR was 2.22 (95% CI 1.67–2.95) for diabetic women compared with nondiabetic women. After additional adjustment for BMI and hypertension, the HR was attenuated to 1.61 (1.19–2.18). Further adjustment for smoking status, pack-years of smoking, and parity did not materially change the HR (1.60 [1.19–2.17]). Secondary analyses with additional adjustment for race, alcohol consumption, fruit and vegetable intake, and physical activity showed a similar HR of 1.61 (1.19–2.19). In all of the multivariate models, BMI and history of hypertension as well as type 2 diabetes were significantly associated with the risk of renal cell cancer. The results for either clear cell (n = 224) or nonclear cell (n = 106) were similar to the results for overall renal cell cancer (1.84 [1.30–2.60] for clear cell; 1.72 [1.01–2.96] for nonclear cell). When compared with nondiabetic women, diabetic women on any diabetic medication status (none, oral medications only, and insulin with or without oral medications) experienced higher HRs for renal cell cancer (1.81 [1.20–2.75], 1.51 [1.00–2.28], 1.29 [0.57–2.95], respectively). To exclude the possible cases of renal cell cancer preceding diabetes, we dropped five cases of cancer occurring within 2 years of diabetes diagnoses, and the increased risk was still significant (1.48 [1.08–2.02]).
Table 2.
History of type 2 diabetes and HRs of renal cell cancer among participants in the Nurses’ Health Study, 1976–2008
| No. of RCC cases | Person- years | Age-adjusted HR [95% CI] | Multivariate HR [95% CI]* | Multivariate HR [95% CI]† | |
|---|---|---|---|---|---|
| History of type 2 diabetes | |||||
| No | 270 | 3,303,773 | 1 (referent) | 1 (referent) | 1 (referent) |
| Yes | 60 | 227,397 | 2.22 [1.67–2.95] | 1.61 [1.19–2.18] | 1.60 [1.19–2.17] |
RCC, renal cell cancer.
*Adjusted for age in months, BMI (kg/m2, continuous), and hypertension (yes, no);
†adjusted for everything in *, and smoking status (never, past, current), pack-years of smoking (continuous), and parity (nulliparous, 1–2, 3, 4, ≥5 children).
The increased HRs of renal cell cancer were observed up to 15 years of duration of diabetes, and then the HR diminished (Ptrend = 0.01; Table 3). Diabetic women whose duration of diabetes was 5–10 years had the strongest HR of 2.07 (95% CI 1.28–3.36). When the analysis was confined to the incident diabetes during follow-up with 256 cases of renal cell cancer, similar association was observed (data not shown). Diabetic women had consistently higher cumulative incidence of renal cell cancer than nondiabetic women, and the cumulative incidence curves did not cross over the follow-up period (Supplementary Fig. 1).
Table 3.
Duration of type 2 diabetes and HRs of renal cell cancer
| No. of RCC cases | Person-years | Age-adjusted HR [95% CI] | Multivariate HR [95% CI]* | |
|---|---|---|---|---|
| Duration of type 2 diabetes | ||||
| No type 2 diabetes | 270 | 3,303,773 | 1 (referent) | 1 (referent) |
| ≤5 years | 21 | 75,151 | 2.46 [1.57–3.85] | 1.79 [1.13–2.83] |
| 5.1–10 years | 19 | 54,610 | 2.96 [1.85–4.74] | 2.07 [1.28–3.36] |
| 10.1–15 years | 12 | 38,954 | 2.66 [1.48–4.76] | 1.92 [1.06–3.47] |
| >15 years | 8 | 58,682 | 1.04 [0.51–2.11] | 0.78 [0.38–1.59] |
| Ptrend† | 0.02 | 0.01 |
RCC, renal cell cancer.
*Adjusted for age in months, BMI (kg/m2, continuous), hypertension (yes, no), smoking status (never, past, current), pack-years of smoking (continuous), and parity (nulliparous, 1–2, 3, 4, ≥5 children);
†calculated among women with type 2 diabetes using time since diagnosis of diabetes (months, continuous).
In stratified analyses by levels of BMI, history of hypertension, and smoking status, the positive associations between type 2 diabetes and renal cell cancer were consistent across different strata (Pinteraction ≥ 0.32).
In addition, combined effects of obesity, hypertension, and type 2 diabetes on the risk of renal cell cancer were observed (Fig. 1). Women who had both obesity and diabetes had a significantly increased risk of renal cell cancer than obese nondiabetic women (HR 1.92 [95% CI 1.26–2.91]). Compared with nonobese nondiabetic women, obese diabetic women had a HR of 2.34 (1.62–3.39); however, obese nondiabetic women did not show a significantly increased HR (1.22 [0.91–1.64]). Exclusion of women with BMI <18.5 kg/m2 did not alter the association (data not shown). Similarly, women who had both hypertension and diabetes had a higher HR of 1.71 (1.23–2.36) compared with women who had hypertension but no diabetes. When we considered the conditions of obesity, hypertension, and type 2 diabetes together, a higher number of comorbid conditions increased the risk of renal cell cancer with significant linear trend (Ptrend < 0.001). Women who had all three conditions showed a strikingly elevated risk than women without any comorbidity (HR 4.13 [95% CI 2.76–6.18]).
Figure 1.
Combined effects of type 2 diabetes, obesity, and hypertension on the risk of renal cell cancer in the Nurses’ Health Study, 1976–2008. Comorbid conditions include obesity (BMI ≥30 kg/m2), history of hypertension, and type 2 diabetes. HRs were derived from Cox proportional models adjusted for age in months, BMI (kg/m2, continuous), history of hypertension, smoking (status and pack-years), and parity (nulliparous, 1–2, 3, 4, 5+ children) as appropriate. Ptrend values are from two-sided Wald tests for linear trend. T2D, type 2 diabetes; HT, hypertension. *P < 0.01 with each referent of leftmost category. **P < 0.002.
Obesity, hypertension, and type 2 diabetes accounted for 31% (population-attributable risk) of incident renal cell cancer among this population of women.
CONCLUSIONS
In this large prospective study of women, type 2 diabetes was significantly associated with an increased risk of renal cell cancer. Moreover, the risk was dose dependently elevated with an increasing number of comorbid metabolic conditions.
Prior epidemiologic studies suggested some but inconclusive evidence for the relationship between diabetes and renal cell cancer. Most case–control studies reported no association (8,10,11). In the cohorts of hospitalized diabetic patients, the incidence rates of renal cell cancer were higher than in the general populations (12,13). Two general population cohort studies found no significant association (9,19). Some limitations of prior studies have hampered interpretation: sampling prevalent cases that are not ideal for etiologic research when prognosis of outcome is related to exposure (8,10,11), lack of generalizability (12,13), relatively short duration of follow-up given the slow proliferation and unknown latency of renal cell cancer (9,13), and failure to update diabetes status during follow-up (9,19).
Several underlying mechanisms might explain the link between diabetes and renal cell cancer. The first mechanism is hyperinsulinemia in type 2 diabetes. Insulin acts as a growth factor for tumor cell proliferation and stimulates IGF-1 production, which also plays a role in carcinogenesis (2,4,20). Growth factors might be important contributors for renal cell cancer development given its peculiar biologic characteristics (i.e., spontaneous regression of metastatic lesions after primary tumor excision) (21) and laboratory evidence (22). Second, hyperglycemia may affect carcinogenesis, since increased glucose metabolism is one of the central characteristics of malignant tissues (4,23). Third, renal hypertrophy, which develops in the earlier course of diabetes, might have implications in carcinogenesis, although pathogenic significance of this mechanical change is unclear (12). Finally, inflammatory cytokines, reactive oxygen, and lipid peroxidation are other possible mechanisms.
This study supports hyperinsulinemia as a plausible mechanism of renal cell cancer development with some evidence. First, comorbidity of obesity, hypertension, and type 2 diabetes elevated the risk of renal cell cancer dose dependently. All these conditions are the components of metabolic syndrome, and insulin resistance is underlying pathophysiology (20). Since individuals with multiple metabolic components are more closely related to hyperinsulinemia, our results support the insulin mechanism. Moreover, obese diabetic women had almost twofold higher risk of renal cell cancer than obese nondiabetic women, but the risk was not different between obese nondiabetic and nonobese nondiabetic women. This finding suggests that metabolic derangement such as hyperinsulinemia is more essential for cancer development. In addition, diabetes without obesity may mainly represent a failure of insulin secretion rather than insulin resistance, thus the lack of association between diabetes without obesity and renal cell cancer adds further support to the insulin mechanism. Second, increased risk was observed during the relatively early years of diabetes, but the risk plateaued in the later stages. Other recent studies also observed increased risks of colorectal and breast cancer during the early years of diabetes (24,25). This time-specific incidence pattern appears consistent with the natural course of hyperinsulinemia in type 2 diabetes. Typically, type 2 diabetes develops after long-term insulin resistance and compensatory hyperinsulinemia; then pancreatic β-cell failure eventually leads to hypoinsulinemia over many years (12,19). Nonetheless, considering the small number of cases of renal cell cancer after 15 years of diabetes in this cohort, the lack of association could be obtained by chance.
This study has several limitations. First, detection bias cannot be ignored because diabetic patients are more likely to be under enhanced surveillance for kidney complications. However, exclusion of the cancer cases within 2 years of diabetes diagnoses still resulted in a significant association. Second, despite a large cohort size, the number of cases in some subgroups (i.e., duration of diabetes ≥15 years) was small. Third, residual confounding could exist, although we adjusted for most of the important confounders. Finally, this study consisted of women and thus the results may not be generalized to men.
Strengths of this study include a prospective design and relatively large number of renal cell cancer cases. To our knowledge, this cohort provides the longest follow-up for the largest population of women in which the association between diabetes and renal cell cancer has been evaluated. We ascertained renal cell cancer with histological evidence. Self-reports of physician-diagnosed diabetes were highly accurate according to a validation study (15). This study examined the risk of renal cell cancer only in the diagnosed diabetic women, but misclassification as a result of undiagnosed diabetes should be low since we updated diabetes status biennially and the nurses in this study have a low rate of undiagnosed diabetes (15). We also updated the information on most of the established risk factors for renal cell cancer.
In conclusion, type 2 diabetes was independently associated with an elevated risk of renal cell cancer in this cohort of women. When combined with obesity and hypertension, the elevated risk of renal cell cancer is high. Future studies that focus on more direct measurement of hyperinsulinemia are warranted.
Supplementary Material
Acknowledgments
This study was supported by research grants CA-137764 and CA-87969 from the National Institutes of Health.
No potential conflicts of interest relevant to this article were reported.
H.-K.J. researched data, wrote and edited the manuscript, and contributed to discussion. W.C.W. and E.C. contributed to discussion and reviewed and edited the manuscript. H.-K.J. and E.C. had full access to all data in the study and take responsibility for the integrity of data and the accuracy of data analysis.
The authors thank Rong Tilney, Channing Laboratory, for computer support.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc11-0132/-/DC1.
References
- 1.Centers for Disease Control and Prevention. National Diabetes Surveillance System: prevalence of diabetes [Internet], 2009. Available from http://www.cdc.gov/diabetes/statistics/prev/national/figpersons.htm Accessed 17 April 2010
- 2.Calle EE, Kaaks R. Overweight, obesity and cancer: epidemiological evidence and proposed mechanisms. Nat Rev Cancer 2004;4:579–591 [DOI] [PubMed] [Google Scholar]
- 3.Giovannucci E. Metabolic syndrome, hyperinsulinemia, and colon cancer: a review. Am J Clin Nutr 2007;86:s836–s842 [DOI] [PubMed] [Google Scholar]
- 4.Xue F, Michels KB. Diabetes, metabolic syndrome, and breast cancer: a review of the current evidence. Am J Clin Nutr 2007;86:s823–s835 [DOI] [PubMed] [Google Scholar]
- 5.Giovannucci E, Harlan DM, Archer MC, et al. Diabetes and cancer: a consensus report. Diabetes Care 2010;33:1674–1685 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.World Cancer Research Fund/American Institute for Cancer Research Food, Nutrition, Physical Activity, and the Prevention of Cancer: a Global Perspective. Washington, DC, AICR, 2007 [Google Scholar]
- 7.Chow WH, Devesa SS, Warren JL, Fraumeni JF., Jr Rising incidence of renal cell cancer in the United States. JAMA 1999;281:1628–1631 [DOI] [PubMed] [Google Scholar]
- 8.Zucchetto A, Dal Maso L, Tavani A, et al. History of treated hypertension and diabetes mellitus and risk of renal cell cancer. Ann Oncol 2007;18:596–600 [DOI] [PubMed] [Google Scholar]
- 9.Setiawan VW, Stram DO, Nomura AM, Kolonel LN, Henderson BE. Risk factors for renal cell cancer: the multiethnic cohort. Am J Epidemiol 2007;166:932–940 [DOI] [PubMed] [Google Scholar]
- 10.Goodman MT, Morgenstern H, Wynder EL. A case-control study of factors affecting the development of renal cell cancer. Am J Epidemiol 1986;124:926–941 [DOI] [PubMed] [Google Scholar]
- 11.La Vecchia C, Negri E, Franceschi S, D’Avanzo B, Boyle P. A case-control study of diabetes mellitus and cancer risk. Br J Cancer 1994;70:950–953 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Lindblad P, Chow WH, Chan J, et al. The role of diabetes mellitus in the aetiology of renal cell cancer. Diabetologia 1999;42:107–112 [DOI] [PubMed] [Google Scholar]
- 13.Wideroff L, Gridley G, Mellemkjaer L, et al. Cancer incidence in a population-based cohort of patients hospitalized with diabetes mellitus in Denmark. J Natl Cancer Inst 1997;89:1360–1365 [DOI] [PubMed] [Google Scholar]
- 14.National Diabetes Data Group Classification and diagnosis of diabetes mellitus and other categories of glucose intolerance. Diabetes 1979;28:1039–1057 [DOI] [PubMed] [Google Scholar]
- 15.Hu FB, Li TY, Colditz GA, Willett WC, Manson JE. Television watching and other sedentary behaviors in relation to risk of obesity and type 2 diabetes mellitus in women. JAMA 2003;289:1785–1791 [DOI] [PubMed] [Google Scholar]
- 16.Lopez-Beltran A, Scarpelli M, Montironi R, Kirkali Z. 2004 WHO classification of the renal tumors of the adults. Eur Urol 2006;49:798–805 [DOI] [PubMed] [Google Scholar]
- 17.Rimm EB, Stampfer MJ, Colditz GA, Chute CG, Litin LB, Willett WC. Validity of self-reported waist and hip circumferences in men and women. Epidemiology 1990;1:466–473 [DOI] [PubMed] [Google Scholar]
- 18.Colditz GA, Martin P, Stampfer MJ, et al. Validation of questionnaire information on risk factors and disease outcomes in a prospective cohort study of women. Am J Epidemiol 1986;123:894–900 [DOI] [PubMed] [Google Scholar]
- 19.Washio M, Mori M, Khan M, et al. ; JACC Study Group Diabetes mellitus and kidney cancer risk: the results of Japan Collaborative Cohort Study for Evaluation of Cancer Risk (JACC Study). Int J Urol 2007;14:393–397 [DOI] [PubMed] [Google Scholar]
- 20.Zhou JR, Blackburn GL, Walker WA. Symposium introduction: metabolic syndrome and the onset of cancer. Am J Clin Nutr 2007;86:s817–s819 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Oya M. Renal cell carcinoma: biological features and rationale for molecular-targeted therapy. Keio J Med 2009;58:1–11 [DOI] [PubMed] [Google Scholar]
- 22.Stadler W, Vogelzang NJ. Human renal cancer carcinogenesis: a review of recent advances. Ann Oncol 1993;4:451–462 [DOI] [PubMed] [Google Scholar]
- 23.Jones SC, Saunders HJ, Qi W, Pollock CA. Intermittent high glucose enhances cell growth and collagen synthesis in cultured human tubulointerstitial cells. Diabetologia 1999;42:1113–1119 [DOI] [PubMed] [Google Scholar]
- 24.Flood A, Strayer L, Schairer C, Schatzkin A. Diabetes and risk of incident colorectal cancer in a prospective cohort of women. Cancer Causes Control 2010;21:1277–1284 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Michels KB, Solomon CG, Hu FB, et al. ; Nurses’ Health Study Type 2 diabetes and subsequent incidence of breast cancer in the Nurses’ Health Study. Diabetes Care 2003;26:1752–1758 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.