Abstract
OBJECTIVE
Increased oxidative stress (OS) and impaired anti-OS defenses are important in the development and persistence of insulin resistance (IR). Several anti-inflammatory and cell-protective mechanisms, including advanced glycation end product (AGE) receptor-1 (AGER1) and sirtuin (silent mating-type information regulation 2 homolog) 1 (SIRT1) are suppressed in diabetes. Because basal OS in type 2 diabetic patients is influenced by the consumption of AGEs, we examined whether AGE consumption also affects IR and whether AGER1 and SIRT1 are involved.
RESEARCH DESIGN AND METHODS
The study randomly assigned 36 subjects, 18 type 2 diabetic patients (age 61 ± 4 years) and 18 healthy subjects (age 67 ± 1.4 years), to a standard diet (>20 AGE equivalents [Eq]/day) or an isocaloric AGE-restricted diet (<10 AGE Eq/day) for 4 months. Circulating metabolic and inflammatory markers were assessed. Expression and activities of AGER1 and SIRT1 were examined in patients’ peripheral blood mononuclear cells (PMNC) and in AGE-stimulated, AGER1-transduced (AGER1+), or AGER1-silenced human monocyte-like THP-1 cells.
RESULTS
Insulin and homeostasis model assessment, leptin, tumor necrosis factor-α and nuclear factor-κB p65 acetylation, serum AGEs, and 8-isoprostanes decreased in AGE-restricted type 2 diabetic patients, whereas PMNC AGER1 and SIRT1 mRNA, and protein levels normalized and adiponectin markedly increased. AGEs suppressed AGER1, SIRT-1, and NAD+ levels in THP-1 cells. These effects were inhibited in AGER1+ but were enhanced in AGER1-silenced cells.
CONCLUSIONS
Food-derived pro-oxidant AGEs may contribute to IR in clinical type 2 diabetes and suppress protective mechanisms, AGER1 and SIRT1. AGE restriction may preserve native defenses and insulin sensitivity by maintaining lower basal OS.
Insulin action is regulated by multiple factors, including SIRT1, a member of the sirtuin (silent mating type information regulation 2 homolog) 1 family of NAD+ deacetylases, which acts via signaling mediators and transcription factors, including nuclear factor-κB (NF-κB), forkhead box class O, peroxisome proliferator–activated receptor-γ, and adiponectin (1–3). Because SIRT1 activity also modulates the functions of monocytes and macrophages, native defenses may play a key role in insulin resistance (IR), and type 2 diabetes (3,4). SIRT1 activity is decreased in diabetes (4,5), as is advanced glycation end product (AGE) receptor-1 (AGER1) (6). Because AGEs are oxidants that are normally controlled by AGER1 (7–9), decreased AGER1 may result in increased oxidative stress (OS) and inflammation (6). In addition, exposure to glycoxidants when AGER1 levels are reduced may have a negative effect on SIRT1, which could contribute to IR.
The increasing prevalence of IR and type 2 diabetes is directly related to the Western lifestyle and diet (10). Excessive intake of fats or carbohydrates is thought to play a major role in the development of IR (11,12), although a direct link has not been established. A clear relationship has been found between inflammation, OS, and IR (13). Therefore, because AGEs increase inflammation and OS in normal subjects, as well as in diabetic patients, they may also play a role in IR.
Glycoxidants are partially absorbed as food-derived AGE peptides and AGE lipids by mechanisms not fully elucidated (14). Experiments in animals have shown a strong link between high oral glycoxidant intake, IR, type 2 diabetes, and diabetes complications (15–18). Direct evidence that oral AGEs promote OS and cause metabolic changes was provided by studies of mice that were pair fed a low-AGE diet or the same diet supplemented with a well defined AGE (methylglyoxal [MG]-BSA) (16). An excess of AGEs led to OS, IR, and renal/vascular disease, whereas restriction of AGEs, without altering caloric or nutrient intake, reduced OS and inflammation, ameliorated IR, and extended the life span in mice (16). Clinical studies in healthy subjects, diabetic patients, and individuals with chronic kidney disease showed that AGE restriction substantially reduced OS and inflammation and improved native defenses, including AGER1 (9,19).
In the current study, we investigated the relationship between IR and dietary AGEs in type 2 diabetic patients. We report that AGE restriction lowers insulin levels, markers of IR, and inflammation. In addition, the suppressed expression and function of AGER1 and SIRT1 in diabetic peripheral blood mononuclear cells (PMNCs) are nearly normalized by AGE restriction, consistent with restoration of host defenses.
RESEARCH DESIGN AND METHODS
Study design
The study enrolled 18 type 2 diabetic patients (14 women, 4 men; average age, 61 ± 4 years), without renal disease or overt cardiovascular disease, and a usual diet rich in AGE (dietary AGE intake ∼>20 AGE equivalents [Eq]/day; Table 1). All study subjects continued to receive standard medical care: 20% were treated only with diet, and 80% received oral antidiabetic medications, including 15 with metformin and 1 each with pioglitazone, glipizide, and glimepiride; 60% were receiving statins and ACE inhibitors or angiotensin-receptor blockers, and 40% were taking aspirin (81 mg daily).
Table 1.
Baseline clinical characteristics and other parameters in the study population
| Variables | Diabetes |
Healthy |
|
|---|---|---|---|
| n = 18 | n = 18 | P | |
| Age (years) | 61 ± 4 | 67 ± 1 | 0.165 |
| Sex | NS | ||
| Male | 4 | 4 | |
| Female | 14 | 14 | |
| BMI (kg/m2) | 32.3 ± 1.6 | 27.3 ± 1.4 | 0.024 |
| Waist circumference (cm) | 108 ± 4 | 93 ± 4 | 0.013 |
| Fasting blood glucose (mg/dL) | 120 ± 14 | 84 ± 3 | 0.016 |
| Insulin (μU/mL) | 17 ± 1 | 8 ± 1 | 0.001 |
| HOMA-IR | 5.00 ± 0.51 | 1.66 ± 0.24 | 0.001 |
| Triglycerides (mg/dL) | 100 ± 11 | 80 ± 9 | 0.157 |
| HDL cholesterol (mg/dL) | 51 ± 3 | 72 ± 4 | 0.002 |
| Serum CML (units/mL) | 17.4 ± 1.1 | 12 ± 0.5 | 0.001 |
| Serum MG (nmol/mL) | 2.6 ± 0.10 | 1.1 ± 0.06 | 0.001 |
| Intracellular CML (units/mg) | 7.9 ± 1.8 | 5.7 ± 2.3 | 0.005 |
| Intracellular MG (nmol/mg) | 0.87 ± 0.28 | 0.70 ± 0.38 | 0.148 |
| 8-Isoprostane (pg/mL) | 234 ± 14 | 130 ± 11 | 0.033 |
| Plasma leptin (ng/mL) | 36 ± 3.6 | 15 ± 2.7 | 0.001 |
| Plasma adiponectin (µg/mL) | 7 ± 0.5 | 16 ± 2.6 | 0.004 |
| AGER1 (mRNA) | 133 ± 11 | 225 ± 28 | 0.011 |
| RAGE (mRNA) | 532 ± 77 | 464 ± 67 | 0.511 |
| SIRT1 (mRNA) | 282 ± 27 | 378 ± 27 | 0.029 |
| p66shc (mRNA) | 113 ± 20 | 66 ± 6 | 0.047 |
| NOX p47phox (mRNA) | 220 ± 24 | 125 ± 19 | 0.026 |
| TNF-α (ng/mg protein in PMNCs) | 18.5 ± 0.8 | 10 ± 0.5 | 0.001 |
| Caloric intake (kcal/day) | 2,329 ± 248 | 2,120 ± 215 | 0.934 |
| AGE intake (AGE Eq/day) | 23 ± 3 | 18 ± 1.3 | 0.135 |
| Creatinine clearance* | 92 ± 7 | 98 ± 4 | 0.431 |
Continuous data are expressed as mean ± SEM and categoric data as n. P values reflect differences between means of diabetic and healthy subjects at baseline. NS, not significant.
*Calculated as mL/min/1.73 m2.
They were randomly assigned to an AGE-restricted diet (n = 12) or their usual diet (n = 6) for 4 months. The AGE-restricted group received instructions on how to modify cooking time and temperature but not the quantity or nutrient composition of food. They were advised to boil, poach, stew, or steam food and to avoid frying, baking, or grilling, methods, which limit dietary AGE intake by ∼40–50% (9,19,20). The control group comprised 18 age-matched (age 67 ± 1.4 years), healthy volunteers selected from a larger well characterized cohort that was randomized to the same AGE-restricted diet for 4 months (9).
A dietitian monitored participants by telephone 1–2 times per week and at monthly clinic visits. The study diets were designed to maintain daily requirements of calories and nutrients in both arms but to restrict AGE intake only on the AGE-restricted arm. Nutritional intake was closely monitored in both groups.
The study and consent forms were approved by the Mount Sinai School of Medicine Institutional Review Board. All participants provided informed consent.
Human subjects
Participants received a physical examination and provided a fasting blood sample and a 24-h urine collection at baseline and at 4 months. Routine blood and urine tests were performed by the hospital clinical laboratory.
Dietary intake
Daily dietary AGE content, from 3-day food records that emphasized cooking methods, was estimated from a database that listed AGE values of ∼560 foods and was expressed as AGE equivalents/day (AGE Eq = 1,000 kilounits) (20). The 3-day food record is based on established guidelines developed to allow estimation of food and beverage consumption at home and away from home. The dietitian reviewed the record with the subject, probing for details on portion sizes and preparation methods, to ensure accuracy and compliance. Nutrient calculations were estimated by using the Food Processor 10.1 nutrient software program (ESHA Research, Salem, OR).
Assessment of AGEs, insulin, and inflammation
Derivatives of Nε-carboxymethyl-lysine (CML) and methylglyoxal (MG) in serum were quantified by established enzyme-linked immunosorbent assays (ELISAs) using monoclonal antibodies (4G9 and MG3D11) (9,21), validated against synthetic standards, CML-BSA (23 modified lysines/mol) and MG-BSA (20 MG-modified arginines/mol), based on high-performance liquid chromatography and gas chromatography-mass spectroscopy (21). Insulin was measured by an ELISA kit (ALPCO Diagnostics, Salem, NH). IR was estimated by the homeostasis model assessment (HOMA) index as [FI × (fasting glucose/22.5)], where FI is insulin in microunits per milliliterand fasting glucose is in millimoles per liter(9). ELISA kits were used for measuring plasma leptin, adiponectin (Millipore, Billerica, MA), and PMNC tumor necrosis factor (TNF)-α (Biosource International, Camarillo, CA).
PMNCs
PMNCs were separated from fasting, EDTA-anticoagulated blood by Ficoll-Hypaque Plus gradient (American Biosciences, Uppsala, Sweden) and used to isolate mRNA and protein (9,19). Total RNA was extracted by TRIzol (Invitrogen-Molecular Probes, Inc., Eugene, OR). The extracted RNA had an optical density of 280/260 ratio of between 1.8 and 2.0. Total RNA was reverse-transcribed using Superscript III RT (Invitrogen, Carlsbad, CA).
Cell culture and transient transfection
THP-1 human monocytes (1 × 106/mL) (American Type Culture Collection, Manassas, VA) were cultured in RPMI-1640 medium (1% FBS). THP-1 cells were transfected with AGER1, SIRT1 or short-hairpin RNA AGER1 (0.5 µg of DNA) by using the human monocyte cell line nucleofector kit (Amaxa Biosystems, Cologne, Germany). Quiescent cells were exposed to CML-BSA, MG-BSA, or BSA, with or without the following inhibitors: sirtinol (10 µmol/L; Calbiochem, La Jolla, CA); N-acetylcysteine ([NAC], 5 mmol/L; Sigma-Aldrich, St. Louis, MO); apocynin (300 µmol/L; Sigma-Aldrich); and Mn superoxide dismutase (1,000 units/mL; Sigma-Aldrich).
AGEs used for in vitro studies
Synthetic preparations of CML-BSA (23 CML-Lys/mol), MG-BSA (22 MG-Arg/mol) (21), and BSA (Fraction V; Sigma-Aldrich) were rendered LPS-negative before use by a Detoxigel column (Pierce, Rockford, IL), based on Limulus assay (BioWhittaker, Walkerville, MD).
Quantitative RT-PCR assay
AGER1, receptor for AGE (RAGE), the 66-kDa protein from the src homology and collagen homology domain (p66shc), SIRT1, and NADPH oxidase 1 (NOX) p47phox mRNA levels were assessed by quantitative SYBR Green real-time PCR (9). Primer sequences were as follows:
AGER1, forward primer 5′-CTGGGGCTCTTCATCTTCAG-3′, reverse primer 5′-GTTGCATCTCCCACAGAGGT-3′;
RAGE, forward primer 5′-AGGAGCGTGCAGAACTGAAT-3′, reverse primer 5′-TTGGCAAGGTGGGGTTATAC-3′;
p66shc, forward primer 5′-AGGAAGGGCAGCTGATGAT-3′, reverse primer 5′-GCGTGGGCTTATTGACAAAG-3′;
NOXp47phox, forward primer 5′-ACAGCGTCCGTTTTCTGC-3′, reverse primer 5′-AGCGGTTCAGGATGAGGTC-3′; and
SIRT1, forward primer 5′-CGGAAACAATACCTCCACCT-3′, reverse primer 5′-CACCCCAGCTCCAGTTAGAA-3′.
Emission from each sample was recorded during thermal cycling, and the raw fluorescence data were processed using Sequence Detection System software (Applied Biosystems, Carlsbad, CA) to produce threshold cycle (Ct) values for each sample. β-Actin and glyceraldehyde-3-phosphate dehydrogenase (GAPDH) housekeeping genes were used for internal normalization. The transcript copy number of target genes was determined based on their Ct values (9).
Western analysis and immunoprecipitation
Cell proteins were separated on 8% SDS-PAGE gels, transferred onto nitrocellulose (NT) membranes for probing with primary and secondary antibodies, and visualized by an enhanced chemiluminescence system (Roche, Mannheim, Germany) (7,18). For immunoprecipitation, the lysate (300 µg protein) was incubated overnight at 4°C with the appropriate antibody, followed by 60 μL protein A/G plus agarose beads (Santa Cruz Biotechnology, Santa Cruz, CA) for 2 h. Bound immune complexes in radioimmunoprecipitation assay lysis buffer were used for immunoblotting after SDS-PAGE and NT transfer (9).
NF-κB p65 acetylation
Cells (PMNCs, THP-1) were disrupted in lysis buffer (Sigma-Aldrich, C2978), and 100 µg protein was immunoprecipitated with anti-NF-κB-p65 (Santa Cruz Biotechnology) at 4°C overnight. A total of 60 µL protein agarose (A/G) beads were added, and immunoprecipitates were immunoblotted for acetyl-lysine residues (4). For densitometric analysis, acetyl-p65 was normalized for total p65.
NAD/NADH determination
NAD and NADH were measured using an Amplite Fluorimetric NAD/NADH assay kit (AAT Bioquest, Inc., Sunnyvale, CA). Cells (wild-type or AGER1-transfected) were lysed after stimulation with MG-BSA (60 µg/mL) for 72 h in the presence or absence of antioxidants NAC (5 mmol/L) and apocynin (300 µmol/L).
Statistical analysis
Data in the tables and figures are presented as means ± SEM. The Kolmogorov-Smirnov goodness-of-fit test was used to test for normal distribution. Variables not normally distributed were logarithmically converted for analyses. Differences of means between groups were analyzed by the Student t test or ANOVA, followed by the Bonferroni correction for multiple comparisons, depending on the number of groups. Correlation analyses were also examined by the Pearson correlation coefficient.
Significance of changes during the interventional study was assessed by comparing 1) change of means between baseline and end of study within each group by paired t test, 2) percentage of change from baseline to the end of the study between the AGE-restricted and the regular AGE diet groups by the Mann-Whitney test, and 3) differences between the means of both groups at the end of the study by unpaired t test. Significant differences were defined as a value of P < 0.05 and are based on two-sided tests. Data analysis was performed in consultation with a statistician, using SPSS 17.0 software (SPSS, Chicago, IL).
RESULTS
Baseline data
The type 2 diabetic patients, age- and sex-matched with nondiabetic control subjects, had similar levels of creatinine clearance (Table 1). Compared with healthy subjects, type 2 diabetic participants had significantly higher fasting blood glucose, plasma insulin, HOMA, BMI, waist circumference, serum CML (sCML), serum MG (sMG), and leptin but lower adiponectin. They also had significantly higher levels of serum AGEs and plasma 8-isoprostanes (Table 1).
AGER1 and SIRT1 mRNA levels in PMNCs from diabetic subjects were significantly lower than in healthy subjects (Table 1). Concentrations of pro-OS p66shc and NAPDH oxidase p47phox mRNA and TNF-α protein, a proinflammatory cytokine, were elevated, as were intracellular AGEs (iCML; Table 1). These data were consistent with high baseline OS.
Intervention data
Serum and plasma changes after AGE restriction.
AGE restriction (by 50%), without altering nutrient intake, led to markedly lower levels of sCML and sMG, as well as 8-isoprostanes in type 2 diabetic subjects (Table 2, Fig. 1A). Plasma insulin, HOMA, and leptin levels were also decreased by ∼30% below baseline by AGE restriction (Table 2, Fig. 1A). However, adiponectin levels were doubled after AGE restriction, resulting in a markedly lower leptin/adiponectin ratio (Fig. 1A, inset).
Table 2.
Intervention: Changes in biochemical, metabolic, and cellular parameters in diabetic patients and in healthy control subjects after AGE restriction
| Variable | Diabetic patients |
P‡ | P§ | |||||
|---|---|---|---|---|---|---|---|---|
| AGE-restricted diet (n = 12) |
Regular AGE diet (n = 6) |
|||||||
| Baseline | End | P* | Baseline | End | P† | |||
| sCML (units/mL) | 17.1 ± 1.3 | 11.6 ± 1.1 | 0.005 | 17.8 ± 2 | 24.2 ± 4 | 0.199 | 0.001 | 0.012 |
| sMG (nmol/mL) | 2.6 ± 0.2 | 1.8 ± 0.2 | 0.005 | 2.6 ± 0.2 | 3.5 ± 0.3 | 0.039 | 0.001 | 0.009 |
| iCML (units/mg) | 8.1 ± 0.9 | 6.5 ± 0.5 | 0.148 | 7.6 ± 0.3 | 10.5 ± 0.9 | 0.023 | 0.007 | 0.001 |
| iMG (nmol/mg) | 0.97 ± 0.10 | 0.52 ± 0.05 | 0.002 | 0.76 ± 0.12 | 1.08 ± 0.15 | 0.117 | 0.003 | 0.004 |
| AGER1 (mRNA) | 125 ± 15 | 193 ± 20 | 0.018 | 144 ± 16 | 97 ± 16 | 0.069 | 0.003 | 0.003 |
| RAGE (mRNA) | 530 ± 111 | 270 ± 70 | 0.064 | 467 ± 110 | 690 ± 109 | 0.179 | 0.002 | 0.018 |
| SIRT-1 (mRNA) | 268 ± 24 | 409 ± 53 | 0.040 | 300 ± 53 | 205 ± 38 | 0.176 | 0.007 | 0.010 |
| TNF-α (ng/mg) | 18 ± 1 | 14.4 ± 2 | 0.078 | 20 ± 2 | 26 ± 2 | 0.030 | 0.002 | 0.029 |
| Insulin (μU/mL) | 19 ± 1 | 12 ± 1.2 | 0.001 | 14 ± 1.7 | 19 ± 2 | 0.069 | 0.001 | 0.021 |
| FBG (mg/dL) | 114 ± 7 | 111 ± 9 | 0.801 | 131 ± 37 | 129 ± 26 | 0.970 | 0.205 | 0.688 |
| HOMA | 5.3 ± 0.4 | 3.4 ± 0.6 | 0.023 | 4.5 ± 1.2 | 6.2 ± 0.5 | 0.393 | 0.001 | 0.160 |
| HbA1c (%) | 6.4 ± 0.2 | 6.6 ± 0.4 | 0.347 | 6.7 ± 0.5 | 6.5 ± 0.4 | 0.770 | 0.089 | 0.656 |
| 8-Isoprostane (pg/mL) | 233 ± 17 | 141 ± 18 | 0.006 | 236 ± 25 | 313 ± 77 | 0.289 | 0.053 | 0.039 |
| Leptin (ng/mL) | 38 ± 0.6 | 26 ± 2.6 | 0.074 | 34 ± 5 | 52 ± 5 | 0.023 | 0.003 | 0.044 |
| Adiponectin (µg/mL) | 5.6 ± 0.6 | 10.4 ± 0.9 | 0.002 | 7.7 ± 0.7 | 4.6 ± 0.5 | 0.006 | 0.003 | 0.001 |
| Healthy control subjects | ||||||||
|---|---|---|---|---|---|---|---|---|
| AGE-restricted diet (n = 9) | Regular AGE diet (n = 9) | P‡ | P§ | |||||
| Baseline | End | P* | Baseline | End | P† | |||
| sCML (units/mL) | 12.4 ± 0.5 | 9.3 ± 1.0 | 0.016 | 11.7 ± 0.8 | 14.0 ± 1 | 0.168 | 0.002 | 0.012 |
| sMG (nmol/mL) | 1.1 ± 0.1 | 0.9 ± 0.1 | 0.049 | 1.0 ± 0.1 | 1.2 ± 0.1 | 0.330 | 0.026 | 0.052 |
| iCML (units/mg) | 5.5 ± 1.0 | 7.0 ± 1.2 | 0.366 | 5.9 ± 0.6 | 5.3 ± 0.7 | 0.502 | 0.186 | 0.256 |
| iMG (nmol/mg) | 0.63 ± 0.12 | 0.76 ± 0.18 | 0.538 | 0.75 ± 0.12 | 0.63 ± 0.12 | 0.514 | 0.137 | 0.552 |
| AGER1 (mRNA) | 226 ± 46 | 207 ± 45 | 0.767 | 224 ± 36 | 278 ± 43 | 0.345 | 0.137 | 0.270 |
| RAGE (mRNA) | 534 ± 133 | 372 ± 81 | 0.323 | 413 ± 65 | 628 ± 136 | 0.174 | 0.001 | 0.125 |
| SIRT1 (mRNA) | 383 ± 34 | 288 ± 100 | 0.388 | 368 ± 42 | 420 ± 169 | 0.783 | 0.686 | 0.634 |
| TNF-α (ng/mg) | 10.0 ± 1.3 | 8.4 ± 0.7 | 0.293 | 8.6 ± 0.6 | 11.8 ± 1 | 0.015 | 0.002 | 0.013 |
| Insulin (μU/mL) | 10.6 ± 1 | 11.3 ± 2.4 | 0.802 | 5.9 ± 1.1 | 7.4 ± 1.4 | 0.437 | 0.117 | 0.198 |
| FBG (mg/dL) | 86 ± 3 | 88 ± 6 | 0.710 | 83 ± 4 | 80 ± 4 | 0.509 | 0.785 | 0.259 |
| HOMA | 2.2 ± 0.3 | 2.5 ± 0.6 | 0.621 | 1.3 ± 0.3 | 1.5 ± 0.3 | 0.755 | 0.409 | 0.122 |
| 8-Isoprostane (pg/mL) | 135 ± 10 | 90 ± 9 | 0.006 | 125 ± 18 | 165 ± 23 | 0.198 | 0.002 | 0.014 |
| Leptin (ng/mL) | 16 ± 4 | 13 ± 4 | 0.675 | 14 ± 4 | 17 ± 6 | 0.673 | 0.386 | 0.634 |
| Adiponectin (µg/mL) | 16 ± 4 | 15.6 ± 4 | 0.882 | 16 ± 4 | 18 ± 3 | 0.698 | 0.102 | 0.683 |
Data are presented as mean ± SEM. FBG, fasting blood glucose.
*Statistical significance between baseline and end of study means in the AGE-restricted diet group.
†Statistical significance between baseline and end of study means in the regular AGE diet group.
‡Statistical significance in percentage change between baseline and end of study between the AGE-restricted diet and the regular diet groups.
§Statistical significance between the means of both groups at the end of the study.
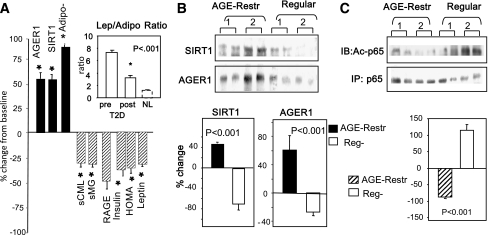
Figure 1.
A: AGE restriction reduces IR and improves inflammation in type 2 diabetic patients. Changes after AGE restriction (×4 months) in circulating factors (by ELISAs), plasma insulin, and HOMA, leptin, adiponectin, serum CML, MG, or in PMNCs, and AGER1, SIRT1, RAGE mRNA (by RT-PCR), are shown as percentage (mean ± SEM) above or below the baseline. *P < 0.050. Inset: Leptin (Lep)/adiponectin (Adipo) ratio before and after treatment is shown relative to normal control subjects (NL, at baseline, open bars). B: AGE restriction enhances SIRT1 and AGER1 protein expression in PMNCs of type 2 diabetic patients. PMNCs obtained at entry (1) and at the end of the study (2) are shown for subjects exposed to AGE restriction (AGE-Restr) vs. regular diet (Reg). SIRT1 and AGER1 protein levels were assessed by Western blotting (upper panels), followed by densitometric analysis (lower panels). C: AGE restriction enhances SIRT1 deacetylation of NF-κB p65. Levels of NF-κB p65 acetylation are shown at entry (1) and at the end of study (2) after immunoprecipitation (IP) and immunoblotting (IB) against acetyl-lysine residues. Data are shown as the percentage (mean ± SEM) change from entry (1). P values are as indicated.
Type 2 diabetic subjects on the regular diet showed no significant changes, except for higher sMG, iCML, leptin, and TNF-α values (Table 2), consistent with sustained high AGE intake and AGE accumulation. Neither the diabetic patients nor the healthy subjects had changes in weight (96.0 ± 7 to 97.3 ± 8 kg vs. 83.6 ± 6 to 82.0 ± 6 kg, respectively), BMI, plasma lipids, blood glucose, or HbA1c after 4 months. Healthy subjects on the AGE-restricted diet had no significant changes, with the exception of decreased sAGEs and 8-isoprostanes (Table 2).
PMNC changes in the AGE-restriction cohort.
The suppressed basal mRNA levels of AGER1 and SIRT1 in type 2 diabetic patients were increased by ∼50%, almost to the normal range in the AGE-restricted cohort (Fig. 1A; Table 2) (9). The changes in mRNA of AGER1 and SIRT1 correlated with changes in protein expression (Fig. 1B). Intracellular AGE levels in the AGE-restricted group were decreased, iMG (P = 0.002) and iCML (P = 0.148; Table 2), consistent with increased AGER1 expression.
There was also a reduction in NF-κB acetyl-p65 (Fig. 1C), associated with trends of lower RAGE mRNA and TNF-α protein in PMNCs from AGE-restricted type 2 diabetic subjects (Table 2). In contrast, in diabetic subjects who ate the regular diet, PMNC SIRT1 remained depressed (Fig. 1B and C; Table 2), whereas acetyl-p65, TNF-α, and RAGE remained elevated in diabetic subjects, consistent with higher circulating oxidants, AGEs, and 8-isoprostane (Table 2).
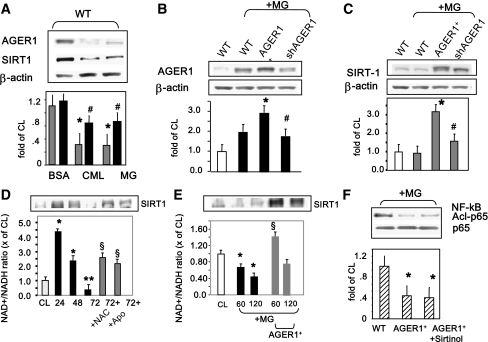
In vitro effects of AGEs on THP-1 AGER1 and SIRT1 expression and function
Because SIRT1 (4,23) and AGER1 (6–8) are suppressed in patients with diabetes (high OS), monocyte-like THP-1 cells were used as inflammatory cells to investigate the observations in PMNCs. AGER1 and SIRT1 protein expression levels were coordinately suppressed in THP-1 cells after chronic exposure to CML or MG (but not unmodified BSA; Fig. 2A). In addition, AGER1 and SIRT1 expression was enhanced in AGER1-overexpressing (AGER1+) cells treated with MG but reduced in AGER1-silenced THP-1 cells (Fig. 2B and C). After a transient induction, a marked time–dependent reduction of the NAD+/NADH ratio was noted in association with suppressed SIRT1 levels, and this effect was prevented by antioxidants (NAC, apocynin; Fig. 2D) and by AGER1 overexpression (AGER1+; Fig. 2E). In addition, the AGE-induced NF-κB p65 hyperacetylation seen in wild-type cells was blocked in AGER1+ cells (Fig. 2F), consistent with preserved SIRT1 function when AGER1 is intact. These data were in line with the PMNC findings from type 2 diabetic patients.
Figure 2.
AGEs suppress AGER1, SIRT1 protein, and NAD+ levels as well as NF-κB p65 deacetylation in THP-1 cells. A: Western blots (upper panels) and densitometry (lower panels) results are shown for AGER1 (black bars) and SIRT1 (gray bars) protein expression in THP-1 cells (wild-type [WT]) stimulated with CML-BSA (150 μg/mL), MG-BSA (60 μg/mL), and BSA (60 μg/mL) for 72 h. B and C: MG-induced effects on SIRT1 are AGER1-dependent. WT or THP-1 cells transfected with AGER1 (AGER1+) or short-hairpin RNA for AGER1 (shAGER1) were stimulated by MG (60 μg/mL) for 24 h before Western blots (upper panels) and densitometry plots (lower panels; AGER1, black bars; SIRT1, gray bars; WT, open bars). Data (mean ± SEM) of three to five experiments, derived from test/β-actin ratio, are shown as fold above control (cells alone, WT). *P < 0.001 vs. BSA or cells alone. #P < 0.002 vs. maximal values. D and E: AGE-induced effects on SIRT1 are NAD+-dependent and regulated by OS (D) and AGER1 (E). THP-1 cells were cultured with MG-BSA (60 μg/mL) or media (CL) for up to 72 h prior to Western blotting for SIRT1 (top inset) and NAD+/NADH ratio in the presence or absence of antioxidants (NAC or apocynin) in WT or AGER1+-transduced cells (E). NAD+/NADH ratio is shown as fold (mean ± SE) above control (n = 3, each in triplicate). *P < 0.001 vs. control. §P < 0.002 vs. maximal increase. F: NF-κB p65 hyperacetylation is induced by AGEs but is blocked by AGER1. Acetyl-p65 was determined in THP-1 cells, after MG stimulation (60 μg/mL) for 72 h in the presence or absence of SIRT1 inhibitor, sirtinol (10 μmol/L). Western blots and density plots are shown as mean ± SEM from four independent experiments. *P < 0.002 vs. nonstimulated or vs. nontransduced THP-1 cells.
CONCLUSIONS
IR remains an unresolved scientific and therapeutic problem. Increased OS and impaired anti-OS defenses are important factors in the development and persistence of IR (2–4). The current study shows that AGE restriction can improve IR in type 2 diabetes. Plasma insulin, markers of inflammation, and OS were substantially improved in diabetic subjects by an intervention that restricts oxidant (AGE) load without altering energy balance. These findings are consistent with evidence showing that excessive food AGEs promote inflammation and OS in humans (9,19) and IR in mice (15,16). That plasma insulin was nearly normalized after the AGE restriction indicates that tissue glucose uptake was improved. Therefore, a reduced demand on β-cells for insulin release appears to be directly related to the AGE restriction. While the findings must be confirmed in larger cohorts, AGE restriction may have therapeutic advantages in IR.
Although endogenous glucose or lipids contribute to elevated AGEs (22), exogenously AGE-modified nutrients are an important source in both human subjects and animals (9,14,16,19,20). The significant reduction in serum AGEs and lipid peroxides (8-isoprostanes) after AGE restriction in the current study confirms the hypothesis that elevated AGEs in type 2 diabetes result from increased dietary AGE intake, independently from glycemic control (19).
AGE restriction normalized AGER1, SIRT1, and SIRT1-dependent NF-κB p65 deacetylation levels, and there was a concomitant attenuation of proinflammatory mediators (i.e., RAGE and TNF-α) (9). The decreased basal AGER1 and SIRT1 (mRNA and protein) levels in type 2 diabetic PMNCs suggests a link between these two mechanisms. Since plasma insulin and leptin levels fell, whereas adiponectin levels increased with AGE restriction, the changes in AGER1 expression reflected adjustments in both the inflammatory and the metabolic states, effects previously attributed to SIRT1 (2–4,23). Thus, high AGE and low AGER1 levels in type 2 diabetes may partly account for the persistence of IR in these patients.
Given that downregulation of AGER1 (7–9) and SIRT1 is linked to high OS conditions (4,5), the current findings also indicate that normal SIRT1 function may depend on the ability of intact AGER1 to control AGEs and OS. Thus, the loss of AGER1 function may be one mechanism leading to SIRT1 downregulation in type 2 diabetes. This postulate is supported in the current study by the high basal levels of intracellular AGEs and low AGER1 levels in type 2 diabetic PMNC. The fact that these levels are nearly normalized after AGE restriction lends further support to this hypothesis. These data also suggest that low steady-state levels of intracellular AGEs may be crucial for maintaining AGER1 intact (7–9,16,24).
Because this was the first time that AGEs and AGER1 were linked to the deacetylases and to SIRT1, we probed these relationships in inflammatory monocyte–like THP-1 cells. After prolonged exposure to AGEs, AGER1 and SIRT1 were both suppressed in these cells or became unresponsive. AGEs acted via an OS-dependent decrease in NAD+, explaining the eventual downregulation of SIRT1, and consequently, the hyperacetylation of NF-κB p65 observed in diabetic PMNCs (2,4). Since the AGE-induced effects on SIRT1 and NF-κB were blocked in THP-1 cells by genetic modulation of AGER1 expression, AGER1 is likely to be involved in the regulation of inflammatory responses controlled by SIRT1. The data also suggest that controlling the pro-oxidant effects of AGEs could help preserve normal AGER1 and SIRT1 functions.
From a clinical perspective, AGE restriction markedly increased adiponectin levels and reduced the initially high leptin/adiponectin ratio, a marker of IR, indicating that AGEs also affect insulin-sensitive tissues (2–5). Adiponectin improves insulin sensitivity and is controlled by SIRT1 (25); therefore, the doubling in adiponectin levels after AGE-restriction provides another insight into the improved metabolic state in type 2 diabetic patients.
These data show that chronic exposure to excessive exogenous (food) oxidants fosters an impairment in both native antioxidant defenses as well as insulin action and that reducing oral AGEs can ameliorate these defects. This approach does not restrict energy or caloric intake. Since the effects of AGE restriction were additive to standard medical therapy, the intervention could be a valuable addition to the current management of patients with type 2 diabetes. Larger trials are warranted to validate the findings and establish the long-term effects of this intervention on diabetes.
Acknowledgments
This work was supported by MERIT grants AG-23188 and AG-09453 (to H.V.) and from the National Institutes of Health, National Institute of Research Resources (Grant M01-RR-00071) to the General Clinical Research Center at Mount Sinai School of Medicine for clinical and statistical support.
No potential conflicts of interest relevant to this article were reported.
J.U. researched the data and reviewed and edited the manuscript. W.C. researched the data and wrote, reviewed, and edited the manuscript. M.R. researched the data. S.G. researched the data and contributed to the discussion. R.P., X.C., and L.Z. researched the data. G.E.S. reviewed and edited the manuscript. H.V. designed the study, obtained support, researched the data, contributed to the discussion, and wrote, reviewed, and edited the manuscript.
Part of this study was submitted in abstract form to the 71st Scientific Sessions of the American Diabetes Association, 24–28 June 2011, San Diego, California.
References
- 1.Haigis MC, Sinclair DA. Mammalian sirtuins: biological insights and disease relevance. Annu Rev Pathol 2010;5:253–295 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Liang F, Kume S, Koya D. SIRT1 and insulin resistance. Nat Rev Endocrinol 2009;5:367–373 [DOI] [PubMed] [Google Scholar]
- 3.Olefsky JM, Glass CK. Macrophages, inflammation, and insulin resistance. Annu Rev Physiol 2010;72:219–246 [DOI] [PubMed] [Google Scholar]
- 4.de Kreutzenberg SV, Ceolotto G, Papparella I, et al. Downregulation of the longevity-associated protein sirtuin 1 in insulin resistance and metabolic syndrome: potential biochemical mechanisms. Diabetes 2010;59:1006–1015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cardellini M, Menghini R, Martelli E, et al. TIMP3 is reduced in atherosclerotic plaques from subjects with type 2 diabetes and increased by SirT1. Diabetes 2009;58:2396–2401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.He CJ, Koschinsky T, Buenting C, Vlassara H. Presence of diabetic complications in type 1 diabetic patients correlates with low expression of mononuclear cell AGE-receptor-1 and elevated serum AGE. Mol Med 2001;7:159–168 [PMC free article] [PubMed] [Google Scholar]
- 7.Lu C, He JC, Cai W, Liu H, Zhu L, Vlassara H. Advanced glycation end product (AGE) receptor 1 is a negative regulator of the inflammatory response to AGE in mesangial cells. Proc Natl Acad Sci U S A 2004;102:11767–11772 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Cai W, He JC, Zhu L, Lu C, Vlassara H. Advanced glycation end product (AGE) receptor 1 suppresses cell oxidant stress and activation signaling via EGF receptor. Proc Natl Acad Sci U S A 2006;103:13801–13806 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Vlassara H, Cai W, Goodman S, et al. Protection against loss of innate defenses in adulthood by low advanced glycation end products (AGE) intake: role of the antiinflammatory AGE receptor-1. J Clin Endocrinol Metab 2009;94:4483–4491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ford ES, Giles WH, Mokdad AH. Increasing prevalence of the metabolic syndrome among U.S. adults. Diabetes Care 2004;27:2444–2449 [DOI] [PubMed] [Google Scholar]
- 11.Riccardi G, Giacco R, Rivellese AA. Dietary fat, insulin sensitivity and the metabolic syndrome. Clin Nutr 2004;23:447–456 [DOI] [PubMed] [Google Scholar]
- 12.Malik VS, Popkin BM, Bray GA, Després JP, Hu FB. Sugar-sweetened beverages, obesity, type 2 diabetes mellitus, and cardiovascular disease risk. Circulation 2010;121:1356–1364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Shoelson SE, Lee J, Goldfine AB. Inflammation and insulin resistance. J Clin Invest 2006;116:1793–1801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Koschinsky T, He CJ, Mitsuhashi T, et al. Orally absorbed reactive glycation products (glycotoxins): an environmental risk factor in diabetic nephropathy. Proc Natl Acad Sci USA 1997;94:6474–6479 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Hofmann SM, Dong HJ, Li Z, et al. Improved insulin sensitivity is associated with restricted intake of dietary glycoxidation products in the db/db mouse. Diabetes 2002;51:2082–2089 [DOI] [PubMed] [Google Scholar]
- 16.Cai W, He JC, Zhu L, et al. Oral glycotoxins determine the effects of calorie restriction on oxidant stress, age-related diseases, and lifespan. Am J Pathol 2008;173:327–336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lin RY, Reis ED, Dore AT, et al. Lowering of dietary advanced glycation endproducts (AGE) reduces neointimal formation after arterial injury in genetically hypercholesterolemic mice. Atherosclerosis 2002;163:303–311 [DOI] [PubMed] [Google Scholar]
- 18.Zheng F, He C, Cai W, Hattori M, Steffes M, Vlassara H. Prevention of diabetic nephropathy in mice by a diet low in glycoxidation products. Diabetes Metab Res Rev 2002;18:224–237 [DOI] [PubMed] [Google Scholar]
- 19.Vlassara H, Cai W, Crandall J, et al. Inflammatory mediators are induced by dietary glycotoxins, a major risk factor for diabetic angiopathy. Proc Natl Acad Sci USA 2002;99:15596–15601 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Uribarri J, Woodruff S, Goodman S, et al. Advanced glycation end products in foods and a practical guide to their reduction in the diet. J Am Diet Assoc 2010;110:911–916, e12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cai W, Gao QD, Zhu L, Peppa M, He C, Vlassara H. Oxidative stress-inducing carbonyl compounds from common foods: novel mediators of cellular dysfunction. Mol Med 2002;8:337–346 [PMC free article] [PubMed] [Google Scholar]
- 22.Kilhovd BK, Juutilainen A, Lehto S, et al. High serum levels of advanced glycation end products predict increased coronary heart disease mortality in nondiabetic women but not in nondiabetic men: a population-based 18-year follow-up study. Arterioscler Thromb Vasc Biol 2005;25:815–820 [DOI] [PubMed] [Google Scholar]
- 23.Yoshizaki T, Milne JC, Imamura T, et al. SIRT1 exerts anti-inflammatory effects and improves insulin sensitivity in adipocytes. Mol Cell Biol 2009;29:1363–1374 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Torreggiani M, Liu H, Wu J, et al. Advanced glycation end product receptor-1 transgenic mice are resistant to inflammation, oxidative stress, and post-injury intimal hyperplasia. Am J Pathol 2009;175:1722–1732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Qiao L, Shao J. SIRT1 regulates adiponectin gene expression through Foxo1-C/enhancer-binding protein α transcriptional complex. J Biol Chem 2006;281:39915–39924 [DOI] [PubMed] [Google Scholar]