Abstract
OBJECTIVE
To determine the relationship between selected cytokines and diabetes in Chinese subjects.
RESEARCH DESIGN AND METHODS
Adult patients with recent-onset type 1 diabetes (n = 53), latent autoimmune diabetes in adults (LADA) (n = 250), and type 2 diabetes (n = 285) from multiple centers were compared with normal subjects (n = 196). We centrally tested serum GAD antibodies (GADAs), interleukin-6 (IL-6), lipocalin 2 (LCN2), high-sensitivity C-reactive protein (hs-CRP), and adiponectin.
RESULTS
After adjustment for age, sex, and BMI, all diabetes types had increased IL-6 and LCN2 (P < 0.01), and all four cytokines were increased in LADA (P < 0.01). In type 1 diabetes, adiponectin but not hs-CRP was increased (P < 0.01), whereas in type 2 diabetes, hs-CRP but not adiponectin was increased (P < 0.01). Adiponectin was correlated positively with GADA titer and negatively with hs-CRP (P < 0.01 for both).
CONCLUSIONS
In China, inflammatory markers are increased in all three major types of diabetes, but probably for different reasons, even in autoimmune diabetes.
Altered inflammatory mediators in diabetes could either reflect the cause of the disease or be secondary to metabolic derangements associated with diabetes. In type 2 diabetes, some cytokines (interleukin-6 [IL-6] and lipocalin 2 [LCN2]) are associated with insulin resistance (1) and others, such as serum high-sensitivity C-reactive protein (hs-CRP) and adiponectin, with cardiovascular risk (2,3). If these altered cytokines are secondary to the disease, then we should find them in diabetes, irrespective of type. If they are involved specifically in that disease process, then a specific profile of altered cytokine levels might be found in a particular type of diabetes. We hypothesized that a diabetes type–specific cytokine profile would be associated with autoimmune diabetes and, therefore, found in latent autoimmune diabetes in adults (LADA) and type 1 diabetes.
RESEARCH DESIGN AND METHODS
We studied cross-sectionally clinic- and hospital-based adult diabetic patients (aged >30 years) within 1 year from diagnosis. We ascertained subjects with LADA and type 2 diabetes from the LADA China multicenter study (46 hospitals throughout China contributed); type 1 diabetes, defined by WHO criteria (4), from the Type 1 Diabetes Collaboration Net (18 hospitals in Hunan Province); and normal subjects were screened by 75-g oral glucose tolerance test from 5,000 Chinese in a population-based study. Definition of LADA (5–7) was 1) GAD antibody (GADA) positive, 2) age >30 years at diagnosis, 3) independence from insulin treatment 6 months postdiagnosis, and 4) without ketoacidosis. Type 2 diabetic patients were GADA negative and noninsulin treated 6 months postdiagnosis. Subjects with hs-CRP >10 mg/L or taking anti-inflammatory drugs within 3 months were excluded. Metabolic syndrome was defined by National Cholesterol Education Program-Adult Treatment Panel III criteria (8). This study was approved by ethics committees at Second Xiangya Hospital of Central South University and at each center and conducted according to the Declaration of Helsinki. All participants provided written informed consent.
Height, weight, waist circumference, hip circumference, and blood pressure were recorded locally, and fasting sera samples were processed centrally. GADA was measured by radioligand assay (9). ELISA determined high-sensitivity IL-6 (IL-6 HS; R&D Systems, Minneapolis, MN), 7% intraassay and 5% interassay coefficient of variation (CV); LCN2 (10), 3.8–6.0% intraassay and 3.1–5.2% interassay CV; adiponectin (11) 5–6% intraassay and 6–8% interassay CV. Hs-CRP was measured by immunoturbidometric assay (Orine Diagnostica) with 2.1–3.3% intraassay and 3.4–4.6% interassay CV.
Statistical analysis
We used SPSS (version 13; SPSS, Chicago, IL) for statistical analysis. Data are expressed when normally distributed as means ± SD and when skewed as median (25th–75th percentiles). Logarithmic transformations were applied on non–normally distributed parameters before comparison. Frequency differences were compared using χ2 test. Variance analysis compared means by one-way ANOVA as appropriate. We used a general linear model of univariate analysis adjusted for age, sex, and BMI; log-transformed cytokine value was the dependent variable, different diabetes groups were fixed, and age, sex, and BMI were covariates (Fig. 1). Multivariate regression models investigated differences in log-transformed cytokine concentrations (dependent variables), with increasing number of variables (model 1: unadjusted; model 2: sex and age adjusted; model 3: age, sex, and BMI [independent variables] adjusted) (Supplementary Table 2). Linear relationships were evaluated by partial correlations test adjusted age, sex, and BMI. Data were not corrected for multiple comparisons and are descriptive; P < 0.01 was considered significant.
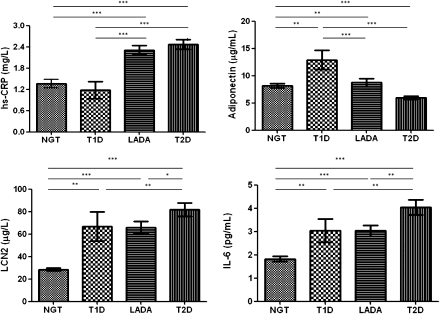
Figure 1.
Cytokine levels in subtypes of diabetes and normal subjects. Univariate of general linear model adjusted according to age, sex, and BMI between groups. *P < 0.05, **P < 0.01, ***P < 0.001. NGT, normal glucose tolerance subjects; T1D, type 1 diabetic subjects; T2D, type 2 diabetic subjects.
RESULTS
Results are shown in Supplementary Table 1. Of 784 subjects, patients with both LADA and type 2 diabetes were significantly older than subjects with normal glucose tolerance or type 1 diabetic patients. As expected, LADA patients had lower insulin secretion than type 2 diabetic patients, while in type 1 diabetic patients, insulin secretion was lower than in both LADA and type 2 diabetic patients. Metabolic syndrome in type 1 diabetic and control subjects was less frequent than in both LADA and type 2 diabetic subjects. We used univariate and multivariate regression models to adjust age, sex, and BMI differences (Fig. 1 and Supplementary Table 2). After adjustment, all three types of diabetes (type 1 diabetes, LADA, and type 2 diabetes) showed increased IL-6 and LCN2. All four cytokines were increased in LADA. In type 1 diabetes, adiponectin but not hs-CRP was increased. In type 2 diabetes, hs-CRP but not adiponectin was increased, and adiponectin was decreased after adjustment. GADA titer was positively correlated with adiponectin (r = 0.14, P < 0.01) and negatively correlated with hs-CRP (r = −0.15, P < 0.001) (Supplementary Tables 3 and 4). In LADA subjects, hs-CRP was strongly related to BMI (r = 0.363, P < 0.001).
CONCLUSIONS
Some inflammatory markers were increased in diabetes (i.e., IL-6 and LCN2) irrespective of diabetes type, implying that cytokine changes are secondary features of the disease independent of obesity, and consistent with a proinflammatory effect in diabetes in general. Nevertheless, obesity (waist-to-hip ratio) was associated with all four cytokines assayed, and the pattern of cytokine changes differed according to diabetes type.
Cytokines (IL-6, TNFα, and IL-1 receptor antagonist) in Europeans with these same major diabetes types were also positively associated with BMI, which was higher in diabetic patients than in control subjects and highest in type 2 diabetes but similar in LADA and type 1 diabetes; after correction, only TNFα in LADA and type 1 diabetes was no longer different from that in control subjects (5). In both the European study and this Chinese study, IL-6 showed remarkably similar increases in major diabetes types; IL-6, as well as LCN2, levels were higher than in control subjects and highest in type 2 diabetes (5). However, hs-CRP was increased in both LADA and type 2 diabetes, but not type 1 diabetes, while adiponectin was only increased in LADA and type 1 diabetes. Despite adiponectin being positively correlated with GADA titer, it has no established role in autoimmune diabetes and certainly cannot predict it (12). However, low-grade inflammation could be important in autoimmunity, potentially explaining any benefit of rosiglitazone (13). Indeed, each cytokine (IL-6, LCN2, hs-CRP, and adiponectin) was increased in Chinese LADA, though probably for different reasons (14). Given the relative lack of obesity in China, comparative Chinese and European studies could delineate the relative roles of obesity, diabetes, and autoimmunity on cytokines. Surprisingly, therefore, metabolic syndrome was prevalent in this large LADA cohort, in contrast to European studies (5,6). These results point toward a complex relationship between diabetes types and altered cytokine levels.
Supplementary Material
Acknowledgments
This study was supported by the European Foundation for the Study of Diabetes (EFSD) grant awards for collaborative diabetes research between China and Europe supported by Bristol-Myers Squibb Company, by the Aid Program for Science and Technology Innovative Research Team in Higher Educational Institutions of Hunan Province, and by the National Science Foundation grant for collaboration between Hong Kong and mainland China (30831160518). No other potential conflicts of interest relevant to this article were reported.
Y.X. researched data, wrote the manuscript, and contributed to discussion. P.Z. and X.L. researched data. G.H. researched data and contributed to discussion. Z.L. contributed to discussion. A.X. researched data, contributed to discussion, and reviewed and edited the manuscript. R.D.L and Z.Z. wrote the manuscript, contributed to discussion, and reviewed and edited manuscript.
Parts of this study were presented at the 70th Scientific Sessions of the American Diabetes Association, Orlando, Florida, 25–29 2010.
The authors thank investigators from the LADA China Study and from the Type 1 Diabetes Collaboration Net for collecting blood samples and data, and thank the subjects. The authors thank Zhihong Che of Central South University and Jialiang Zhang of University of Hong Kong for building ELISA assays, and Aimin Xu, University of Hong Kong, for LCN2 and adiponectin assay reagents. The authors thank Lily Ho-Le of Blizard Institute of Cell and Molecular Science for editing the manuscript.
Footnotes
This article contains Supplementary Data online at http://care.diabetesjournals.org/lookup/suppl/doi:10.2337/dc11-0039/-/DC1.
References
- 1.Esteve E, Ricart W, Fernández-Real JM. Adipocytokines and insulin resistance: the possible role of lipocalin-2, retinol binding protein-4, and adiponectin. Diabetes Care 2009;32(Suppl. 2):S362–S367 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Danesh J, Whincup P, Walker M, et al. Low grade inflammation and coronary heart disease: prospective study and updated meta-analyses. BMJ 2000;321:199–204 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Goldstein BJ, Scalia R. Adiponectin: A novel adipokine linking adipocytes and vascular function. J Clin Endocrinol Metab 2004;89:2563–2568 [DOI] [PubMed] [Google Scholar]
- 4.World Health Organization, Department of Noncommunicable Disease Surveillance. Definition, Diagnosis and Classification of Diabetes and its Complications: Report of a WHO Consultation. Part 1: Diagnosis and classification of diabetes Geneva, Switzerland, World Health Org., 1999, p. 1-59 [Google Scholar]
- 5.Pham MN, Hawa MI, Pfleger C, et al.; Action LADA Study Group. Pro- and anti-inflammatory cytokines in latent autoimmune diabetes in adults, type 1 and type 2 diabetes patients: Action LADA 4. Diabetologia. 24 February 2011 [Epub ahead of print] [DOI] [PubMed]
- 6.Hawa MI, Thivolet C, Mauricio D, et al. ; Action LADA Group Metabolic syndrome and autoimmune diabetes: action LADA 3. Diabetes Care 2009;32:160–164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Leslie RD. Predicting adult-onset autoimmune diabetes: clarity from complexity. Diabetes 2010;59:330–331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults: Executive summary of the Third Report of the National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III). JAMA 2006;285:2486–2497 [DOI] [PubMed] [Google Scholar]
- 9.Petersen JS, Hejnaes KR, Moody A, et al. Detection of GAD65 antibodies in diabetes and other autoimmune diseases using a simple radioligand assay. Diabetes 1994;43:459–467 [DOI] [PubMed] [Google Scholar]
- 10.Wang Y, Lam KSL, Kraegen EW, et al. Lipocalin-2 is an inflammatory marker closely associated with obesity, insulin resistance, and hyperglycemia in humans. Clin Chem 2007;53:34–41 [DOI] [PubMed] [Google Scholar]
- 11.Xu A, Yin S, Wong LC, Chan KW, Lam KSL. Adiponectin ameliorates dyslipidemia induced by the human immunodeficiency virus protease inhibitor ritonavir in mice. Endocrinology 2004;145:487–494 [DOI] [PubMed] [Google Scholar]
- 12.Truyen I, De Grijse J, Van Schravendijk C, et al. ; Belgian Diabetes Registry Adiponectin levels do not predict clinical onset of type 1 diabetes in antibody-positive relatives. Diabetologia 2007;50:2143–2146 [DOI] [PubMed] [Google Scholar]
- 13.Yang ZF, Zhou ZG, Li X, Huang G, Lin J. Rosiglitazone preserves islet beta-cell function of adult-onset latent autoimmune diabetes in 3 years follow-up study. Diabetes Res Clin Pract 2009;83:54–60 [DOI] [PubMed] [Google Scholar]
- 14.Kristiansen OP, Mandrup-Poulsen T. Interleukin-6 and diabetes: the good, the bad, or the indifferent? Diabetes 2005;54(Suppl. 2):S114–S124 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.