Abstract
Background
An estimated 136 000 concussions occur per academic year in high schools alone. The effects of repetitive concussions and the potential for catastrophic injury have made concussion an injury of significant concern for young athletes.
Purpose
The objective of this study was to describe the mechanism of injury, symptoms, and management of sport-related concussions using the High School Reporting Information Online (HS RIO) surveillance system.
Study Design
Descriptive epidemiology study.
Methods
All concussions recorded by HS RIO during the 2008–2009 academic year were included. Analyses were performed using SPSS software. Chi-square analysis was performed for all categorical variables. Statistical significance was considered for P < .05.
Results
A total of 544 concussions were recorded. The most common mechanism (76.2%) was contact with another player, usually a head-to-head collision (52.7%). Headache was experienced in 93.4%; 4.6% lost consciousness. Most (83.4%) had resolution of their symptoms within 1 week. Symptoms lasted longer than 1 month in 1.5%. Computerized neuropsychological testing was used in 25.7% of concussions. When neuropsychological testing was used, athletes were less likely to return to play within 1 week than those for whom it was not used (13.6% vs 32.9%; P < .01). Athletes who had neuropsychological testing appeared less likely to return to play on the same day (0.8% vs 4.2%; P = .056). A greater proportion of injured, nonfootball athletes had computerized neuropsychological testing than injured football players (23% vs 32%; P = .02)
Conclusion
When computerized neuropsychological testing is used, high school athletes are less likely to be returned to play within 1 week of their injury. Concussed football players are less likely to have computerized neuropsychological testing than those participating in other sports. Loss of consciousness is relatively uncommon among high school athletes who sustain a sport-related concussion. The most common mechanism is contact with another player. Some athletes (1.5%) report symptoms lasting longer than 1 month.
Keywords: concussion, sport-related concussion, mild traumatic brain injury, athletic injury, sports
Concussion is a common injury in high school sports. An estimated 136 000 concussions occur per academic year in high schools alone.12 Recently, there has been a renewed focus on this injury in both the medical and lay media. Several concerning issues have been raised. The potential for catastrophic outcomes, as described by Saunders and Harbaugh,25 has raised the level of concern. Cumulative effects resulting from repetitive injury have been described.5,13,22,23 Despite this, many high school athletes do not report their injuries.19 As there is currently no cure or well-documented treatment for sport-related concussion, efforts in clinical management are focused on the timing and strategies used for safe return to play.20,21
Increased interest has resulted in more medical publications over the last 9 years than all of the previous years combined.6 However, relatively little original data have been published. The epidemiology of concussion, symptoms of concussion, duration of symptoms, neurocognitive deficits, and duration of neurocognitive deficits have been reported previously, in certain sports or specific populations.4,8,9,10–12,14,17,29 This is the first report we are aware of to use a large, nationally representative sample of high school students from various sports to describe the mechanism of injury, symptoms, and certain aspects of the management of sport-related concussions.
METHODS
A total of 544 concussions were recorded in a sample of high school athletes using the High School Reporting Information Online (HS RIO) injury surveillance system. The HS RIO has been described previously in detail.7,24,26 Briefly, HS RIO is an Internet-based injury surveillance system that collects data on injuries in high school athletes participating in 9 sports: football, boys’ soccer, girls’ soccer, boys’ basketball, girls’ basketball, wrestling, baseball, volleyball, and softball. Schools are categorized according to the US Census geographic region (northeast, midwest, south, west) and size (≤1000 students or >1000 students). Schools are randomly chosen from each of these substrata to obtain 100 study schools. Certified athletic trainers affiliated with the National Athletic Trainers’ Association working at each of the schools record data weekly using the Internet-based data collection tool. Injuries were defined as those (1) resulting from participation in organized high school athletic practice or competition and (2) requiring medical attention from a certified athletic trainer. Data regarding sport played, date of injury, age, gender, level of competition, basic injury mechanism, type of symptoms, duration of symptoms, date returned to play, and use of computerized neuropsychological testing are collected. The diagnosis of concussion, the determination of recovery, and the protocol for returning an athlete to play were determined by the athletic trainers according to their usual practice. No definitions of “concussion” or “recovery” were imposed by us, as HS RIO is used for all sports injury surveillance, not only concussion. Institutions participating in HS RIO receive a participant incentive of $300 per year for entering data.
Concussions recorded during the 2008–2009 academic year were extracted from the database. Analyses were performed using SPSS software (version 16.0, SPSS Inc, Chicago, Illinois). Chi-square analysis was performed for all categorical variables. Statistical significance was considered for P < .05.
RESULTS
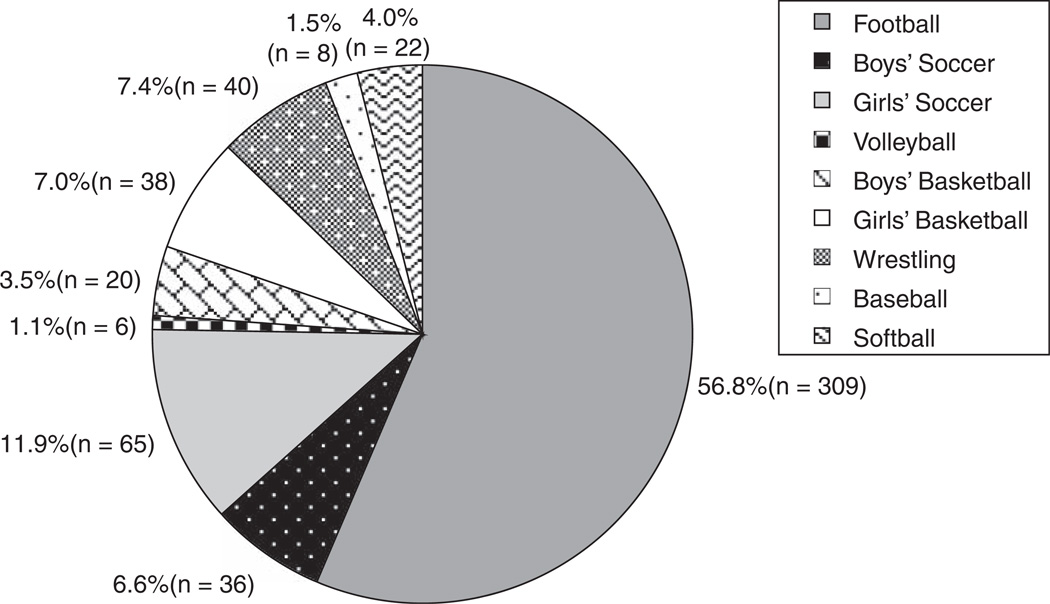
A total of 544 concussions were recorded by HS RIO over the 2008–2009 academic year. The injuries were evenly distributed by grade in school, with 24.8% occurring in freshmen, 24.4% in sophomores, 28.1% in juniors, and 22.6% in seniors. The majority of injuries (51.7%) were recorded in varsity athletes, with 30.1% occurring in junior varsity players and 13.8% in players on a freshman team. Most (68.5%) occurred during competition as opposed to practice. The concussion was the first reported concussion in 89.5%, while only 10.5% were recurrent injuries. Twenty-eight percent of the concussions occurred in 16-year-old athletes. Table 1 shows the distribution by age for the 518 injuries for which age was recorded. Figure 1 shows the distribution by sport and reveals that more than half of recorded concussions occurred during football.
TABLE 1.
Distribution of Concussion by Age Group
| Age, y | No. of Concussions | Percentage |
|---|---|---|
| 13 | 4 | 0.8 |
| 14 | 84 | 16.2 |
| 15 | 121 | 23.4 |
| 16 | 145 | 28.0 |
| 17 | 110 | 21.2 |
| 18 | 54 | 10.4 |
Figure 1.
Distribution of concussions by sport.
The basic injury mechanism was recorded for 521 (95.8%) of the concussions. The most common basic injury mechanism was contact with another player (76.2%), followed by contact with the playing surface (15.5%) and contact with a playing apparatus (7.7%). The specific type of contact was reported for 370 (93.2%) of the 397 concussions resulting from player-to-player contact. The most common type was head-to-head collisions (52.7%); 38.9% resulted from collisions between the head of the injured athlete and a different body part of another player, and 8.4% resulted from the injured athlete’s head striking the playing surface secondary to player-to-player contact.
Symptoms were recorded in 540 (99.3%) of the injuries; 93.4% of concussed athletes experienced a headache, while 24.3% had amnesia and only 4.6% had a loss of consciousness. Table 2 shows the percentage of concussed athletes experiencing each of the recorded symptoms. For 41 injuries (7.5%), symptoms were written in by hand under the heading “other.” Symptoms written in by hand included, “blurred vision,” “vomiting,” “feeling slowed down,” and “feeling in a fog,” among others.
TABLE 2.
Symptoms of Concussion Recorded by HS RIOa
| Symptom Recorded | No. of Concussions Resulting in Symptom |
Percentage of Concussions Resulting in Symptom |
|---|---|---|
| Headache | 508 | 93.4 |
| Dizziness/unsteadiness | 406 | 74.6 |
| Difficulty concentrating | 308 | 56.6 |
| Confusion/disorientation | 250 | 46.0 |
| Vision changes/sensitivity to light | 204 | 37.5 |
| Nausea | 157 | 28.9 |
| Drowsiness | 144 | 26.5 |
| Amnesia | 132 | 24.3 |
| Sensitivity to noise | 103 | 18.9 |
| Tinnitus | 58 | 10.7 |
| Irritability | 50 | 9.2 |
| Loss of consciousness | 25 | 4.6 |
| Hyperexcitability | 12 | 2.2 |
| Other | 41 | 7.5 |
Percentages do not total 100, as athletes could report more than 1 symptom. HS RIO, High School Reporting Information Online injury surveillance system.
Of the 530 concussions (97.4%) for which time to symptom resolution was recorded, 27.0% had resolution of their symptoms in less than 24 hours, 36.2% between 1 and 3 days, and 20.2% between 4 and 6 days. In 15.1% of players, symptoms lasted longer than 1 week, but resolved in less than a month; 1.5% had symptoms lasting longer than 1 month. Although it did not reach statistical significance (P = .12), athletes younger than 15 years of age appeared more likely to have symptoms lasting longer than 1 month.
In 132 injuries (25.7%), computerized neuropsychological testing was used to evaluate the athlete after the concussion.
Return-to-play data were collected for 520 (95.6%) of the injuries. Seventeen athletes (3.3%) were returned to play on the same day of their injury. The age of the athlete was not associated with the likelihood of returning to play on the same day of injury. When neuropsychological testing was used to assess the athlete after the injury, athletes were less likely to return to play in less than 1 week than those for whom neuropsychological testing was not used (13.6% vs 32.9%; P < .01). Similarly, athletes who had neuropsychological testing used to evaluate their concussions were less likely to return to play on the same day as their injury, although this finding did not quite reach statistical significance (0.8% vs 4.2%; P = .056). A greater proportion of injured, nonfootball athletes had computerized neuropsychological testing used in their care than injured football players (23% vs 32%; P = .02)
DISCUSSION
Computerized neuropsychological testing was used to assess 25.7% of concussions and correlated with the timing of return to play. Although it is now recognized as one of “the cornerstones of concussion evaluation,”3,20 routine neuropsychological testing in the setting of sports-related concussion is a relatively new concept.1,9 This is the first study, of which we are aware, to query the use of computerized neuropsychological testing in high school athletes using a large, nationally representative sample. Interestingly, those injured athletes evaluated with computerized neuropsychological testing were less likely to return to play on the same day, and less likely to return to play within a week of their injury. There are several possible explanations for this finding. It is possible that, despite reporting symptom resolution, these athletes had deficits in their neurocognitive function, adding further evidence to the benefit of neuropsychological testing in the management of sport-related concussion. Several previous studies have shown such a benefit.4,10,17,29 However, athletes’ neuropsychological test scores were not collected. Thus, this analysis could not be performed with the current data. Another possibility is that clinicians who use computerized neuropsychological testing are more conservative in their management, and thus are less likely to return athletes to play on the same day or within the same week as their injury. It is also possible that athletes deemed to have more severe injuries were more likely to receive neuropsychological testing.
Injured football players were less likely to have computerized neuropsychological testing during their evaluation than those athletes injured in other sports. Again, this may be interpreted in several different ways. Perhaps schools with limited financial resources are more likely to have football programs, given its popularity, than they are to have other sports. Similarly, they may not have the resources to purchase computerized test programs. Another possibility is that football programs may be reluctant to use computerized neuropsychological testing in the assessment of a concussion for fear that athletes may miss more playing time.
As with other studies, we found that most sport-related concussions sustained by high school athletes occur during games as opposed to practice,16 and headache is the most common symptom of concussion.14,16 Loss of consciousness is uncommon, occurring in less than 5% of concussions in our study. This is lower than reported by other investigators who examined high school athletes. Field et al11 noted loss of consciousness in 11% of high school athletes sustaining a sport-related concussion. In a different study of high school athletes, Collins et al8 reported 10% of concussed athletes experienced a loss of consciousness. One possible explanation for this difference in the percentage of concussions involving a loss of consciousness is a change over time in the understanding of sport-related concussion. Significant misunderstandings of this injury have been documented in youth coaches as recently as 2007, with 42% of coaches believing a concussion only occurs when an athlete loses consciousness.28 However, in a later study of parents of young rugby players published in 2009, 95% reported that a player need not be “knocked out” to have been concussed.27 The percentage of diagnosed concussions associated with a loss of consciousness is likely decreasing, as the athletic community learns that loss of consciousness is not necessary for concussion diagnosis.
Although the mechanism of concussion has been recorded in various sports such as soccer2 and American football,15,18,30 this is the first study we are aware of to record the specific mechanisms of injury in a large, representative, national sample of American high school athletes in various sports. We found that contact between 2 players’ heads, or between the head of the injured athlete and a different body part of another athlete, accounted for a much greater number of injuries than contact between the injured athlete’s head and the playing surface. Of particular interest is that, of the 101 concussions that occurred during soccer, none were due to contact with the ball when the athlete was purposefully heading the ball.
It has been suggested that younger athletes have longer recovery times than older athletes. Studies performed in high school athletes have revealed longer recovery times than those of college or professional athletes.11,17 Guskiewicz et al14 described symptom duration in National Collegiate Athletic Association football players, reporting that 88% had resolution of their symptoms within 1 week. In our study, 15.1% of students remained symptomatic for longer than 7 days, while 1.5% had symptoms lasting longer than 1 month. Within the limited age range of the high school population, significant associations between age and duration of symptoms were not seen in these 544 injuries. Although those athletes younger than 15 years of age appeared to be more likely to have symptoms lasting longer than 1 month, this finding did not reach statistical significance (P = .12).
This study has limitations, in addition to those mentioned in the above discussion. First, data are entered by athletic trainers working in the field at their respective institutions. Athletic trainers have their own individual threshold for diagnosis, management strategies, and return-to-play protocols. Therefore, the definition of “concussion,” the determination of recovery, and the approach to assessment and management could not be standardized for study purposes. As a result, however, the data represent what is actually occurring on a national level in US high schools. Second, as noted above, the neuropsychological test scores were not collected; thus, associations between neuropsychological testing, sport played, and return to play cannot be definitively interpreted.
CONCLUSION
When computerized neuropsychological testing is used in the evaluation of a concussion, high school athletes are less likely to be returned to play on the same day or within the same week as their injury. Injured football players are less likely to have computerized neuropsychological testing used in the evaluation of a concussion than those participating in other sports. Most concussions occur during player-to-player contact. Loss of consciousness is relatively uncommon among high school athletes who sustain a sport-related concussion. Of high school athletes who sustain a sport-related concussion, 15% report having symptoms lasting longer than 7 days, while 1.5% report symptoms lasting longer than 1 month.
Footnotes
The authors declared that they had no conflicts of interests in their authorship and publication of this contribution.
For reprints and permission queries, please visit SAGE’s Web site at http://www.sagepub.com/journalsPermissions.nav
REFERENCES
- 1.Alves WM, Rimel RW, Nelson WE. University of Virginia prospective study of football-induced minor head injury: status report. Clin Sports Med. 1987;6(1):211–218. [PubMed] [Google Scholar]
- 2.Andersen TE, Arnason A, Engebretsen L, Bahr R. Mechanisms of head injuries in elite football. Br J Sports Med. 2004;38(6):690–696. doi: 10.1136/bjsm.2003.009357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Aubry M, Cantu R, Dvorak J, et al. Summary and agreement statement of the First International Conference on Concussion in Sport, Vienna 2001: recommendations for the improvement of safety and health of athletes who may suffer concussive injuries. Br J Sports Med. 2002;36(1):6–10. doi: 10.1136/bjsm.36.1.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Broglio SP, Macciocchi SN, Ferrara MS. Neurocognitive performance of concussed athletes when symptom free. J Athl Train. 2007;42(4):504–508. [PMC free article] [PubMed] [Google Scholar]
- 5.Cantu RC. Chronic traumatic encephalopathy in the National Football League. Neurosurgery. 2007;61(2):223–225. doi: 10.1227/01.NEU.0000255514.73967.90. [DOI] [PubMed] [Google Scholar]
- 6.Cantu RC. Consensus statement on concussion in sport—the 3rd International Conference on Concussion, Zurich, November 2008. Neurosurgery. 2009;64(5):786–787. doi: 10.1227/01.NEU.0000348539.13887.D3. [DOI] [PubMed] [Google Scholar]
- 7.Centers for Disease Control and Prevention. Sports-related injuries among high school athletes—United States, 2005–06 school year. MMWR Morb Mortal Wkly Rep. 2006;55(38):1037–1040. [PubMed] [Google Scholar]
- 8.Collins MW, Field M, Lovell MR, et al. Relationship between postconcussion headache and neuropsychological test performance in high school athletes. Am J Sports Med. 2003;31(2):168–173. doi: 10.1177/03635465030310020301. [DOI] [PubMed] [Google Scholar]
- 9.Collins MW, Grindel SH, Lovell MR, et al. Relationship between concussion and neuropsychological performance in college football players. JAMA. 1999;282(10):964–970. doi: 10.1001/jama.282.10.964. [DOI] [PubMed] [Google Scholar]
- 10.Erlanger D, Saliba E, Barth J, Almquist J, Webright W, Freeman J. Monitoring resolution of postconcussion symptoms in athletes: preliminary results of a web-based neuropsychological test protocol. J Athl Train. 2001;36(3):280–287. [PMC free article] [PubMed] [Google Scholar]
- 11.Field M, Collins MW, Lovell MR, Maroon J. Does age play a role in recovery from sports-related concussion? A comparison of high school and collegiate athletes. J Pediatr. 2003;142(5):546–553. doi: 10.1067/mpd.2003.190. [DOI] [PubMed] [Google Scholar]
- 12.Gessel LM, Fields SK, Collins CL, Dick RW, Comstock RD. Concussions among United States high school and collegiate athletes. J Athl Train. 2007;42(4):495–503. [PMC free article] [PubMed] [Google Scholar]
- 13.Gronwall D, Wrightson P. Cumulative effect of concussion. Lancet. 1975;2(7943):995–997. doi: 10.1016/s0140-6736(75)90288-3. [DOI] [PubMed] [Google Scholar]
- 14.Guskiewicz KM, McCrea M, Marshall SW, et al. Cumulative effects associated with recurrent concussion in collegiate football players: the NCAA Concussion Study. JAMA. 2003;290(19):2549–2555. doi: 10.1001/jama.290.19.2549. [DOI] [PubMed] [Google Scholar]
- 15.Guskiewicz KM, Mihalik JP, Shankar V, et al. Measurement of head impacts in collegiate football players: relationship between head impact biomechanics and acute clinical outcome after concussion. Neurosurgery. 2007;61(6):1244–1252. doi: 10.1227/01.neu.0000306103.68635.1a. [DOI] [PubMed] [Google Scholar]
- 16.Guskiewicz KM, Weaver NL, Padua DA, Garrett WE., Jr Epidemiology of concussion in collegiate and high school football players. Am J Sports Med. 2000;28(5):643–650. doi: 10.1177/03635465000280050401. [DOI] [PubMed] [Google Scholar]
- 17.Lovell MR, Collins MW, Iverson GL, et al. Recovery from mild concussion in high school athletes. J Neurosurg. 2003;98(2):296–301. doi: 10.3171/jns.2003.98.2.0296. [DOI] [PubMed] [Google Scholar]
- 18.McCaffrey MA, Mihalik JP, Crowell DH, Shields EW, Guskiewicz KM. Measurement of head impacts in collegiate football players: clinical measures of concussion after high- and low-magnitude impacts. Neurosurgery. 2007;61(6):1236–1243. doi: 10.1227/01.neu.0000306102.91506.8b. discussion 1243. [DOI] [PubMed] [Google Scholar]
- 19.McCrea M, Hammeke T, Olsen G, Leo P, Guskiewicz K. Unreported concussion in high school football players: implications for prevention. Clin J Sport Med. 2004;14(1):13–17. doi: 10.1097/00042752-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 20.McCrory P, Johnston K, Meeuwisse W, et al. Summary and agreement statement of the 2nd International Conference on Concussion in Sport, Prague 2004. Br J Sports Med. 2005;39(4):196–204. doi: 10.1136/bjsm.2005.018614. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McCrory P, Meeuwisse W, Johnston K, et al. Consensus statement on concussion in sport: the 3rd International Conference on Concussion in Sport held in Zurich, November 2008. J Athl Train. 2009;44(4):434–448. doi: 10.4085/1062-6050-44.4.434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Omalu BI, DeKosky ST, Hamilton RL, et al. Chronic traumatic encephalopathy in a national football league player: part II. Neurosurgery. 2006;59(5):1086–1092. doi: 10.1227/01.NEU.0000245601.69451.27. discussion 1092–1093. [DOI] [PubMed] [Google Scholar]
- 23.Omalu BI, DeKosky ST, Minster RL, Kamboh MI, Hamilton RL, Wecht CH. Chronic traumatic encephalopathy in a National Football League player. Neurosurgery. 2005;57(1):128–134. doi: 10.1227/01.neu.0000163407.92769.ed. [DOI] [PubMed] [Google Scholar]
- 24.Rechel JA, Yard EE, Comstock RD. An epidemiologic comparison of high school sports injuries sustained in practice and competition. J Athl Train. 2008;43(2):197–204. doi: 10.4085/1062-6050-43.2.197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Saunders RL, Harbaugh RE. The second impact in catastrophic contact-sports head trauma. JAMA. 1984;252(4):538–539. [PubMed] [Google Scholar]
- 26.Shankar PR, Fields SK, Collins CL, Dick RW, Comstock RD. Epidemiology of high school and collegiate football injuries in the United States, 2005–2006. Am J Sports Med. 2007;35(8):1295–1303. doi: 10.1177/0363546507299745. [DOI] [PubMed] [Google Scholar]
- 27.Sullivan SJ, Bourne L, Choie S, et al. Understanding of sport concussion by the parents of young rugby players: a pilot study. Clin J Sport Med. 2009;19(3):228–230. doi: 10.1097/JSM.0b013e3181a41e43. [DOI] [PubMed] [Google Scholar]
- 28.Valovich McLeod TC, Schwartz C, Bay RC. Sport-related concussion misunderstandings among youth coaches. Clin J Sport Med. 2007;17(2):140–142. doi: 10.1097/JSM.0b013e31803212ae. [DOI] [PubMed] [Google Scholar]
- 29.Van Kampen DA, Lovell MR, Pardini JE, Collins MW, Fu FH. The “value added” of neurocognitive testing after sports-related concussion. Am J Sports Med. 2006;34(10):1630–1635. doi: 10.1177/0363546506288677. [DOI] [PubMed] [Google Scholar]
- 30.Viano DC, Casson IR, Pellman EJ. Concussion in professional football: biomechanics of the struck player, part 14. Neurosurgery. 2007;61(2):313–327. doi: 10.1227/01.NEU.0000279969.02685.D0. [DOI] [PubMed] [Google Scholar]