Abstract
Circumscribed choroidal hemangiomas are rare ophthalmic entities that cause diminution in vision due to accumulation of subretinal and/or intraretinal fluid in the macular area. Various treatment options ranging from conventional laser to photodynamic therapy have been employed to destroy the tumor and reduce the exudation; however, either the inability to penetrate through the exudative fluid or the collateral retinal damage induced by these treatment modalities make them unsuitable for lesions within the macula. We evaluated the role of intravitreal bevacizumab, a pan-vascular endothelial growth factor (VEGF) inhibitor, in reducing the sub- and intraretinal fluid in three patients with circumscribed choroidal hemangiomas. All the patients had complete resolution of the serous retinal detachment that was maintained till at least 12 months after the first injection. Intravitreal bevacizumab may be used in combination with thermal laser or photodynamic therapy in treating circumscribed choroidal hemangiomas with subretinal fluid.
Keywords: Bevacizumab, circumscribed choroidal hemangiomas, photodynamic therapy, transpupillary thermotherapy
Choroidal hemangiomas are benign vascular tumors that sometimes present with visual impairment due to cystoid macular edema (CME), exudative retinal detachment, retinal pigment epithelium alterations or subretinal fibrosis.[1,2] Circumscribed choroidal hemangiomas (CCH) are usually located in the macular and peripapillary region.[3] Various modalities like cryotherapy,[4] laser photocoagulation, plaque radiotherapy,[5] proton beam irradiation,[6] transpupillary thermotherapy (TTT),[7] and photodynamic therapy (PDT)[8] have been reported in literature for the treatment of CCH. Of late, bevacizumab has come up as a new treatment option in many retinal and choroidal vascular diseases.[9] In this report we present our long-term experience with three cases of CCH treated with intravitreal bevacizumab.
Case Reports
Case 1
A 35-year-old man presented with gradual diminution of vision in his right eye in October 2005. His best corrected visual acuity (BCVA) was 20/200 in the right eye and 20/20 in the left eye. On examination he was found to have CCH in the macular area with serous retinal detachment involving the fovea, which was confirmed with optical coherence tomography (OCT). As the patient could not afford PDT, TTT was performed. TTT was repeated in February 2006, with no improvement in the serous detachment and CME [Fig. 1a, b, and e). After taking informed written consent, 1.25 mg of bevacizumab (Avastin) was injected intravitreally and was repeated after six weeks. Three months later, his BCVA improved to 20/100, with a marked decrease in the serous detachment and CME on OCT. At the 12-month follow-up, fundus fluorescein angiography (FFA) demonstrated only staining, without any leakage, and BCVA was maintained at 20/100 [Fig. 1c, d, and f].
Figure 1.
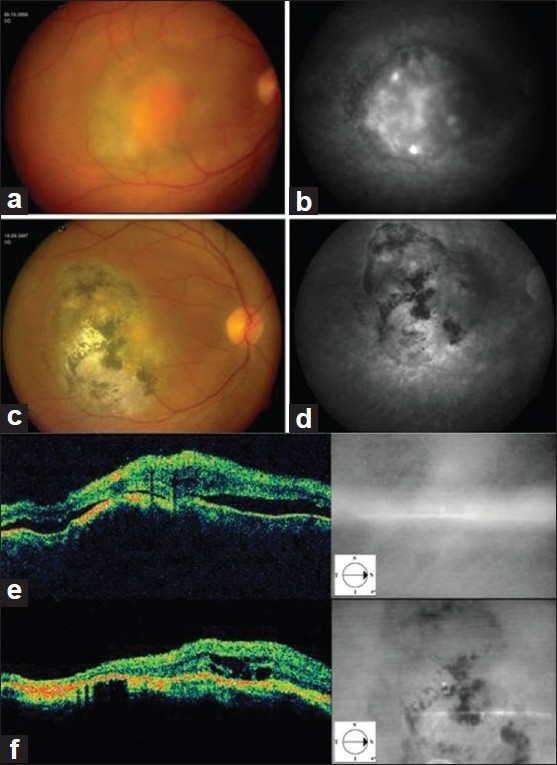
Circumscribed choroidal hemangioma temporal to the fovea in patient 1 (a). The FFA clearly delineates the hemangioma with leak into the surrounding subretinal space (b). Twelve months after the first intravitreal avastin injection, the fluid has completely resolved and the fovea is attached again (c). FFA shows staining at the hemangioma site, suggestive of an inactive lesion (d). OCT images pre (e) and 12 months post (f) the avastin injection. Resolution of serous detachment is complete, however, intraretinal cystic edema has persisted
Case 2
A 36-year-old man presented with gradual diminution of vision in his right eye since the past one month. His BCVA was 20/100 in the right eye and 20/20 in the left eye. On examination he was found to have CCH superotemporal to the fovea [Fig. 2]. As the lesion was extrafoveal, conventional laser photocoagulation was performed over the lesion. At the three-month follow-up, the patient had no improvement in BCVA, and FFA showed persisting leakage. OCT also demonstrated serous retinal detachment and CME. Intravitreal bevacizumab (1.25 mg) was injected twice, six weeks apart. Three months after the first injection his BCVA improved to 20/80, which was maintained at the 12-month follow-up. Similar to the previous case, OCT demonstrated a disappearance of the serous detachment, but showed persisting cystic changes, nasal to the fovea.
Figure 2.
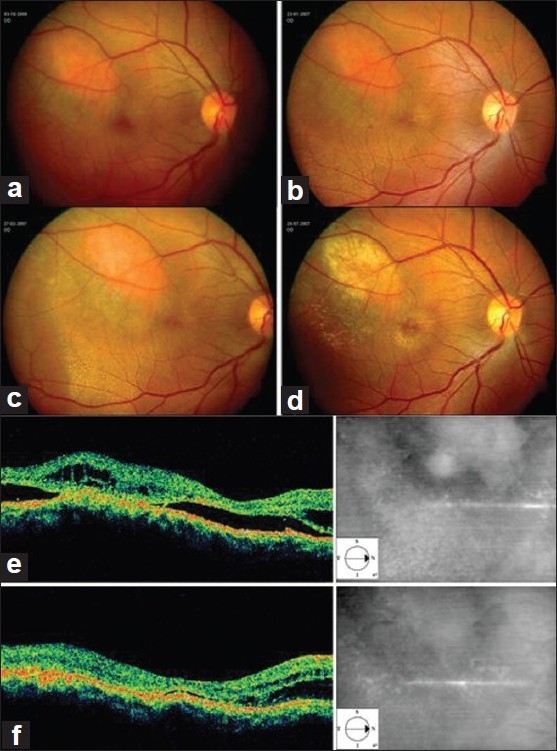
Pre-injection (a) and sequential post-injection (b, c, and d) photographs of a circumscribed hemangioma in patient 2, showing gradual resolution of the subretinal fluid from the macular area. OCT images before (e) and 12 months after the first avastin injection (f) show absence of subretinal fluid at the fovea, with persistence of intraretinal and a pocket of subretinal fluid in the extra-foveal region
Case 3
A 40-year-old man presented with gradual diminution of vision in his right eye for the past five months. His BCVA was hand movements close to face in the right eye and 20/20 in the left eye. On examination he was found to have a large CCH, superonasal to the disc. OCT demonstrated serous detachment and intraretinal cystic spaces involving the macula [Fig. 3a–c]. He was treated with intravitreal bevacizumab (1.25 mg) injection as the primary treatment. At six weeks BCVA was unchanged and OCT demonstrated the absence of the serous detachment [Fig. 3d], but persisting intraretinal cystic spaces [Fig. 3e]. A second intravitreal injection of bevacizumab (1.25 mg), in combination with conventional laser photocoagulation was performed at that time. At the 12-month follow-up, [Fig. 3c], there was no further improvement in BCVA.
Figure 3.
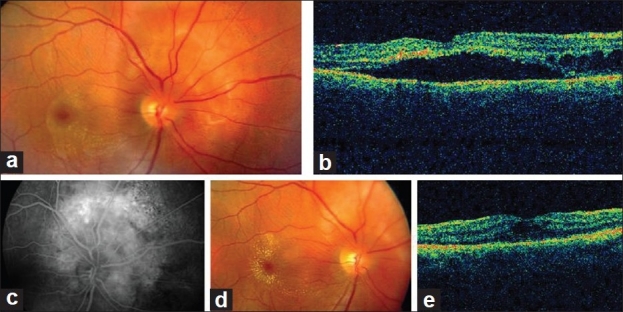
Large choroidal hemangioma located superonasal to the disc in patient 3 (a) with subretinal fluid and intraretinal cysts seen more nasally on the OCT line scan (b). The lesion shows a characteristic mottled appearance on angiography (c). At the six-month follow-up, post injection, the macular edema has disappeared with the consolidation of macular exudates (d). The 12-month OCT shows absence of any subretinal exudation although intraretinal cysts are still present (e)
Discussion
Circumscribed choroidal hemangiomas are composed of endothelial cell lined thin-walled vessels that rarely increase in size and may remain quiescent for months or years.[3] As a result, treatment is usually considered when the patient suffers from vision loss. Confluent laser photocoagulation probably causes tumor destruction and a decrease in the serous retinal detachment.[5] However, visual complications from intense photocoagulation have essentially ruled it out as a modality to treat CCH involving the macular area.[8] TTT has also been reported to decrease both tumor size and the associated exudation, but the visual benefits in treated patients have been disappointing.[7] PDT has been shown to cause atrophy of the hemangioma vessels, thereby decreasing the leakage and associated vision loss in a series of patients.[8] Although PDT is emerging as the treatment of choice for circumscribed choroidal hemangiomas, the high expenses involved, limit the number of patients that can afford it, particularly in developing countries. In addition, PDT may not provide the desired results in larger tumors as well as significantly high retinal detachments overlying the tumor mass, due to limited penetration of the laser beam.
An increasing number of articles have reported favorable anatomic and functional results following the use of intravitreal bevacizumab in various choroidal and retinal vascular pathologies.[9] Being a pan-VEGF inhibitor it causes both regression of abnormal vessels as well as reduction of leakage from them. As the vision loss in choroidal hemangiomas is usually caused by sub- as well as intraretinal accumulation of fluid rather than by the tumor itself, any treatment modality that causes resolution of the fluid for a prolonged period of time will lead to a better functional gain.[8] Sagong et al, have recently documented sustained improvement in visual acuity using intravitreal bevacizumab in three cases of CCH, with serous retinal detachment involving the fovea.[10] All three patients were given intravitreal injections within two weeks of decrease in vision and two patients further underwent PDT after one week, with good visual recovery and restoration of normal foveal architecture. In our series, the first injection of bevacizumab was administered after the macula had been detached for at least five months, due to either delayed presentation by the patient or initial treatment failure with conventional laser or TTT. Although there was complete resorption of the subretinal fluid in these patients, the intraretinal cystic changes were still present on the last visit, suggesting irreversible anatomic and functional damage to the fovea, precluding restoration of near normal visual acuity.
In conclusion, the results of the three patients treated so far suggest that intravitreal bevacizumab can cause complete resolution of leakage from a choroidal hemangioma that is sustained for a significant period. It may be used as a primary mode of treatment, especially for subfoveal lesions, or as a means to decrease the height of the overlying fluid so as to make laser photocoagulation or TTT more effective in extra foveal tumors. Further studies with larger number of patients and longer follow-up are required to confirm these findings.
References
- 1.Anand R, Augsburger JJ, Shields JA. Circumscribed choroidal hemangiomas. Arch Ophthalmol. 1989;107:1338–42. doi: 10.1001/archopht.1989.01070020408045. [DOI] [PubMed] [Google Scholar]
- 2.Augsburger JJ, Shields JA, Moffat KP. Circumscribed choroidal hemangiomas: Long-term visual prognosis. Retina. 1981;1:56–61. [PubMed] [Google Scholar]
- 3.Witschel H, Font RL. Hemangioma of the choroid: A clinicopathologic study of 71 cases and a review of the literature. Surv Ophthalmol. 1976;20:415–31. doi: 10.1016/0039-6257(76)90067-9. [DOI] [PubMed] [Google Scholar]
- 4.Humphrey WT. Choroidal hemangioma: Response to cryotherapy. Ann Ophthalmol. 1979;11:100–4. [PubMed] [Google Scholar]
- 5.Madreperla SA, Hungerford JL, Plowman PN, Laganowski HC, Gregory PT. Choroidal hemangiomas: Visual and anatomic results of treatment by photocoagulation or radiation therapy. Ophthalmology. 1997;11:1773–8. doi: 10.1016/s0161-6420(97)30027-x. [DOI] [PubMed] [Google Scholar]
- 6.Zografos L, Egger E, Bercher L, Chamot L, Munkel G. Proton beam irradiation of choroidal hemangiomas. Am J Ophthalmol. 1998;128:261–8. doi: 10.1016/s0002-9394(98)00150-0. [DOI] [PubMed] [Google Scholar]
- 7.Garcia-Arumi J, Ramsay LS, Guraya BC. Transpupillary thermotherapy for circumscribed choroidal hemangiomas. Ophthalmology. 2000;107:351–6. doi: 10.1016/s0161-6420(99)00046-9. [DOI] [PubMed] [Google Scholar]
- 8.Madreperla SA. Choroidal hemangioma treated with photodynamic therapy using verteporfin. Arch Ophthalmol. 2001;119:1606–10. doi: 10.1001/archopht.119.11.1606. [DOI] [PubMed] [Google Scholar]
- 9.Mandal S, Garg S, Venkatesh P, Mithal C, Vohra R, Mehrotra A. Intravitreal bevacizumab for subfoveal idiopathic choroidal neovascularization. Arch Ophthalmol. 2007;125:1487–92. doi: 10.1001/archopht.125.11.1487. [DOI] [PubMed] [Google Scholar]
- 10.Sagong M, Lee J, Chang W. Application of intravitreal bevacizumab for circumscribed choroidal hemangiomas. Korean J Ophthalmol. 2009;23:127–31. doi: 10.3341/kjo.2009.23.2.127. [DOI] [PMC free article] [PubMed] [Google Scholar]


