Abstract
A 16 year old girl presented with irritation and watering of the right eye for 3 months. On examination, the superior perilimbal sclera was ectatic with incarcerated uveal tissue covered by conjunctiva. The conjunctiva showed discreet, yellow white mucoid spots. Excision biopsy of the conjunctiva showed subepithelial spherules of sporangia containing numerous endospores, suggestive of rhinosporidiosis. Diathermy was applied to flatten the staphyloma. The ectatic area was covered with a corneal patch graft. The patient was started on prednisolone acetate eye drops and oral dapsone for 6 months. Corneal graft was well incorporated and conjunctivalized by 3 months. Since the graft was not seen within the palpebral aperture, there was good cosmetic result. The corneal graft had the added advantage of transparency which allowed visualization of the underlying tissue to diagnose early recurrence. There was no recurrence at 6 months.
Keywords: Rhinosporidiosis, scleral melt, tectonic graft
Rhinosporidiosis is an infection primarily affecting the mucous membranes of the nose and eye, caused by Rhinosporidium seeberi. It was regarded as a sporozoan by Malbran in 1892, as a protozoan by Seeber and as a phycomycete by Ashworth in 1923. Through molecular biological analysis of the ribosomal DNA, Herr et al, classified the organism into a new clade named Mesomycetozoa.[1]
The presumed mode of infection is from the aquatic habitat, through traumatized epithelium most commonly at nasal sites.[2]
About 10% of cases of rhinosporidiosis are ocular, involving the bulbar and palpebral conjunctiva.[3,4] Bulbar conjunctival involvement in ocular rhinosporidiosis has been seen in 0%, 7.3% and 12.4% of cases.[5–7] There have been 12 cases of scleral ectasia associated with bulbar conjunctival involvement described in the literature.[7–12]
The definitive diagnosis is by microbiological scrapings and histopathological examination of resected tissues.[5,9] This article describes a rare presentation of oculosporidiosis with scleral ectasia and the use of a corneal graft as a mode of treatment.
Case Report
A 16 year old girl with no contributory medical illness presented with irritation and watering of the right eye for 3 months. She had noticed a progressively increasing black mass above her right cornea. There was a history of minor trauma with a stick, 6 months prior to presentation. There was no history of pain, redness, discharge or sudden increase in the size of the mass. There was no history of similar masses elsewhere in the body.
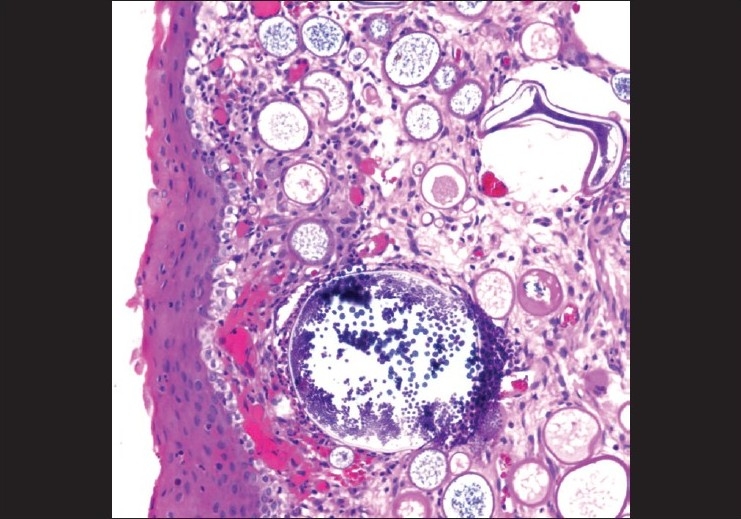
Best corrected visual acuity was 20/40 (R) with +1.5 diopter sphere (Ds) and 20/20 (L). Elevation of the right eye was mildly restricted and the eye was hypotropic. She did not complain of diplopia. Other ocular movements were normal. Her cornea was clear. The superior perilimbal area showed ectatic sclera measuring 8 × 10 mm with incarceration of uveal tissue. The overlying conjunctiva showed dilated vessels and multiple small, discrete, yellowish white mucoid spots on the surface [Fig. 1]. Rest of the anterior segment and fundus was normal. Lacrimal fossa showed no visible mass and syringing of the nasolacrimal duct was normal. Left eye examination was normal. Keratometry was not done. Clinical examination and rigid nasal endoscopy of the nasal cavity showed normal nasal mucosa with no lesions.
Figure 1.

Preoperative photograph showing spherules of rhinosporidiosis in the superior bulbar conjunctiva with staphyloma
The history of trauma with a vegetative matter, absence of other conditions associated with ectatic degenerations of sclera and the possibility of white spots being spores pointed to a probable diagnosis of ocular rhinosporidiosis. Hence, she was advised conjunctival biopsy and patch graft over the staphyloma.
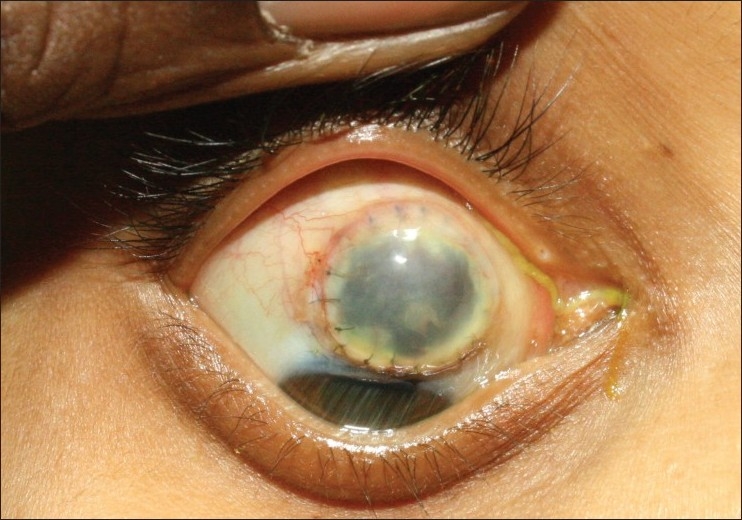
Intraoperatively, the involved conjunctiva was excised with a 1 mm margin except at the limbus where it was cut flush. The ectatic uveal tissue was heat cauterized to cause scarring and flattening. A 11 mm corneal button was used as a tectonic graft after scraping the endothelium and sutured onto healthy sclera with 8-0 nylon. The corneal epithelium was scraped and the surrounding conjunctiva was draped over it after mobilizing it by blunt dissection. Histopathological examination of the excised conjunctiva showed variably sized subepithelial spherules of sporangia containing numerous endospores. There was a mild nongranulomatous reaction of lymphocytes and plasma cells [Fig. 2] which confirmed the diagnosis. Since history, ocular and general examination did not point to any underlying autoimmune disease, no further investigations were done.
Figure 2.
Photomicrograph of the conjunctival biopsy illustrating multiple subepithelial spores filled sporangia of varied sizes associated with a mild chronic inflammatory cell response (H and E, ×200)
Postoperatively, she was given topical prednisolone acetate 1% and cycloplegics. Based on the biopsy report, oral dapsone 100 mg for 6 days in a week for 6 months was started. The steroid drops were gradually tapered. She was reviewed at the end of the week after 1, 3 and 6 months interval [Figs. 3 and 4]. The patient was from a different country and did not come for follow-up after 6 months.
Figure 3.
Six months postoperative photograph with good visualization of the underlying uveal tissue showing no macroscopic recurrence
Figure 4.

Six months postoperative face photograph with good cosmesis
At the third month review, she was asymptomatic and had good cosmetic result and the best corrected visual acuity with +1.00 Ds/–3.5 diopter cylinder (Dcx) 70° was 6/12. The decreased vision in the right eye can be explained by anisometropic amblyopia. The restriction of elevation and hypotropia persisted. The palpebral aperture of the right eye was narrower than the left. The conjunctival epithelium had grown over the graft and the underlying uveal tissue was clearly visible through it. There was no recurrence of rhinosporidiosis.
Discussion
The typical lesion of conjunctival rhinosporidiosis is a freely mobile, pink, sessile or pedunculated lesion. Attachment is usually at the fornices or tarsal conjunctiva. The surface of the polyps is covered with multiple, discrete, grayish white subepithelial cyst-like inclusions.[8]
Scleral melting in the vicinity of the conjunctival lesion is rare, and the pathologic basis for this is unclear. Scleral ectasia with staphyloma formation was noted in this clinical presentation, unlike the classic presentation of a conjunctival polyp. The patient described here was a young woman in good health with no history of rheumatoid arthritis. The fellow eye was normal. There was no nasal focus of infection or history suggestive of contact with infected water other than the history of minor trauma with a branch, prior to onset of the lesion. Recurrence after excision of the conjunctival mass in rhinosporidiosis has been described in different case series.[4,5]
Common differential diagnoses of scleral staphylomata in a quiet eye include scleromalacia perforans, hyaline plaques and spontaneous intercalary perforation.
Scleral thinning over a large area does not allow direct approximation of the edges. The ectatic area predisposes the eye to injury and infection. Thus, there is need for a patch graft over the area. Grafts like buccal mucosa, periosteum, cartilage and fascia lata require an additional surgical procedure other than the ocular procedure. Donor scleral grafts have the advantages of being easily available, strong and easily preservable.[13] However, they are known to become necrotic and melt if there is active inflammation.[14] Amniotic membrane has been used in conjunction with scleral patch grafts when there is associated conjunctival deficiency.[15] This has the advantage of promoting reepithelialization and reduces the chance of scleral melt. However, amniotic membrane alone lacks the tensile strength to support the staphylomatous defect and gets absorbed with time.[16]
Using cornea as a patch graft would allow early visualization of recurrences at the bed of the resected polyp. Conjunctival epithelium can easily grow over a deepithelialized corneal surface. Surrounding episcleral vessels can grow into the corneal graft and allow it to be easily incorporated into the area. This report highlights the value of a corneal patch graft in a rare case of conjunctival rhinosporidiosis with scleral ectasia. On review after 3 and 6 months, the resected bed could be clearly seen with no evidence of recurrence. Complete epithelialization was achieved with good tectonic integrity. There was good cosmetic result and the graft could not be seen in the primary position of gaze.
Conjunctival rhinosporidiosis causing scleral staphyloma is a rare clinical entity. Diagnosis requires a high index of suspicion. Pathological evaluation of the excised lesion confirms the diagnosis. It is important to differentiate this treatable condition from other causes of scleral staphyloma in a quiet eye. The use of corneal patch graft has dual advantages of transparency and tectonic integrity. Using this surgical option compared to a scleral patch graft in areas of the bulbar conjunctiva that are not in the palpebral aperture, would provide good cosmesis, tectonic integrity and allow visualization of early recurrences.
References
- 1.Herr RA, Ajello L, Taylor JW, Arseculeratne SN, Mendoza L. Phylogenetic analysis of Rhinosporidium seeberi's 18S small-subunit ribosomal DNA groups this pathogen among members of the protoctistan Mesomycetozoa clade. J Clin Microbiol. 1999;37:2750–4. doi: 10.1128/jcm.37.9.2750-2754.1999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Karunaratne WA. The pathology of rhinosporidiosis. J Path Bact. 1934;XLII:193–202. [Google Scholar]
- 3.Cohen J, Carvalho RC, Guimarães R, Cruz AA. Oculosporidiosis. Arch Ophthalmol. 1997;115:1340–1. doi: 10.1001/archopht.1997.01100160510030. [DOI] [PubMed] [Google Scholar]
- 4.Arora R, Ramachandran V, Raina U, Mehta DK. Oculosporidiosis in Northern India. Indian Pediatr. 2001;38:540–3. [PubMed] [Google Scholar]
- 5.Shrestha SP, Hennig A, Parija SC. Prevalence of rhinosporidiosis of the eye and its adnexa in Nepal. Am J Trop Med Hyg. 1998;59:231–4. doi: 10.4269/ajtmh.1998.59.231. [DOI] [PubMed] [Google Scholar]
- 6.Pe'er J, Gnessin H, Levinger S, Averbukh E, Levy Y, Polacheck I. Conjunctival oculosporidiosis in east Africa caused by Rhinosporidium seeberi. Arch Pathol Lab Med. 1996;120:854–8. [PubMed] [Google Scholar]
- 7.Kuriakose ET. Corneal Transplantation in scleral staphylomas. Indian J Ophthalmol. 1981;29:411–3. [PubMed] [Google Scholar]
- 8.De Doncker RM, de Keizer RJ, Oosterhuis JA, Maes A. Scleral Melting in a patient with Conjunctival Rhinosporidiosis. Br J Ophthalmol. 1990;74:635–7. doi: 10.1136/bjo.74.10.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Castelino AM, Rao SK, Biswas J, Gopal L, Madhavan HN, Kumar SK. Conjunctival Rhinosporidiosis Associated with Scleral Melting and Staphyloma formation: Diagnosis and Management. Cornea. 2000;19:30–3. doi: 10.1097/00003226-200001000-00007. [DOI] [PubMed] [Google Scholar]
- 10.Sunderraj P. Scleral melting and conjunctival rhinosporidiosis. Br J Ophthalmol. 1992;76:191. doi: 10.1136/bjo.76.3.191-a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Kuriakose ET. Oculorsporidiosis. Br J Ophthalmol. 1963;47:346–9. doi: 10.1136/bjo.47.6.346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.John SS, Mohandas SG. Conjunctival oculosporidiosis with scleral thinning and staphyloma formation. Indian J Ophthalmol. 2005;53:272–4. doi: 10.4103/0301-4738.18912. [DOI] [PubMed] [Google Scholar]
- 13.Ozcan AA, Bilgic E, Yagmur M, Ersöz TR. Surgical management of scleral defects. Cornea. 2005;24:308–11. doi: 10.1097/01.ico.0000141228.10849.17. [DOI] [PubMed] [Google Scholar]
- 14.Sangwan VS, Jain V, Gupta P. Structural and functional outcomes of scleral patch grafts. Eye. 2007;21:930–5. doi: 10.1038/sj.eye.6702344. [DOI] [PubMed] [Google Scholar]
- 15.Hanada K, Shimazaki J, Shimmura S, Tsubota K. Multilayered amniotic membrana transplantation for severe ulceration of cornea and sclera. Am J Ophthalmol. 2001;131:324–31. doi: 10.1016/s0002-9394(00)00825-4. [DOI] [PubMed] [Google Scholar]
- 16.Ma DH, Wang SF, Su WY, Tsai RJ. Amniotic Membrane Graft for the Management of Scleral Melting and Corneal Perforation in Recalcitrant Infectious Scleral and Corneoscleral Ulcers. Cornea. 2002;21:275–83. doi: 10.1097/00003226-200204000-00008. [DOI] [PubMed] [Google Scholar]


