Abstract
Sub acute left-sided bacterial endocarditis is a serious condition that may be overlooked due to highly variable clinical manifestations. We present the case of a 45-year-old man who presented with complaints of fullness in his abdomen and splenomegaly that referred to the surgery clinic. He underwent diagnostic splenectomy. 3 month after splenectomy endocarditis was diagnosed. We recommend echocardiography in the work up of isolated splenomegaly.
Keywords: Echocardiography, endocarditis, splenomegaly
INTRODUCTION
Infective endocarditis (IE) is an infection of the endocardial surface of the heart. IE also produces a wide variety of systemic signs and symptoms through several mechanisms, including both sterile and infected emboli and various immunological phenomena.[1] Subacute left-sided bacterial endocarditis is a serious condition that may be overlooked due to highly variable clinical manifestations. We present the case of a 45-year-old man who presented with complaints of fullness in his abdomen and was referred to a surgeon.
CASE REPORT
A 45-year-old man presented to the surgery clinic with a 30-day history of fullness in the abdomen. The patient had poor appetite and fatigue and denied any history of trauma, autoimmune disease, peptic ulcer, or any gastrointestinal (GI) problem, sweating, allergies, any other medical conditions or weight loss. A symptomatic review of the cardiopulmonary, gastrointestinal, and genitourinary systems was unremarkable. He did not smoke or use illicit drugs or alcohol and had not traveled recently; further, there have been no changes in his daily routine. The patient had never had any major surgery and did not consume any drug but his history demonstrated acute renal failure two months ago because of which he underwent dialysis via jugular catheter. Kidney was recovered and the patient discharged in a good condition with normalisation of creatinine.
On physical examination, the patient appeared asthenic, and had no respiratory distress or jaundice. His Glasgow Coma Scale score was 15. A detailed cranial nerve examination demonstrated no abnormalities, and funduscopy was normal. The patient's neck was supple, and his cerebellar function tests were normal. His blood pressure was 130/80 mm Hg, and heart rate was regular, ie, 80 bpm. The respiratory rate was 16 breaths/min, and he was afebrile, with a recorded temperature of 36.7°C. His heart sounds were muffle. The lungs were clear on auscultation, and his abdomen was soft and non-tender. But spleen was 4 cm under costal margin, and hepatomegaly or lymphadenopathy was not detected. Motor and sensory examination of all four limbs was normal.
A workup of the patient was initiated. A complete blood cell count, chest X-ray, liver enzymes examination, thyroid function test, malaria smear, kala-azar, infectious mononucleosis Ab, anti-nuclear factor, Coomb's test, blood cultures, Serology for HIV, hepatitis and other infections, electrocardiogram, and urinalysis all showed normal findings. Only rheumatoid factor was positive. Electrolytes and creatinine were normal. Abdominal sonography was performed and it was normal (no portal hypertension, splenic or portal vein thrombosis) except for splenomegaly. MRI Chest/Abdomen, upper GI endoscopy was performed and was normal. A bone marrow aspiration and biopsy was done for him, which was normal. Because of progressively enlarged splenomegaly, the patient underwent diagnostic splenectomy. In pathology examination, no specific finding or abscess was noted. The patient was discharged though he did not feel well. Three months after splenectomy, the patient had chest pain and was referred to a cardiologist. On physical examination, the patient appeared asthenic; he had a grade 3/6 diastolic murmur in the aortic area and conjunctival haemorrhage. Two-dimensional echocardiography was done and showed oscillating hypermobile mass (vegetation) on aortic valve and severe aortic regurgitation [Figure 1]. Coronary angiography was normal; patient was referred to a cardiac surgeon. Blood cultures were negative. Our patient presented with one major criterion and three minor criteria, thus satisfying the Duke criteria [2] for definite endocarditis. An emergency operation was performed after the diagnosis. Findings at operation included phlegmon on the aortic valve leaflets with anterior leaflet perforation. The valve was replaced with a St Jude prosthetic valve. The patient was discharged from the hospital after he recovered well from surgery. In the culture of the valve, Streptococcus viridans was present [Figure 2].
Figure 1.
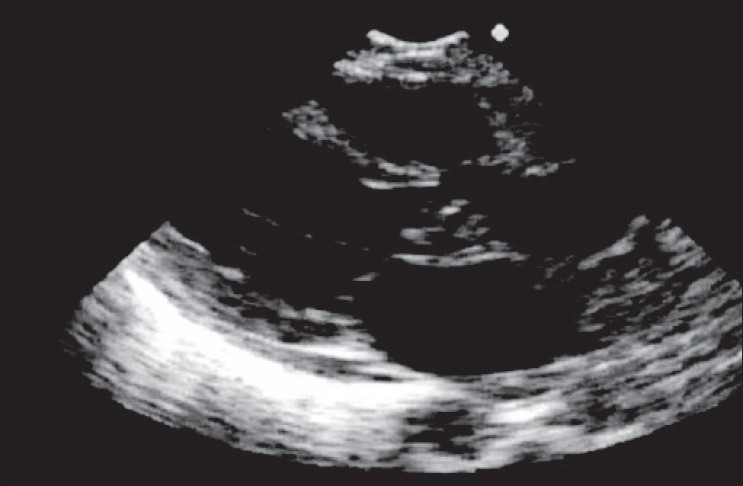
Aortic valve vegetation
Figure 2.
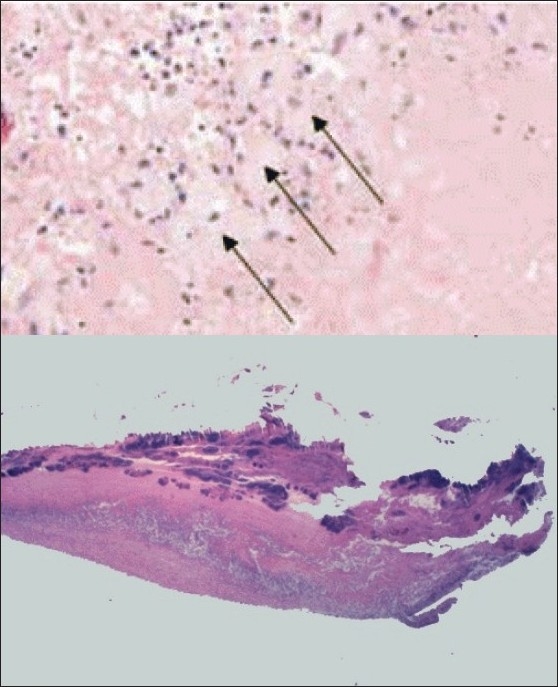
Valve vegetation pathology: x400. A pleiomorphic cellular infiltrate at the vegetation border can be seen including histiocytes (arrows)
DISCUSSION
Approximately 5% of cases of possible IE yield negative blood culture results.[1,2] Overall, the most common cause of culture-negative IE is prior use of antibiotics such as that seen in our patient who was advised to use antibiotics after catheter insertion and splenectomy. IE remains a diagnostic and therapeutic challenge. If left untreated, IE is generally fatal. The symptoms of early subacute native valve endocarditis (NVE) are usually subtle and nonspecific. They include low-grade fever (absent in 3-15% of patients), anorexia, weight loss, influenza-like syndromes, polymyalgia-like syndromes, pleuritic pain, syndromes similar to rheumatic fever (e.g., fever, dulled sensorium such as that seen in typhoid, headaches), and abdominal symptoms (e.g., right upper quadrant pain, vomiting, postprandial distress, appendicitis-like symptoms).[2] Murmurs are absent in approximately one-third of patients with acute IE.[3] The most common type is an aortic regurgitation murmur. Patients with splenomegaly may come to medical attention for a variety of reasons and may complain of left upper quadrant pain or fullness or of early satiety . The approach to the patient with undiagnosed splenomegaly[5] must be individualised. Our patient was a typical mismanaging case,[2] because the surgeon and haematologist had not paid attention to history of catheter insertion.[3,4] Our patient's cardiac examination could not confirm a murmur at initial presentation necessary to diagnose and referring patient to cardiologist.[6] In the absence of this, clinicians are encouraged to utilise transthoracic echocardiogram as an important tool to establish the diagnosisand work up of isolated splenomegaly .
CONCLUSION
This patient did not present with the common sign and symptoms associated with an IE; hence, we recommend echocardiography in the work up of isolated splenomegaly.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Habib G. Embolic risk in subacute bacterial endocarditis: Determinants and role of transesophageal echocardiography. Curr Cardiol Rep. 2003;5:129–36. doi: 10.1007/s11886-003-0080-6. [DOI] [PubMed] [Google Scholar]
- 2.Karchmer AW. Braunwald's heart disease. Text Book of cardiovascular medicine. 8th ed. Philadelphia: Saunders; 2008. Infective endocarditis; pp. 1713–7. [Google Scholar]
- 3.Bayram NA, Ayhan H, KeleŞ T, Durmaz T, Bozkurt E. Infective endocarditis mimicking left atrial myxoma. J Echocardiogr. 2010;8:124–5. doi: 10.1007/s12574-010-0044-y. [DOI] [PubMed] [Google Scholar]
- 4.Miller DL, O’Grady NP. Guidelines for the prevention of intravascular catheter-related infections: Recommendations relevant to interventional radiology. J Vasc Interv Radiol. 2003;14:S355–8. doi: 10.1016/s1051-0443(07)60120-1. [DOI] [PubMed] [Google Scholar]
- 5.Cronin CC, Brady MP, Murphy C, Kenny E, Whelton MJ, Hardiman C. Splenectomy in patients with undiagnosed splenomegaly. Postgrad Med J. 1994;70:288–91. doi: 10.1136/pgmj.70.822.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Koike N, Kaneko T, Ezure M, Sato Y, Hasegawa Y, Okada S, et al. A case of ulcerative colitis after mitral valve replacement due to infective endocarditis. Jpn J Cardiovasc Surg. 2009;38:327–31. [Google Scholar]


