Abstract
Bacterial pathogens display a variety of protection mechanisms against the inhibitory and lethal effects of host cationic antimicrobial peptides (CAMPs). To identify Yersinia pestis genes involved in CAMP-resistance, libraries of DSY101 (KIM6 caf1 pla psa) minitransposon Tn5AraOut mutants were selected at 37°C for resistance to the model CAMPs polymyxin B or protamine. This approach targeted genes that needed to be repressed (null mutations) or induced (upstream PBAD insertions) for the detection of CAMP resistance, and predictably for improved pathogen fitness in mammalian hosts. Ten mutants demonstrated increased resistance to polymyxin B or protamine, with the mapped mutations pointing towards genes suspected to participate in modifying membrane components, genes encoding transport proteins or enzymes, or the regulator of a ferrous iron uptake system (feoC). Not all the mutants were resistant to both CAMPs used for selection. None of the polymyxin B- and only some protamine-resistant mutants, including the feoC mutant, showed increased resistance to rat bonchoalveolar lavage fluid (rBALF) known to contain cathelicidin and β-defensin 1. Thus, findings on bacterial resistance to polymyxin B or protamine don’t always apply to CAMPs of the mammalian innate immune system, such as the ones in rBALF.
Keywords: Yersinia pestis, minitransposon, polymyxin B, protamine, LL-37
1. Introduction
Yersinia pestis is best known as the causative agent of bubonic plague, a disease transmitted by the bite of infected fleas. However, if inhaled, this pathogen also produces a severe primary pneumonia known as pneumonic plague, which is contagious and most often lethal. This bacterial agent uses an arsenal of virulence factors that render its entrance into the host as surreptitious as possible. These tools are thought to be most important during the first few hours following infection to avoid alarming the innate immune system and to avoid phagocytosis. We and others have previously shown that in addition to being antiphagocytic, the surface proteins F1 and Psa inhibit bacterial uptake by respiratory tract epithelial cells or macrophages [1–3]. The antiphagocytic mechanism of Psa was suggested to be due to Psa binding to host receptors that don’t direct internalization [4]. Y. pestis injects several antiphagocytic proteins directly into host cells through its type III secretion system (T3SS) [5, 6], some of which have strong anti-inflammatory properties [6–11]. In addition, Y. pestis also makes a non-inflammatory LPS at mammalian body temperature, thereby escaping the typical LPS-induced stimulation of TLR4 [12, 13]. Although the anti-inflammatory activities of Y. pestis also affect DCs and their migratory properties [14, 15], Y. pestis delivered through a fleabite still spreads to the local lymph node, causing lymphadenitis (bubo). Further spreading steps leading to bacteremia or septicemia are not infrequent, particularly when bubonic plague remains untreated. Plague lethality is generally assumed to be due to sepsis. Dissemination is facilitated by core LPS, the Psa fimbriae, the outer-membrane adhesin Ail and the plasminogen activator outer membrane protein Pla [16–20]. Pla acts as a protease that cleaves plasminogen to plasmin and mediates bacterial binding to extracellular matrix proteins [21, 22]. It is essential for bubonic plague, (but not for septicemic plague) after flea-mediated transmission [18, 19, 23, 24]. Pla is also essential for the development of (but not for the dissemination from) primary pneumonic plague [25].
Y. pestis has not only evolved to survive but also to thrive in a hostile host environment that includes the antimicrobial peptides of the innate immune system, as best exemplified by successful bacterial replication in local lymph nodes or lungs, leading to bubonic or primary pneumonic plague, respectively. Although the anti-inflammatory molecules of Y. pestis might down-regulate the expression of host cationic mammalian antimicrobial peptides (CAMPs) [26, 27], it is likely that this bacterium also expresses a battery of tools aimed at inactivating CAMPs in vivo. Accordingly, we recently observed that Pla, through its proteolytic activities, increased bacterial resistance to CAMPs at 37°C in vitro [48]. Curiously, this activity was counteracted in vitro by the F1 protein, an in-vivo expressed protein, suggesting that Y. pestis might use additional mechanisms of bacterial resistance to CAMPs. In addition to antimicrobial peptide degradation by proteases, other bacteria have been reported to trap CAMPs extracellularly, alter their surface, particularly their surface charge, pump CAMPs out, or modulate host cell expression or degradation of CAMPs [28, 29]. The aim of this study was to identify new Y. pestis genes involved in any of these survival strategies. For this purpose, a minitransposon with an outward-oriented inducible promoter was constructed and used to identify genes that either increase CAMP resistance by being repressed (null mutants) or that demonstrate resistance by being activated (inducible gene expression).
2. Results
2.1. Isolation of CAMP-resistant minitransposon mutants
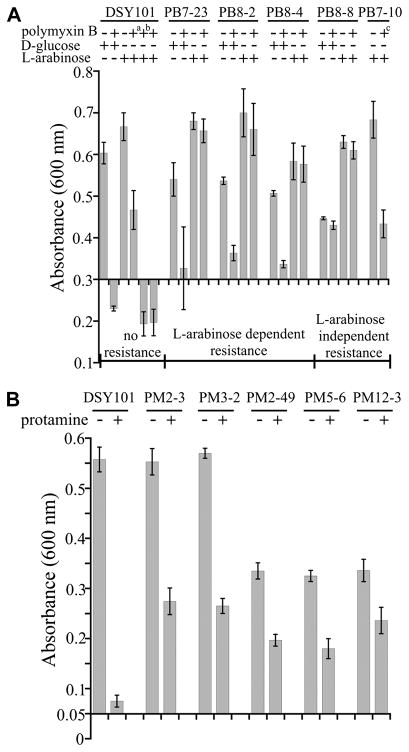
Tn5AraOut mutants of strain DSY101 that demonstrated increased resistance to polymyxin B or protamine were isolated as described in Materials and Methods. Briefly, Y. pestis strain DSY101 was transformed with plasmid pTn5AraOut and bacteria were selected on kanamycin-containing media at 37°C cont aining L-arabinose and supplemented with polymyxin B or protamine at concentrations previously shown to inhibit strain DSY101 growth. Selection was done in the presence of arabinose to simultaneously obtain both arabinose-dependent and -independent CAMP-resistant mutants. Consistency in the phenotypes of clone-purified mutants was confirmed for five polymyxin-resistant and five protamine-resistant isolates on selective agar plates. No spontaneous resistant bacteria could be isolated in parallel control experiments with mock(H2O)-transformed bacteria, strongly suggesting that the isolated polymyxin- and protamine-resistant clones were due to the minitransposon insertions. These mutants were further characterized by determining the arabinose-dependency of their resistance and by a quantitative analysis of their CAMP resistance levels. For this, each strain was grown in broth to log phase and further multiplication or killing was studied in the presence or absence of CAMPs. Bacterial growth was monitored in the presence of 0.2% arabinose, to activate the inducible promoter on the minitransposon, or 0.2% glucose as a repressor of this promoter (negative control). All our studies were done with bacteria grown at 37°C, since our aim was to evaluate CAMP effects on Y. pestis at mammalian body temperature. In addition to the determination of MICs, growth was analyzed more precisely by determining absorbance values (A600). That all the mutants and the parental strain grew somewhat better in the presence of arabinose than in the presence of glucose was probably related to a previously described negative effect of glucose on Y. pestis growth [30]. However, this effect did not interfere with the interpretation of the results concerning antimicrobial resistance, since bacterial growth of the mutants was compared with growth of the parental strain studying both media with or without polymyxin B. Fig. 1A shows that polymyxin B was clearly bactericidal on parental strain DSY101 at 1.25 μg/ml or more, the lower dose of 0.625 μg/ml being still able to inhibit bacterial growth, as compared to the bacteria in polymyxin B-free broth. In contrast, four of the five mutants grew well at the significantly higher dose of 5 μg/ml polymyxin B, growth of three of these resistant mutants (PB7-23, PB8-2 and PB8-4) being clearly arabinose-dependent, since their growth was inhibited by polymyxin B only in the absence of arabinose. Mutant PB8-8 demonstrated arabinose-independent polymyxin B-resistance, its growth being not inhibited by polymyxin B, irrespective of the presence or absence of arabinose (Fig. 1A). Similarly, mutant PB7-10 still grew in the presence of twice the concentrations of polymyxin B that was killing the parental strain in the presence of arabinose (Fig. 1A) or glucose (data not shown), indicating also arabinose-independent polymyxin B resistance. The five mutants selected on protamine agar were able to grow significantly in the presence of a protamine-concentration that blocked multiplication of the parental strain DSY101 (Fig. 1B). Interestingly, protamine resistance was arabinose-independent for all the five mutants (data not shown). Although three of the mutants grew slower than the parental strain in the absence of protamine, mutants PM2-3 and PM3-2 grew as well, indicating that protamine-resistance wasn’t necessarily linked to some effect on bacterial multiplication under the used growth conditions. Taken together, the quantitative analysis of bacterial growth in broth clearly confirmed the polymyxin B and protamine resistance phenotypes of the mutants.
Fig 1.
Bacterial growth with the CAMPs used to select the mutants. (A) Bacteria were grown in BHI with or without glucose or arabinose to an A600 of 0.3 at 37°C, polymyxin B was added to a concentration of 5 μg/ml (or a0.625 μg/ml, b1.25 μg/ml, and c2.5 μg/ml), the cultures were further incubated for 18 h before measuring growth (A600). MICs were determined in microtiter plates and were 1 μg/ml for DSY101 and 8 μg/ml for all the mutants (except PB7-10, 4 μg/ml). (B) Bacteria were grown in BHI to an A600 of 0.3 at 37°C, diluted to an A 600 of 0.05 (to use concentrations of protamine that do not interfere significantly with A600 reading), protamine was added to a concentration of 0.4 mg/ml and the cultures were further incubated for 18 h before measuring growth (A600). MICs were determined in microtiter plates and were 0.4 mg/ml for DSY101 and 0.8 mg/ml for all the mutants. All the data are means of at least three independent experiments with standard errors.
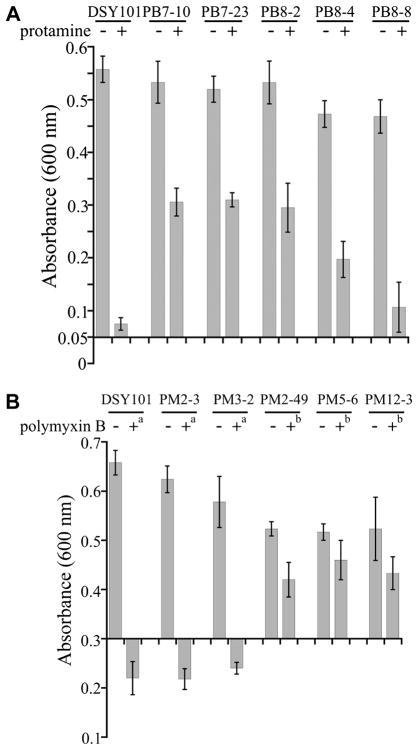
2.2. Dissociation of polymyxin B and protamine resistance
To determine whether the two CAMPs target different bacterial components or possibly share their mode of actions, the polymyxin B resistant mutants were tested for protamine resistance, and vice versa, using the same experimental conditions described above, including the inducer arabinose in all the assays. Although four polymyxin B resistant mutants were also resistant to protamine, strain PB8-8 didn’t multiply significantly with protamine (Fig. 2A). Conversely, mutant strains PM2-3 and PM3-2 that showed resistance to protamine were killed by polymyxin B, whereas the other three protamine resistant mutants grew in the presence of polymyxin B (Fig. 2B). That some mutants showed a dissociation of resistance properties between polymyxin B and protamine highlighted the existence of different cationic peptide-specific mechanisms of CAMP resistance.
Fig 2.
Bacterial growth with CAMPs different from the ones used to select the mutants. (A) The polymyxin B-resistant mutants and the parental strain DSY101 were grown in BHI to an A600 of 0.3 at 37°C, diluted to an A 600 of 0.05, protamine was added to a concentration of 0.4 mg/ml and the cultures were further incubated for 18 h before measuring growth (A600). MICs were determined in microtiter plates and were 0.8 mg/ml for all the mutants. (B) The protamine-resistant mutants were grown in BHI to an A600 of 0.3 at 37°C, polymyxin B was added to a concentrati on of a1.25 μg/ml or b5 μg/ml, the cultures were further incubated for 18 h before measuring growth (A600). MICs were determined in microtiter plates and were 1 μg/ml (PM2-3, PM3-2 ) or 16 μg/ml (PM2-49, PM5-6 and PM12-3). All the data are means of at least three independent experiments with standard errors.
2.3. Susceptibility of selected mutants towards rBALF antimicrobials and LL-37
Since the polymyxin B- and protamine-resistance profiles were only partially overlapping, we wondered how the mutants would respond to constitutively expressed respiratory tract antimicrobial peptides. Again, the assays were undertaken as described above, in the presence of arabinose. By first testing bacterial growth in rBALF, which contains rCRAMP [4], the rat ortholog of the human cathelicidin LL-37, it was observed that all the mutants selected for polymyxin B resistance did not multiply (Fig. 3A). In contrast and with the exception of strain PM2-3 and PM3-2, the three other mutants selected for protamine resistance were able to grow in the presence of rBALF. To test these results more specifically, we investigated growth of these mutants in the presence of the purified mammalian CAMP, LL-37. Confirming the data obtained with rBALF, all the rBALF-susceptible mutants were also sensitive to LL-37, as exemplified with mutant PB7-23 (Fig. 3B). The other rBALF-susceptible mutants showed comparable LL-37 concentration-dependent killing effects, with ≥ 103 reductions of CFUs for 160 μg/ml LL-37. Conversely, the three rBALF-resistant mutants were also resistant to LL-37 (Fig. 3B). To summarize, only two of the polymyxin B-susceptible mutants (PM2-3 and PM3-2) were resistant to protamine and rBALF/LL-37 and all polymyxin B-resistant mutants (most being also protamine-resistant) were susceptible to rBALF/LL-37. These results indicated that polymyxin B- or protamine-resistance is not necessarily representative of resistance towards mammalian antimicrobial peptides, such as the ones of the respiratory tract.
Fig 3.
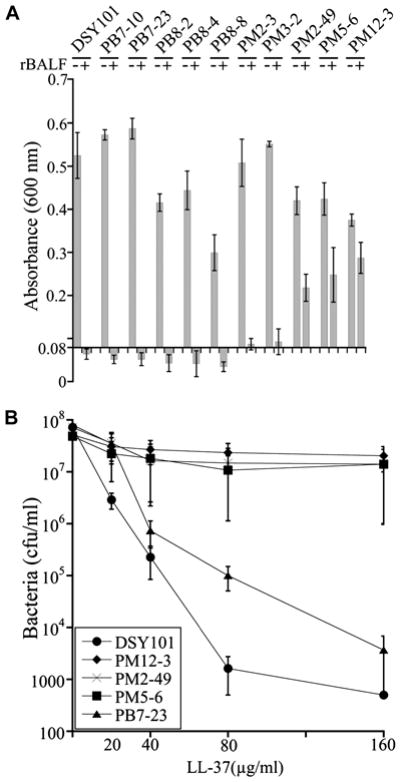
Bacterial growth of all the mutants in the presence of rBALF or LL-37. (A) Bacteria were grown in BHI to an A600 of 0.3 at 37°C, diluted to an A 600 of 0.08, rBALF was added to a concentration of 60 μg/ml protein and the cultures were further incubated for 18 h before measuring growth (A600). MICs were determined in microtiter plates and were 60μg/ml protein for DSY101, all the polymyxin B mutants, PM2-3 and PM3-2, and 120 μg/ml protein for PM2-49, PM5-6 and PM12-3. (B) Bacteria were grown in BHI to an A600 of 0.3 at 37°C, diluted to an A 600 of 0.08, LL-37 was added to 20, 40, 80 or 160 μg/ml protein and the cultures were further incubated for 18 h before determining bacterial survival (CFUs). All the data are means of at least three independent experiments with standard errors.
2.4. Mapping Tn5AraOut in the CAMP-resistant mutants
The mutants were further characterized by mapping their Tn5AraOut insertion sites and orientations as described in Materials and Methods (Table 3). Briefly, DNA including Tn5AraOut for each of the ten resistant mutants was cloned by using different restriction enzymes. For each mutant-restriction enzyme pair, plasmid clones of similar sizes were obtained and DNA flanking the minitransposon inserts of these plasmids was sequenced. Sequencing plasmids from each individual mutant always yielded the same flanking sequences, strongly suggesting that each mutant had only one Tn5AraOut copy in its genome. This was confirmed by Southern blot analysis using genomic DNA restricted with either one of two different enzymes and a probe lacking the corresponding sites, each mutant showing only one major hybridizing fragment (Supplemental Fig. 1). Moreover, since spontaneous resistant mutants were not detected with mock transformed bacteria, the mapped minitransposon inserts were most likely responsible for the described resistance phenotypes. Further supportive evidence on single transposon insertions responsible for resistance phenotypes in individual mutants were derived from detailed characterization of mutants of interest, as described below. Three of the CAMP-resistant mutants selected with polymyxin B had an arabinose-dependent resistance phenotype that was presumably linked to the activation of downstream genes (Table 3 and Fig. 1A). For example, mutant PB7-23 had the arabinose-inducible promoter upstream of the pbgP operons, which includes 7 cotranscribed genes (pmrHFIJKLM or arnBCADTEF) required for the synthesis of 4-aminoarabinose that is added to the phosphates of lipid A in Y. pestis LPS [13, 31, 32]. Arabinose-dependent induction of pmrH transcription was confirmed in this mutant by qRT-PCR (mean ± standard error = 15.0 ± 4.5 fold increase with the inducer, n = 4, versus 1.4 ± 0.7 without inducer, n = 3, P = 0.037). The detection of such a mutant in our screen supported our experimental method, since it had been previously shown that 4-aminoarabinose-decorated LPS renders Y. pestis more resistant to polymyxin B. The two other mutants with arabinose-inducible resistance to polymyxin B (PB8-4 and PB8-2) had minitransposon insertions upstream of two single or monocistronic genes, y2568 which encodes a hypothetical protein, and y1522 which encodes an Hcp-like protein that is not linked to any of the five predicted type 6 secretion systems (T6SS) of Y. pestis [33]. In contrast, two arabinose-independent polymyxin B-resistant mutants (PB7-10 and PB8-8) had minitransposon insertions in the promoter region of asmA and hflC orthologs of E. coli. AsmA modulates porins, glycerophosphates and LPS levels in the outer membrane [34–36], whereas hflC encodes a repressor of the proteolytic activity of the integral inner membrane protein FtsH [37] which can regulate LPS concentrations through proteolysis of LpxC [38, 39]. Thus, apart from the targeted hypothetical protein, the mutants selected for increased resistance to polymyxin B had a Tn5AraOut insertion in gene loci for bacterial envelope components or potentially secreted molecules. Of the five additional CAMP resistant mutants that were selected with protamine, four had mutations in orthologs of E. coli or Salmonella transport systems, including two independent minitransposon insertions (PM2-3 and PM3-2) in the gene for the low affinity metal phosphate transporter PitA [40, 41]. The PM2-49 mutant had its transposon insertion mapped 42 bp upstream of a predicted operator site for the GalR repressor of the galactose import system MglBAC [42]. Polymyxin B resistance of this mutant was arabinose-independent. This was consistent with mglB transcription in PM2-49, which was turned on whether it was induced (mean ± standard error = 6.9 ± 4.8 fold increased transcript levels, n= 4, as compared to the parental strain) or not (9.2 ± 6.1 fold increased transcript levels, n = 3; induction effect P = 0.394), as detected by qRT-PCR. Thus, the minitransposon insert of PM2-49 is suggested to have inactivated GalR-mediated repression of the mglBAC operon [43]. The protamine-resistant mutant PM5-6 had an insertion in y0958 that encodes a putative glycerophosphoryldiester diesterase, designated GlpQ-like. That protamine resistance of this mutant was linked to the inactivation of this gene and not to a potential activation of downstram dinP transcription was confirmed by dinP qRT-PCR (comparison with the parental strain, P = 0.99). The GlpQ-like orf predicts a significantly different primary structure than those of the E. coli (or Y. pestis) GlpQ and UgpQ enzymes, which are involved in the intracellular uptake and production of sn-glycerol-3-phosphate, a carbon and energy source and a precursor for novel phospholipid synthesis and recycling of membrane phospholipids [44]. The last protamine-resistant mutant (PM12-3) mapped in the predicted inhibitor of the ferrous iron importer system designated Feo, as discussed later [45].
Table 3.
Mapped Tn5AraOut insertions in CAMPs-resistant mutants
| Mutants | Locus tag | Gene | Protein | Arabinose dependency | Schematic diagram |
|---|---|---|---|---|---|
| PB7-1 | y2644 | asmA | putative assembly protein | − |
|
| PB7-23 | yl917-yl923 | pbgPoperon | UDP-4-amino-4-deoxy-L-arabinose—oxoglutarate aminotransferase,etc. | + |
|
| PB8-2 | yl522 | hcp-\\ke | DUF796, T6SS effector hep like | + |
|
| PB8-4 | y2568 | unknown | hypothetical protein | + |
|
| PB8-8 | y0634 | hflC | FtsH protease regulator HflC | − |
|
| PM2-3& PM3-2 | y3862 | pilA | phosphate ABC transporter permease | − |
|
| PM2-49 | y2662 | mglB | galactose-binding protein | − |
|
| PM5-6 | y0958 | glpQ-Yike | glycerophosphoryl diester phosphodiesterase family protein | − |
|
| PM12-3 | y3910 | feoC | ferrous iron transport protein C,transcriptional regulator | − |
|
2.5. CAMP resistance and bacterial surface modifications
Most of the mutants detected in this study had Tn5AraOut insertions that were located in or upstream of genes encoding proteins involved in membrane components or molecular transport through membranes. LPS, a major component of the outer membrane, is known to interact with CAMPs. Accordingly, one Tn5AraOut insertion located upstream of the pbgP operon involved in LPS modification (Table 3, PB7-23) showed arabinose-dependent resistance to CAMPs. Thus, we wondered whether the increased CAMP-resistance of some of the other mutants could be related to an indirect effect on LPS. We first analyzed LPS levels by SDS-PAGE and found no significant differences between the mutants and the parental strain (data not shown). Subsequently, we evaluated whether the mutations affected bacterial surface properties resulting in a reduction of CAMP binding by labeling the bacteria grown at 37°C with dansyl-conjugated polymyxin B. Preliminary microscopic evaluation suggested decreased binding of polymyxin B for several mutants (not shown). To evaluate this effect in a quantitative manner, the level of binding was determined by fluorometry. Five polymyxin B-resistant mutants (PB7-10, PB7-23, PM2-49, PM5-6 and PM12-3) showed a significant decrease in polymyxin B binding (Fig. 4), whereas polymyxin-B susceptible mutant PM2-3 bound polymyxin B as well as the parental strain. These data supported the assumption that the polymyxin B-resistant mutants with the corresponding mapped mutations (asmA, pbgP, mglB, glpQ-like and feoC) are involved in modifying the molecules or molecular composition of the bacterial outer membrane. Other mechanisms might explain the phenotypes of mutants PB8-4 (hypothetical gene) and PB8-2 (hcp-like gene). Arabinose-induced expression of the latter gene (y1522) in PB8-2 slightly increased polymyxin B binding, albeit not significantly. Since Hcp proteins have been reported in other bacteria to be secreted in the medium, spent broth of PB8-2 was tested by western blot analysis. Although the protein was present in the bacteria, it could not be detected in spent broth of the minitransposon mutant (not shown). A mutant lacking the corresponding gene and complemented with a plasmid expressing the Hcp-like protein from an ITPG-inducible plasmid gave the same result (not shown). Increased polymyxin B resistance was only detected in the complemented strain when production of the plasmid-encoded protein was activated, confirming the arabinose-dependency of the minitransposon mutant phenotype. Moreover, deletion of the neighboring y1523 gene, which could have been affected in its promoter region (Table 3), did not increase polymyxin B resistance, indicating that this gene was not involved in the PB8-2 phenotype. The Hcp-like protein could not be detected in membrane fractions or on the surface of PB8-2 (not shown), possibly because of the insufficient basal expression of a complementary type 6 export machinery. That the observed phenotype was due to an indirect effect resulting from the accumulation of the y1522 gene product in the cytoplasm was unlikely, since E. coli or Salmonella enterica strains expressing the y1522 in trans were not polymyxin B resistant (not shown).
Fig 4.
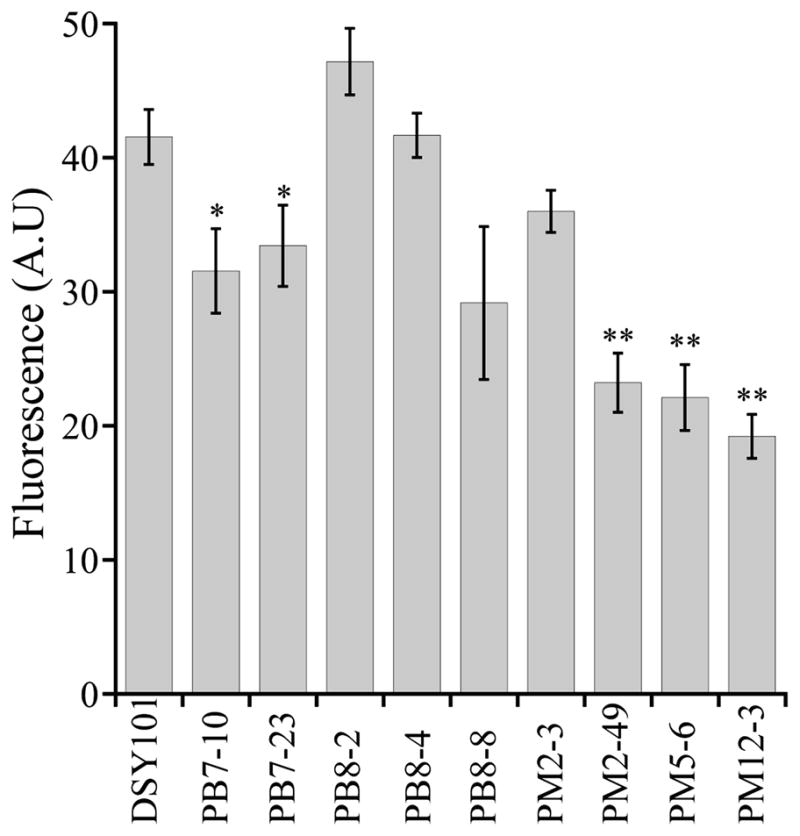
Binding of polymyxin B to bacterial surfaces. Standardized concentrations of bacteria were incubated with dansyl-polymyxin B for fluorometric analysis and determination of arbitrary units (A.U.) of fluorescence, as described in Material and Methods. All the data are means of at least three independent experiments with standard errors. Unpaired t-tests comparing each mutant to the parental strain DSY101 showed statistical significant differences for several comparisons (* P < 0.05, ** P < 0.001).
2.6. CAMP resistance and inactivation of feoC
As expected, polymyxin B resistance of the feoC::Tn5AraOut strain and a feoC deletion were comparably increased (Fig. 2B and Fig. 5). Since the feoC gene has been suggested to be a repressor of the feoAB genes [45], polymyxin B resistance was thought to be associated with feoAB derepression. Accordingly, a feoBC mutant (and a feoB mutant, not shown) was as sensitive to polymyxin B as the parental strain DSY101 (Fig. 5). Moreover, when the feoAB genes were expressed from an inducible vector, they overrode feoC repression in DSY101, confirming the proposed model (Fig. 5). These results suggested that feoC represses the feoAB genes in vitro and that the feoAB genes are involved in mediating polymyxin B resistance. Increased FeoAB-mediated ferrous iron uptake is anticipated to cause oxidative stress by the Fenton reaction, resulting in induction of the Fur regulon. In addition to repressing iron uptake systems, Fur up-regulates the expression of a variety of genes, including the ones for several surface proteins and catalase (or hydroperoxidase II) [46]. Accordingly, the feoC::Tn5AraOut mutant was four times as much resistant to peroxide as the parental strain (MIC of 16 mM versus 4 mM, respectively), suggesting increased catalase expression as a response to the activation of the FeoAB-mediated ferrous iron import. Since the feoC::Tn5AraOut mutant was also more resistant to protamine and rBALF, as compared to the parental strain, we wondered whether the feoC gene was repressed in vivo, possibly increasing bacterial resistance to CAMPs, and thus improving bacterial survival, growth and dissemination in an infected host. To test this possibility, the parental strain KIM5 and an isogenic feoB mutant were administered together by the s.c. route to C57BL/6 mice and dissemination of the two bacteria was studied over time. Interestingly, the parental strain was always found in higher numbers than the feoB mutant when bacteria were isolated from the livers and spleens (Fig. 6). Bacteria could not be detected in the organs of many mice, indicating that Y. pestis KIM5 administered s.c. at the dose used had been rapidly eliminated in the host. Although daily differences were statistically significant in the liver only at day 4 (P < 0.005), differences of the aggregated data for the four studied days were highly significant (P < 0.002 for the livers and P < 0.0004 for the spleens). These results suggested that feoB is expressed in vivo and improves bacterial dissemination, possibly by increasing CAMP-resistance and/or purveying iron to the multiplying bacteria.
Fig 5.
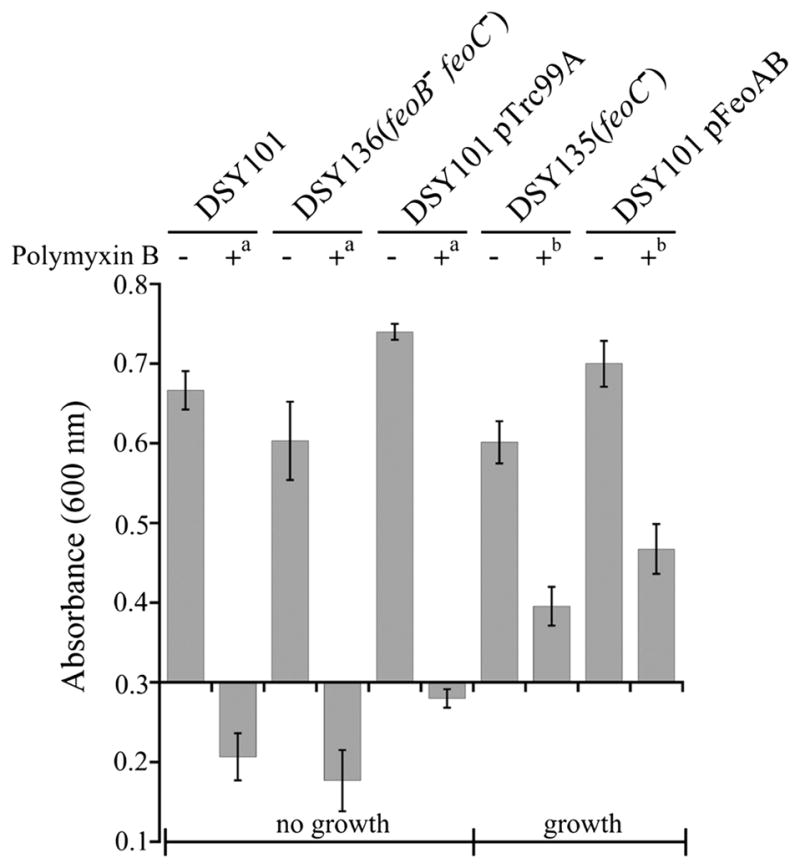
Growth of feo mutants and complemented strains in the presence of polymyxin B. (A) Bacteria were grown in BHI to an A600 of 0.3 at 37°C, polymyxin B was added to a concentration of a1.25 μg/ml or b5 μg/ml, the cultures were further incubated for 18 h before measuring growth (A600). All the data are means of at least three independent experiments with standard errors.
Fig 6.
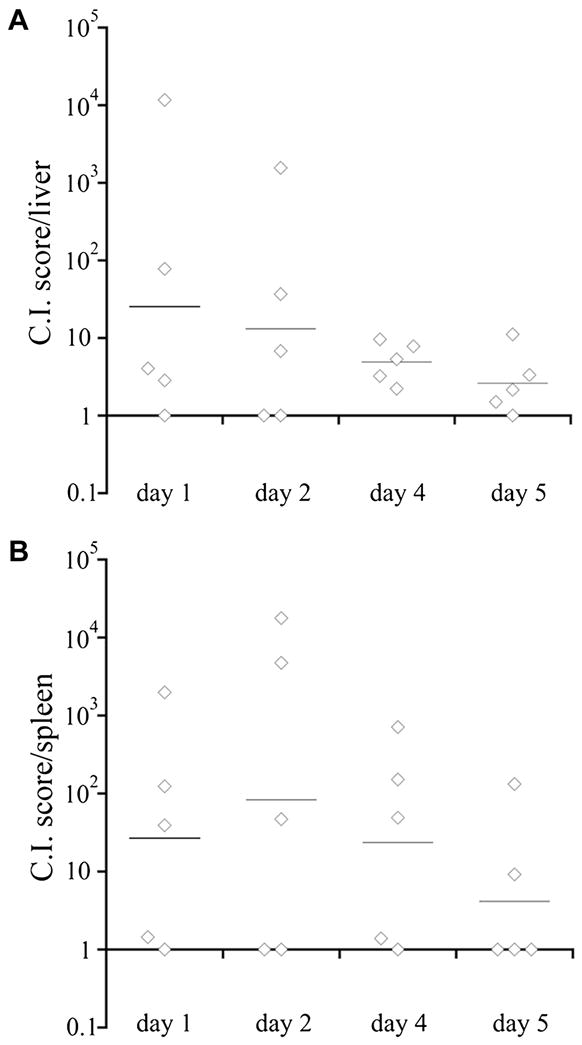
Y. pestis KIM5 and DSY137 (KIM5 feoB) competition experiment in mice. C57BL/6 mice were challenged s.c. with a 1:1 mixture of KIM5 and DSY137 (3×107 CFU each). Five mice were sacrificed on days 1, 2, 4 and 5 and CFUs were determined in livers (A) and spleens (B) to calculate competitive index (C.I.) scores (KIM5 CFUs divided by the DSY137 CFUs). C.I. scores for each mouse are shown as diamonds and bars represent geometric means.
3. Discussion
Y. pestis encounters constitutively expressed CAMPs such as the cathelicidin LL-37 when it accesses the lower respiratory tract or the skin after a fleabite [47]. We have previously shown that cathelicidins and β-defensins have bactericidal activities towards Y. pestis and that Pla inactivates these CAMPs [48]. Since the F1 protein inhibits the CAMP-inactivating effect of Pla and both proteins are expressed in vivo, it is likely that Y. pestis utilizes other mechanisms to resist CAMPs in host tissues. The goal of this study was to identify new Y. pestis genes involved in CAMP resistance. Traditionally, such genes have been detected in various pathogens by screening for CAMP sensitive mutants out of a library of knockout mutants [49–51]. This approach implies that the “resistance” genes are expressed in vitro. Here, we used a minitransposon engineered with an inducible promoter to identify genes that need to be repressed or activated for detection of CAMP resistance. By selecting mutants for increased resistance towards CAMPs, we focused on genes that could be beneficial to bacterial survival in vivo whether repressed or activated, as determined with null mutations or inducible promoter insertions, respectively.
The used protocol identified several genes encoding proteins that were previously described in other bacteria to be involved directly or indirectly in the organization of the outer membrane. For example, a mutation resulting in an inducible polymyxin B resistance was related to the activation of the pbgP operon which decorates the phosphates of lipid A with 4-aminoarabinose, an LPS modification reported to increase polymyxin B resistance in various bacteria [31]. Other genes involved in polymyxin B resistance detected in this study, such as asmA [34–36] and hflC [37, 38] have been previously shown to have indirect effect on LPS levels in the outer membrane. Consistent with a reduction in LPS levels, we observed that polymyxin B binding to the surface of the corresponding mutants was reduced. Whether import machineries for phosphate (PitA, GlpQ-like protein) and galactose (MglBAC) have indirect effects on species structures and compositions of membrane lipids that can explain CAMP resistance remains to be studied.
The y1522 and y3910 genes were investigated in more details since their gene products were potentially involved in modulating new mechanisms of CAMP-resistance. Expression of the Hcp-like protein encoded by the y1522 gene determined CAMP resistance, irrespective of whether induced expression was from the ara promoter of the minitransposon or from the trc promoter of a complementing plasmid in a y1522 mutant. Hcp proteins are type 6 secreted proteins that form hexameric rings suggested to assemble in a tubular system for effector molecule delivery to eukaryotic cells [52, 53]. Similar to some hcp genes of other bacteria, y1522 is an orphan hcp gene (i.e. unlinked to any of the T6SS gene clusters). Hcp proteins are either secreted or tightly associated to bacterial surfaces [33, 52, 54]. Interestingly, the y1522 gene product was not secreted or detected in bacterial membranes under the growth conditions used. Thus, it remains possible that the y1522 product is only secreted under specific conditions that were not duplicated here. Alternatively, artificial expression of the Hcp-like product of y1522 without activated expression of its corresponding T6SS might not result in secretion. Finally, expression of the Hcp-like product of y1522 might result in activation of an intracellular response that indirectly leads to CAMP resistance independent of type 6 secretion. Although a Y. pestis mutant lacking one of its Hcp molecule was not attenuated in models of bubonic or pneumonic plague, replication of this mutant in J774.A1 macrophages was limited, suggesting some nonessential role of a T6SS in Y. pestis pathogenesis [55].
CAMP resistance of the feoC::Tn5AraOut mutant was duplicated with a feoC (y3910) deletion mutant, confirming that the phenotype was due to the disruption of feoC. FeoC has been proposed to be a repressor of the feoAB operon [45], which encodes one of the two ferrous iron uptake systems of Y. pestis, the other one being encoded by the yfeABCD genes [56]. Consistent with the regulatory role of FeoC, FeoC-independent expression of FeoA and FeoB mimicked the CAMP-resistant phenotype obtained with the feoC mutant. Moreover, a feoBC deletion mutant was as sensitive to CAMP as the parental non-mutated strain. Taken together, these data indicated that induction of FeoAB expression increased CAMP resistance and supported a regulatory role for FeoC. How activation of ferrous iron uptake into the bacterial cytoplasm results by itself in CAMP resistance is not clear. One potential mechanism is that this resistance was directed by the Y. pestis Fur protein, which differentially regulates a large number of proteins, including membrane proteins [46]. This would be consistent with our finding that feoC−-mediated resistance to all tested CAMPs was linked to decreased polymyxin B-binding, suggesting some membrane modifications. Moreover, intracellular iron acts as a co-regulator of the Fur protein to down-regulate iron uptake systems, protecting the bacterial cell against the toxic effects of the Fenton reaction [57]. In addition, Fur activates the expression of various scavenging proteins of oxidative intermediates, including catalase [46, 58]. Consistent with the activation of the Fur pathway, the feoC mutant was also more resistant to peroxide than the parental strain. A feoB mutant of Y. pestis was attenuated in a competition assay with the parental strain after s.c. administration to mice, highlighting the bacterial use of its Feo system in vivo to augment virulence. Similarly, E. coli or Salmonella feoA or feoB mutants demonstrated reduced virulence properties in mice models of infections [45]. Interestingly, Y. pestis has two ferrous uptake systems (Yfe and Feo) and both systems were shown to be needed but redundant for optimal Y. pestis growth in a murine macrophage cell line [56]. A yfe mutant had a 100-fold increased LD50 after s.c. infection of mice [59]. In vivo studies with a feo yfe double mutant might show a more drastic effect on virulence and bring further evidence to the current data that supports a role for intra-macrophage survival of Y. pestis in the early stages of plague [60]. Additional studies will be needed to differentiate the contributions of the feo genes in iron replenishment and CAMP resistance for the intracellular survival and growth of Y. pestis. Interestingly, another study has recently linked iron uptake with polymyxin B resistance in Y. pseudotuberculosis, a coregulator of the yfe and pbgP genes being responsible for both phenotypes [61].
Finally, this study illustrates a clear dissociation between the resistance profiles of Y. pestis mutants towards polymyxin B, protamine and rBALF/LL-37. Increased resistance of the hflC or pitA mutants was specific for polymyxin B or for protamine, respectively. Moreover, only three of the protamine-resistant and none of the polymyxin B-resistant mutants showed increased resistance towards rBALF, known to contain at least rCRAMP and rat β-defensin 1 [48]. The three rBALF-resistant mutants were also resistant to human cathelicidin LL-37, whereas growth of the polymyxin B-resistant mutant PB7-23 with an activated pbgP operon was significantly affected by LL-37. The latter result was surprising since LL-37 was described to activate the PhoPQ two-component system in Salmonella [62], which itself activates the pbgP operon in Salmonella and Y. pestis [31]. Whether mammalian CAMPs are not good activators of the Y. pestis PhoPQ system, aminoarabinose decoration of LPS doesn’t protect Y. pestis significantly from LL-37 or the experimental conditions used were suboptimal to detect an effect remains to be determined. Previously detected differences between polymyxin B, cecropin A and/or defensin A resistance of Y. pestis phoP or lpxM lpxP or Y. pseudotuberculosis pbgP operon mutants remained essentially unexplained [13, 63, 64]. Nevertheless, accumulating evidence indicates that CAMP resistance is CAMP-type specific and that this specificity is determined by a variety of bacterial genes, particularly those capable of modulating directly or indirectly the bacterial surface architecture, including the composition and content of its protein and lipid species.
4. MaterIals and Methods
4.1. Bacterial strains, growth conditions and reagents
Bacterial strains and plasmids used in this study are listed in Table 1. Media and media components were from Difco (BD Diagnostics, Sparks, MD). Y. pestis strains were grown overnight in brain heart infusion (BHI) broth at 26°C, diluted to an A 600 of 0.1 in BHI and further grown at 37°C. For colony selection, Y. pestis was grown on BHI or TB agar (10 g tryptose, 2.5 g NaCl, 3.0 g Bacto beef extract paste and 1.5% Bacto-agar per liter) for 24–48 h at 26°C for colony counts or at 37°C for mutant selection. For quantitative RT-PCR, bacteria grown at 26°C in heart Infusion (HI) were sub-cultured in HI for 4 h at 37°C. E. coli strains were grown at 37°C in LB broth or agar. When required, the media were supplemented with kanamycin (Km, 45 mg/l), ampicillin (Ap, 200 mg/l) or chloramphenicol (Cm, 20 mg/l). When appropriate, the arabinose and lactose promoters were induced with 0.2% L-arabinose and 1mM IPTG, respectively, using X-Gal (40 mg/l) as chromogenic substrate with the latter. Reagents, including polymyxin B sulfate salt and salmon protamine sulfate salt were from Sigma-Aldrich Corp. (St Louis, MO), and LL-37 was from AnaSpec (Fremont, CA). Rat bronchoalveolar lavage fluid (rBALF) was generously supplied by Sandra R. Bates-Kenney, and was shown to contain the cathelicidin rCRAMP and rat β-defensin 1 [48].
Table 1.
Bacterial strains and plasmids
| Strain or plasmid | Description | Source |
|---|---|---|
| E. coli | ||
| CC118λpir | Δ(ara-leu) ΔaraD lacX74 galE galK phoA thi-1 rpsE rpoB argE(Am) recA1, lysogenized with λpir phage | [74] |
| DH5α | fhuA2 Δ(argF-lacZ)U169 phoA glnV44 φ80 Δ(lacZ)M15 gyrA96 recA1 relA1 endA1 thi-1 hsdR17 | Invitrogen Corp., Carlsbad, CA |
| BL21(DE3) | E. coli B (DE3)[F− dcm ompT hsdSB (rB− mB−)] | Novagen, EMD Biosc., Madison, WI |
| Y. pestis | ||
| KIM5 | Y. pestis KIM pgm | [75] |
| KIM6 | KIM5 pCD1− (LCR−) | [75] |
| DSY88 | KIM6 Δcaf Δpsa pPCP1ΩaphA Δpla | [48] |
| DSY101 | DSY88 PCP1Δpla | This study |
| DSY131 | DSY101 Δy1522::aphA | This study |
| DSY132 | DSY101 Δy1523::aphA | This study |
| DSY133 | DSY131 pTrc99A | This study |
| DSY134 | DSY131 pHcpy1522 | This study |
| DSY135 | DSY101 Δy3910(feoC)::aphA | This study |
| DSY136 | DSY101 Δy3910–y3911(feoBC)::aphA | This study |
| DSY137 | KIM5 Δy3911(feoB)::aphA | This study |
| Plasmids | ||
| pNJ17 | TnAraOut delivery vehicle; Kmr | [65] |
| pRL27 | Plasmid with mini-Tn5 and oriR6K; Kmr | [66] |
| pTn5AraOut | pRL27 with araC-PBAD from pNJ17; Kmr | This study |
| pRS415 | lacZ transcriptional fusion vector; Apr | [76] |
| pSIM9 | pRK2 gam exo bet; Cmr | [77] |
| pKD4 | Plasmid with the Kmr template for PCR | [72] |
| pET22b(+) | Expression vector; His6 affinity tag; Apr | Novagen |
| pETHcp | pET22b(+)-y1522; Apr | This study |
| pTrc99A | Expression vector with trc (trp-lac) promoter; Apr | [78] |
| pHcpy1522 | pTrc99A-y1522 | This study |
| pFeoAB | pTrc99A-y3911–y3912 | This study |
4.2. Construction and testing of plasmid pTn5AraOut
Preliminary studies showed that the minitransposon miniTn5 of pRL27 transposed efficiently in KIM6. Plasmid pTn5AraOut was engineered by inserting the EcoRI fragment of pNJ17 that contains the araC gene and PBAD promoter [65] into the SwaI site of pRL27, which carries a miniTn5 delivery vector [66]. The araC-PBAD DNA fragment was blunted by filling in its protruding ends with the Klenow fragment of DNA polymerase before the ligation reaction. A successful construct carrying the miniTn5 with PBAD facing out was identified by restriction analysis and renamed pTn5AraOut. Preliminary studies showed that the minitransposon of pRL27 transposed efficiently in KIM6 and the transposition efficiency of Tn5AraOut was only marginally lower than that of pRL27. To test the function of the arabinose-dependent promoter in Tn5AraOut, E. coli DH5α harboring the promoter-trap plasmid pRS415 was transformed with pTn5AraOut and the bacteria were screened for β-galactosidase activity on LB agar plates containing Ap, Km, X-gal and L-arabinose. Bacteria isolated from Lac+ (blue) colonies were shown by restriction analysis to harbor Tn5AraOut upstream of the lacZ gene in pRS415. Arabinose-dependent induction was further confirmed on MacConkey agar plates.
4.3. Minitransposon mutagenesis, mutant selection and screening
Y. pestis strain DSY101 was randomly mutagenized with the minitransposon Tn5AraOut. For this, plasmid pTn5AraOut was introduced into strain DSY101 by 20 independent electroporations, using in parallel water as negative controls. After 3 h recovery at 26°C, the bacteria were incubated in ka namycin-containing BHI broth at 37°C, overnight, in a roller drum. Mutants resistant to antimicrobial peptides were then selected on TB-kanamycin agar plates containing 0.2% L-arabinose and supplemented with polymyxin B (4 mg/l, 4 × MIC) or protamine (1 g/l, 1 × MIC on agar plates) after incubation at 37°C for 2–3 days. Colonies were isolated and re sistance to the corresponding cationic antimicrobials was verified by growing the bacteria to an A600 of 0.6 in BHI-kanamycin broth with 0.2% L-arabinose at 37°C and plating in duplicate 0.01 ml onto corresponding cationic antimicrobial selection agar plates. Growth was inspected after incubation at 37°C for 1–3 days. Because of the intrinsic property of Y. pestis to aggregate [67, 68], most consistent absorbance data (A600) were obtained by growing the bacteria in glass tubes and dissociating the aggregated bacteria by strong vortex mixing just before absorbance readings. Bacteria were grown at 37°C to an A600 of 0.3 in 3 ml BHI-kanamycin broth, with 0.2% L-arabinose or 0.2% D-glucose when appropriate to differentiate arabinose-dependent from arabinose-independent resistance. Serial two-fold dilutions of polymyxin B (1.25–5 mg/l) were directly added to such cultures. In contrast, dilutions of protamine (0.2 – 0.8 g/l), rat bronchoalveolar lavage fluid (rBALF, 30 – 240 μg protein/ml), LL-37 (20 – 160 μg/ml) or H2O2 (1 – 32 mM) were added to BHI cultures, prepared as described above and diluted 10-fold. The latter dilutions were needed to use concentrations of inhibitors that did not interfere significantly with A600 readings. The experiments with rBALF were done with 0.5 ml cultures and the ones with LL-37 were done with 0.1 ml cultures in smaller tubes. The bacterial cultures were further incubated in a roller drum or agitated at 37°C for 18 hours, when final A600 values were checked, or CFUs were determined for the LL-37 experiment.
4.4. Determination of MICs
Y. pestis DSY101 and its derived mutants being unable to grow significantly at 37°C in small volumes of cation-adjusted Mueller-Hinton broth (100 μl/well, 96-well microtiter plate; according to the NCCLS, now CLSI, guidelines), MICs were evaluated by the following method. Briefly, bacteria were grown to an A600 of 0.08 – 0.1 in BHI broth at 37°C, diluted 10 fold in BHI (approximately 10 6 CFU/ml), and distributed into round-bottom wells of 96-well microtiter plates (105 CFU/well). Serial two-fold dilutions of the various antimicrobials were prepared in triplicates and MICs were determined after overnight incubation on a rotary shaker at 37°C. MI Cs were defined as the lowest concentration of antimicrobials that inhibited visible growth.
4.5. Southern blotting, subcloning and sequencing of minitransposon insertion sites
To check for single insertions by Southern blotting, genomic DNA was extracted from parental strain Y101 or minitransposon mutants (DNA purification kit, Gentra, USA) and digested with StyI or HpaI and separated on a 0.8% Seakem LE agarose gel. DNA was then transferred to Nytran SPC nylon membranes (GE Healthcare BioSciences Corp., Piscataway, NJ) by the capillary transfer method. A 575-bp coding region of the kanamycin resistance gene that lacks StyI and HpaI sites was amplified from pTn5AraOut with primers PrMK150 and PrMK151 (Table 2), labeled with the DIG High Prime DNA Labeling and Detection Starter Kit II (Roche, Indianapolis, IN) and used for hybridization as described by the supplier. To clone minitransposon insertion sites, genomic DNA of each mutant was digested with either one of a variety of restriction enzymes. Subsequently, the digested DNA was treated with T4 DNA ligase and used to transform E. coli CC118λpir by electroporation. Circularized DNA fragments containing the Tn5AraOut replicated as plasmids, most clones originating from genomic DNA originally restricted with BclI or BamHI. The plasmids were isolated and served as template for DNA sequencing, using a pair of outward-facing primers (pTn5AraOutUP and pTn5AraOutLOW, Table 2) that anneal to the oriR6K or araC-PBAD ends of the minitransposon. The Y. pestis KIM genome [69] was analyzed by BLAST [70] with the obtained sequences to determine the minitransposon insertion sites.
Table 2.
Primers
| Name | Sequence 5′ – 3′ |
|---|---|
| Tn5AraOutUP | tgccatagcatttttatccat |
| Tn5AraOutLOW | aacaagccagggatgtaacg |
| dinP-PrMK140 | ggtaagtttggtcgcgtattgtgg |
| dinP-PrMK141 | atcctcggccagtgttttctcc |
| pmrH-PrMK142 | cgagatcaatggattggtgagcag |
| pmrH-PrMK143 | gaacttaagccgacggactctgg |
| mglB-PrMK144 | gtattgctggctaagggcgtgaaag |
| mglB-PrMK145 | gtagctatccaatgccttgcgagaag |
| 16SrDNA-PrMK146 | gtgtgaagaaggccttcgggttg |
| 16SrDNA-PrMK147 | ttagccggtgcttcttctgcgag |
| rpoB-PrMK148 | tgctgtacaacgcacgtatcatccc |
| rpoB-PrMK149 | caggcaatttacggcgacggtc |
| PrMK150 | tcgggcaatcaggtgcgacaatctat |
| PrMK151 | gtctgcgattccgactcgtccaacat |
| y1522KOUP | aataataagggatggtgtaggccatccccgaataaagtgtaggctggagctgcttc |
| y1522KOLOW | ccctgcatcttgaaggcgacgggtatataaggacatcatatgaatatcctccttag |
| y1522VFUP | tcaccccctgaggatatagat |
| y1522VFLOW | ggatgagcaagggcaactaac |
| y1523KOUP | gaagctgtcctcagtatgaccacgtaggaaaccaggtgcggtgtaggctggagctgcttc |
| y1523KOLOW | tcgccataaccagagcggagcctcagttcttggaacccgtcatatgaatatcctccttag |
| y1523VFUP | caggcgagcggttattctatc |
| y1523VFLOW | ctccatgtcggcttaactgtt |
| feoCKOUP | attgatcacccattagccagccgtaaaaagagggggaacggtgtaggctggagctgcttc |
| feoCKOLOW | atacggaatcaacatattgagatgcccatatgggcatctccatatgaatatcctccttag |
| feoCVFUP | tcacccattagccagccgtaa |
| feoCVFLOW | gctgacgccgaggtttat |
| feoBKOUP | cgcgcagtttgattttaatttattgatatcacgttggatcgtgtaggctggagctgcttc |
| feoBKOLOW | cgttgagggcaatcgcatcacgtagttgcagtaggctggccatatgaatatcctccttag |
| feoBVFUP | ttctatctgcgctacggtttg |
| feoBVFLOW | gctgatggccttcgggaca |
| y1522CMUP | gactcccgggttaatacacgcgatcatcccat |
| y1522CMLOW | gactcgtctcccatgagaatggctaacatgatt |
| feoABCMUP | gactcgtctcccatgcatcttatcccccaacgatcctacaaa |
| feoABCMLOW | gactcccgggtttttacggctggctaatgggtga |
| pETHCP-UP | gactcatatgagaatggctaacatgatt |
| pETHCP-LOW | gactctcgagatacacgcgatcatcccagatgctataaccact |
4.6. Quantitative RT-PCR
HI broth cultures of bacteria grown to log-phase at 37°C were split in two and grown further in the presence of 0.2% arabinose or glucose for 20 minutes. The cells were pelleted at 6000 × g for 10 min at 4°C and RNA was extracted using Trizol reagent (Invitrogen Corp., Carlsbad, CA) according to the manufacturer’s protocol. Residual genomic DNA contamination in 10 μg RNA samples was removed by treating with the Turbo DNA-free Kit (Ambion, Austin, TX). RNA concentration was determined with the ND1000 spectrophotometer (NanoDrop products, Wilmington, DE) and RNA integrity was verified by agarose gel electrophoresis. Four hundred nanogram of RNA was used in reverse transcription reactions using random hexamer primers and Superscript RTIII Reverse Transcriptase (Invitrogen Corp.) according to manufacturer’s protocol. Quantitative Real-Time RT-PCR was carried out using cDNA corresponding to 20 ng RNA, gene-specific primers (Table 2) and the Power SYBR Green PCR Master Mix with the ABI Fast 7500 Real-Time PCR System (Applied Biosystems, Foster City, CA). Expression levels were normalized to the transcription levels for the house keeping gene rpoB [20]. Statistical significance of compared results between the parental strain and mutants or arabinose-induced and non-induced conditions was determined by the unpaired t-test (P < 0.05).
4.7. Preparation and analysis of LPS
LPS was prepared and resolved by SDS-PAGE as described elsewhere [71]. Briefly, overnight bacterial cultures were diluted to an A600 of 0.5, and the cell pellets from 1 ml aliquots were suspended in 50 μl of lysis buffer (2% SDS, 4% 2-mercaptoethanol, 10% glycerol, 1 M Tris-HCl [pH 6.8], 0.002% bromophenol blue). The samples were heated at 100°C for 10 min, cooled to room temperature, and incubated with 25 μg of proteinase K (Roche Diagnostics, Mannheim, Germany) at 60°C for 1 h. The sample preparations were resolved by electrophoresis on a 12% polyacrylamide gel at 150 V, and the gels were silver stained (Silver Stain Kit; Bio-Rad, Hercules, CA).
4.8. Dansyl-polymyxin B binding test
Bacteria were grown at 37°C to an A 600 of approximately 0.3 – 0.4 in 3 ml BHI broth. Bacteria were twice centrifuged and resuspended in PBS, adjusted to an A600 of 0.3 and 3 ml aliquots were concentrated by centrifugation and resuspension in 400μl PBS. Half of this bacterial suspension was supplemented with dansyl-polymyxin B (Molecular Probes, Eugene, OR) to a final concentration of 2 μg/ml, whereas the other half was used as negative control to evaluate background fluorescence. After incubation at 37°C for 5 minutes, the bacteria were centrifuged and washed twice in PBS, resuspended in 400μl PBS and used for fluorescence microscopy or fluorometry. For the latter analysis, the bacterial suspension was transferred to transparent flat-bottom 96-well microtiter plates in triplicate. The A600 and fluorescence values were read with a BioTek’s Synergy™ HT Microplate Reader. The following calculations were done: Standardized fluorescence (arbitrary units or A.U.) value = (fluorescence (A.U.)/A600)test − (fluorescence (A.U.)/A600)control. Data were presented as means ± SD of three separate experiments and statistical significance was determined by the unpaired t-test.
4.9. Construction of deletion mutants and plasmids, and complementation assays
Some of the genes targeted by Tn5AraOut were deleted from strain DSY101 by using the lambda red recombination system [72]. Briefly, primers flanking the corresponding genes were designed and used with pKD4 (Table 2) as template to prepare amplicons for the replacement of the target genes with a kanamycin cassette. Strain DSY101 carrying the lambda red plasmid pSIM9 (Table 1) was grown to log phase at 26°C, the red recombinase genes were induced for 15 min at 42°C, and the bacteria were transformed by electroporation with the gel-purified amplicons. Kanamycin-resistant recombinants were selected on BHI agar and verified by colony PCR, using primers that hybridize to flanking sequences of the target genes. Mutants cured of pSIM9 were selected by bacterial growth at 37°C. Using this ap proach, deletion mutants were engineered for genes y1522(hcp-like), y1523, y3910(feoC) and y3910–3911(feoCB) in strain DSY101, and for gene y3911 in strain KIM5. The resulting strains were designated DSY131, DSY132, DSY135, DSY136 and DSY137, respectively (Table 1). Moreover, genes y1522, or y3911 and y3912(feoA) together, were cloned by PCR into the NcoI-XmaI sites of the expression plasmid pTrc99A for complementation studies. The generated plasmids were designated pHcpy1522 and pFeoAB, respectively (Table 1). Gene y1522 was also cloned by PCR into the NdeI-XhoI restriction sites of pET22b(+) to generate plasmid pETHcp (Table 1). Mutants complemented with plasmid constructs or with the empty vector were grown in BHI broth overnight at 26°C, sub-cultured in BHI with IPTG (0.1 mM) at 37°C and grown for 2–3 h to an A 600 of 0.3. Polymyxin B was added (1.25–5 mg/l) and further growth was monitored (A600) after 18 hours at 37°C.
4.10. Expression and purification of the Hcp-like protein
The Hcp-like protein encoded by y1522 was expressed and purified from E. coli BL21(DE3)pETHcp following the standard protocol (Qiagen, Valencia, CA). The protein antigen was used to prepare polyclonal rabbit antisera (Cocalico Biologicals, Inc.). To determine whether the protein was secreted, bacteria and spent media of a 10 ml culture (BHI, 37°C for 18 h) were studied by SDS-PAGE and W estern blot. For this, spent media were first filtered (Millex, MF-milliporeTM, 0.22 μm, Millipore, Billerica, MA), concentrated to 1 ml (Amicon Ultra-15, 10 kDa, Millipore), precipitated in 10% TCA and the pellet was rinsed twice in 0.5 ml cold acetone before being resuspended in 100 μl sample buffer and split in two for SDS-PAGE and Western blot analysis. The gels were stained with Coomassie Blue and the blots were probed with the specific antibody, HRP-conjugated secondary antibody and enhanced chemiluminescence substrate [73].
4.11. Infection of mice
Six to eight week old female C57BL/6 mice were purchased from the Jackson Laboratories. The mice were provided food and fresh water ad libitum during the experiments, which were performed following the guidelines of the University of Pennsylvania Institutional Animal Care and Use Committee. Bacteria were grown at 26°C, washed two times by centrifugation and suspension steps in sterile PBS. Numbers of colony-forming units (CFU) inoculated were determined by plating serial dilutions onto TB agar plates [48]. Mice were anesthetized (ketamine/xylazin 100/10mg/kg body weight intra-peritoneally, i.p.) and infected subcutaneously (s.c.) with 3×107 CFU each of KIM5 and DSY137 (KIM5 feoB) in 200μl PBS. At days 1, 2, 4 and 5, livers and spleens were surgically removed and homogenized in 5 ml sterile PBS by using a Stomacher Lab Blender (Seward Medical Limited). CFU/organ were determined by plating serial dilutions onto TB agar plates containing or lacking kanamycin. CFUs for KIM5 were calculated by subtracting the DSY137 CFUs (Km plates) from the total CFUs (no antibiotic). Competitive index (C.I.) scores were calculated as the ratio of the KIM5 CFUs to the DSY137 CFUs. Statistical significance was determined by the paired t-test.
Supplementary Material
Supplementary Fig. 1. Southern blots to detect minitransposon insertions in mutant strains. Genomic DNA from the wild type and mutant strains was digested with StyI (A) or HpaI (B) and probed with a 575-bp DIG-labeled probe complementary to the kanamycin resistance gene of Tn5AraOut.
Acknowledgments
We thank Jun (Jay) Zhu and Mark Goulian for plasmids, Sandra Bates for the gifts of rat broncheoalveolar lavage fluid. This work was supported by NIH grant RAI076695, a University of Pennsylvania Research Foundation grant and Research Initiative Funds from the University of Pennsylvania Veterinary Center for Infectious Disease to DMS. JG was a two-year visiting student from Beijing University, supported by the China Scholarship Council (CSC).
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Liu F, Chen H, Galván EM, Lasaro MA, Schifferli DM. Effects of Psa and F1 on the adhesive and invasive interactions of Yersinia pestis with human respiratory tract epithelial cells. Infect Immun. 2006;74:5636–44. doi: 10.1128/IAI.00612-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Huang XZ, Lindler LE. The pH 6 antigen is an antiphagocytic factor produced by Yersinia pestis independent of Yersinia outer proteins and capsule antigen. Infection and immunity. 2004;72:7212–9. doi: 10.1128/IAI.72.12.7212-7219.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Du Y, Rosqvist R, Forsberg A. Role of fraction 1 antigen of Yersinia pestis in inhibition of phagocytosis. Infection and immunity. 2002;70:1453–60. doi: 10.1128/IAI.70.3.1453-1460.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Galván EM, Chen H, Schifferli DM. The Psa fimbriae of Yersinia pestis interact with phosphatidylcholine on alveolar epithelial cells and pulmonary surfactant. Infect Immun. 2007;2007:1272–9. doi: 10.1128/IAI.01153-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cornelis GR. The Yersinia Ysc-Yop ‘type III’ weaponry. Nat Rev Mol Cell Biol. 2002;3:742–52. doi: 10.1038/nrm932. [DOI] [PubMed] [Google Scholar]
- 6.Viboud GI, Bliska JB. Yersinia Outer Proteins: Role in Modulation of Host Cell Signalling Responses and Pathogenesis. Annu Rev Microbiol. 2005;59:69–89. doi: 10.1146/annurev.micro.59.030804.121320. [DOI] [PubMed] [Google Scholar]
- 7.Mukherjee S, Keitany G, Li Y, Wang Y, Ball HL, Goldsmith EJ, et al. Yersinia YopJ acetylates and inhibits kinase activation by blocking phosphorylation. Science. 2006;312:1211–4. doi: 10.1126/science.1126867. [DOI] [PubMed] [Google Scholar]
- 8.Lemaitre N, Sebbane F, Long D, Hinnebusch BJ. Yersinia pestis YopJ suppresses tumor necrosis factor alpha induction and contributes to apoptosis of immune cells in the lymph node but is not required for virulence in a rat model of bubonic plague. Infection and immunity. 2006;74:5126–31. doi: 10.1128/IAI.00219-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Brubaker RR. Interleukin-10 and inhibition of innate immunity to Yersiniae: roles of Yops and LcrV (V antigen) Infection and immunity. 2003;71:3673–81. doi: 10.1128/IAI.71.7.3673-3681.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Depaolo RW, Tang F, Kim I, Han M, Levin N, Ciletti N, et al. Toll-like receptor 6 drives differentiation of tolerogenic dendritic cells and contributes to LcrV-mediated plague pathogenesis. Cell Host Microbe. 2008;4:350–61. doi: 10.1016/j.chom.2008.09.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ye Z, Kerschen EJ, Cohen DA, Kaplan AM, van Rooijen N, Straley SC. Gr1+ Cells Control Growth of YopM-Negative Yersinia pestis during Systemic Plague. Infection and immunity. 2009 doi: 10.1128/IAI.00284-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Montminy SW, Khan N, McGrath S, Walkowicz MJ, Sharp F, Conlon JE, et al. Virulence factors of Yersinia pestis are overcome by a strong lipopolysaccharide response. Nature immunology. 2006;7:1066–73. doi: 10.1038/ni1386. [DOI] [PubMed] [Google Scholar]
- 13.Rebeil R, Ernst RK, Gowen BB, Miller SI, Hinnebusch BJ. Variation in lipid A structure in the pathogenic Yersiniae. Molecular microbiology. 2004;52:1363–73. doi: 10.1111/j.1365-2958.2004.04059.x. [DOI] [PubMed] [Google Scholar]
- 14.Robinson RT, Khader SA, Locksley RM, Lien E, Smiley ST, Cooper AM. Yersinia pestis evades TLR4-dependent induction of IL-12(p40)2 by dendritic cells and subsequent cell migration. J Immunol. 2008;181:5560–7. doi: 10.4049/jimmunol.181.8.5560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Velan B, Bar-Haim E, Zauberman A, Mamroud E, Shafferman A, Cohen S. Discordance in the effects of Yersinia pestis on the dendritic cell functions manifested by induction of maturation and paralysis of migration. Infection and immunity. 2006;74:6365–76. doi: 10.1128/IAI.00974-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zhang P, Skurnik M, Zhang SS, Schwartz O, Kalyanasundaram R, Bulgheresi S, et al. Human DC-SIGN (CD209) is a receptor for Yersinia pestis that promotes phagocytosis by dendritic cells. Infection and immunity. 2008 doi: 10.1128/IAI.01246-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang SS, Park CG, Zhang P, Bartra SS, Plano GV, Klena JD, et al. Plasminogen activator Pla of Yersinia pestis utilizes murine DEC-205 (CD205) as a receptor to promote dissemination. The Journal of biological chemistry. 2008;283:31511–21. doi: 10.1074/jbc.M804646200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cathelyn JS, Crosby SD, Lathem WW, Goldman WE, Miller VL. RovA, a global regulator of Yersinia pestis, specifically required for bubonic plague. Proceedings of the National Academy of Sciences of the United States of America. 2006;103:13514–9. doi: 10.1073/pnas.0603456103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sodeinde OA, Subrahmanyam YV, Stark K, Quan T, Bao Y, Goguen JD. A surface protease and the invasive character of plague. Science. 1992;258:1004–7. doi: 10.1126/science.1439793. [DOI] [PubMed] [Google Scholar]
- 20.Felek S, Tsang TM, Krukonis ES. Three Yersinia pestis adhesins facilitate Yop delivery to eukaryotic cells and contribute to plague virulence. Infection and immunity. 2010;78:4134–50. doi: 10.1128/IAI.00167-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sodeinde OA, Sample AK, Brubaker RR, Goguen JD. Plasminogen activator/coagulase gene of Yersinia pestis is responsible for degradation of plasmid-encoded outer membrane proteins. Infect Immun. 1988;56:2749–52. doi: 10.1128/iai.56.10.2749-2752.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Lahteenmaki K, Virkola R, Saren A, Emody L, Korhonen TK. Expression of plasminogen activator pla of Yersinia pestis enhances bacterial attachment to the mammalian extracellular matrix. Infect Immun. 1998;66:5755–62. doi: 10.1128/iai.66.12.5755-5762.1998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Welkos SL, Friedlander AM, Davis KJ. Studies on the role of plasminogen activator in systemic infection by virulent Yersinia pestis strain C092. Microb Pathog. 1997;23:211–23. doi: 10.1006/mpat.1997.0154. [DOI] [PubMed] [Google Scholar]
- 24.Sebbane F, Jarrett CO, Gardner D, Long D, Hinnebusch BJ. Role of the Yersinia pestis plasminogen activator in the incidence of distinct septicemic and bubonic forms of flea-borne plague. Proceedings of the National Academy of Sciences of the United States of America. 2006;103:5526–30. doi: 10.1073/pnas.0509544103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lathem WW, Price PA, Miller VL, Goldman WE. A plasminogen-activating protease specifically controls the development of primary pneumonic plague. Science. 2007;315:509–13. doi: 10.1126/science.1137195. [DOI] [PubMed] [Google Scholar]
- 26.Kerschen EJ, Cohen DA, Kaplan AM, Straley SC. The plague virulence protein YopM targets the innate immune response by causing a global depletion of NK cells. Infection and immunity. 2004;72:4589–602. doi: 10.1128/IAI.72.8.4589-4602.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Endsley JJ, Torres AG, Gonzales CM, Kosykh VG, Motin VL, Peterson JW, et al. Comparative Antimicrobial Activity of Granulysin against Bacterial Biothreat Agents. Open Microbiol J. 2009;3:92–6. doi: 10.2174/1874285800903010092. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Peschel A, Sahl HG. The co-evolution of host cationic antimicrobial peptides and microbial resistance. Nat Rev Microbiol. 2006;4:529–36. doi: 10.1038/nrmicro1441. [DOI] [PubMed] [Google Scholar]
- 29.Nizet V. Antimicrobial peptide resistance mechanisms of human bacterial pathogens. Curr Issues Mol Biol. 2006;8:11–26. [PubMed] [Google Scholar]
- 30.Higuchi K, Carlin CE. Studies on the nutrition and physiology of Pasteurella pestis. I. A casein hydrolyzate medium for the growth of Pasteurella pestis. Journal of bacteriology. 1957;73:122–9. doi: 10.1128/jb.73.1.122-129.1957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Winfield MD, Latifi T, Groisman EA. Transcriptional regulation of the 4-amino-4-deoxy-L-arabinose biosynthetic genes in Yersinia pestis. The Journal of biological chemistry. 2005;280:14765–72. doi: 10.1074/jbc.M413900200. [DOI] [PubMed] [Google Scholar]
- 32.Yan A, Guan Z, Raetz CR. An undecaprenyl phosphate-aminoarabinose flippase required for polymyxin resistance in Escherichia coli. The Journal of biological chemistry. 2007;282:36077–89. doi: 10.1074/jbc.M706172200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Bingle LE, Bailey CM, Pallen MJ. Type VI secretion: a beginner’s guide. Curr Opin Microbiol. 2008;11:3–8. doi: 10.1016/j.mib.2008.01.006. [DOI] [PubMed] [Google Scholar]
- 34.Misra R, Miao Y. Molecular analysis of asmA, a locus identified as the suppressor of OmpF assembly mutants of Escherichia coli K-12. Molecular microbiology. 1995;16:779–88. doi: 10.1111/j.1365-2958.1995.tb02439.x. [DOI] [PubMed] [Google Scholar]
- 35.Xiong X, Deeter JN, Misra R. Assembly-defective OmpC mutants of Escherichia coli K-12. Journal of bacteriology. 1996;178:1213–5. doi: 10.1128/jb.178.4.1213-1215.1996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Deng M, Misra R. Examination of AsmA and its effect on the assembly of Escherichia coli outer membrane proteins. Molecular microbiology. 1996;21:605–12. doi: 10.1111/j.1365-2958.1996.tb02568.x. [DOI] [PubMed] [Google Scholar]
- 37.Gottesman S. Proteolysis in bacterial regulatory circuits. Annu Rev Cell Dev Biol. 2003;19:565–87. doi: 10.1146/annurev.cellbio.19.110701.153228. [DOI] [PubMed] [Google Scholar]
- 38.Inagawa T, Kato J, Niki H, Karata K, Ogura T. Defective plasmid partition in ftsH mutants of Escherichia coli. Mol Genet Genomics. 2001;265:755–62. doi: 10.1007/s004380100488. [DOI] [PubMed] [Google Scholar]
- 39.Langklotz S, Schakermann M, Narberhaus F. Control of lipopolysaccharide biosynthesis by FtsH-mediated proteolysis of LpxC is conserved in enterobacteria but not in all gram-negative bacteria. Journal of bacteriology. 2011;193:1090–7. doi: 10.1128/JB.01043-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Jackson RJ, Binet MR, Lee LJ, Ma R, Graham AI, McLeod CW, et al. Expression of the PitA phosphate/metal transporter of Escherichia coli is responsive to zinc and inorganic phosphate levels. FEMS Microbiol Lett. 2008;289:219–24. doi: 10.1111/j.1574-6968.2008.01386.x. [DOI] [PubMed] [Google Scholar]
- 41.Willsky GR, Malamy MH. Characterization of two genetically separable inorganic phosphate transport systems in Escherichia coli. Journal of bacteriology. 1980;144:356–65. doi: 10.1128/jb.144.1.356-365.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Richarme G, Caldas TD. Chaperone properties of the bacterial periplasmic substrate-binding proteins. The Journal of biological chemistry. 1997;272:15607–12. doi: 10.1074/jbc.272.25.15607. [DOI] [PubMed] [Google Scholar]
- 43.Semsey S, Krishna S, Sneppen K, Adhya S. Signal integration in the galactose network of Escherichia coli. Molecular microbiology. 2007;65:465–76. doi: 10.1111/j.1365-2958.2007.05798.x. [DOI] [PubMed] [Google Scholar]
- 44.Tommassen J, Eiglmeier K, Cole ST, Overduin P, Larson TJ, Boos W. Characterization of two genes, glpQ and ugpQ, encoding glycerophosphoryl diester phosphodiesterases of Escherichia coli. Mol Gen Genet. 1991;226:321–7. doi: 10.1007/BF00273621. [DOI] [PubMed] [Google Scholar]
- 45.Cartron ML, Maddocks S, Gillingham P, Craven CJ, Andrews SC. Feo--transport of ferrous iron into bacteria. Biometals. 2006;19:143–57. doi: 10.1007/s10534-006-0003-2. [DOI] [PubMed] [Google Scholar]
- 46.Zhou D, Qin L, Han Y, Qiu J, Chen Z, Li B, et al. Global analysis of iron assimilation and fur regulation in Yersinia pestis. FEMS Microbiol Lett. 2006;258:9–17. doi: 10.1111/j.1574-6968.2006.00208.x. [DOI] [PubMed] [Google Scholar]
- 47.Dürr UH, Sudheendra US, Ramamoorthy A. LL-37, the only human member of the cathelicidin family of antimicrobial peptides. Biochim Biophys Acta. 2006;1758:1408–25. doi: 10.1016/j.bbamem.2006.03.030. [DOI] [PubMed] [Google Scholar]
- 48.Galván EM, Lasaro MA, Schifferli DM. Capsular antigen fraction 1 and Pla modulate the susceptibility of Yersinia pestis to pulmonary antimicrobial peptides such as cathelicidin. Infection and immunity. 2008;76:1456–64. doi: 10.1128/IAI.01197-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Groisman EA, Parra-Lopez C, Salcedo M, Lipps CJ, Heffron F. Resistance to host antimicrobial peptides is necessary for Salmonella virulence. Proc Natl Acad Sci U S A. 1992;89:11939–43. doi: 10.1073/pnas.89.24.11939. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Parra-Lopez C, Baer MT, Groisman EA. Molecular genetic analysis of a locus required for resistance to antimicrobial peptides in Salmonella typhimurium. Embo J. 1993;12:4053–62. doi: 10.1002/j.1460-2075.1993.tb06089.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Peschel A, Otto M, Jack RW, Kalbacher H, Jung G, Gotz F. Inactivation of the dlt operon in Staphylococcus aureus confers sensitivity to defensins, protegrins, and other antimicrobial peptides. The Journal of biological chemistry. 1999;274:8405–10. doi: 10.1074/jbc.274.13.8405. [DOI] [PubMed] [Google Scholar]
- 52.Pukatzki S, McAuley SB, Miyata ST. The type VI secretion system: translocation of effectors and effector-domains. Curr Opin Microbiol. 2009;12:11–7. doi: 10.1016/j.mib.2008.11.010. [DOI] [PubMed] [Google Scholar]
- 53.Leiman PG, Basler M, Ramagopal UA, Bonanno JB, Sauder JM, Pukatzki S, et al. Type VI secretion apparatus and phage tail-associated protein complexes share a common evolutionary origin. Proceedings of the National Academy of Sciences of the United States of America. 2009 doi: 10.1073/pnas.0813360106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Pieper R, Huang ST, Robinson JM, Clark DJ, Alami H, Parmar PP, et al. Temperature and growth phase influence the outer-membrane proteome and the expression of a type VI secretion system in Yersinia pestis. Microbiology (Reading, England) 2009;155:498–512. doi: 10.1099/mic.0.022160-0. [DOI] [PubMed] [Google Scholar]
- 55.Robinson JB, Telepnev MV, Zudina IV, Bouyer D, Montenieri JA, Bearden SW, et al. Evaluation of a Yersinia pestis mutant impaired in a thermoregulated type VI-like secretion system in flea, macrophage and murine models. Microbial pathogenesis. 2009;47:243–51. doi: 10.1016/j.micpath.2009.08.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Perry RD, Mier I, Jr, Fetherston JD. Roles of the Yfe and Feo transporters of Yersinia pestis in iron uptake and intracellular growth. Biometals. 2007;20:699–703. doi: 10.1007/s10534-006-9051-x. [DOI] [PubMed] [Google Scholar]
- 57.Imlay JA. Cellular defenses against superoxide and hydrogen peroxide. Annu Rev Biochem. 2008;77:755–76. doi: 10.1146/annurev.biochem.77.061606.161055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Pieper R, Huang ST, Parmar PP, Clark DJ, Alami H, Fleischmann RD, et al. Proteomic analysis of iron acquisition, metabolic and regulatory responses of Yersinia pestis to iron starvation. BMC Microbiol. 2010;10:30. doi: 10.1186/1471-2180-10-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Bearden SW, Perry RD. The Yfe system of Yersinia pestis transports iron and manganese and is required for full virulence of plague. Molecular microbiology. 1999;32:403–14. doi: 10.1046/j.1365-2958.1999.01360.x. [DOI] [PubMed] [Google Scholar]
- 60.Bliska JB, Casadevall A. Intracellular pathogenic bacteria and fungi--a case of convergent evolution? Nat Rev Microbiol. 2009;7:165–71. doi: 10.1038/nrmicro2049. [DOI] [PubMed] [Google Scholar]
- 61.Arafah S, Rosso ML, Rehaume L, Hancock RE, Simonet M, Marceau M. An iron-regulated LysR-type element mediates antimicrobial peptide resistance and virulence in Yersinia pseudotuberculosis. Microbiology (Reading, England) 2009;155:2168–81. doi: 10.1099/mic.0.026690-0. [DOI] [PubMed] [Google Scholar]
- 62.Bader MW, Sanowar S, Daley ME, Schneider AR, Cho U, Xu W, et al. Recognition of antimicrobial peptides by a bacterial sensor kinase. Cell. 2005;122:461–72. doi: 10.1016/j.cell.2005.05.030. [DOI] [PubMed] [Google Scholar]
- 63.Rebeil R, Ernst RK, Jarrett CO, Adams KN, Miller SI, Hinnebusch BJ. Characterization of late acyltransferase genes of Yersinia pestis and their role in temperature-dependent lipid A variation. Journal of bacteriology. 2006;188:1381–8. doi: 10.1128/JB.188.4.1381-1388.2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Marceau M, Sebbane F, Ewann F, Collyn F, Lindner B, Campos MA, et al. The pmrF polymyxin-resistance operon of Yersinia pseudotuberculosis is upregulated by the PhoP-PhoQ two-component system but not by PmrA-PmrB, and is not required for virulence. Microbiology (Reading, England) 2004;150:3947–57. doi: 10.1099/mic.0.27426-0. [DOI] [PubMed] [Google Scholar]
- 65.Judson N, Mekalanos JJ. TnAraOut, a transposon-based approach to identify and characterize essential bacterial genes. Nature biotechnology. 2000;18:740–5. doi: 10.1038/77305. [DOI] [PubMed] [Google Scholar]
- 66.Larsen RA, Wilson MM, Guss AM, Metcalf WW. Genetic analysis of pigment biosynthesis in Xanthobacter autotrophicus Py2 using a new, highly efficient transposon mutagenesis system that is functional in a wide variety of bacteria. Arch Microbiol. 2002;178:193–201. doi: 10.1007/s00203-002-0442-2. [DOI] [PubMed] [Google Scholar]
- 67.Felek S, Lawrenz MB, Krukonis ES. The Yersinia pestis autotransporter YapC mediates host cell binding, autoaggregation and biofilm formation. Microbiology (Reading, England) 2008;154:1802–12. doi: 10.1099/mic.0.2007/010918-0. [DOI] [PubMed] [Google Scholar]
- 68.Kolodziejek AM, Sinclair DJ, Seo KS, Schnider DR, Deobald CF, Rohde HN, et al. Phenotypic characterization of OmpX, an Ail homologue of Yersinia pestis KIM. Microbiology (Reading, England) 2007;153:2941–51. doi: 10.1099/mic.0.2006/005694-0. [DOI] [PubMed] [Google Scholar]
- 69.Deng W, Burland V, Plunkett G, 3rd, Boutin A, Mayhew GF, Liss P, et al. Genome sequence of Yersinia pestis KIM. J Bacteriol. 2002;184:4601–11. doi: 10.1128/JB.184.16.4601-4611.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Cummings L, Riley L, Black L, Souvorov A, Resenchuk S, Dondoshansky I, et al. Genomic BLAST: custom-defined virtual databases for complete and unfinished genomes. FEMS Microbiol Lett. 2002;216:133–8. doi: 10.1111/j.1574-6968.2002.tb11426.x. [DOI] [PubMed] [Google Scholar]
- 71.Hitchcock PJ, Brown TM. Morphological heterogeneity among Salmonella lipopolysaccharide chemotypes in silver-stained polyacrylamide gels. Journal of bacteriology. 1983;154:269–77. doi: 10.1128/jb.154.1.269-277.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Datsenko KA, Wanner BL. One-step inactivation of chromosomal genes in Escherichia coli K-12 using PCR products. Proc Natl Acad Sci U S A. 2000;97:6640–5. doi: 10.1073/pnas.120163297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Chen H, Schifferli DM. Mucosal and systemic immune responses to chimeric fimbriae expressed by Salmonella enterica Serovar Typhimurium vaccine strains. Infect Immun. 2000;68:3129–39. doi: 10.1128/iai.68.6.3129-3139.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Herrero M, De Lorenzo V, Timmis KN. Transposon vectors containing non-antibiotic resistance selection markers for cloning and stable chromosomal insertion of foreign genes in gram-negative bacteria. J Bacteriol. 1990;172:6557–67. doi: 10.1128/jb.172.11.6557-6567.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Goguen JD, Yother J, Straley SC. Genetic analysis of the low calcium response in Yersinia pestis mu d1(Ap lac) insertion mutants. Journal of bacteriology. 1984;160:842–8. doi: 10.1128/jb.160.3.842-848.1984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Simons RW, Houman F, Kleckner N. Improved single and multicopy lac-based cloning vectors for protein and operon fusions. Gene. 1987;53:85–96. doi: 10.1016/0378-1119(87)90095-3. [DOI] [PubMed] [Google Scholar]
- 77.Datta S, Costantino N, Court DL. A set of recombineering plasmids for gram-negative bacteria. Gene. 2006;379:109–15. doi: 10.1016/j.gene.2006.04.018. [DOI] [PubMed] [Google Scholar]
- 78.Amann E, Ochs B, Abel KJ. Tightly regulated tac promoter vectors useful for the expression of unfused and fused proteins in Escherichia coli. Gene. 1988;69:301–15. doi: 10.1016/0378-1119(88)90440-4. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary Fig. 1. Southern blots to detect minitransposon insertions in mutant strains. Genomic DNA from the wild type and mutant strains was digested with StyI (A) or HpaI (B) and probed with a 575-bp DIG-labeled probe complementary to the kanamycin resistance gene of Tn5AraOut.