Uncertainty of diagnosis can weigh heavily on the patient, and perceptions of what medical personnel may consider a minor procedure do not necessarily reflect the patient’s experience.
Abstract
Purpose:
To assess the level of distress in women awaiting radiologic procedures.
Materials and Methods:
In this institutional review board–approved and HIPAA-compliant study, 214 women between 18 and 86 (mean, 47.9) years of age completed the State Trait Anxiety Inventory (STAI), Impact of Events Scale (IES), Center for Epidemiologic Studies Depression Scale (CES-D), and Perceived Stress Scale (PSS) immediately prior to their procedures. One hundred twelve women awaited breast biopsy; 42, hepatic chemoembolization for cancer; and 60, uterine fibroid embolization. Data were analyzed with multivariate analysis of variance and post hoc Tukey tests. Results are reported as means and 95% confidence intervals (CIs).
Results:
All three patient groups experienced abnormally high mean PSS, IES, and CES-D scores, but only the breast biopsy group had highly abnormal anxiety levels. Breast biopsy patients had a significantly higher mean STAI score of 48 (95% CI: 45, 50) than did women awaiting hepatic chemoembolization (mean score, 26; 95% CI: 22, 29; P < .001) and fibroid embolization (mean score, 24; 95% CI: 21, 27; P < .001). IES ratings did not differ significantly among the groups, with a mean score of 26 (95% CI: 23, 29) for breast biopsy patients, 23 (95% CI: 18, 28) for hepatic chemoembolization patients, and 23 (95% CI: 18, 27) for fibroid embolization patients. The CES-D score did not differ significantly among breast biopsy (mean score, 15; 95% CI: 13, 17), hepatic chemoembolization (mean score, 14; 95% CI: 11, 18), and fibroid embolization (mean score, 12; 95% CI: 9, 15) patients. PSS ratings of breast biopsy patients were significantly higher (mean score, 18; 95% CI: 16, 19) than those of hepatic chemoembolization patients (mean, 15; 95% CI: 13, 17; P < .01), but they were not significantly different from those of women awaiting fibroid embolization (mean, 16; 95% CI: 14, 18; P = .23).
Conclusion:
Uncertainty of diagnosis can be associated with greater stress than is awaiting more invasive and potentially risky treatment.
© RSNA, 2011
Introduction
Greater patient comfort and less invasiveness are the promise of newer diagnostic and therapeutic imaging procedures in radiology. The prevailing reliance on technical solutions, however, may distract from the psychological, emotional, or subjective aspects of the patient encounter (1). While many of the image-guided interventions, such as large-core breast biopsy or angioplasty for example, are “minimally invasive,” as compared with their alternative open surgical methods, their anticipation still can evoke an array of distressing emotions (2–6). Patients awaiting therapeutic procedures commonly report anxiety (7), fears about the unknown, pain, possibility of further interventions, complications, destruction of body image, disruption of life plans, loss of control, disability, and loss of life (8). One might assume that diagnostic tests, which typically carry fewer risks than invasive therapeutic procedures, would create less distress. Diagnostic tests, however, inherently harbor uncertainty, which can be a potent stressor and has been linked to poor coping with health-related issues, as well as poor adaptation and recovery (9).
Untreated distress not only has its human toll for the patient, but also considerably taxes departmental resources in terms of appointment cancellations, patients’ lack of cooperation, extended room times, increased medication use, prolonged recovery, and inability to complete imaging procedures well or at all, with adverse impact on both image quality and reimbursement (6,10–14).
Addressing patients’ distress efficiently requires knowledge about when and for whom intervention would be the most needed and effective. Yet, comparative assessment of psychological distress in conjunction with imaging procedures has been difficult to achieve, to our knowledge. Our study therefore took advantage of the availability of preprocedural surveys from two large prospective randomized controlled trials that were performed in radiology with patients at various stages of diagnosis (3–5). We compared distress levels in women awaiting large-core breast biopsy for diagnosis of suspicious lesions with distress levels of women undergoing invasive, potentially risky treatment of diagnosed malignancies of the liver (hepatic chemoembolization) and those undergoing invasive, potentially risky treatment of diagnosed benign uterine tumors (fibroid embolization). The null hypothesis was that there would be no differences in the distress levels among the three patient groups, as measured with standardized psychological questionnaires. This assessment is a first step in the comparative evaluation of stressors in the radiology department, and the results of such an evaluation then can help guide specific interventions toward better outcomes.
Materials and Methods
Participants
Participants were recruited through the radiology department of an urban, tertiary, university-affiliated medical center (Beth Israel Deaconess Medical Center, Boston, Mass) during the course of two large prospective randomized trials on assessment of the efficacy of guidance in self-hypnotic relaxation methods during and after large-core breast biopsy or embolization of benign fibroids and malignant liver tumors. The outcomes of the intra- and postprocedural components of these studies were reported separately (3–5). For our current study, only the patients’ preprocedural questionnaires, which were obtained prior to randomization and prior to the patient’s entering the examination room, were used as outcome measures.
The institutional review board of our institution (Beth Israel Deaconess Medical Center) approved the studies. Health Insurance Portability and Accountability Act regulations were met. Eligible participants had to be able to hear and understand English and meet the inclusion criteria for mental functioning, as assessed through the Mini-Mental State Examination (15) and Schedule for Affective Disorders and Schizophrenia (16). In addition, the following exclusions were applied to fibroid embolization patients: pregnancy, body weight less than 55 kg, severe chronic obstructive pulmonary disease, home use of oxygen, and intolerance to midazolam or fentanyl.
Procedures
Consents for the diagnostic and therapeutic procedures were obtained by the primary operating physicians and medical personnel and included senior residents, fellows, radiology attending physicians, physician assistants, and nurse practitioners between the ages of approximately 26 and 57 years of age. They explained to the patients what would be done; answered questions pertaining to the medical aspects, risks, and alternatives; and obtained signed informed consent. Consent for breast biopsy included information about mainly risks of bleeding, infection, and inability to obtain a final diagnosis. Consent for both hepatic chemoembolization and fibroid embolization procedures included information about mainly contrast agent allergy, explanation of the postembolization syndrome with possible fever and discomfort, sepsis, vascular injury, nontarget embolization, and possible need for subsequent surgery. Liver cancer patients received additional information about the side effects of chemotherapy. For embolization patients, the consent form also included the possibility that they may be given sedatives, with “risks including (but not limited to) allergic reactions, drug reactions, bleeding, blood clots, breathing problems which in rare instances may require a breathing tube, nerve injury, brain damage, infection, or loss of bodily function or life.” Complications with breast biopsy are self-contained and not life-threatening—unless the lung or heart were punctured in careless hands and the operator were unable to remedy the situation or get help—events so rare that they are not included in the consent. With embolizations, however, there is a real, albeit small risk to life and limb which is included in the consent. Patients, in general, had some preprocedural counseling either at a preprocedural visit in the Interventional Radiology or Liver Center Clinic, or at the conclusion of the diagnostic mammogram when the breast radiologist would explain the need for the breast biopsy and how it is performed.
Consecutive patients who had completed their medical consent were evaluated for study eligibility by a research assistant. The research assistant asked consecutive eligible patients to participate in a study in which the effect of a self-hypnotic relaxation exercise on the intra- and postprocedural experience would be assessed. Patients were informed that they would be randomized to three treatment groups and that their chances were one in three of being in a standard care group, an attention group in which an additional person would sit with them during the procedure, or a self-hypnotic relaxation group in which a person would sit with them and read a hypnosis script. All patients were assured that they would receive a local anesthetic. While breast biopsy patients would receive a local anesthetic only, patients in the embolization study were also assured that they could receive as much medication as they wished within the realm of safety. Patients were also asked to fill out four questionnaires prior to their randomization.
Patients who consented were handed identical stacks of four standardized psychological questionnaires: the State Trait Anxiety Inventory (STAI), Impact of Events Scale (IES), Center for Epidemiologic Studies Depression Scale (CES-D), and Perceived Stress Scale (PSS) under the supervision of trained research assistants who were physicians, medical students, or premedical students with a background in mental health services. Patients were at liberty with regard to the sequence in which they would fill out the questionnaires.
Outcome Measures
State Trait Anxiety Inventory.—The STAI is one of the most commonly used instruments to measure anxiety in both clinical and research settings (17). This measure is used to differentiate between long-standing trait and temporary state anxiety. For the purpose of this study, state anxiety was assessed. The State Anxiety form of this self-report questionnaire (State Anxiety Inventory S-Form) refers to the intensity of anxiety experienced in reaction to a specific event at a given time, assessing “feelings of apprehension, tension, nervousness, and worry.” It is a 20-item self-rating instrument with scores as follows: score 1, not at all; score 2, somewhat; score 3, moderately so; and score 4, very much so. Eleven of these questions express presence of anxiety (eg, “I am tense,” “I feel strained,” “I am jittery”), and nine describe absence of anxiety (eg, “I feel calm,” “I feel self-confident,” “I feel at ease”). The latter statements are reverse scored, and thus the highest possible anxiety score is 80. For women who are 45–49 years of age, Spielberger et al report a mean score of 35.9 and a standard deviation of 11.9 (17).
Impact of Events Scale.—The IES is a measure of subjective distress for any specific life event (18). This 15-item self-report instrument is used to assess experiences of intrusive thoughts (Intrusion subscale) and attempts to consciously avoid such experiences (Avoidance subscale) that are commonly associated with subjective distress about life situations. Answers are given in four ratings from not at all (score 0) to often (score 5), with a possible range from zero to 75. Horowitz identified threshold levels for low clinical concern as total IES scores of less than 8.5; he considered scores of 8.6–19.0 as levels for medium concern and scores of greater than 19.0 as levels for high concern and warranting further evaluation (19).
Center for Epidemiologic Studies Depression Scale.—The CES-D was developed by Radloff (20) to study the epidemiology of depression in the general population and addresses four components: depressed affect, reduced positive affect, somatic symptoms, and interpersonal problems. The CES-D contains 20 items, which are rated from zero to three on a four-point system, with total scores between zero and 60. Sixteen items query negative experiences such as depressed mood and feelings of guilt, worthlessness, and helplessness, and four items investigate level of positive affect and sense of well-being, which are reverse scored. In Radloff’s original article, mean scores relating to absence versus presence of certain life events were around eight versus 11 for absence versus presence of illness or injury; eight versus 17 for absence versus presence of separation; and 8.5 versus 17 for married versus widowed status. Scores of 16 or greater are traditionally interpreted as suggestive of clinically significant depression (21).
Perceived Stress Scale.—The PSS is used to measure the degree to which situations in one’s life are appraised as stressful (22). The original PSS contained 14 questions; subsequently, the authors found 10 questions adequate (23). In the 10-item version, patients rate their perception of their lives as unpredictable, uncontrollable, or overloading, with a score as follows: score 0, never, and score 4, very often. The PSS, which originally addressed the preceding month, was adapted to pertain to the week preceding the radiology visit. Although there is overlap with measures of psychological distress (particularly depressive symptoms), PSS scores are considered better predictors of physical symptoms and health services use in the subsequent weeks (22). The maximal score is 40. The normative mean and standard deviation for women between 45 and 54 years of age are 12.6 and 6.1, respectively.
Statistical Analysis
Sample size was determined to assess how many enrolled patients would be needed to detect a moderate effect size (difference of approximately 0.5 standard deviation) for three groups and four outcome measures. The results of a power analysis (α level = .05; β level = .2; power, 0.80) indicated that a sample of approximately 168 participants was required to conduct a multivariate analysis of variance.
All data were coded and entered into a software program (SPSS, version 15; SPSS, Chicago, Ill) for further analysis. We conducted a multivariate analysis of variance with regard to four domains of psychological distress: state anxiety (STAI), impact of events (IES), depressive mood (CES-D), and perceived stress (PSS). Because the overall multivariate analysis of variance was significant, these were followed by analysis of main effects within each domain. To clarify differences among the three patient groups, post hoc Tukey Honestly Significantly Different tests were performed. Results are reported as means and 95% confidence intervals (CIs).
Results
Patients
Between February 2002 and June 2006, 551 women awaiting the targeted radiology procedures were assessed for eligibility to enroll. The Figure shows the patient flow profile. Of these, 362 met inclusion criteria for the current study, and 214 filled out all four questionnaires.
Participant flow.
The final patient population included 112 women awaiting breast biopsy and 102 women awaiting fibroid embolization. Because the hepatic chemoembolization group was the only group that included male participants in the original sample, male participants in this group were excluded to create a more coherent, albeit smaller, sample of 42 women with known hepatic malignancy.
Patient characteristics are shown in Table 1. There were no significant differences in age or patient weight among the groups.
Table 1.
Sample Characteristics
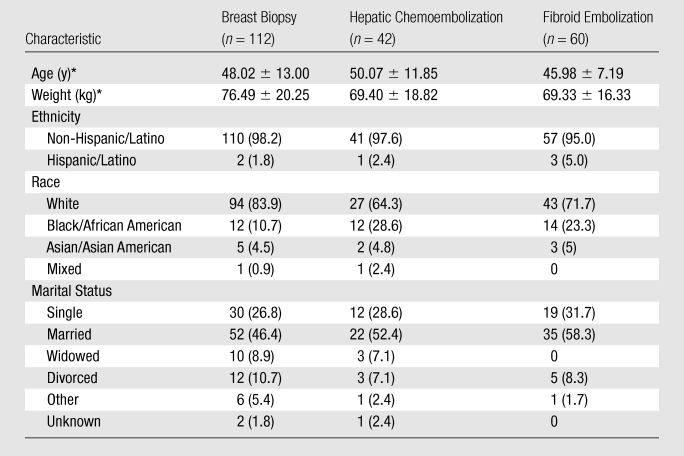
Note.—Data are numbers of patients, and numbers in parentheses are percentages except where otherwise specified.
Data are means ± standard deviations.
Overall Group Differences
Multivariate analysis of variance showed significant group differences for overall psychological distress (F = 23.49; df = 8, 416; P < .001), with the following results for the four domains: (a) for state anxiety (STAI), F = 87.85, with df = 2, 211 and P < .001; (b) for impact of events (IES), F = 0.93, with df = 2, 211 and P = .4; (c) for depressive mood (CES-D), F = 1.82, with df = 2, 211 and P = .17; and (d) for perceived stress (PSS), F = 3.68, with df = 2, 211 and P = .03. Table 2 shows the results of the subsequent Tukey tests and comparative normative values from the literature.
Table 2.
Outcome Measures
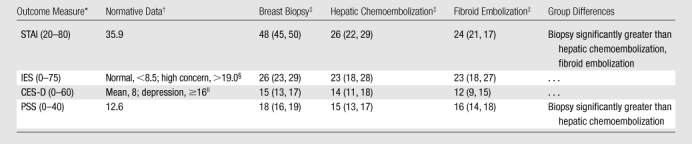
Note.—All four scales are structured such that the lower the ratings, the less distress.
Numbers in parentheses are ranges of possible scores.
Data are mean scores. Numbers in parentheses are 95% CIs.
Normal refers to values at threshold levels for low clinical concern (< 8.5). Values at threshold levels for high concern indicate that further evaluation should be performed.
Depression refers to clinically significant depression.
STAI Scores
Breast biopsy patients reported significantly higher levels of anxiety, with a mean STAI score of 48 (95% CI: 45, 50), than did women awaiting hepatic chemoembolization, with a mean STAI score of 26 (95% CI: 22, 29) (P < .001) and women awaiting fibroid embolization, with a mean STAI score of 24 (95% CI: 21, 27) (P < .001).
IES Ratings
For all groups, mean impact of events ratings were in the range considered of high clinical concern above the cutoff of 19 but were not significantly different among the three groups. The mean IES score was 26 (95% CI: 23, 29) for breast biopsy patients, 23 (95% CI: 18, 28) for hepatic chemoembolization patients, and 23 (95% CI: 18, 27) for fibroid embolization patients.
CES-D Scores
Overall depressive mood levels prior to the procedure were not significantly different for the three groups; the mean CES-D score was 15 (95% CI: 13, 17) for breast biopsy patients, 14 (95% CI: 11, 18) for hepatic chemoembolization patients, and 12 (95% CI: 9, 15) for fibroid embolization patients.
PSS Ratings
The mean PSS score of the breast biopsy patients of 18 (95% CI: 16, 19) was significantly higher than were the scores of hepatic chemoembolization patients, with a mean score of 15 (95% CI: 13, 17; P < .01), but it was not significantly different from the mean score for women awaiting fibroid embolization (score of 16; 95% CI: 14, 18; P = .23).
Discussion
All groups in our study—whether awaiting diagnostic breast biopsy or invasive treatment of malignant liver cancers or of benign uterine fibroids—experienced abnormally high mean levels of perceived stress, impact of events, and depressed mood, but only women awaiting breast biopsy experienced highly abnormal anxiety levels. While anticipatory anxiety surrounding breast biopsy is well described (2,4,24), it was surprising to find in our study that awaiting breast biopsy and diagnosis proved a greater stressor in terms of anxiety and perceived stress than did awaiting much riskier invasive treatment of known cancer and elicited comparable levels of depressive mood and impact on life. This finding suggests that the invasiveness of the procedure has less influence on patients’ distress than does uncertainty of outcome. This result is supported by the finding that stress levels did not differ between women who were treated for known benign disease and those who were treated for known cancer.
The adverse effect of uncertainty was also shown in women undergoing large-core breast biopsy after their biopsy in a different study; women who had not yet heard their diagnosis on the 5th postprocedural day showed highly abnormal patterns of cortisol secretion. Their pattern was significantly different from that of women who had learned they had benign disease and was indistinguishable from that of women who had just learned they had cancer (25). A similar adverse effect of uncertainty about diagnosis on cortisol secretion was also found in a study of men undergoing prostate biopsy (26), suggesting that the results of our current study are not necessarily sex specific.
Literature on uncertainty suggests that this factor may adversely affect adherence to treatment (27). In a study with pediatric patients undergoing transplantation, uncertainty was significantly correlated with anxiety and depressive symptoms, and depressive symptoms correlated inversely with treatment adherence (28). Strategies to address uncertainty by providing interventions for patients early on can reduce negative affect and subsequent adverse consequences (12).
In comparison with breast biopsy patients, the hepatic chemoembolization and fibroid embolization groups had already received a clear diagnosis and had made treatment decisions. While undergoing treatment can hold the perception of danger, it also offers the opportunity to improve symptoms and, in case of cancer, chances of survival.
Social support can greatly affect the distress individuals experience (29,30). Age, weight, and distribution of different marital states were relatively homogeneous among the three groups in our study, but there is a variation in racial composition. To which degree the interaction of cultural and genetic phenomena and expression of disease affect the propensity to distress could not be disentangled in the current sample.
Attention to patient’s acute distress before and during procedures is important because distress may cause hemodynamic instability, procedural complications, and other adverse events (14). Stress and anxiety may cause adverse events through elevated levels of blood pressure, heart rate, coronary constriction, and stress hormones (31). Growing evidence suggests that patients’ preoperative anxiety level is a predictor of the experience of pain and anxiety during procedures (6,10). Patients with negative affect also tend to have longer procedural times than do others, and they request and receive more medication, which may result in an increased likelihood of adverse events (6).
Diagnostic imaging procedures and biopsies (including breast biopsies) are considered minor procedures. Physicians may want to question their own notions about what they consider “minor” because the patient’s subjective experience of events can be quite different (32). Our finding with regard to psychological impact of diagnostic testing as compared with therapeutic procedures concurs with prior evidence in radiology and other domains. Mueller et al (32) observed that diagnostic testing (ie, computed tomography–guided chest or abdominal biopsy) resulted in more anxiety than did more complicated treatments (ie, biliary drainage or cholecystectomy), but it was not clear whether these differences were significant. Previous reports indicate that patients’ experience waiting for and undergoing diagnostic interventions such as cardiac catherization are anxiety provoking, stressful, or even traumatic (33). Male patients undergoing cardiac catherization reported being most distressed from the psychological aspects of testing (ie, uncertainty, fear of the unknown, or potential effects on their future) and not from the technical or physiological aspects of the intervention (34).
A limitation of our study was the inclusion of women only and exclusion of many patients from the original set compared with the final set. While the literature suggests similar adverse effects of uncertainty on cortisol levels in men undergoing prostate biopsy and the just mentioned adverse psychological effects of testing in men undergoing cardiac catheterization, it is not possible to generalize the finding to a male patient population in radiology. Patients undergoing fibroid embolization and hepatic chemoembolization may also experience uncertainty, but mainly about the outcome, because the diagnosis is already known. The groups were based on stage of diagnosis and treatment, not randomization, with patients undergoing breast biopsy representing the purely diagnostic group (eg, not knowing the diagnosis before filling out the questionnaires) and with patients undergoing fibroid embolization or hepatic chemoembolization representing groups who know their diagnosis as benign or malignant before filling out the questionnaires. Compared with the patients in the breast biopsy group, a higher percentage of patients in the fibroid embolization and liver chemoembolization groups filled out all four questionnaires. This may have introduced bias. On the basis of reports of the research assistants, this was mainly due to the impatience of the biopsy team getting patients moving through the department rather than to unwillingness of the women to fill out the questionnaires. As such, wait time for the examination (or lack thereof) may have affected the psychological measures. It is also possible, however, that a higher level of stress in the breast biopsy group may have contributed to this outcome. In addition, the timing between the filling out of the study questionnaires after having been informed about the risks and benefits of the medical procedures may have had an effect on the outcome. It is also unknown how the consent for the initial study assessing the effect of self-hypnotic relaxation on the patient experience may have affected the patients’ perception of distress when they filled out their questionnaires.
Radiologists and other health care professionals are typically not trained, prepared, or available to provide psychological support for patients, although this deficiency can be safely remedied by means of targeted training (13,35,36). Alerting the medical community about the experience of patients at different stages of diagnosis and treatment can be a first step in targeting resource use to better outcomes. These findings have implications for the design, staffing, and resource allocation of waiting areas, particularly for mammography. Specifically, lack of communicative collaboration among radiologists, technologists, and other health care professionals can engender confusion and further anxiety (37). Breast biopsy patients could greatly profit from interventions that reduce anxiety, specifically nonpharmacologic interventions. It has been shown by our group and other investigators that these techniques can be applied across the medical professions represented in the busy biopsy or interventional suite to decrease anxiety, pain, drug use, complications, and procedural time while reducing cost (3,38,39).
We conclude that it would be wise to assume that there is no such thing as a “simple” diagnostic test. Uncertainty of diagnosis can weigh heavily on the patient, and perceptions of what medical personnel may consider “minor” do not necessarily reflect the patient’s experience. Training medical personnel in how to communicate with these patients and to assuage their distress promises not only to relieve the patients’ distress but also to positively affect departmental resources.
Advances in Knowledge.
All patient groups in this study—whether awaiting diagnostic breast biopsy or invasive treatment of malignant liver cancers or benign uterine fibroids—experienced abnormally high mean levels of perceived stress, impact of events, and depressed mood; but only women awaiting breast biopsy experienced highly abnormal anxiety levels.
Awaiting breast biopsy proved a greater stressor in terms of anxiety and perceived stress than awaiting much riskier invasive treatment of known cancer and elicited comparable levels of depressed mood and impact on life.
Stress levels did not differ among embolization patients who were treated for known benign disease and those treated for known cancer.
Findings suggest that the invasiveness of the procedure has less influence on patients’ distress than does uncertainty of outcome.
Implications for Patient Care.
Health care providers are advised to set aside their own notions about “minor” and “major” procedures and appreciate more the distress associated with uncertainty of diagnosis.
There is no such thing as a “simple” diagnostic procedure.
Because patient distress can severely tax the patients and the departmental resources, it is best to provide emotional support early during their visit from radiology teams that are trained in how to diffuse distress.
Disclosures of Potential Conflicts of Interest: N.F. No potential conflicts of interest to disclose. E.V.L. Financial activities related to the present article: none to disclose. Financial activities not related to the present article: founded Hypnalgesics, which is dedicated to train medical teams in communication, Comfort TalkTM, and guidance in self-hypnotic relaxation, and applied for a Small Business Innovation Grant from Hypnalgesics. Other relationships: none to disclose.
Acknowledgments
We are deeply grateful for the time and effort the patients invested in this study.
Received November 17, 2010; revision requested January 5, 2011; final revision received January 10; accepted February 9; final version accepted February 18.
Supported by the U.S. Army Medical Research and Material Command (DAMD 17-01-1-0153) and a Ruth L. Kirschstein National Research Service Award (grant T32-59367).
Funding: This research was supported by the National Institutes of Health (grants RO1 AT-0002-05, K24 AT01074-01, and T32-59367).
Abbreviations:
- CES-D
- Center for Epidemiologic Studies Depression Scale
- CI
- confidence interval
- IES
- Impact of Events Scale
- PSS
- Perceived Stress Scale
- STAI
- State Trait Anxiety Inventory
References
- 1.Peteet JR, Stomper PC, Ross DM, Cotton V, Truesdell P, Moczynski W. Emotional support for patients with cancer who are undergoing CT: semistructured interviews of patients at a cancer institute. Radiology 1992;182(1):99–102 [DOI] [PubMed] [Google Scholar]
- 2.Bugbee ME, Wellisch DK, Arnott IM, et al. Breast core-needle biopsy: clinical trial of relaxation technique versus medication versus no intervention for anxiety reduction. Radiology 2005;234(1):73–78 [DOI] [PubMed] [Google Scholar]
- 3.Lang EV, Benotsch EG, Fick LJ, et al. Adjunctive non-pharmacological analgesia for invasive medical procedures: a randomised trial. Lancet 2000;355(9214):1486–1490 [DOI] [PubMed] [Google Scholar]
- 4.Lang EV, Berbaum KS, Faintuch S, et al. Adjunctive self-hypnotic relaxation for outpatient medical procedures: a prospective randomized trial with women undergoing large core breast biopsy. Pain 2006;126(1-3):155–164 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lang EV, Berbaum KS, Pauker SG, et al. Beneficial effects of hypnosis and adverse effects of empathic attention during percutaneous tumor treatment: when being nice does not suffice. J Vasc Interv Radiol 2008;19(6):897–905 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schupp CJ, Berbaum K, Berbaum M, Lang EV. Pain and anxiety during interventional radiologic procedures: effect of patients’ state anxiety at baseline and modulation by nonpharmacologic analgesia adjuncts. J Vasc Interv Radiol 2005;16(12):1585–1592 [DOI] [PubMed] [Google Scholar]
- 7.Viegas Lde S, Turrini RN, da Silva Bastos Cerullo JA. An analysis of nursing diagnoses for patients undergoing procedures in a Brazilian interventional radiology suite. AORN J 2010;91(5):544–547 [DOI] [PubMed] [Google Scholar]
- 8.Johnston M. Anxiety in surgical patients. Psychol Med 1980;10(1):145–152 [DOI] [PubMed] [Google Scholar]
- 9.Mishel MH. Perceived uncertainty and stress in illness. Res Nurs Health 1984;7(3):163–171 [DOI] [PubMed] [Google Scholar]
- 10.Auerbach SM, Martelli MF, Mercuri LG. Anxiety, information, interpersonal impacts, and adjustment to a stressful health care situation. J Pers Soc Psychol 1983;44(6):1284–1296 [DOI] [PubMed] [Google Scholar]
- 11.Jenkins CD, Stanton BA, Jono RT. Quantifying and predicting recovery after heart surgery. Psychosom Med 1994;56(3):203–212 [DOI] [PubMed] [Google Scholar]
- 12.Kagan I, Bar-Tal Y. The effect of preoperative uncertainty and anxiety on short-term recovery after elective arthroplasty. J Clin Nurs 2008;17(5):576–583 [DOI] [PubMed] [Google Scholar]
- 13.Lang EV, Ward C, Laser E. Effect of team training on patients’ ability to complete MRI examinations. Acad Radiol 2010;17(1):18–23 [DOI] [PubMed] [Google Scholar]
- 14.Martin ML, Lennox PH, Buckley BT. Pain and anxiety: two problems, two solutions. J Vasc Interv Radiol 2005;16(12):1581–1584 [DOI] [PubMed] [Google Scholar]
- 15.Folstein MF, Folstein SE, McHugh PR. “Mini-mental state”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975;12(3):189–198 [DOI] [PubMed] [Google Scholar]
- 16.Endicott J, Spitzer RL. A diagnostic interview: the schedule for affective disorders and schizophrenia. Arch Gen Psychiatry 1978;35(7):837–844 [DOI] [PubMed] [Google Scholar]
- 17.Spielberger CD, Sarason IG, Defares PB. Stress and anxiety. Washington, DC: Hemisphere, 1985; 1–285 [Google Scholar]
- 18.Horowitz M, Wilner N, Alvarez W. Impact of Event Scale: a measure of subjective stress. Psychosom Med 1979;41(3):209–218 [DOI] [PubMed] [Google Scholar]
- 19.Joseph S. Psychometric evaluation of Horowitz’s Impact of Event Scale: a review. J Trauma Stress 2000;13(1):101–113 [DOI] [PubMed] [Google Scholar]
- 20.Radloff LS. The CES-D scale: a self-report depression for research in the general population. Appl Psychol Meas 1977;1(3):385–401 [Google Scholar]
- 21.McDowell I, Newell C. Measuring health: a guide to rating scales and questionnaires. 2nd ed. Oxford, England: Oxford University Press, 1996; 29–37 [Google Scholar]
- 22.Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. J Health Soc Behav 1983;24(4):385–396 [PubMed] [Google Scholar]
- 23.Cohen S, Williamson GM. Perceived stress in a probability sample of the United States. In: Spacapan S, Oskamp S, eds. Social psychology of health. Beverly Hills, Calif: Sage, 1988; 1–257 [Google Scholar]
- 24.Hughson AV, Cooper AF, McArdle CS, Smith DC. Psychosocial morbidity in patients awaiting breast biopsy. J Psychosom Res 1988;32(2):173–180 [DOI] [PubMed] [Google Scholar]
- 25.Lang EV, Berbaum KS, Lutgendorf SK. Large-core breast biopsy: abnormal salivary cortisol profiles associated with uncertainty of diagnosis. Radiology 2009;250(3):631–637 [DOI] [PubMed] [Google Scholar]
- 26.Gustafsson O, Theorell T, Norming U, Perski A, Ohström M, Nyman CR. Psychological reactions in men screened for prostate cancer. Br J Urol 1995;75(5):631–636 [DOI] [PubMed] [Google Scholar]
- 27.Han PK, Moser RP, Klein WM. Perceived ambiguity about cancer prevention recommendations: associations with cancer-related perceptions and behaviours in a US population survey. Health Expect 2007;10(4):321–336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Maikranz JM, Steele RG, Dreyer ML, Stratman AC, Bovaird JA. The relationship of hope and illness-related uncertainty to emotional adjustment and adherence among pediatric renal and liver transplant recipients. J Pediatr Psychol 2007;32(5):571–581 [DOI] [PubMed] [Google Scholar]
- 29.Cohen S, Wills TA. Stress, social support, and the buffering hypothesis. Psychol Bull 1985;98(2):310–357 [PubMed] [Google Scholar]
- 30.Spiegel D, Morrow GR, Classen C, et al. Group psychotherapy for recently diagnosed breast cancer patients: a multicenter feasibility study. Psychooncology 1999;8(6):482–493 [DOI] [PubMed] [Google Scholar]
- 31.Krantz DS, Kop WJ, Santiago HT, Gottdiener JS. Mental stress as a trigger of myocardial ischemia and infarction. Cardiol Clin 1996;14(2):271–287 [PubMed] [Google Scholar]
- 32.Mueller PR, Biswal S, Halpern EF, Kaufman JA, Lee MJ. Interventional radiologic procedures: patient anxiety, perception of pain, understanding of procedure, and satisfaction with medication—a prospective study. Radiology 2000;215(3):684–688 [DOI] [PubMed] [Google Scholar]
- 33.Anderson KO, Masur FT., 3rd Psychologic preparation for cardiac catheterization. Heart Lung 1989;18(2):154–163 [PubMed] [Google Scholar]
- 34.Beckerman A, Grossman D, Marquez L. Cardiac catheterization: the patients’ perspective. Heart Lung 1995;24(3):213–219 [DOI] [PubMed] [Google Scholar]
- 35.Lang EV, Berbaum KS. Educating interventional radiology personnel in nonpharmacologic analgesia: effect on patients’ pain perception. Acad Radiol 1997;4(11):753–757 [DOI] [PubMed] [Google Scholar]
- 36.Lang EV, Laser E, Anderson B, et al. Shaping the experience of behavior: construct of an electronic teaching module in nonpharmacologic analgesia and anxiolysis. Acad Radiol 2002;9(10):1185–1193 [DOI] [PubMed] [Google Scholar]
- 37.Lown BA, Roy E, Gorman P, Sasson JP. Women’s and residents’ experiences of communication in the diagnostic mammography suite. Patient Educ Couns 2009;77(3):328–337 [DOI] [PubMed] [Google Scholar]
- 38.Lang EV, Rosen MP. Cost analysis of adjunct hypnosis with sedation during outpatient interventional radiologic procedures. Radiology 2002;222(2):375–382 [DOI] [PubMed] [Google Scholar]
- 39.Montgomery GH, Bovbjerg DH, Schnur JB, et al. A randomized clinical trial of a brief hypnosis intervention to control side effects in breast surgery patients. J Natl Cancer Inst 2007;99(17):1304–1312 [DOI] [PubMed] [Google Scholar]



