Abstract
Visceral leishmaniasis is a disease caused by a haemoflagellate protozoan of the genus Leishmania. It has a wide geographical spread. Classic cases are found primarily in children and present with typical features that include fever, anaemia, hepatosplenomegaly, hypergammaglobulinaemia, and pancytopenia. The diagnosis is usually achieved by bone marrow smears, culture and serology; however, it can manifest itself atypically, mostly in patients infected with HIV and geriatric immunocompetent patients. We report an unusual case of visceral leishmaniasis diagnosed in a 27 year-old HIV-infected male who presented with abdominal discomfort and diarrhoea of four weeks duration associated with nausea and vomiting, but with no typical symptoms or signs of visceral leishmaniasis. The diagnosis was established through the identification of the Leishmania organism in duodenal and colonic biopsies and confirmed by subsequent bone marrow smears.
Keywords: Visceral leishmaniasis, HIV, Duodenal biopsy, Case report, Iraq
Leishmaniases are a group of zoonotic diseases caused by a haemoflagellate protozoan of the genus Leishmania. The parasites are present in the macrophages of a wide variety of vertebrates. They are transmitted to man from the animal reservoir through the bite of female sand flies of the Phlebotomus species.1 There are several species of Leishmania that can infect human and result in a spectrum of diseases known as leishmaniasis.2 Depending on the mode of presentation there are three main types: cutaneous leishmaniasis, which is often self-limiting, mucosal leishmaniasis and visceral leishmaniasis.3 Visceral leishmaniasis affects mainly the mononuclear phagocytic system of the bone marrow, liver and spleen1 and is caused mainly by Leishmania donovani and Leishmania infantum species.2 It shows a wide geographical spread in more than 88 countries all over the world.4
Clinically, typical cases of visceral leishmaniasis are found primarily in children.4 It’s features include fever, anaemia, hepatosplenomegaly, adenomegaly, hypergammaglobulinaemia, and pancytopenia, but it can also manifest itself atypically, mostly in patients infected with HIV and geriatric immunocompetent patients.5 The definitive diagnosis of visceral leishmaniasis is achieved by identification of the organism in a bone marrow biopsy. The characteristic Leishmania amastigotes are round to ovoid in shape and can be identified after routine haematoxylineosin or Giemsa staining.4,6 Other diagnostic tools include isolation of promastigotes by Novy-McNeal-Nicolle (NNN) culture2,4 and serological tests to detect antileishmanial antibodies, but the latter have low sensitivity.3,4 Histopathological identification of leishmania organisms in tissue sections is quite easy and very sensitive;4 however, the diagnosis of leishmaniasis in paraffin sections may be difficult in some conditions, such as when the parasites are present in unusual sites which is frequently observed in visceral leishmaniasis that develops in immunocompromised patients.2,7 This is a presentation of an unusual case of visceral leishamniasis diagnosed in an HIV-infected patient, with atypical clinical features, who was unexpectedly diagnosed through the identification of the Leishmania organism in an unusual site.
Case report
The patient was a 27 year-old Yemeni male, diagnosed with HIV infection 8 years previously, who presented with abdominal discomfort and diarrhoea of four weeks duration associated with nausea and vomiting, but no fever or anorexia. The diarrhoea (5–6 times a day) was watery and accompanied by mucus, but with no blood. On physical examination, the patient was conscious, oriented, afebrile and not pale. His vital signs were stable. His chest was clear and abdominal examination showed mild subumbilical tenderness, but no abdominal mass or organ enlargement was detected. No lymphadenopathy was present. The patient was not receiving any antiretroviral therapy.
Laboratory investigations showed leukocytes 10.88x103/μl, 83% neutrophils, 8.4% lymphocytes and 8.4% monocytes. The haemoglobin level was 136 g/l, erythrocytes sedimentation rate 16 mm/hour. Urine examination showed mild proteinuria and his serum creatinine was mildly elevated at 2.1 mg/dl. Stool samples were negative for Cryptosporidium and Clostridium difficile toxin and repeated stool culture revealed no pathogens. His CD4 cell count was 210 cells/mm3. An abdominal ultrasound showed no abnormalities. An upper GIT endoscopy showed normal oesophageal and gastric mucosa; however, the mucosa of the second part of the duodenum showed congestion with a peculiar whitish nodular appearance [Figure 1]. A colonoscopy showed normal colonic mucosa. Multiple biopsies were taken from the oesophagus, stomach, duodenum and colon for histopathological examination to exclude microscopic lesions and opportunistic infections.
Figure 1:
Upper GIT endoscopy revealing whitish nodular appearance of the duodenal mucosa.
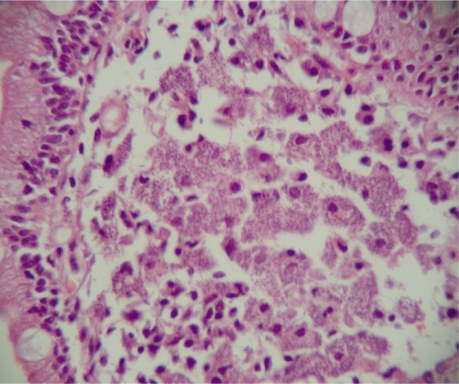
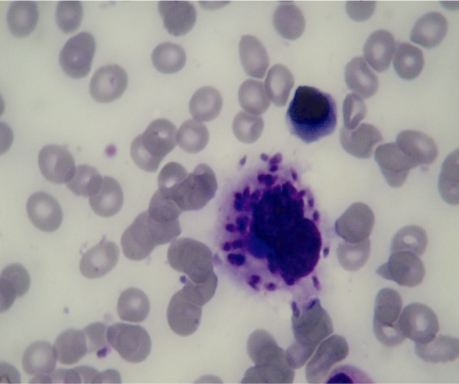
The histopathological examination demonstrated widening of the duodenal villi with infiltration of duodenal and rectal mucosa by a large number of macrophages filled with intracytoplasmic Leishmania amastigote parasites (Donovan bodies) [Figure 2]. Gastric and oesophageal biopsies showed no significant pathologic changes. The case was diagnosed as visceral leishmaniasis. Subsequent bone marrow aspirate (showing Leishman–Donovan bodies) confirmed the diagnosis [Figure 3]. The patient was treated with sodium stibogluconate (20 mg/kg/day), but he was lost to follow-up after 1 week of therapy.
Figure 2:
Duodenal biopsy showing many macrophages with abundant intracytoplasmic leishmaniae.
Figure 3:
Bone marrow aspirate smear revealing intracytoplasmic leishmaniae.
Discussion
Although it affects mainly immunocompetent individuals, Leishmania is considered an opportunistic pathogen in immunosuppressed patients particularly those with AIDS.8,9 On the other hand, HIV infection increases the risk of developing visceral leishmaniasis by 100–1,000 times in endemic areas.10 In fact, some studies showed that visceral leishmaniasis is the fourth most common opportunistic parasitic disease in HIV-positive individuals after pneumocystosis, toxoplasmosis, and cryptosporidiosis.4,10,11 Indeed, both HIV and leishmaniasis result in a cumulative deficiency of the cellular immune response since both agents damage similar immune resources thus promoting chronicity and, when untreated, result in death.6,10 The first case of leishmania/HIV coinfections was diagnosed in 198512 and almost all cases of Leishmania co-infection with HIV have been described in patients with HIV-1.13 According to data from the World Health Organization, HIV-Leishmania co-infection is widely distributed.14 The most common areas are southern European countries (like Spain), and Brazil, India, Bangladesh and Nepal.1,10 The real impact of HIV-Leishmania co-infection is probably underestimated owing to constraints in the surveillance and reporting of cases.
The majority of leishmaniasis cases in HIV-positive patients appear in the advanced stages of the disease. In about 80% of patients, the number of CD4 lymphocytes is less than 200/mm3 while in c. 20 % of patient.1,4,15 In the current case, the number was low (210 cells/mm3). Leishmaniasis has different characteristics in patients with AIDS compared with immunocompetent patients.8 Classic visceral leishmaniasis in immunocompetent individuals is found primarily in children, but in recent years an increasing number of adult cases have been observed mostly in HIV patients.4,5,15–17 In the latter, the location is more likely to be atypical such as gastrointestinal tract, larynx, lungs, kidneys, pancreas and testes.5,6 Organomegaly, which is one of the typical clinical features of classical visceral leishmaniasis in immunocompotent individuals, is usually absent in HIV positive adults3 as in our case. Also cytopenia is more frequent in immunosuppressed individuals along with negative serology and higher relapse rate after therapy. 5,6,8,10 The gastrointestinal involvement and overt malabasorption in visceral leishmaniasis is reported more freqently in those with concomitant HIV infection.3,5,8,18–20 Lesions have been seen from the oesophagus to the rectum;6 however, the duodenum is the most common site.5 The exact pathogenesis of the diarrhoea and malabsorption is not clear, but it has been suggested that these symptoms in enteropathic visceral lesihsmaniasis may be a combination of the mechanical occlusion of the mucosa by parasites, bacterial overgrowth, partial villous atrophy, competition between the host and the parasite for nutrients, altered motility, bile salt deconjugation and lymphatic blockade.3
Endoscopic examination of these patients is usually performed because of diarrhoea and epigastralgia. The findings are variable and may be unremarkable,6,18,21 showing non-specific inflammation,5,22 or an atrophic mucosal pattern.8 In the current case, the mucosa of the second part of the duodenum showed congestion with a peculiar whitish nodular appearance, a rare and unusual finding also reported by others.1 The colonoscopy showed a normal colonic mucosal pattern. Histopathological examination of intestinal (duodenal and colonic) biopsies shows intact architecture and abundant macrophages with intracytoplasmic Leishmania amastigotes (Donovan bodies).5,6,19,22 Some cases may show duodenal villous atrophy.3,22
Conclusion
In conclusion, clinicians should be alert about the possibility of leishmaniasis in HIV positive patients presenting with diarrhoea, particularly in patients from endemic areas. Also pathologists should pay attention to the possible finding of Leishmania amastigotes in biopsies from intestinal mucosa in HIV infected patients.
References
- 1.Del Olmo Martínez L, Aller de la Fuente R, Velayos Jiménez B, Fernández Salazar L, González Hernández JM. Visceral leishmaniasis diagnosed by duodenal biopsy. Gastroenterol Hepatol. 2009;101:439–51. [PubMed] [Google Scholar]
- 2.Hofman V, Borusset P, Mougneau E, Marty P, Lamat L, Antoine JC, et al. Immunostaining of visceral leishmaniasis caused by leishmania infantum using monoclonal antibody (19-11) to the leishmania homologue of receptors for activated c-kinase. Am J Clin Pathol. 2003;120:567–74. doi: 10.1309/R3DK-4MR3-W6E5-PH17. [DOI] [PubMed] [Google Scholar]
- 3.Hicks L, Kant P, Tay PH, Vincini V, Schuster H, Rotimi O, et al. Visceral leishmaniasis presenting with intestinal failure: A case report and literature review. Eur J Gastroenterol Hepatol. 2009;21:117–22. doi: 10.1097/MEG.0b013e32830e6fdb. [DOI] [PubMed] [Google Scholar]
- 4.Alvar J, Canavate C, Gutierrez-Solar B, Jiménez M, Laguna F, López-Vélez R, et al. Leishmania and human immunodeficiency virus co-infection: The first 10 years. Clin Microbiol Rev. 1997;10:298–319. doi: 10.1128/cmr.10.2.298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Alvarez-Nebreda ML, Alvarez-Fernández E, Rada S, Brañas F, Marañón E, Vidán MT, et al. Unusual duodenal presentation of leishmaniasis. J Clin Pathol. 2005;58:1321–2. doi: 10.1136/jcp.2005.027029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kostiuk O, Levi I, Krieger M, Assouline-Dayan Y, Barshack Intestinal leishmaniasis in a patient with AIDS. Isr Med Assoc J. 2006;8:714–15. [PubMed] [Google Scholar]
- 7.Albrecht H, Sobottka I, Emminger C. Visceral leishmaniasis emerging as an important opportunistic infection in HIV infected persons living in areas nonendemic for Leishmania donovani. Arch Pathol Lab Med. 1996;120:189–98. [PubMed] [Google Scholar]
- 8.Ellul P, Piscopo T, Vassallo M. Visceral leishmaniasis diagnosed on duodenal biopsy. Clin Gastroenterol Hepatol. 2007;5:A26. doi: 10.1016/j.cgh.2007.04.026. [DOI] [PubMed] [Google Scholar]
- 9.McBride MO, Fisher M, Skinner CJ, Golden R, Main J. An unusual gastrointestinal presentation of leishmaniasis. Scand J Infect Dis. 1995;27:297–8. doi: 10.3109/00365549509019026. [DOI] [PubMed] [Google Scholar]
- 10.Paredes R, Munoz J, Diaz I, Domingo P, Gurgui M, Clotet B. Leishmaniasis in HIV infection. J Postgrad Med. 2003;49:39–49. doi: 10.4103/0022-3859.929. [DOI] [PubMed] [Google Scholar]
- 11.Montalban C, Calleja JL, Erice A, Laguna F, Clotet B, Podzamczer D, et al. Co-operative Group for the Study of Leishmaniasis in AIDS. Visceral Leishmaniasis in patients infected with human immunodeficiency virus. J Infect. 1990;21:261–70. doi: 10.1016/0163-4453(90)93933-j. [DOI] [PubMed] [Google Scholar]
- 12.De la Loma A, Alvar J, Martínez E, Blázquez J, Alcalá A, Nájera R. Leishmaniasis or AIDS? Trans R Soc Trop Med Hyg. 1985;79:421–2. doi: 10.1016/0035-9203(85)90400-6. [DOI] [PubMed] [Google Scholar]
- 13.Sacramento R, Horta A, Vasconcelos O, Coelho H, Granato C, Rocha A. Leishmaniasis visceral en enfermo infectado por VIH-2. Rev Clin Esp. 1995;195:591–92. [PubMed] [Google Scholar]
- 14.World Health Organization Leishmania/HIV co-infection. Epidemiological analysis of 692 retrospective cases. Wkly Epidemiol Rec. 1997;72:49–54. [PubMed] [Google Scholar]
- 15.Moreno-Camacho A, López-Vélez R, Muñoz Sanz A, Labarga-Echevarría P. Intestinal parasitic infections and leishmaniasis in patients with HIV infection. Enferm Infecc Microbiol Clin. 1998;1:52–60. [PubMed] [Google Scholar]
- 16.Bel Haj Salah M, Mekni A, Khanfir M, Bellil K, Benhaha-Bellil S, Chelly I, et al. Unusual presentation of visceral leishmaniasis in an immunocompetent patient. Med Mal Infect. 2006;36:167–9. doi: 10.1016/j.medmal.2005.11.013. [DOI] [PubMed] [Google Scholar]
- 17.Alvar J. Leishmaniasis and Aids co-infection. The Spanish example. Parasitol Today. 1994;10:160–3. doi: 10.1016/0169-4758(94)90270-4. [DOI] [PubMed] [Google Scholar]
- 18.Baba CS, Makharia GK, Mathur P, Ray R, Gupta SD, Samantaray JC. Chronic diarrhoea and malabsorption caused by Leishmania donavani. Indian J Gastroenterol. 2006;25:309–10. [PubMed] [Google Scholar]
- 19.Zimmer G, Guillou L, Gauthier T, Iten A, Saraga EP. Digestive leishmaniasis in acquired immunodeficiency syndrome: A light and electron microscopic study of two cases. Mod Pathol. 1996;9:966–9. [PubMed] [Google Scholar]
- 20.Hofman V, Marty P, Perrin C, Saint-Paul MC, Le Fichoux Y, Michiels JF, et al. The histological spectrum of visceral leishmaniasis caused by Leishmania infantum MON-1 in acquired immune deficiency syndrome. Hum Pathol. 2000;31:75–84. doi: 10.1016/s0046-8177(00)80202-6. [DOI] [PubMed] [Google Scholar]
- 21.Alonso MJ, Muñoz E, Picazo A, Abad MM, Gómez F, Roldán M, et al. Duodenal leishmaniasis diagnosed by biopsy in two HIV-positive patients. Pathol Res Pract. 1997;193:43–50. doi: 10.1016/s0344-0338(97)80092-1. [DOI] [PubMed] [Google Scholar]
- 22.Laguna F, García-Samaniego J, Soriano V, Valencia E, Redondo C, Alonso MJ, et al. Gastrointestinal leishmaniasis in human immunodeficiency virus-infected patients: Report of five cases and review. Clin Infect Dis. 1994;19:48–53. doi: 10.1093/clinids/19.1.48. [DOI] [PubMed] [Google Scholar]