Abstract
As the American population ages, older adults are accounting for a larger percentage of the drug abusing population, but little attention has been given to this age group especially in regards to evaluating responsivity to different treatment modalities. Contingency management (CM) is a highly effective behavioral treatment that provides positive tangible reinforcers for objective evidence of behavior change. The purpose of this study was to examine main and interactive effects of age on outcomes in cocaine dependent patients receiving CM with standard care (SC) or SC alone. Patients (N = 393) participating in one of three randomized trials of CM for cocaine dependence were divided into young, middle and older age cohorts. Baseline characteristics and outcomes were compared across the age groups. The oldest age group had more medical problems than the youngest and middle age groups, but fewer legal difficulties and psychiatric symptoms. The oldest age group remained in treatment significantly longer than the other age groups, regardless of the type of treatment received. Although all age groups benefited from CM in terms of retention and longest duration of abstinence achieved, a significant age by treatment interaction effect emerged, with the older cohort improving relatively less from CM than the younger age groups. These findings demonstrate that age may play a role in moderating intervention outcomes, and tailoring CM to the needs of older/middle age substance abusers may be important for improving outcomes in this growing population.
Keywords: cocaine, contingency management, substance abuse treatment, age differences
Introduction
As the American population ages, older adults are accounting for a larger percentage of the drug abusing population (Colliver, Compton, Gfroerer, & Condon, 2006; Substance Abuse and Mental Health Service Administration, 2010). However, little attention has been given to substance abuse among older adults. With advancements in medicine and medical treatments, substance abusers are living longer than before, and investigation of effects of age on substance abuse and its treatment are needed.
Colliver et al. (2006) projects that illicit drug users among the older age cohort will increase from approximately 1.6 million in 1999-2001 to about 3.5 million in 2020. Correspondingly, the number of older adults needing drug abuse treatment is also expected to rise (Gfroerer, Penne, Pemberton, & Folsom, 2003). Among admissions to substance abuse treatment, individuals aged 40 years and older increased from 22.1% in 1992 to 36.3% in 2008 (Substance Abuse and Mental Health Service Administration, 2010). Further, the proportion of treatment admissions 40 years and older who reported primary cocaine abuse more than doubled from 7.4% in 1992 to 15.1% in 2008, whereas the proportion who reported primary alcohol abuse decreased from 73.4% to 54.9% in this same time frame (Substance Abuse & Mental Health Service Administration, 2010).
Patients seeking substance abuse treatment may differ with respect to characteristics and treatment needs based on their ages. For example, in a sample of over 600,000 people above age 40 entering treatment for substance abuse, a higher proportion who reported primary cocaine abuse were African American than white (Substance Abuse and Mental Health Service Administration, 2010). In addition, and as expected, older adults were more likely to be married than younger adults (Satre, Mertens, Areán, & Weisner, 2004).
Age may also impact substance use related problems because older age is associated with loneliness and greater medical problems (Bucholz, Hesselbrock, Shayka, Nurnberger, Shuckit, Schmidt, & Reich, 1995; Schonfeld & Dupree, 1995). In a study of adults in a large managed care chemical dependency program (Satre et al., 2004), older adults had fewer close friends than younger or middle age adults. Older adults also reported more health problems and poorer physical functioning than younger substance abusers (Colliver et al., 2006; Lofwall, Brooner, Bigelow, Kindbom, & Strain, 2005; Rajaratnam, Sivesind, Todman, Roane, & Seewald, 2009).
On the other hand, older compared with younger substance abusing patients tend to have fewer legal difficulties, less psychiatric comorbidity, and fewer social problems. Colliver et al. (2006) found that older substance abuse treatment patients were less likely to have been referred to treatment by the criminal justice system relative to younger patients, and Satre et al. (2004) likewise noted fewer legal problems among older patients. Prigerson, Desai, and Rosenheck (2001) found that the prevalence of a comorbid psychiatric disorder is less common in older substance abusers than in younger substance abusers. Finally, Satre et al. (2004) noted that older adults were less likely than younger adults to have friends or family who encouraged substance use, and five years following treatment, they had fewer family/social difficulties.
In response to substance abuse treatment, older patients do equally well and sometimes better than younger patients (Satre, Mertens, Areán, & Weisner, 2003; Satre et al., 2004). Although younger adults are more likely to enter treatment (Siegel, Falck, Wang, & Carlson, 2002), older and middle aged substance abusers are more likely to remain engaged in treatment (Satre et al., 2003; Maglione, Chao, & Anglin, 2000; McKellar, Kelly, Harris, & Moos, 2006). In one study (Satre et al., 2004), long-term 5-year follow-up evaluations revealed that older adults had higher abstinence rates from drugs and alcohol in the past 30 days as well as over the past year compared to younger adults.
Further, some treatment strategies may be better suited for different age groups. Blow, Walton, Chermack, Mudd, & Brower (2000) suggested that older adults who receive elder-specific alcohol treatment had improved outcomes across a range of measures including abstinence from alcohol and improved general health and pain. Another study (Rice, Longabaugh, Beattie, & Noel, 1993) found higher rates of abstinence when older alcohol abusing adults received cognitive behavioral therapy compared to standard psychotherapy. Among a middle age group, relationship enhancement therapy was most effective.
Contingency management (CM) is an effective treatment modality in a wide range of patients ranging from adolescents to adults. CM is based on basic behavioral principles that providing tangible reinforcers when a desired behavior occurs will increase the frequency of that behavior. CM interventions are efficacious in treating cocaine dependence (DeRubeis and Crits-Cristoph, 1998; Lussier, Heil, Mongeon, Badger, & Higgins, 2006; Prendergast, Podus, Finney, & Greenwell, 2006), and a recent meta-analysis (Dutra, Stathopoulou, Basden, Leyro, Powers, & Otto, 2008) finds that CM has the largest effect size of psychosocial treatments for substance use disorders. However, to our knowledge, only one study has examined the effect of age on treatment outcomes of CM. Peirce, Petry, Roll, Kolodner, Krasnansky, Stabile, et al. (2009) examined the association of demographic characteristics and outcomes in patients randomized to CM treatments or standard care (SC). They found a non-significant trend toward patients over the age of 40 submitting more stimulant-negative urine samples than younger patients for those enrolled in outpatient psychosocial (non-methadone) treatment programs. This study did not examine effects of age on other treatment outcomes such as retention, and it did not evaluate whether persons of different ages respond differently to CM and SC interventions.
The present study aimed to fill gaps in the literature on age and treatment outcomes with a focus on middle age and older substance abusers, defined for the purposes of this study as those 40 years or older. The primary purposes were to examine age-related differences in demographics and baseline characteristics and evaluate the impact of age on treatment outcomes of cocaine abusing patients receiving CM and SC treatments. We expected that older patients may differ with respect to younger patients in terms of some demographic characteristics such as race, as well as differences in severity and patterns of polysubstance use. We also anticipated that psychosocial functioning may differ across age groups with older cocaine abusers endorsing more medical problems, and younger adults experiencing more legal and psychiatric difficulties. We hypothesized that the older cohort may remain in treatment longer than the younger cohorts. Both main and interaction effects of age and treatment condition were analyzed to determine if the older cohort responds differently to CM and SC treatments.
Methods
Participants
Participants were 393 individuals from one of three studies (Petry, Tedford, Austin, Nich, Carroll, & Rounsaville, 2004; Petry, Alessi, Tedford, Austin, & Tardif, 2005a; Petry, Alessi, Carroll, Hanson, MacKinnon, Rounsaville, & Sierra, 2006a). Participants were recruited from four outpatient community-based drug abuse treatment clinics throughout the Northeast. The mean age, years of cocaine use, and level of education did not significantly differ between patients at the clinics (all ps> 0.05), and the content and structure of services were also similar across treatment centers. Participants who were 18 years or older, met current Diagnostic and Statistical Manual of Mental Disorders (DSM-IV; American Psychiatric Association, 1994) criteria for cocaine dependence, and were able to understand study procedures were included in the studies. Exclusion criteria were uncontrolled psychopathology (e.g., active suicidal ideation, mania) or in recovery for pathological gambling (although there is no evidence of increased gambling with prize CM in research to date; Petry & Alessi, 2010; Petry, Kolodner, Li, Peirce, Roll, Stitzer, & Hamilton, 2006b). All patients provided written informed consent, approved by the University of Connecticut Health Center Institutional Review Board.
Procedures
Participants completed a demographics questionnaire and several indices to measure drug abuse severity, psychosocial problems, and psychiatric symptoms. These included the drug use modules of the Structured Clinical Interview for the DSM-IV (First, Spitzer, Gibbon, & Williams, 1996), as well as the Addiction Severity Index (ASI; McLellan, Luborsky, Cacciola, & Griffin, 1985) and Brief Symptom Inventory (BSI; Derogatis, 1993).
The ASI measured psychosocial functioning across a variety of domains including alcohol use, drug use, medical, employment, legal, and family/social. Higher scores in each domain indicate a greater severity of symptoms, with composite scores ranging from 0.00-1.00.
The Brief Symptom Inventory (BSI) assessed severity of past week psychiatric symptoms using a 5-point scale for 9 dimensions: obsessive-compulsive, somatization, depression, anxiety, hostility, interpersonal sensitivity, phobic anxiety, paranoid ideation, and psychotocism. Higher scores indicate a greater severity of symptoms. The Global Severity Index (GSI), a general index of psychiatric symptoms, was utilized as well. It measures overall distress levels.
Treatments
After completing the baseline evaluations, participants were randomly assigned to a treatment condition using a computerized urn randomization procedure (Stout, Wirtz, Carbonari, & Del Boca, 1994). All the primary studies (Petry et al., 2004, 2005a, 2006a) included three treatment conditions, one of which was SC, and the other two were CM interventions. As the treatments are detailed in the original reports, they are only briefly described below.
SC treatment
Individuals in all studies assigned to the SC condition received intensive outpatient substance abuse treatment. Therapy consisted of group sessions covering topics such as coping and life skills, AIDS education, relapse prevention, and 12-step treatment. During the intensive phase, which lasted 2-4 weeks, group sessions were held 3-5 days per week, followed by aftercare which consisted of one group session per week for up to 12 months. Patients also submitted up to 21 breath and urine samples over the 12-week treatment period. The breath sample was screened for alcohol using an Alcosensor IV Altometer (Intoximeters, St Louis, MO, USA), and the urine specimen was screened for cocaine and opioids using Ontrak TesTstiks (Roche, Somersville, NJ, USA).
CM treatment
Patients assigned to a CM condition received the same treatment as the SC described above, and they submitted breath and urine samples according to the same schedule. They also earned reinforcement for providing substance negative urine and breath samples and/or for completing goal-related activities. Abstinence was reinforced for submission of samples testing negative for three substances concurrently: cocaine, opioids, and alcohol. Goal-related activities were consistent with each patient’s treatment plan. For example, if the goal was medical, the activity might be to make or attend a doctor’s appointment. Objective verification in the forms of receipts, brochures, or bulletins was necessary for reinforcement (see Petry, Tedford, & Martin, 2001 for examples). In conditions for which both goal-related activities and abstinence were reinforced, the reinforcement schedules were independent of each other (e.g., failure to complete scheduled activities did not affect reinforcement for abstinence).
All three trials (Petry et al., 2004, 2005a, 2006a) shared the primary goal of evaluating the efficacy of CM plus SC versus SC alone, and all three found benefits of CM. The three trials were comparable in targeted population, recruitment from community clinics, treatment intensity and duration, and assessment measures and intervals. A high level of consistency across studies provided the rationale for combining SC conditions and combining CM conditions for the analyses in the present report. Because four of the six CM conditions in the trials reinforced both abstinence and completion of goal-related activities, sample sizes were too small (and confounded by study) to further divide CM treatments based on reinforcement target.
Data Analysis
Figure 1 shows the age distributions of patients participating in these studies. Patients were classified into one of three groups based on their age at time of treatment initiation: under 30, 30-39, or 40 years of age or more. These cutpoints were selected based on the distribution of patients across ages, along with demarcations according to decades. Only 12 (2.2%) patients were over age 50, so including categories of older aged adults (e.g., 50 and higher, or 60 and higher) would result in very small sample sizes as shown in Figure 1.
Figure 1.
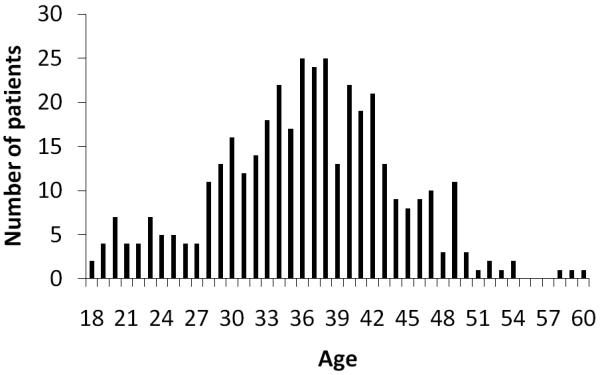
Age distribution of patients.
Demographics and baseline characteristics were compared across the three age groups using χ2 tests and analysis of variance (ANOVA), followed by post-hoc Student Newman Keuls tests when overall analyses were significant. Although not all variables were normally distributed, these tests are robust to departures from normality when the sample size is large (Lumley, Diehr, Emerson, & Chen, 2002). Baseline variables that differed significantly between age groups and were putatively related to dependent variables were included as covariates in subsequent analyses.
Multivariate analysis of covariance (MANCOVA) evaluated the relationship between psychosocial functioning and age category, with gender, race, and alcohol dependence status included as covariates. The dependent variables were BSI-GSI scores and ASI medical, employment, alcohol, drug, legal and family/social scores. BSI-GSI scores were utilized rather than ASI-psychiatric scores as they are a more sensitive indicator of psychiatric symptoms.
Primary during treatment outcomes were: weeks retained in treatment, longest duration of consecutive abstinence (LDA), and proportion of negative samples submitted. An intent-to-treat analysis was used, and these measures were available on 100% of randomized patients. MANCOVA examined the relationship between age category and these three dependent measures, controlling for gender, race, alcohol dependence, and treatment condition (SC or CM); a treatment condition by age category interaction term was also included to assess whether the different age groups responded differently to the interventions. LDA was defined as the greatest number of consecutive weeks of objectively verified abstinence from alcohol, cocaine, and opioids during the treatment period (range 0 – 12 weeks). Positive samples for one or more drugs, missed samples, or unexcused absences on a testing day broke the string of abstinence. Proportions of samples submitted that were negative concurrently for cocaine, alcohol, and opioids were calculated with the number of samples submitted in the denominator, so that missing samples did not impact this variable, and this variable was not confounded by differences in retention. The mean (SD) number of samples submitted was 11.1 (5.9) and did not differ by age group, F (2, 390) = 0.81, p = .45.
Results
Demographic and baseline characteristics
Baseline and demographic characteristics are presented in Table 1 for patients across the three age categories. Gender, ethnicity, and marital status all differed significantly between the age groups with the oldest age group more likely to be female and divorced/separated or have been married at some point than the younger and middle age groups. The middle and oldest age groups were also more likely to be African American than the younger group.
Table 1.
Demographic characteristics and baseline variables based on age category
| Variable | Age 18-29 (n=70) |
Age 30-39 (n=186) |
Age ≥ 40 (n=137) |
Statistical test, p value |
|---|---|---|---|---|
| Recruitment site (no., %) | X2(6) = 5.12, p= 0.53 | |||
| Site A | 5 (7.1) | 16 (8.6) | 10 (7.3) | |
| Site B | 22 (31.4) | 54 (29.0) | 55 (40.1) | |
| Site C | 21 (30.0) | 61 (32.8) | 40 (29.2) | |
| Site D | 22 (31.4) | 55 (29.6) | 32 (23.4) | |
| Treatment group (no.,%) | X2(2) = 0.05, p = 0.98 | |||
| Contingency Management | 20 (28.6) | 54 (29.0) | 41 (29.9) | |
| Standard Care | 50 (71.4) | 132 (70.1) | 96 (70.1) | |
| Studies (no., %) | X2(4) = 6.30, p = 0.18 | |||
| Petry et al. (2004) | 25 (35.7) | 62 (33.3) | 33 (24.1) | |
| Petry et al. (2005a) | 23 (32.9) | 70 (37.6) | 49 (35.8) | |
| Petry et al. (2006a) | 22 (31.4) | 54 (29.0) | 55 (40.1) | |
| Female (no.,%)* | 32 (45.7)a | 80 (43.0)a | 85 (62.0)b | X2(2) = 12.10, p = 0.003 |
| Ethnicity (no.,%)* | X2(6) = 30.80, p = 0.000 | |||
| African American | 17 (24.3)a | 110 (59.1)b | 79 (57.7)b | |
| Caucasian | 40 (57.1)a | 51 (27.4)b | 45 (32.8)b | |
| Hispanic | 10 (14.3) | 22 (11.8) | 12 (8.8) | |
| Other | 3 (4.3) | 3 (1.6) | 1 (0.7) | |
| Marital status (no.,%)* | X2(6) = 39.44, p = 0.000 | |||
| Never married | 52 (74.3)a | 109 (58.6)b | 49 (35.8)c | |
| Married/Living with partner | 13 (18.6) | 32 (17.2) | 30 (21.9) | |
| Separated/Divorced | 5 (7.1)a | 44 (23.7)b | 54 (39.4)c | |
| Widowed | 0 (0.0) | 1 (0.5) | 4 (2.9) | |
| Annual income | $9,580 (11,090) |
$8,790 (16,410) |
$10,820 (14,350) |
F(2,390) = 0.73, p = 0.48 |
| Years of education | 11.5 (1.5) | 11.5 (1.6) | 11.8 (1.7) | F(2,390) = 1.82, p = 0.16 |
| Cocaine, opioid, or alcohol positive sample at intake (no.,%) |
15 (21.4) | 32 (17.3) | 26 (19.0) | X2(2) = 0.59, p = 0.75 |
| Past year DSM alcohol dependence (no.,%)* |
24 (34.3) | 97 (52.2) | 84 (61.3) | X2(2) = 13.56, p = 0.001 |
| Past month days of use | ||||
| Cocaine | 4.7 (7.8) | 3.7 (6.4) | 3.0 (5.8) | F(2,390) = 1.67, p = 0.19 |
| Cannabis* | 3.7 (8.6)a | 1.8 (5.7)b | 1.0 (3.4)b | F(2,390) = 5.49, p = 0.004 |
| Alcohol | 1.1 (3.1) | 2.7 (6.0) | 2.8 (5.9) | F(2,390) = 2.51, p = 0.08 |
| Opioids* | 1.0 (3.6)a | 0.1 (0.8)b | 1.2 (4.7)a | F(2,390) = 4.61, p = 0.01 |
| No. of alcohol treatments* | 1.0 (2.8)a | 3.0 (7.0)a | 6.8 (21.4)b | F(2,390) = 5.08, p = 0.007 |
| No. of drug treatments* | 2.8 (5.5)a | 4.6 (7.5)a | 7.4 (13.6)b | F(2,390) = 6.00, p = 0.003 |
| No. of inpatient psychiatric treatments |
0.6 (1.5) | 0.8 (1.7) | 1.2 (3.3) | F(2,390) = 2.06, p = 0.13 |
| No. of outpatient psychiatric treatments |
1.4 (3.1) | 1.2 (3.1) | 1.1 (2.3) | F(2,390) = 0.23, p = 0.79 |
Values represent means and (standard deviations) unless indicated.
Significant between group difference.
Different subscripts represent groups that differ significantly (p<.05) using Student Newman Keuls tests.
Baseline substance abuse variables were also significantly associated with age. The oldest and middle age groups were more likely to have met past year DSM criteria for alcohol dependence compared to younger adults. In addition, the oldest age group used opiates more frequently in the past month than the middle age group, and they used cannabis less frequently than the youngest age group. The oldest age group also had significantly more drug and alcohol abuse treatment attempts than the younger and middle aged groups.
After controlling for gender (p < .001; with women having increased employment problems), race (p < .001; with African Americans having the lowest BSI-GSI score and alcohol problems and Caucasians the greatest family/social problems but lowest employment problems), and alcohol dependence (p < .001; with alcohol dependent patients having high BSI-GSI and alcohol scores; data not shown), the omnibus analysis evaluating the association between age and psychosocial indices was significant, F (14,760) = 3.49, p < .001. The oldest age group had significantly lower BSI-GSI scores than younger and middle age adults, as depicted in Table 2. Those over 40 years also had greater medical problems, but less severe legal difficulties, than the youngest age group.
Table 2.
Addiction Severity Index composite and Brief Symptom Inventory (BSI) scores based on age category
| Variable | Age 18-29 | Age 30-39 | Age ≥ 40 | Statistical test & p value |
|---|---|---|---|---|
| BSI Global | ||||
| Severity Index * | 1.00 (0.10)a | 1.07 (0.08)a | 0.87 (0.09)b | F(2, 385) = 3.56, p = 0.03 |
| Medical * | 0.14 (0.05)a | 0.22 (0.04)ab | 0.27 (0.04)b | F(2, 385) = 3.31, p = 0.04 |
| Employment | 0.67 (0.04) | 0.76 (0.03) | 0.71 (0.04) | F(2, 385) = 2.44, p = 0.09 |
| Alcohol | 0.19 (0.03) | 0.25 (0.02) | 0.24 (0.03) | F(2, 385) = 2.39, p = 0.09 |
| Drug use | 0.17 (0.01) | 0.14 (0.01) | 0.14 (0.01) | F(2, 385) = 1.86, p = 0.16 |
| Legal * | 0.18 (0.03)a | 0.09 (0.02)b | 0.10 (0.03)b | F(2, 385) = 4.89, p = 0.01 |
| Family/social | 0.23 (0.03) | 0.18 (0.03) | 0.17 (0.03) | F(2, 385) = 1.60, p = 0.20 |
Groups differ, p<.05.
Values represent adjusted means and standard errors.
Different subscripts represent groups that differ significantly (p<.05) using Student Newman Keuls tests.
BSI scales and individual items from the ASI indices on which the age categories differed are shown in Table 3. The oldest age group evidenced less substantial psychiatric symptoms across the majority of BSI scales than younger or middle aged adults. ASI individual medical items such as days of medical problems in the past month, chronic medical problems, and regular medication usage were more often endorsed by the oldest and middle-aged groups compared with the youngest group. On the other hand, the oldest and middle-aged groups were less likely to have engaged in illegal activities in the past month in comparison to the youngest age group.
Table 3.
Brief Symptom Inventory (BSI) scales and Addiction Severity Index (ASI) individual items based on age category
| Variable | Age 18-29 | Age 30-39 | Age ≥ 40 | Statistical test, p value |
|---|---|---|---|---|
| BSI Scales | ||||
| Obsessive-compulsive | 1.23 (0.13) | 1.30 (0.11) | 1.05 (0.12) | F (2,385) = 2.85, p = 0.06 |
| Depression* | 1.08 (0.13)ab | 1.26 (0.11)a | 0.92 (0.13)b | F (2,385) = 3.67, p = 0.03 |
| Paranoid Ideation* | 1.21 (0.12)a | 1.19 (0.10)a | 0.88 (0.11)b | F (2,385) = 5.99, p = 0.003 |
| Psychoticism* | 1.05 (0.12)ab | 1.15 (0.10)a | 0.87 (0.11)b | F (2,385) = 4.51, p = 0.01 |
| Interpersonal-sensitivity* | 0.98 (0.14)ab | 1.19 (0.11)a | 0.92 (0.13)b | F (2,385) = 3.42, p = 0.03 |
| Anxiety | 0.98 (0.12) | 1.13 (0.10) | 1.02 (0.11) | F (2,385) = 1.19, p = 0.31 |
| Phobic anxiety | 0.82 (0.11) | 0.92 (0.09) | 0.72 (0.10) | F (2,385) = 2.68, p = 0.07 |
| Hostility* | 0.84 (0.11)a | 0.81 (0.09)a | 0.52 (0.10)b | F (2,385) = 6.27, p = 0.002 |
| Somaticism | 0.69 (0.10) | 0.72 (0.08) | 0.71 (0.09) | F (2,385) = 0.05, p = 0.95 |
| ASI Medical Items | ||||
| Days of medical problems in past month* |
2.5 (1.5)a | 5.2 (1.2)ab | 7.1 (1.3)b | F (2,385) = 4.40, p = 0.01 |
| Times hospitalized for medical problems |
5.9 (1.5) | 2.6 (1.3) | 3.34 (1.4) | F (2,385) = 2.40, p = 0.09 |
| Any chronic medical problems (no.,%)* |
14 (20.0)a | 56 (30.1)a | 60 (43.8)b | X2(2) = 13.26, p = 0.001 |
| Any medication taken regularly (no.,%) * |
13 (18.6)a | 47 (25.3)a | 50 (36.5)b | X2(2) = 8.68, p = 0.01 |
| ASI Legal Items | ||||
| Days of illegal activities in past month* |
1.1 (0.4)a | 0.1 (0.3)b | 0.2 (0.3)b | F (2,385) = 4.32, p = 0.01 |
| On probation or parole (no., %) |
23 (32.9) | 43 (23.1) | 36 (26.3) | X2(2) = 2.52, p = 0.28 |
| Presently waiting for charges (no.,%) |
21 (30.0) | 32 (17.2) | 28 (20.4) | X2(2) = 5.09, p = 0.08 |
Groups differ, p<.05.
Values represent adjusted means and standard errors unless otherwise noted.
Different subscripts represent groups that differ significantly (p<.05) using Student Newman Keuls tests.
During treatment outcomes
Multivariate analyses, controlling for gender [p = .03, with men submitting higher proportions of negative samples than women], race [p = .03, with African Americans submitting the lowest proportion of negative samples], alcohol dependence status [p = .12], and treatment condition [ps < .002, with CM associated with greater retention and LDA], revealed a significant effect of age category as a main effect on treatment outcomes. As a main effect, age was significantly associated with duration of time in treatment, F (2,382) = 3.09, p = .05, but not with LDA or proportion of negative samples submitted. The average (SD) time in treatment for the youngest age group was 6.2 (0.6) weeks, and for the middle age cohort it was 6.7 (0.5) weeks, and 7.6 (0.5) weeks for the oldest age group.
As shown in Figures 2, 3, and 4, there was a significant age category by treatment condition interaction effect for all three primary treatment outcomes, F (2,383) = 5.41, 5.32, and 5.47, all ps = .005 for retention, LDA, and proportion negative samples, respectively. In general, the older age group benefited less from CM than the younger age groups.
Figure 2.
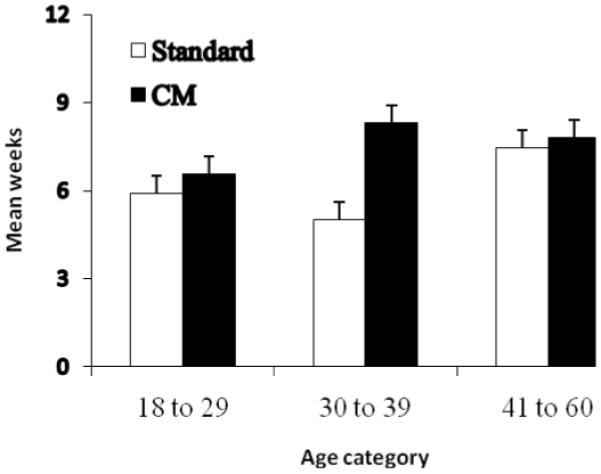
Weeks retained in treatment based on age category and treatment condition. Values represent mean weeks and standard errors of the mean. Significant age, p = .05, and age by treatment condition effects were noted, p = .005.
Figure 3.
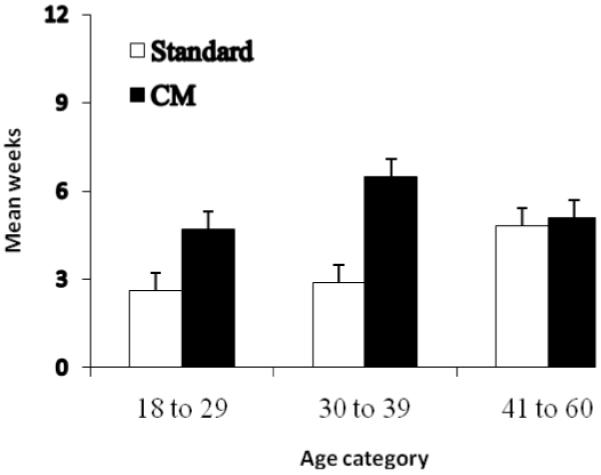
Longest duration of abstinence achieved based on age category and treatment condition. Values represent mean weeks of documented abstinence from cocaine, opioids and alcohol and standard errors of the mean. Significant age by treatment condition effects were noted, p = .005.
Figure 4.
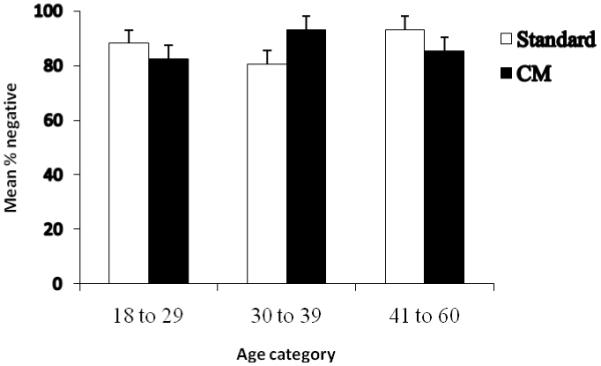
Proportions of negative samples submitted based on age category and treatment condition. Values represent mean proportions of samples submitted that tested negative for cocaine, opioids and alcohol concurrently and standard errors of the mean. Significant age by treatment condition effects were noted, p = .005.
Discussion
Few studies have examined effects of age on treatment outcomes of cocaine dependent adults in general, and none have evaluated the effects of age in terms of responsivity to CM compared with SC interventions. Results from this study show that treatment seeking cocaine abusers in the older/middle aged cohort vary from younger patients, and they respond differently to treatment interventions. The clinical implications of these findings are also discussed.
In the present study, patients seeking treatment for cocaine abuse showed differences in respect to some baseline characteristics based on their ages. Individuals in the oldest age group were more likely to be female and African American than patients in the youngest age group. Our findings complement previous studies showing older adults had less severe legal difficulties than younger adults (Satre et al., 2004). The older group also had significantly lower psychiatric symptoms compared to younger and middle aged groups, a finding similar to Prigerson et al. (2001) and Satre et al. (2003) in samples of veterans and general substance dependent patients, respectively. As in the present study, Rajaratnam et al. (2009) found lower rates of psychiatric symptoms in older compared with younger methadone maintained patients. Thus, despite high rates of lifetime psychiatric diagnoses in older substance abuse patients (Reiger, Farmer, Rae, Locke, Keith, Judd, & Goodwin, 1990; Lofwall et al., 2005; Moos, Mertens, & Brennan, 1993), current psychiatric symptoms appear to be lower than in younger age cohorts.
Moreover, several baseline health and substance abuse variables were significantly associated with age. The oldest age group evidenced higher past month opiate use compared to the middle age group. Our study and another (Satre et al., 2004) found older aged substance abusers had more prominent medical problems and a greater severity of health related issues, perhaps related to prolonged substance abuse (Frishman, Del Vecchio, Sanal, & Ismail, 2003a, Frishman, Del Vecchio, Sanal, & Ismail, 2003b) or exacerbation of existing medical problems (Vupputuri, Batuman, Muntner, Bazzano, Lefante, Whelton, et al., 2004; Warner, Greene, Buchsbaum, Cooper & Robinson, 1998). Consequently, the concerns and clinical needs of substance abuse patients appear to vary by age.
Additionally, our study found that age as a main effect was associated with retention, with the oldest cohort spending a longer time in treatment compared to the younger and middle age groups. Results from this study are somewhat consistent with existing literature suggesting that older patients do as well as, and sometimes better than, younger patients with respect to treatment retention (Satre et al., 2003, 2004; Maglione et al., 2000; McKellar et al., 2006). Although Satre et al. (2003) noted older age was associated with 5-year long-term abstinence, they concluded age was not a significant independent predictor of abstinence, but was likely explained by other patient characteristics, such as greater abstinence goals. In the present study, older adults remained in treatment longer, but age as a main effect did not impact drug use outcomes; when collapsing across treatment conditions, longest duration of abstinence and percent negative samples submitted were comparable across age groups.
As noted in the primary studies (Petry et al., 2004, 2005a, 2006a), CM significantly improved retention and longest duration of abstinence achieved, but older individuals in general benefited less from CM than younger individuals. The significant age by treatment condition effect may be partially explained by the higher rates of positive responses to SC treatment found in this age group, at least in terms of retention, making further improvement in this index difficult to achieve. Significant age by treatment interactions were found for all three outcomes, indicating relatively less benefit of CM in the older cohort. Although older patients did not benefit as much from CM as their younger peers, CM was not ineffective in this cohort. With the exception of percent negative samples which was very high overall and may be impacted by ceiling effects in outpatient samples (Petry et al., 2005b), the two other outcomes (retention and LDA) showed improvement in older adults treated with CM compared with SC.
Several studies have suggested specific treatment strategies such as cognitive behavioral therapy or age-specific groups that focus on issues relevant to this population (e.g., health problems, isolation, and loneliness) may be effective for older adults (Blow et al., 2000; Rice, et al., 1993; Schonfeld & Dupree, 1995). Subsequent studies may assess if CM when added to other treatment approaches optimizes treatment outcomes in the older cohort of patients.
Although the focus of this study was on older and middle aged adults, the percentage of older adults over the age of 50 was small (2.2%). Studies have shown that the baby boomers (born between 1946 and 1964) have higher rates of illicit drug use than other generations (Gfroerer and Epstein, 1999; Gfroerer et al., 2003), and drug admissions are expected to increase from this age group until 2019 (Lofwall, Schuster, & Strain, 2008; Han, Gfroerer, Colliver, & Penne, 2009). A large proportion of adults in our study were in their 40’s, which means they may fall into this cohort, but these results may not generalize to even older populations of cocaine abusers. Future studies should examine CM outcomes using samples of cocaine abusing adults with more individuals above the ages of 50 and 60.
Although the primary during treatment outcome measures used in this study (treatment retention, longest duration of abstinence, and proportion of negative drug samples submitted) are valid indicators of substance abuse treatment outcomes (Grella, Hser, Joshi, & Anglin, 1999; Higgins, Badger, & Budney, 2000; Rounsaville, Petry, & Carroll, 2003), we did not measure any very long-term (e.g. 5 year) post treatment outcomes. Another limitation is that this was a retrospective analysis combining data from three studies, and we did not prospectively examine how different aged patients respond to CM and other interventions.
Strengths of this study include a large patient population, randomized study designs, multiple outcome measures, intent to treat analyses, and use of four community based treatment centers. Additionally, the gender composition in our sample consisting of a high percentage of females in each age group (especially in the oldest age group) improves on studies with largely male dominated samples (e.g., Rice et al., 1993). All these features increase generalization of the results. Furthermore, substance use was monitored frequently using objective indicators, and possible confounding variables were controlled in our analyses, providing a clearer understanding of the relationship between age and treatment outcomes.
In summary, the present findings complement and extend previous research on the relationship between age and substance abuse treatment outcomes. This study additionally provides new insight on the interactive effects of age and treatment conditions involving CM. As the number of older substance abusers continuously increases, more research is needed to ascertain which types of treatment modalities best suit the individual needs of older and middle aged cocaine abusers, and how treatment can be improved for this growing population.
Acknowledgements
Funding for this research and preparation of this report was provided by National Institutes of Health grants P30-DA023918, T35AG026757, R01-DA13444, R01-DA016855, R01-DA14618, R01-DA022739, R01-DA021567, R01-DA018883, R01-DA027615, R01-DA024667, R01-MH60417-Suppl, P50-DA09241, P60-AA03510, and General Clinical Research Center Grant M01-RR06192.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/PHA
References
- American Psychiatric Association . Diagnostic and statistical manual of mental disorders. 4th ed. Author; Washington, DC: 1994. [Google Scholar]
- Blow FC, Walton MA, Chermack ST, Mudd SA, Brower KJ. Older adult treatment outcome following elder-specific inpatient alcoholism treatment. Journal of Substance Abuse Treatment. 2000;19:67–75. doi: 10.1016/s0740-5472(99)00101-4. [DOI] [PubMed] [Google Scholar]
- Bucholz KK, Hesselbrock VM, Shayka JJ, Nurnberger JI, Schuckit MA, Schmidt I, Reich T. Reliability of individual diagnostic criterion items for psychoactive substance dependence and the impact on diagnosis. Journal of Studies on Alcohol. 1995;56:500–505. doi: 10.15288/jsa.1995.56.500. [DOI] [PubMed] [Google Scholar]
- Colliver JD, Compton WM, Gfroerer JC, Condon T. Projecting drug use among aging baby boomers in 2020. Annals of Epidemiology. 2006;16:257–265. doi: 10.1016/j.annepidem.2005.08.003. [DOI] [PubMed] [Google Scholar]
- Derogatis LR. Brief Symptom Inventory (BSI): Administration, scoring and procedure manual. National Computer Systems, Inc.; Minneapolis: 1993. [Google Scholar]
- DeRubeis RJ, Crits-Cristoph P. Empirically supported individual and group psychological treatments for adult mental disorders. Journal of Consulting and Clinical Psychology. 1998;66:37–52. doi: 10.1037//0022-006x.66.1.37. [DOI] [PubMed] [Google Scholar]
- Dutra L, Stathopoulou G, Basden SL, Leyro TM, Powers MB, Otto MW. A Meta-Analytic Review of Psychosocial Interventions for Substance Use Disorders. American Journal of Psychiatry. 2008;165:179–87. doi: 10.1176/appi.ajp.2007.06111851. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders, Clinician Version. American Psychiatric Press, Inc.; Washington, DC: 1996. [Google Scholar]
- Frishman WH, Del Vecchio A, Sanal S, Ismail A. Cardiovascular manifestations of substance abuse part 1: cocaine. Heart Disease. 2003a;5:187–201. doi: 10.1097/01.hdx.0000074519.43281.fa. [DOI] [PubMed] [Google Scholar]
- Frishman WH, Del Vecchio A, Sanal S, Ismail A. Cardiovascular manifestations of substance abuse: part 2: alcohol, amphetamines, heroin, cannabis, and caffeine. Heart Disease. 2003b;5:253–271. doi: 10.1097/01.hdx.0000080713.09303.a6. [DOI] [PubMed] [Google Scholar]
- Gfroerer JC, Epstein JF. Marijuana initiates and their impact on future drug abuse treatment need. Drug and Alcohol Dependence. 1999;54:229–237. doi: 10.1016/s0376-8716(98)00167-7. [DOI] [PubMed] [Google Scholar]
- Gfroerer J, Penne M, Pemberton M, Folsom R. Substance abuse treatment need among older adults in 2020: The impact of the aging baby-boom cohort. Drug and Alcohol Dependence. 2003;69:127–135. doi: 10.1016/s0376-8716(02)00307-1. [DOI] [PubMed] [Google Scholar]
- Grella CE, Hser YI, Joshi V, Anglin MD. Patient histories, retention, and outcome models for younger and older adults in DATOS. Drug and Alcohol Dependence. 1999;57:151–166. doi: 10.1016/s0376-8716(99)00082-4. [DOI] [PubMed] [Google Scholar]
- Han B, Gfroerer JC, Colliver JD, Penne MA. Substance use disorder among older adults in the United States in 2020. Addiction. 2009;104:88–96. doi: 10.1111/j.1360-0443.2008.02411.x. [DOI] [PubMed] [Google Scholar]
- Higgins ST, Badger GJ, Budney AJ. Initial abstinence and success in achieving longer-term cocaine abstinence. Experimental and Clinical Psychopharmacology. 2000;8:377–386. doi: 10.1037//1064-1297.8.3.377. [DOI] [PubMed] [Google Scholar]
- Lofwall MR, Brooner RK, Bigelow GE, Kindbom K, Strain EC. Characteristics of older opioids maintenance patients. Journal of Substance Abuse Treatment. 2005;28:265–272. doi: 10.1016/j.jsat.2005.01.007. [DOI] [PubMed] [Google Scholar]
- Lofwall MR, Schuster A, Strain EC. Changing profile of abused substances by older persons entering treatment. Journal of Nervous and Mental Disease. 2008;196:898–905. doi: 10.1097/NMD.0b013e31818ec7ee. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lumley T, Diehr P, Emerson S, Chen L. The importance of the normality assumption in large public health data sets. Annual Review of Public Health. 2002;23:151–69. doi: 10.1146/annurev.publhealth.23.100901.140546. [DOI] [PubMed] [Google Scholar]
- Lussier JP, Heil SH, Mongeon JA, Badger GJ, Higgins ST. A metaanalysis of voucher-based reinforcement therapy for substance use disorders. Addiction. 2006;101:192–203. doi: 10.1111/j.1360-0443.2006.01311.x. [DOI] [PubMed] [Google Scholar]
- Maglione M, Chao B, Anglin MD. Correlates of outpatient drug treatment dropout among methamphetamine users. Journal of Psychoactive Drugs. 2000;32:221–228. doi: 10.1080/02791072.2000.10400232. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Luborsky L, Cacciola JS, Griffin JE. New data from the Addiction Severity Index: Reliability and validity in three centers. Journal of Nervous and Mental Disease. 1985;163:412–423. doi: 10.1097/00005053-198507000-00005. [DOI] [PubMed] [Google Scholar]
- McKellar J, Kelly J, Harris A, Moos R. Pretreatment and during treatment risk factors for dropout among patients with substance use disorders. Addictive Behaviors. 2006;31:450–460. doi: 10.1016/j.addbeh.2005.05.024. [DOI] [PubMed] [Google Scholar]
- Moos RH, Mertens JR, Brennan PL. Patterns of diagnosis and treatment among late-middle-aged and older substance abuse patients. Journal of Studies on Alcohol. 1993;54:479–487. doi: 10.15288/jsa.1993.54.479. [DOI] [PubMed] [Google Scholar]
- Peirce JM, Petry NM, Roll JM, Kolodner K, Krasnansky J, Stabile PQ, et al. Correlates of stimulant treatment outcome across treatment modalities. American Journal of Drug and Alcohol Abuse. 2009;35:48–53. doi: 10.1080/00952990802455444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Alessi SM. Prize-based contingency management is efficacious in cocaine abusers with and without recent gambling problems. Journal of Substance Abuse Treatment. 2010;39:282–288. doi: 10.1016/j.jsat.2010.06.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Alessi SM, Tedford J, Austin M, Tardif M. Vouchers versus prizes: Contingency management treatment of substance abusers in community settings. Journal of Consulting and Clinical Psychology. 2005a;73:1005–1014. doi: 10.1037/0022-006X.73.6.1005. [DOI] [PubMed] [Google Scholar]
- Petry NM, Alessi SM, Carroll KM, Hanson T, MacKinnon S, Rounsaville B, Sierra S. Contingency management treatments: Reinforcing abstinence versus adherence with goal-related activities. Journal of Consulting and Clinical Psychology. 2006a;74:592–601. doi: 10.1037/0022-006X.74.3.592. [DOI] [PubMed] [Google Scholar]
- Petry NM, Kolodner KB, Li R, Peirce JM, Roll JM, Stitzer ML, Hamilton JA. Prize-based contingency management does not increase gambling: Results of the National Drug Abuse Treatment Clinical Trials Network multi-site study. Drug and Alcohol Dependence. 2006b;83:269–273. doi: 10.1016/j.drugalcdep.2005.11.023. [DOI] [PubMed] [Google Scholar]
- Petry NM, Peirce JM, Stitzer ML, Blaine J, Roll JM, Cohen A, et al. Effect of prize-based incentives on outcomes in stimulant abusers in outpatient psychosocial treatment programs: a national drug abuse treatment clinical trials network study. Archives of General Psychiatry. 2005b;62:1148–1156. doi: 10.1001/archpsyc.62.10.1148. [DOI] [PubMed] [Google Scholar]
- Petry NM, Tedford J, Austin M, Nich C, Carroll KM, Rounsaville BJ. Prize reinforcement contingency management for treatment of cocaine abusers: How low can we go, and with whom? Addiction. 2004;99:349–360. doi: 10.1111/j.1360-0443.2003.00642.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petry NM, Tedford J, Martin B. Reinforcing compliance with non-drug related activities. Journal of Substance Abuse Treatment. 2001;20:33–44. doi: 10.1016/s0740-5472(00)00143-4. [DOI] [PubMed] [Google Scholar]
- Prendergast M, Podus D, Finney J, Greenwell L. Contingency management for treatment of substance use disorders: a meta-analysis. Addiction. 2006;101:1546–1560. doi: 10.1111/j.1360-0443.2006.01581.x. [DOI] [PubMed] [Google Scholar]
- Prigerson HG, Desai RA, Rosenheck RA. Older adult patients with both psychiatric and substance abuse disorders: Prevalence and health service use. Psychiatric Quarterly. 2001;72:1–18. doi: 10.1023/a:1004821118214. [DOI] [PubMed] [Google Scholar]
- Rajaratnam R, Sivesind D, Todman M, Roane D, Seewald R. The aging methadone maintenance patient: Treatment adjustment, long term success, and quality of life. Journal of Opioid Management. 2009;5:27–37. doi: 10.5055/jom.2009.0004. [DOI] [PubMed] [Google Scholar]
- Reiger DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, Goodwin FK. Co-morbidity of mental disorders with alcohol and other drug abuse: results from the Epidemiologic Catchment Area (ECA) study. Journal of the American Medical Association. 1990;264:2511–2518. [PubMed] [Google Scholar]
- Rice C, Longabaugh R, Beattie M, Noel N. Age group differences in response to treatment for problematic alcohol use. Addiction. 1993;88:1369–1375. doi: 10.1111/j.1360-0443.1993.tb02023.x. [DOI] [PubMed] [Google Scholar]
- Rounsaville BJ, Petry NM, Carroll KM. Single versus multiple drug focus in substance abuse clinical trials research. Drug and Alcohol Dependence. 2003;70:117–125. doi: 10.1016/s0376-8716(03)00033-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Satre DD, Mertens J, Areán PA, Weisner C. Contrasting outcomes of older versus middle-aged and younger adult chemical dependency patients in a managed care program. Journal of Studies on Alcohol. 2003;64:520–530. doi: 10.15288/jsa.2003.64.520. [DOI] [PubMed] [Google Scholar]
- Satre DD, Mertens JR, Areán PA, Weisner C. Five-year alcohol and drug treatment outcomes of older adults versus middle-aged and younger adults in a managed care program. Addiction. 2004;99:1286–1297. doi: 10.1111/j.1360-0443.2004.00831.x. [DOI] [PubMed] [Google Scholar]
- Schonfeld L, Dupree LW. Treatment approaches for older problem drinkers. International Journal of the Addictions. 1995;30:1819–1842. doi: 10.3109/10826089509071057. [DOI] [PubMed] [Google Scholar]
- Siegal HA, Falck RS, Wang J, Carlson RG. Predictors of drug abuse treatment entry among crack-cocaine smokers. Drug and Alcohol Dependence. 2002;68:159–166. doi: 10.1016/s0376-8716(02)00192-8. [DOI] [PubMed] [Google Scholar]
- Stout RL, Wirtz PW, Carbonari JP, Del Boca FK. Ensuring balanced distribution of prognostic factors in treatment outcome research. Journal of Studies on Alcohol Supplement. 1994;12:70–77. doi: 10.15288/jsas.1994.s12.70. [DOI] [PubMed] [Google Scholar]
- Substance Abuse and Mental Health Services Administration . 2008 National Household survey on Drug Abuse. National Clearinghouse for Alcohol and Drug Information (NCADI); Rockville, MD: 2010. [Google Scholar]
- Vupputuri S, Batuman V, Muntner P, Bazzano LA, Lefante JJ, Whelton PK, et al. The risk for mild kidney function decline associated with illicit drug use among hypertensive men. American Journal of Kidney Diseases. 2004;43:629–635. doi: 10.1053/j.ajkd.2003.12.027. [DOI] [PubMed] [Google Scholar]
- Warner EA, Greene GS, Buchsbaum MS, Cooper DS, Robinson BE. Diabetic ketoacidosis associated with cocaine use. Archives of Internal Medicine. 1998;158:1799–1802. doi: 10.1001/archinte.158.16.1799. [DOI] [PubMed] [Google Scholar]


