Abstract
Objectives
To investigate change in positive emotion over a 3-month follow-up period and determine whether this change is associated with recovery of functional status in persons with stroke.
Design
A longitudinal study using information from the Stroke Recovery in Underserved Patients (SRUP) database. Positive emotion and functional status were assessed within 72 hours of discharge from an in-patient medical rehabilitation facility and at 3-month follow-up using established measurement instruments.
Participants
The study included 840 adults 55 years old or older with a first-time stroke and admitted to one of eleven in-patient medical rehabilitation facilities in the United States.
Results
The mean age was 72.9 (SD = 9.52) years, 78.6% were non-Hispanic white and 51.7% were women. The average length of stay was 20.2 (SD = 10.1) days and the most prevalent type of stroke was ischemic (75.0%). Positive emotion increased for 35.6% of the sample, decreased for 29.2%, and 35.2% reported no change. Increases in positive emotion change score compared to no change (b = −3.2, SE = 1.5, p = .032) or a decline (b = −8.9, SE = 1.4, p = <.001) was significantly associated with improved functional status at the 3-month follow-up after adjusting for sociodemographic and clinical variables as well as depressive symptoms.
Conclusion
Positive emotion is a dynamic process and can change over time. In persons with stroke, increases in positive emotion over a 3-month period was significantly associated with an increasing likelihood of recovery of functional status compared to no change or a decline in positive emotion. Understanding factors that influence both increases and decreases in positive emotion has implications for stroke rehabilitation programming and quality of life post-hospital discharge.
Keywords: cerebrovascular accident, recovery, functional status, positive emotion
Stroke is a leading cause of functional loss in the United States and represents a major public health challenge (Kung, Hoyert, Xu, & Murphy, 2008). One factor identified with recovery of functional status following stroke is positive emotion (Ostir, Berges, Ottenbacher, Clow, & Ottenbacher, 2008a). Ostir and colleagues (2008a) in a study of 823 older persons with stroke found higher positive emotion at discharge from an inpatient medical rehabilitation facility significantly increased the likelihood of recovery in motor and cognitive function 3 months later, after adjustment for relevant risk factors including depressive symptoms.
A number of theories have been proposed that link high positive emotion with an increased likelihood of recovery following an acute medical event. One hypothesis known as the “broaden and build hypothesis” suggests that high positive emotion may offset the harmful effects of anxiety or depression that often accompanies the initial onset of illness, and which negatively affects functional recovery (Frederickson, Mancuso, Branigan & Tugade, 2000; Frederickson & Levenson, 1998). Another thought is that positive emotion may foster the ability to better cope and adapt to stressful situations including hospitalization and illness (Folkman, 1997; Frederickson, 2003; Spacapan & Thompson, 1991; Zinn et al., 2004). In a 15-year prospective study of women with stage I and II breast cancer, Greer, Morris, Pettingale, and Haybittle (1990) showed those with a fighting spirit demonstrated the best outcomes as compared to women who viewed their situation as hopeless.
Patients with high positive emotion are also more likely to engage in intentional acts (i.e., thoughts, behaviors, volitional acts) that promote recovery after illness (Dunn & Brody, 2008; Lyubomirsky, Sheldon, & Schkade, 2005). A growing literature further demonstrates linkages between high positive emotion and healthy social relationships (Clark & Watson, 1998), increased optimism about future events (Taylor & Brown, 1994), and greater feelings of control over external events (Ryff & Singer, 1996).
In the present study, we sought to examine change in positive emotion over a 3-month follow-up period in persons with a first-time stroke. Little information is available on the degree or magnitude of positive emotion change that is likely in those recovering from stroke (Ostir, Berges, Ottenbacher, Graham, & Ottenbacher, 2008b). We were further interested in testing whether change in positive emotion would be associated with recovery of functional status. Functional status is clearly an important health outcome linked to independence, life satisfaction, and quality of life (Ahlsio, Britton, Murray, & Theorell, 1984; Beckley, 2006; Indredavik, Bakke, Slordahl, Rokseth, & Haheim, 1998). If change in positive emotion is associated with recovery of functional status poststroke, this may lead to interventions aimed at increasing positive emotion. We hypothesized that increasing positive emotion over a 3-month follow-up would be associated with an increased likelihood of recovery of functional status as compared to no change or decline.
Method
Source of Data
Data were collected as part of a prospective cohort study of persons with stroke (ICD-9 codes 436–439) who received inpatient medical rehabilitation services in 2005–2006. A total of 20 facilities were invited to participate in the study and were provided information describing the goals of the study. Of those invited, 16 agreed to participate. Five facilities in the Gulf coast region and affected by hurricanes (2005) were subsequently removed from the study. The 11 remaining facilities were located across diverse regions of the country, including California, Florida, Iowa, Illinois, Kentucky, New Jersey, New York (2), Texas (2), and Washington DC. Operating bed sizes ranged from 12 to 155 (median bed size = 78); all eleven facilities were accredited by the Joint Commission for Accreditation of Healthcare Organizations (JCAHO); and all but one facility was accredited by the Commission for the Accreditation of Rehabilitation Facilities (CARF).
Prior studies have relied in whole or in part on this data set. The reader is referred to Ostir et al. (2008a) and Ostir et al. (2008b).
Data Collection
Clinical nurse researchers who underwent intensive training and interrater reliability assessments, and blinded to the research questions and hypotheses of the present study conducted interviews. Participants underwent a structured interview within 24 hours of admission to an inpatient medical rehabilitation facility, within 72 hours of discharge, and at a 3-month follow-up. Admission and discharge interviews were conducted in hospital, and follow-up information was collected via telephone interview. Interviews included sociodemograhic, clinical, and emotional items. The interrater reliability and stability of the follow-up information collected using phone interviews has been established, with ICC values for functional assessments ranging from 0.86 to 0.99 (Heinemann, Linacre, Wright, Hamilton, & Granger, 1993; Smith et al., 1996). In-hospital and follow-up interviews were conducted in Spanish or English.
Study Population
Persons with a diagnosis of a first-time stroke and 55 years old or older of either gender were screened for cognitive appropriateness by nursing staff at the inpatient medical rehabilitation facility with regard to their ability to respond to basic orientation questions about person, place, and time. A total of 1006 non-proxy and cognitively appropriate participants were consented.
Of the original 1006 participants interviewed, 166 were excluded from the study. Twenty-nine died, 40 refused follow-up interview, and 78 could not be contacted. An additional 19 were excluded from the analysis because of missing data. The current study included 840 adults (660 non-Hispanic whites, 133 non-Hispanic blacks, and 47 Hispanics) with stroke who had complete information on key variables of interest at discharge from inpatient medical rehabilitation and 3-month follow-up. To evaluate the potential bias of those lost to follow-up, we tested for significant differences across various sociodemographic and clinical measures. No significant differences were found between those included and excluded. Central and local ethical committee approval was sought and obtained. Consent was obtained in-person at the time of the initial interview.
Measures
Positive emotion
Positive emotion was assessed by 4-items from the Center for Epidemiologic Studies Depression Scale (CES-D; Radloff, 1977). This measure of positive emotion has been used in previous studies of persons with stroke (Ostir, Markides, Black, & Goodwin, 2000; Ostir, Markides, Peek, & Goodwin, 2001; Ostir et al., 2008a; Ostir, et al., 2008b). The factor structure of the CES-D has been examined in older populations (Miller, Markides, & Black, 1997). The four positive items included “I felt that I was just as good as other people,” “I felt hopeful about the future,” “I was happy,” and “I enjoyed life.” Responses to the positive items were scored on a 4-point scale (0 to 3). A score of 0 corresponded to a response of “rarely or none of the time,” a 1 to “some or a little,” a 2 to “occasionally or a moderate amount of the time,” and 3 to “most or all of the time.” Summed responses from the four items created a positive emotion summary score (0–12) with higher scores indicating higher positive emotion. A positive emotion change score was calculated as the difference between 3-month follow-up and discharge from inpatient medical rehabilitation, where increasing change scores indicated higher positive emotion. The positive emotion change score was used as a dichotomous (<12 vs. 12) and continuous variable.
Functional status
Functional status was assessed by the In-patient Rehabilitation Facilities-Patient Assessment Instrument (IRF-PAI). The IRF-PAI is a 54-item instrument used to assign medical rehabilitation inpatients to a case-mix group. The case-mix group determines prospective reimbursement for medical rehabilitation by the Centers for Medicare and Medicaid Services (Carter et al., 1997; Stineman et al., 1994a; Stineman et al., 1994b). The functional status items in the IRF-PAI are from the Functional Independence Measure (FIM Instrument), a standardized measure including 18 items covering six domains: self-care, sphincter control, transfer, locomotion, communication, and social cognition. All 18 items are scored into one of seven levels of function, ranging from complete dependence (level 1) to complete independence (level 7). Total FIM ratings have a potential range of 18 to 126, with higher scores indicating greater functional independence. The reliability, validity, and responsiveness of the FIM instrument have been widely investigated (Hamilton, Laughlin, Fielder, & Granger, 1994; Ottenbacher, Hsu, Granger, & Fielder, 1996; Stineman et al., 1996). The reliability (intraclass correlation coefficient) of the Total FIM and of its domains has consistently been found to be > 0.85 (Granger, Cotter, Hamilton, & Fiedler, 1993; Hamilton et al., 1994; Ottenbacher et al., 1996).
Covariates
Sociodemographic and clinical measures known to affect functional status were included as covariates in the statistical models described below. Previous research has demonstrated recovery of functional status following stroke is associated with a number of factors, including age (Kugler, Altenhoner, Piergiorgio & Andreas, 2003), gender (Reeves et al., 2008), stroke type (Katrak, Black, & Peera, 2009), race/ethnicity (Bhandari, Kushel, Price, & Schillinger, 2005), social support (Glass, Matchar, Belyea, & Feussner, 1993), and education (Hanjo, Iso, Ikeda, Inoue, & Tsugane, 2009). Number of comorbidities (Turhan, Ataly, & Muderrisoglu, 2009) and emotional problems, such as depression (Hermann, Black, Lawrence, Szekely, & Szala, 1998), have also been associated with recovery of functional status following stroke.
Sociodemographic measures included age (55–97), gender (female vs. male), marital status (married vs. unmarried), race/ethnicity (white vs. other), and high school education (≥12 years vs. <12). Clinical measures included a comorbidities index (hypertension, heart attack, diabetes, kidney disease and cancer), length of hospital stay (calculated in days from inpatient admission to discharge), stroke type (ischemic vs. hemorrhagic), therapy after discharge (any therapy vs. none), discharge Total FIM score, positive emotion summary score at discharge, and depressive symptoms at discharge. Depressive symptoms were measured using the 16 negative affect items from the CES-D (range 0–48).
Statistical Analysis
Participant characteristics were described by descriptive statistics and reported as means (and standard deviations) for continuous measures and as percentages for categorical measures. The association between positive emotion change score (increase in positive emotion vs. no change; increase in positive emotion vs. decline) and functional status at 3-month follow-up was examined in a multivariate generalized linear regression model. The first step in the model included sociodemographic characteristics (age, gender, race, marital status, and years of school). The second step added clinical variables including length of stay, stroke type, sum of comorbidities index, therapy following discharge, Total FIM score at discharge, depressive symptoms at discharge, and positive emotion summary score at discharge. At the final step (full model), change in positive emotion (increase in positive emotion vs. no change; increase in positive emotion vs. a decline) was added. For all models, testing was two-sided. A p-value < 0.05 was considered to indicate statistical significance. All analyses were performed using SPSS software, version 11.0 (SPSS, Inc., Chicago, IL).
Results
Table 1 shows characteristics for the total sample at discharge from inpatient medical rehabilitation. The mean age was 72.9 (SD = 9.52) years, 51.7% of the sample was women and 52.9% were married. The majority was non-Hispanic white (78.6%) and the most prevalent type of stroke was ischemic (75.0%). A majority of the sample (79.3%) had 12 or more years of education. The mean length of stay was 20.21 (SD = 10.1) days, most of the sample had two or more medical comorbidities (88.2%), and received ongoing therapy following discharge (90.0%).
Table 1.
Sociodemographic and Clinical Characteristics for the Total Sample (n = 840)
| Participant characteristics | % |
|---|---|
| Age (years) | |
| 55–64 | 23.0 |
| 65–74 | 29.6 |
| 75–84 | 35.7 |
| 85+ | 11.7 |
| Gender | |
| Men | 48.3 |
| Women | 51.7 |
| Ethnicity | |
| Non-Hispanic white | 78.6 |
| Non-Hispanic black | 15.8 |
| Hispanic | 5.6 |
| Marital status | |
| Unmarried | 47.1 |
| Married | 52.9 |
| Education (years) | |
| <12 | 20.7 |
| >12 | 79.3 |
| Comorbidities | |
| 0 | 2.4 |
| 1 | 9.4 |
| >2 | 88.2 |
| Stroke type (Ischemic) | 75.0 |
| Post care (any) | 90.0 |
| Length of stay (M, SD) | 20.21 (10.1) |
| FIM Total at discharge (M, SD) | 81.03 (23.25) |
Note. FIM = Functional Independence Measure.
The highest positive emotion score of 12 was reported by 27.9% of the sample (n = 234) at both discharge and follow-up. Group comparisons showed no significant differences between this group and others on sociodemographic characteristics (i.e., age, gender, marital status, age, or years of school). No significant differences were noted on clinical measures including stroke type, follow-up therapy, and medical comorbidities. Differences were found in length of stay (p = < .001), total FIM score (p < .001), and depressive symptoms (p < .001) at discharge. Those who scored 12 on the positive emotion measure at discharge and follow-up had shorter lengths of stay, higher total FIM scores, and reported fewer depressive symptoms at discharge.
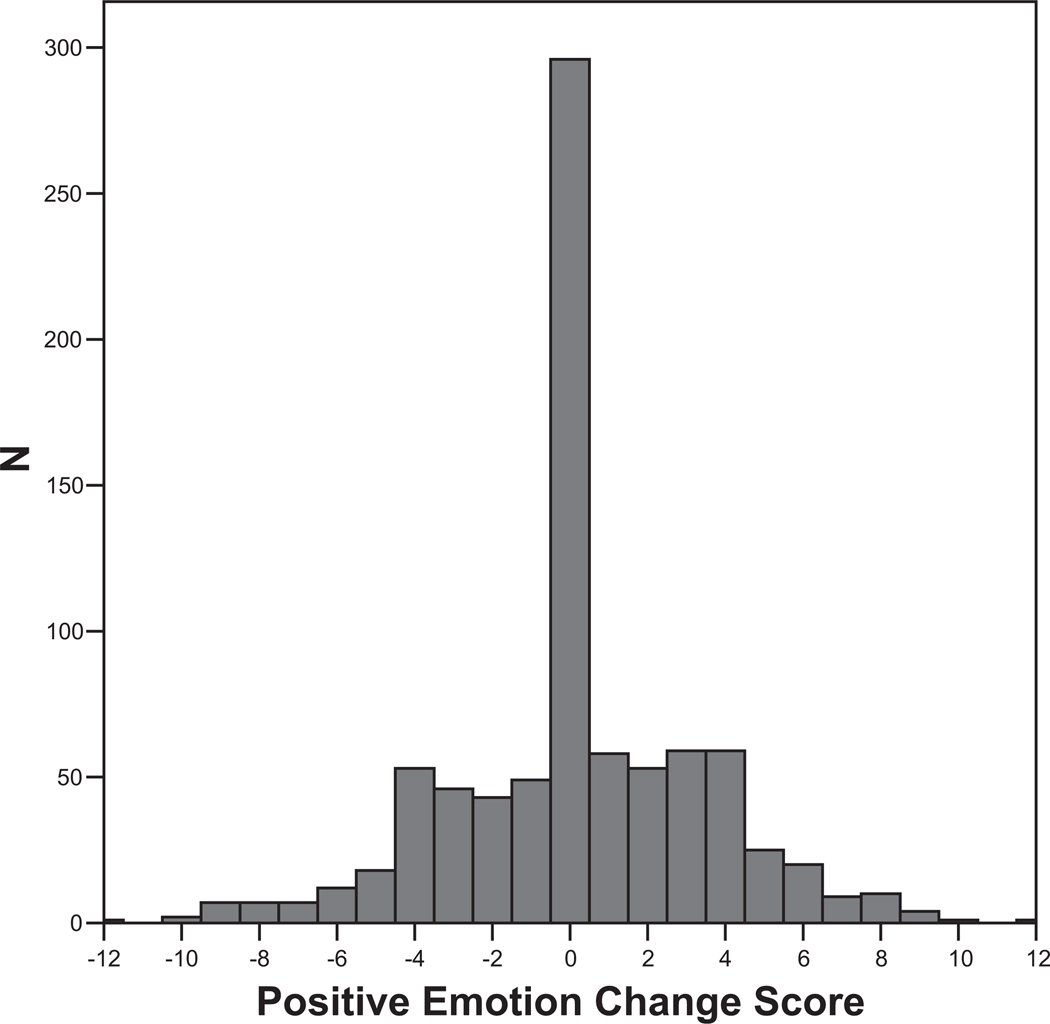
Figure 1 shows the distribution of positive emotion change scores. A total of 35.6% (n = 299) reported an increase in positive emotion between discharge and 3-month follow-up, 29.2% (n = 245) declined, and 35.2% (n = 296) showed no change. Those who reported an increase in positive emotion gained an average of 3.4 points, while those who reported a decline decreased an average of 3.5 points.
Figure 1.
Change in Positive Emotion Between Discharge and 3-Month Follow-up.
Table 2 shows the multivariate generalized linear regression model examining associations between positive emotion change score and Total FIM ratings at 3-month follow-up. For variables in each model, standardized (β) and unstandardized (B) parameter estimates were presented, and a p-value of < 0.05 was considered significant. In the first step of the model, Total FIM at 3-month follow-up was significantly predicted by age (b = −.361, SE = .083, p = <.001), race/ethnicity (b = 4.85, SE = 1.94, p = .013), and marital status (b = −5.41, SE = 1.64, p = .001). With the addition of clinical variables (i.e., length of stay, stroke type, comorbidities index, therapy following discharge from acute medical rehabilitation, Total FIM at discharge, depressive symptoms at discharge, and positive emotion at discharge), age (p = .005) and race/ethnicity (p = < .001) remained significantly associated with Total FIM score at follow-up (Step 2). Additionally, stroke type (b = −1.73, SE = .74, p = .02), comorbidities (b = −1.25, SE = .41, p = .002), follow-up therapy (b = −4.34, SE = 1.7, p = .012), Total FIM score at discharge (b = .651, SE = .024, p = <0.001), depressive symptoms at discharge (b = −.282, SE = .07, p = < .001), and positive emotion summary score at discharge (b = .434, SE = .20, p = .03) were significant predictors of Total FIM at 3-month follow-up. This block accounted for 55% of the variance in the criterion variable. When change in positive emotion (increase in positive emotion change score vs. no change, and increase in positive emotion vs. a decline) was added at the final step (full model), increase in positive emotion change score as compared to no change (b = −3.16, SE = 1.5, p = .032) and a decline in positive emotion (b = −8.93, SE = 1.44, p = < .001) were significant predictors of Total FIM at 3-month follow-up. This block accounted for an additional 2% of the variance in the criterion variable. Age (p = .003), race/ethnicity (p = < .001), follow-up therapy (p = .006), stroke type (p = .012), comorbidities (p = .001), Total FIM at discharge from acute medical rehabilitation (p = < .001), depressive symptoms (p = .002), and positive emotion summary score at discharge (p = < .001) remained significant predictors of Total FIM at 3-month follow-up.
Table 2.
Sociodemographic and Clinical Characteristics at Discharge Associated With Change in Total Functional Independence Measure (FIM) at 3-Month Follow-Up for Participants With Stroke (N = 840)
| Variable | dfs | R2 | ΔR2 | ΔF | B | β |
|---|---|---|---|---|---|---|
| Step 1-Demographics | 5, 834 | .040 | 6.95 | |||
| Age | −.361 | −.151† | ||||
| Female | −1.97 | −.043 | ||||
| Race (White) | 4.85 | .087* | ||||
| Married | −5.41 | −.12** | ||||
| Education (> vs. <12) | 3.05 | .054 | ||||
| Step 2-Clinical variables | 7, 827 | .595 | .555 | 161.86 | ||
| Length of stay | −.082 | −.036 | ||||
| Therapy after DC | −4.34 | −.057* | ||||
| Stroke type | −1.73 | −.052* | ||||
| Comorbidities sum | −1.25 | −.068** | ||||
| Total FIM at DC | .651 | .665† | ||||
| Depressive symptoms DC (8.94, SD = 9.4) | −.282 | −.111† | ||||
| Positive emotion DC (8.97, SD = 3.1) | .434 | .059* | ||||
| Step 3-change in PE | 2, 825 | .615 | .020 | 21.50 | ||
| Positive change vs. no change | −3.16 | −.066* | ||||
| Positive change vs. negative change | −8.93 | −.179† |
Note. DC = discharge; FIM = functional independence measure; PE = positive emotion.
p < .001.
p < .05.
p < .01.
Discussion
The current study examined change in positive emotion over a 3-month follow-up period and tested whether change in positive emotion score was associated with recovery of functional status. We found that 35.6% of participants reported an increase in positive emotion, 29.2% declined, and 35.2% showed no change. These findings add support to the notion that positive emotion is a dynamic process that can vary with time (Ostir et al, 2008). We further showed that gains in positive emotion over the 3-month follow-up were associated with recovery of functional status. Increases in positive emotion scores over the follow-up period, compared to no change or a decline in positive emotion, was significantly associated with higher Total FIM ratings after adjusting for sociodemographic and clinical variables known to affect functional status. It is important to note that the association between increases in positive emotion and functional status was maintained after adjusting for depressive symptoms. Previous studies have demonstrated the independence of positive emotion and depression (Deiner & Lucas, 2000; Folkman & Moskowitz, 2000). Our findings lend further support to the hypothesis that positive emotions and depressive symptoms are independent, and that the presence of one is not simply the absence of the other.
The relationship between change in positive emotion and recovery of functional status may represent a positive feedback loop whereby increases in positive emotion provide motivation to the person with stroke to engage in activities that result in improved functional status. For example, in a rehabilitation setting, a person with high positive emotion may cooperate with the treatment team, engage in exercises to improve function, and employ compensatory strategies. All of which is likely to result in improved functional status. The noted improvements in functional status might, in turn, result in further increases in positive emotion. Lyubomirsky and colleagues (2005) hypothesize a “hierarchy of sustainable happiness” whereby those who possess positive emotion make conscious choices to engage in thoughts and behaviors that bring about functional change. Dunn and Brody (2008) have termed the actions one takes to bring about functional change, “life regulation qualities.” These can include developing and striving to attain personal goals, engaging in regular physical exercise, and participating in meaningful relationships (i.e., giving to others, mentoring another). If properly structured, both the rehabilitation setting and community life following rehabilitation can provide opportunities for such activities. Increases in positive emotion might also impact the cognitive appraisal of the person’s current situation and outlook on the future. Zinn and colleagues (2004) have demonstrated that cognitive status can impact the process of rehabilitation and functional outcome. A person with positive emotion might view the onset of stroke as a challenge to be overcome verses a catastrophic and limiting event. Riener (2007) and Stefanucci, Proffitt, Clore, and Parekh (2008) demonstrated that persons with high positive emotion viewed difficult situations as less challenging compared to those who were anxious or in a depressed mood. A person with a positive outlook might be able to recognize small gains in function as evidence of improvement, producing hope for continued functional change and providing motivation to continue with a challenging therapy regimen or home exercise program. Dunn, Uswatte, and Elliott (2009) report that hope and a future-oriented focus may increase positive emotion and motivate a person to act in ways that enhance the chances of a favorable outcome after onset of disability. Recognizing progress during rehabilitation and continuing to gauge progress after discharge may enhance positive emotion and undo the effects of stress and negative emotion that frequently occur following initial onset of stroke (Frederickson et al., 2000).
A number of studies have demonstrated an association between functional status and other important health-related outcomes such as quality of life and participation in the community. Ahlsio et al (1984) and Indredavik and colleagues (1998) found that following a stroke, those who were independent in performing activities of daily living (ADL) reported significantly higher levels of quality of life as compared to those who were restricted or dependent. Beckley (2006) demonstrated that for people who had sustained a stroke, community participation was related to the person’s ability to perform ADL tasks without support.
Our study has a number of strengths including broad representation, use of ICD-9 codes, and reliable measurement instruments. However, the study is not without limitations. Although data were collected across diverse geographic regions in the United States, study participants were not randomly selected and may not be representative of all persons with stroke. As is the case with all longitudinal studies, biases may have been introduced by missing data or unbalanced representation of the population. We examined change using only two reference points over a relatively brief time period (i.e., 3 months). Multiple assessment points may affect the stability and reliability of measures. Future studies should include additional measurement occasions over a longer period of time to allow for an exploration of fluctuations in emotion and function, and help determine if a dynamic change process continues at greater distances from the onset of stroke. Also, to test our hypotheses concerning the association between change in positive emotion and recovery of functional status, we relied on a regression model to provide information about the degree of variance attributable to change in positive emotion above and beyond that attributable to important demographic and clinical variables. While this statistical procedure is appropriate for theory-testing, our results imply that change in positive emotion may not account for an impressive amount of variance in recovery of functional status (2%) after taking into account the variance attributable to clinical variables selected for this study (55%). Future research could utilize other designs and analyses (e.g., latent growth models, structural equation modeling) that may provide additional information about the relative importance of positive emotion in the prediction of functional outcome following stroke in the context of important clinical variables. Finally, because inter-hospital variability exists with regard to the type and quality of care delivered by acute medical rehabilitation facilities, hospitals participating in this study may not adequately reflect the rehabilitation experience at other facilities. However, it should be noted that facilities included in the study were Joint Commission for Accreditation of Healthcare Organizations (JCAHO) and Commission for the Accreditation of Rehabilitation Facilities (CARF) accredited. Both agencies set guidelines and standards for care in medical rehabilitation facilities.
In summary, this study extends previous work indicating that positive emotion can change over time, and lends support to hypotheses regarding the dynamic state of emotions and the independence of positive and negative emotions. Because knowledge of factors associated with functional recovery is essential in working with persons who have experienced stroke, this line of research remains important. Given that positive emotion has been shown to be both protective of stroke (Ostir et al., 2001; Penninx et al., 2000) and supportive of functional recovery after stroke (Ostir et al., 2008a), further exploration into the role of positive emotions and recovery of functional status after stroke is warranted. This line of research may give rise to interventions that increase positive emotion and support subsequent functional recovery after stroke onset. Continued exploration of associations between positive emotion and important sociodemographic and clinical variables may identify those who are resilient and those who are most vulnerable following a stroke.
Acknowledgments
This research was supported by funding from the National Institutes of Health and the National Institute of Aging for G. Ostir (R01-AG024806 & K01-HD046682), and National Institutes of Child Health and Human Development for I. Berges (R03-HDO05821-01). The authors have no other funding or personal relationships to declare. The funding sources had no role in the design, methods, subject recruitment, data collections, analysis or preparation of the manuscript.
Contributor Information
Gary S. Seale, Division of Rehabilitation Sciences, University of Texas Medical Branch, and Transitional Learning Center at Galveston, Galveston, Texas
Ivonne-Marie Berges, Division of Rehabilitation Sciences, University of Texas Medical Branch, and Sealy Center on Aging, Division of Geriatrics, Department of Medicine, University of Texas Medical Branch.
Kenneth J. Ottenbacher, Division of Rehabilitation Sciences, University of Texas Medical Branch, and Sealy Center on Aging, Division of Geriatrics, Department of Medicine, University of Texas Medical Branch
Glenn V. Ostir, Division of Rehabilitation Sciences, University of Texas Medical Branch, and Sealy Center on Aging, Division of Geriatrics, Department of Medicine, University of Texas Medical Branch
References
- Ahlsio B, Britton M, Murray V, Theorell T. Disablement and quality of life after stroke. Stroke. 1984;15:886–890. doi: 10.1161/01.str.15.5.886. [DOI] [PubMed] [Google Scholar]
- Beckley MN. Community participation following cerebrovascular accident: Impact of the buffering model of social support. American Journal of Occupational Therapy. 2006;60:129–135. doi: 10.5014/ajot.60.2.129. [DOI] [PubMed] [Google Scholar]
- Bhandari VK, Kushel M, Price L, Schillinger D. Racial disparities in outcomes of inpatient stroke rehabilitation. Archives of Physical Medicine and Rehabilitation. 2005;86:2081–2086. doi: 10.1016/j.apmr.2005.05.008. [DOI] [PubMed] [Google Scholar]
- Carter GM, Relles DA, Buchanan JL, Bean T, Donyo T, Rosenfeld L, Rubenstein K, et al. A classification system for inpatient rehabilitation patients: A review and proposed revisions to the Functional Independence Measure-Function Related Groups. Project memo (Final 31 Aug 95–3 Jul 97). NTIS Order Number PB98-105992. Santa Monica, CA: RAND Corp.; 1997. [Google Scholar]
- Clark LA, Watson D. Mood and mundane: Relations between daily life events and self-reported mood. Journal of Personality and Social Psychology. 1998;54:296–308. doi: 10.1037//0022-3514.54.2.296. [DOI] [PubMed] [Google Scholar]
- Deiner E, Lucas RE. Subjective emotional well-being. In: Lewis M, Haviland-Jones JM, editors. Handbook of emotions. New York: Guilford; 2000. pp. 325–337. [Google Scholar]
- Dunn DS, Brody C. Defining the good life following acquired physical disability. Rehabilitation Psychology. 2008;55:413–425. [Google Scholar]
- Dunn DS, Uswatte G, Elliott TE. Happiness, resilience, and positive growth following physical disability: Issues for understanding, research and therapeutic intervention. In: Lopez SJ, editor. Oxford Handbook of Positive Psychology. 2nd Ed. New York: Oxford University Press; 2009. pp. 651–664. [Google Scholar]
- Folkman S. Positive psychological states and coping with severe stress. Social Science & Medicine. 1997;45:1201–1221. doi: 10.1016/s0277-9536(97)00040-3. [DOI] [PubMed] [Google Scholar]
- Folkman S, Moskowitz JT. Positive affect and the other side of coping. American Psychologist. 2000;55:647–654. doi: 10.1037//0003-066x.55.6.647. [DOI] [PubMed] [Google Scholar]
- Frederickson BL. The value of positive emotions–the emerging science of positive psychology in coming to understand why it’s good to feel good. American Scientist. 2003;91:330–335. [Google Scholar]
- Frederickson BL, Levenson RW. Positive emotions speed recovery from the cardiovascular sequelae of negative emotions. Cognition and Emotion. 1998;12:191–220. doi: 10.1080/026999398379718. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frederickson BL, Mancuso RA, Branigan C, Tugade MM. The undoing effect of positive emotions. Motivation and Emotion. 2000;24:237–258. doi: 10.1023/a:1010796329158. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glass TA, Matchar DB, Belyea M, Feussner JR. Impact of social support on outcome in first stroke. Stroke. 1993;24:64–70. doi: 10.1161/01.str.24.1.64. [DOI] [PubMed] [Google Scholar]
- Granger CV, Cotter AC, Hamilton BB, Fiedler RC. Functional assessment scales: A study of persons with stroke. Archives of Physical Medicine and Rehabilitation. 1993;74:133–138. [PubMed] [Google Scholar]
- Greer S, Morris T, Pettingale KW, Haybittle JL. Psychological response to breast cancer and 15-year outcome. Lancet. 1990;335:49–50. doi: 10.1016/0140-6736(90)90173-3. [DOI] [PubMed] [Google Scholar]
- Hamilton BB, Laughlin JA, Fiedler RC, Granger CV. Interrater reliability of the 7-level Functional Independence Measure (FIM) Scandinavian Journal of Rehabilitation Medicine. 1994;26:115–119. [PubMed] [Google Scholar]
- Hanjo K, Iso H, Ikeda A, Inoue M, Tsugane S. Education level and physical function limitations among Japanese community residents– gender differences in progress from stroke. BMC Public Health. 2009;9:131–139. doi: 10.1186/1471-2458-9-131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heinemann AW, Linacre JM, Wright BD, Hamilton BB, Granger C. Relationships between impairment and physical disability as measured by the functional independence measure. Archives of Physical Medicine & Rehabilitation. 1993;74:566–573. doi: 10.1016/0003-9993(93)90153-2. [DOI] [PubMed] [Google Scholar]
- Hermann N, Black SE, Lawrence J, Szekely C, Szalai JP. The Sunnybrook Stroke Study: A prospective study of depressive symptoms and functional outcomes. Stroke. 1998;29:618–624. doi: 10.1161/01.str.29.3.618. [DOI] [PubMed] [Google Scholar]
- Indredavik B, Bakke F, Slordahl SA, Rokseth R, Haheim LL. Stroke unit treatment improves long-term quality of life: A randomized controlled trail. Stroke. 1998;29:895–899. doi: 10.1161/01.str.29.5.895. [DOI] [PubMed] [Google Scholar]
- Katrak PH, Black D, Peera V. Do stroke patients with intracerebral hemorrhage have better functional outcomes than patients with cerebral infarction? Physical Medicine and Rehabilitation. 2009;1:427–433. doi: 10.1016/j.pmrj.2009.03.002. [DOI] [PubMed] [Google Scholar]
- Kugler C, Altenhoner T, Piergiorgio L, Andreas F. Does age influence recovery from ischemic stroke? Journal of Neurology. 2003;250:676–681. doi: 10.1007/s00415-003-1054-8. [DOI] [PubMed] [Google Scholar]
- Kung HC, Hoyert DL, Xu JQ, Murphy SL. National Vital Statistics Reports. Vol. 56. Hyattsville, MD: National Center for Health Statistics; 2008. Deaths: Final data for 2005. [PubMed] [Google Scholar]
- Lyubomirsky S, Sheldon KM, Schkade D. Pursuing happiness: The architecture of sustainable change. Review of General Psychology. 2005;9:111–131. [Google Scholar]
- Miller TQ, Markides KS, Black SA. The factor structure of the CES-D in two surveys of elderly Mexican Americans. Journals of Gerontology: Series B: Psychological Sciences and Social Sciences. 1997;52B:S259–S269. doi: 10.1093/geronb/52b.5.s259. [DOI] [PubMed] [Google Scholar]
- Ostir GV, Berges I, Ottenbacher ME, Clow A, Ottenbacher KJ. Associations between positive emotion and recovery of functional status following stroke. Psychosomatic Medicine. 2008a;70:404–409. doi: 10.1097/PSY.0b013e31816fd7d0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostir GV, Berges I, Ottenbacher ME, Graham JE, Ottenbacher KJ. Positive emotion following a stroke. Journal of Rehabilitation Medicine. 2008b;40:477–481. doi: 10.2340/16501977-0193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ostir GV, Markides KS, Black SA, Goodwin JS. Emotional well-being predicts subsequent functional independence and survival. Journal of the American Geriatrics Society. 2000;48:590–592. doi: 10.1111/j.1532-5415.2000.tb04991.x. [DOI] [PubMed] [Google Scholar]
- Ostir GV, Markides KS, Peek KM, Goodwin JS. The association between emotional well-being and the incidence of stroke in older adults. Psychosomatic Medicine. 2001;63:210–215. doi: 10.1097/00006842-200103000-00003. [DOI] [PubMed] [Google Scholar]
- Ottenbacher KJ, Hsu Y, Granger CV, Fiedler RC. The reliability of the functional independence measure: A quantitative review. Archives of Physical Medicine & Rehabilitation. 1996;77:1226–1232. doi: 10.1016/s0003-9993(96)90184-7. [DOI] [PubMed] [Google Scholar]
- Penninx BW, Guralnik JM, Bandeen-Roche K, Kasper JD, Simonsick EM, Ferrucci L, Fried LP. The protective effect of emotional vitality on adverse health outcomes in disabled older women. Journal of the American Geriatric Society. 2000;48:1359–1366. doi: 10.1111/j.1532-5415.2000.tb02622.x. [DOI] [PubMed] [Google Scholar]
- Radloff LS. The CES-D Scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Reeves MJ, Bushnell CD, Howard G, Gargano JW, Duncan PW, Lynch G, Khatiwoda A, et al. Sex differences in stroke: Epidemiology, clinical presentation, medical care, and outcomes. Lancet Neurology. 2008;7:915–926. doi: 10.1016/S1474-4422(08)70193-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Riener CR. Doctoral dissertation. University of Virginia, 2007; 2007. An effect of mood on the perception of hill slant. [Google Scholar]
- Ryff CD, Singer B. Psychological well-being: Meaning, measurement, and implications for psychotherapy research. Psychotherapy & Psychosomatics. 1996;65:14–23. doi: 10.1159/000289026. [DOI] [PubMed] [Google Scholar]
- Smith PM, Illig SB, Fiedler RC, Hamilton BB, Ottenbacher KJ, Fielder RC. Intermodal agreement of follow-up telephone functional assessment using the Functional Independence Measure in patients with stroke. Archives of Physical Medicine & Rehabilitation. 1996;77:431–435. doi: 10.1016/s0003-9993(96)90029-5. [DOI] [PubMed] [Google Scholar]
- Spacapan S, Thompson SC. Perceived control in vulnerable populations. Journal of Social Issues. 1991;47:1–21. [Google Scholar]
- Stefanucci JK, Proffitt DR, Clore G, Parekh N. Skating down a steeper slope: Fear influences the perception of geographic slant. Perception. 2008;37:321–323. doi: 10.1068/p5796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stineman MG, Escarce JJ, Goin JE, Hamilton BB, Granger CV, Williams SV. A case-mix classification system for medical rehabilitation. Medical Care. 1994a;32:366–379. doi: 10.1097/00005650-199404000-00005. [DOI] [PubMed] [Google Scholar]
- Stineman MG, Hamilton BB, Granger CV, Goin JE, Escarce JJ, Williams SV. Four methods for characterizing disability in the formation of function related groups. Archives of Physical Medicine & Rehabilitation. 1994b;75:1277–1283. [PubMed] [Google Scholar]
- Stineman MG, Shea JA, Jette A, Tassoni CJ, Ottenbacher KJ, Fielder R, Granger CV. The Functional Independence Measure: Tests of scaling, assumptions, structure and reliability across 20 diverse impairment categories. Archives of Physical Medicine & Rehabilitation. 1996;77:1101–1108. doi: 10.1016/s0003-9993(96)90130-6. [DOI] [PubMed] [Google Scholar]
- Taylor SE, Brown JD. Positive illusions and well-being revisited: Separating fact from fiction. Psychological Bulletin. 1994;116:21–27. doi: 10.1037/0033-2909.116.1.21. [DOI] [PubMed] [Google Scholar]
- Turhan N, Ataly A, Muderrisoglu H. Predictors of functional outcome in first ever ischemic stroke: A special interest to ischemic subtypes, co-morbidity, and age. Neurorehabilitation. 2009;24:321–326. doi: 10.3233/NRE-2009-0485. [DOI] [PubMed] [Google Scholar]
- Zinn S, Dudley TK, Bosworth HB, Hoenig HM, Duncan PW, Horner RD. The effect of poststroke cognitive impairment on rehabilitation process and functional outcome. Archives of Physical Medicine & Rehabilitation. 2004;85:1084–1090. doi: 10.1016/j.apmr.2003.10.022. [DOI] [PubMed] [Google Scholar]