Abstract
Background & objectives
Even though Kerala State is well-known for its egalitarian policies in terms of healthcare, redistributive actions and social reforms, and its health indicators close to those of high-resource countries despite a poor per-capita income, it is not clear whether socio-economic disparities in terms of life expectancy are observed. This study was therefore carried out to study the impact of socio-economic level on life expectancy in individuals living in Kerala.
Methods
A cohort of 1,67,331 participants aged 34 years and above in Thiruvananthapuram district, having completed a lifestyle questionnaire at baseline in 1995, was followed up for mortality and cause of death until 2005. Survival estimates were based on the participants’ vital status and death rates were calculated separately for men and women and for several socio-economic factors, stratified by age.
Results
At 40 years, men and women were expected to live another 34 and 37 years, respectively. Life expectancy varied across the participants’ different socio-economic categories: those from high income households with good housing conditions, materially privileged households and small households, had a 2-3 years longer life expectancy as compared to the deprived persons. Also, those who went to college lived longer than the illiterates. The gaps between categories were wider in men than in women.
Interpretation & conclusions
Socio-economic disparity in longevity was observed: wealthy people from Kerala State presented a longer life expectancy.
Keywords: Developing countries, India, life expectancy, socio-economic factors
Improvements in disease prevention and treatment, nutritional intake, level of education, and living and working conditions have resulted in a better quality of life worldwide. One of the markers of the quality of life and national progress is life expectancy1. Inequalities in terms of longevity are observed both between and within countries. A dramatic increase in life expectancy was observed during the 20th century in both developed and developing countries. India for example, experienced a steady increase: before independence in 1947, life expectancy at birth increased from 24 years (1891) to 32 years (1941); however, since the 1950s longevity improved more rapidly, from 41 years (1951) to 61 years (2001)2,3. The latest estimation (2005) for India reports a life expectancy at birth of 62 years for men and 64 for women (men: 77 years and women: 81 years in UK, 75 and 80 in US; 79 and 86 in Japan)3.
Kerala State, in south India, is an exception within the Indian subcontinent. Within a few decades, it has achieved major demographic changes that have promoted greater gender equality, education and investment in human resources4. Despite having a poor per-capita income, Kerala's health indicators and life expectancy are close to those of high-resource countries5–7. According to the Kerala Government Statistics Bureau, in 1993-1995, life expectancy at birth in rural Kerala was 70 years for men and 77 years for women8. Social reforms have brought low poverty rates in urban and rural areas, accompanied by the highest literacy rate in India (Kerala: 90%, India: 65%), especially among women (Kerala: 88%, India: 54%), and a high average marriage age for women (Kerala: 23 years, India: 20 years in 2003)8–13.
However, social and healthcare reforms in Kerala State—the so-called Kerala model or Kerala formula—5,14–16 have presented some challenges such as a high unemployment rate among the educated, a high suicide rate, and a high morbidity rate5–7,17,18.
Socio-economic and demographic factors are known to influence the longevity within individuals, communities, regions or countries19. Although evidence on social inequalities in health comes mostly from high-resource countries, reports from India frequently examine caste associated with health outcome; caste being a marker of socio-economic status. In a recent review, Nayar found that the upper caste group was more likely to use health facilities (for immunization, maternal care, treatments) and had a better health status20. Based on Mumbai cancer registry data, Kurkure and Yeole reported that cancer survival and cancer mortality were both associated with levels of occupation and education21. Kerala's social reforms have aimed to equally distribute wealth to the different social strata, therefore, everyone is expected to benefit from the same developments. The objective of the present study was to address the impact of the socio-economic level on their life expectancy, even though social reforms have closed the gap between individuals.
We present longevity estimates according to socio-economic markers; these estimates are based on actual mortality rates, from an ongoing population-based cohort study in Thiruvananthapuram district, India, jointly organized by the Regional Cancer Centre, Thiruvananthapuram, India and the International Agency for Research on Cancer, Lyon, France.
Material & Methods
The mortality data used in the present study were collected from an ongoing cluster-randomised community-based oral cancer screening trial implemented to evaluate the efficacy of oral visual inspection on oral cancer incidence and mortality. In brief, among 13 panchayaths used as clusters in a rural area of Thiruvananthapuram district, seven were randomised to receive three rounds of oral visual screening by trained health workers at 3-year intervals, and six to a control group to receive health education on the detrimental effects of tobacco and alcohol use and be encouraged to use health-care facilities if needed22,23. Screen-positive persons with suggestive precancerous or cancerous oral lesions were referred to dentists and oncologists for further investigations, and screen-negative individuals were advised to receive repeat screening after 3 years. Both screened and control groups are currently being followed up for cancer incidence and mortality.
A total of 1,91,873 apparently healthy subjects aged 34 and older were eligible; of whom 1,67,331 were recruited from January 1, 1995 and followed up until December 31, 2005 (participation rate: 87% in all, 80% in men, 93% in women). The study protocol was reviewed and approved by both the Scientific and Human Ethics Committees of the Regional Cancer Centre, Thiruvananthapuram and the International Agency for Research on Cancer, Lyon, France. A written informed consent was obtained from each participant.
All participants answered a lifestyle questionnaire administered by trained health workers during house visits. Information on sex, age, education level (illiterate, 1-7 years, 8-10 years, college), occupation [blue collar (manual, technical worker and artisan), white collar (teacher, office worker, professional, and retiree), business, unemployed, housewife], standard of living based on household assets (deprived, middle, privileged), number of permanent household residents, type of house (thatched hut or pucca, tiled hut or pucca, concrete), and total monthly household income in rupees (<1500, 1500-3000, 3001-5000, >5000) were collected. Households were classified as privileged when they had a car, a washing machine or a geyser, as middle when they had a television, a bicycle, a fridge, a cooking gas, a scooter, toilets inside home or a phone and as deprived when they had an audio, a radio or none of the previous items.
Participants with missing information on sex (n=1), and age (n=866) were excluded, which brought the total study sample to 1,66,464 persons (66,466 men and 99,998 women). Income level and household assets were included in the questionnaires of the first two rounds, but not at the third round. Consequently, longevity according to these two items was estimated on 1, 31, 242 individuals.
Each study participant was actively followed up for vital status by field workers through municipal death registers, death records from mosques, churches and social organisations, and during repeated house visits (every 3 years in general). If medical records were not available, the cause of death was established by interviewing a close family member of the deceased person using a verbal autopsy questionnaire24; these questionnaires were then reviewed by a medical doctor for coding the cause of death according to the International Classification of Diseases – 10th Revision25.
Hazards ratios (HR) of mortality were computed using the Cox regression methods, and confidence intervals were based on Wald statistics. Risks were estimated for gender, education level, and monthly income in a multivariate analysis, adjusted for age, gender, education level, income, household assets, house type, randomization group, and number of household residents. Risks of mortality as compared to staying alive were calculated using the Statistical Analysis System (SAS) PHREG procedure26.
For each year of follow up, frequency tables were constructed including the number of participants present at the beginning of that year and the number of deaths occurring during the year, for each single year of age. Then the frequency tables were combined in a single table, by single year of age; it included the total number of persons followed up [or person-years (P-Yrs)] and the total number of deaths by single year of age. Frequency tables were constructed using Excel software.
The mortality rate (Mx) for each single age was defined as the number of deaths between agex and agex+1 divided by the P-Yrs at agex. The probability of dying between agex and agex+1 was defined as qx = 1 – exp-Mx.
Probabilities were estimated for each category of the demographic and socio-economic variables of interest: sex, level of education, occupation, household assets, number of permanent household residents, type of house, and total household income per month.
Probabilities qx were entered in single-year single-decrement life tables in order to estimate life expectancy. At the age of 80, a value of 1 was given (i.e. 100% of the persons were dead at 80). Usually, in life tables produced by the Census Bureau of India, qx = 1 is for age 70 and over; in the present study, enough death cases were available to construct life tables until the age of 80.
Life expectancy according to the socio-economic factors was estimated for all participants, then in men and women separately, for categories including more than 80 death cases. Life expectancy is defined as the number of years a person at a specific age is expected to live and was calculated as ex = Tx / Lx, where
ex = life expectancy of persons alive at agex
Tx = total number of P-Yrs lived by all members of the cohort beyond the agex
Lx = total number of P-Yrs lived by the cohort from agex to agex+1.
Results
A total of 11,764 deaths were registered during the follow-up period. The main causes of death, recorded for 88 per cent of death cases, were chronic and non-communicable diseases. Cardiovascular diseases represented the first cause of death (42%), before cancer (13%) and chronic respiratory diseases (12%).
The Table shows death rates and mortality risks according to gender, education level and monthly income. About 20 per cent were not literate while more than 12 per cent of the study population received a college education. More than half of the subjects had a low household income, and only 8 per cent had an income of more than 5000 Rupees per month. Women had lower mortality rates and risks than men. Mortality rates and adjusted risks decreased with increased level of education, and monthly income in a significant dose-response relationship.
Table.
Characteristics of the participants, mortality rates (per 1000 Person-Years) and mortality risks according to main determinants
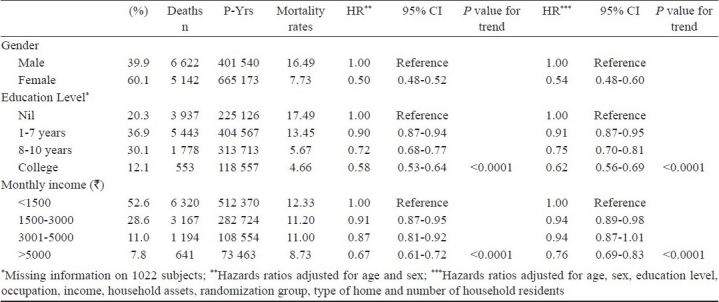
Fig. 1 shows the remaining years of life at 40 years old, according to various factors. At age 40, the study participants were expected to live on average an additional 35.5 years. Women were expected to live three years longer than men (33.8 years for men and 36.9 years for women). Longevity increased with increased education level and increased income level (2 years difference between the low- and the high-income groups). Similarly, according to the household assets, the longevity gap between the deprived and privileged households was 1.5 years, the deprived being expected to live 34.9 years more, while the privileged 36.3 years more. Remaining years of life also differed according to the housing conditions, such as construction quality of the house (1.5 years gap) and the number of residents in the household (1.5 years difference). Those unemployed had a shorter life expectancy, followed by the blue-collar workers and the business people.
Fig. 1.
Remaining years to live at age 40 according to demographic and socio-economic factors.
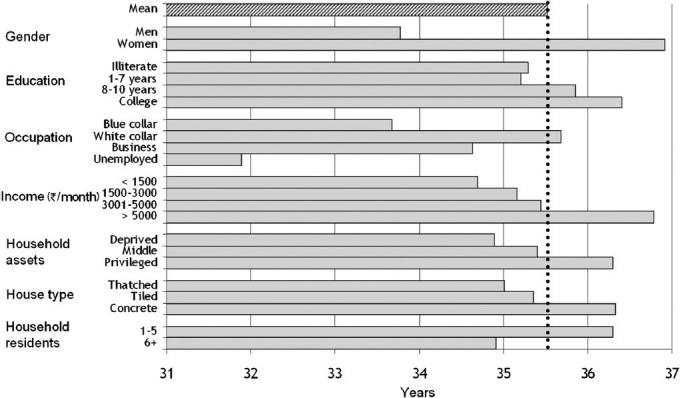
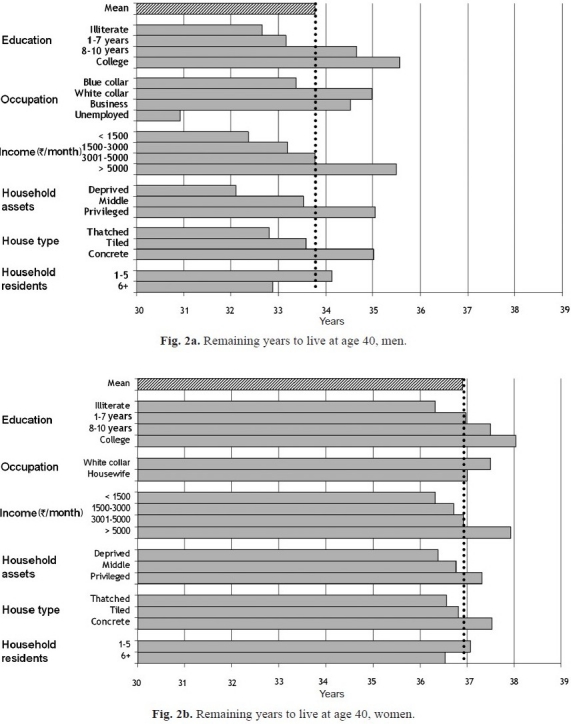
Fig. 2 shows the estimation of life expectancy at age 40, for men and women separately. In both genders, a high socio-economic level was synonymous with a longer life, although the difference between the lower and the higher groups was larger in men. Unemployed men had the shortest remaining life to live, while white collar workers had the longest. Women in the white-collar occupation category lived 6 months longer than housewives.
Fig. 2.
Discussion
An unequal socio-economic distribution in populations is the result of historical, cultural, political, economic and governance processes. These factors ultimately influence the resources available to individuals and populations and shape the nature of investments in public infrastructure related to education, health services, social welfare, household food availability, housing, employment opportunities, transportation, and environmental controls, among others. Socio-economic differentials have generally been associated with significant differences in the general health of populations. These differences are accompanied by many differences in quality of life, both at the individual and the community level that may adversely affect health and survival of populations. The effect of socio-economic inequality on health and longevity reflects a combination of negative exposures and lack of resources by individuals.
Although successive administrations in Kerala in the past several decades are well-known for egalitarian policies in terms of healthcare and social reforms4, and greater redistributive actions, we studied socio-economic differentials in health among a peri-urban population near the capital city of Thiruvananthapuram. Those belonging to the socially disadvantaged categories experienced a higher mortality rate. This is exemplified by the longer life expectancy for the better-off group, with high income. The unfavourable longevity experienced among the unemployed may be a reflection of a poor physical or mental health, often linked to increased mortality rates27. However, this association could not be verified.
Social inequalities in longevity have been extensively reported in affluent societies; evidence from low-resource countries has also recently been described28–34. To our knowledge, these are the first estimates of life expectancy in India according to the socio-economic status, based on the results of a large prospective study. Our findings are consistent with observations from developed and developing countries. An ecological study of factors associated with mortality rates among middle-aged Indian adults, based on national data, showed higher mortality rates among the more deprived35. Progressive healthcare policies in Kerala have provided an easy access to healthcare services to everyone, with a health dispensary within 2 km and a hospital within 5 km of every home4. However, a survey showed that, with the rapid expansion of the private medical sector in Kerala, wealthy individuals are more likely to seek for expensive medical care than for free care36. Nevertheless, it is difficult to say whether this phenomenon can explain the observed health disparities.
In the present study, causes of death were similarly distributed across the different socio-economic indicators, the first cause of death being cardiovascular diseases, and the second being either cancer or respiratory diseases. A cross-sectional survey performed in Kerala State in 1996 reported that vascular disease death ranked first (30% of total deaths), followed by cancer (9%) and accidents (6%)17.
Death registration in low-resource countries is well known for its incompleteness, and Kerala State is no exception. However, we tried to overcome this problem by actively collecting death information from mosques, churches, and repeated house visits. These visits have significantly amplified the proportion of information on death, as compared to the information from the government registries. Moreover, the cause of death also neared completeness by using verbal autopsy, when medical information was not available. The study population included rural and semi-urban communities, with a socio-economic distribution similar to the overall s0 tate, allowing generalization of the findings for Kerala State.
Although a complete life table from birth could not be constructed, the present truncated estimates are based on actual age-specific death rates thanks to the large study sample and the long follow-up duration.
The main causes of high mortality, such as poor sanitation, wide-spread hunger, famine and malnutrition, inadequate access to healthcare and poor education, are not generally applicable to most populations living in Kerala State. Chronic diseases such as cardiovascular diseases and cancers lead to greater morbidity, one of the characteristics of the State5. Increasing life expectancy and the ageing of the population go along with increasing prevalence of non-communicable diseases37. It is important to recognize and respond to emerging challenges in health and welfare in view of the longer longevity, ageing populations and high frequency of chronic diseases, if the already achieved health benefits and progress are to be sustained.
In conclusion, “live better, live longer” is not only the privilege of those in highly developed countries. Despite the overall progress in health and longevity in a low-resource region like the State of Kerala, India, socio-economic disparities in health are prominently observed at the population level38.
Acknowledgments
This project was supported by a grant from the Association for International Cancer Research (AICR) St Andrews, UK. Additional data collection was supported by the Cancer Research UK (CRUK), UK. The authors are grateful to the study participants and their families, the assistance of the staff of the Panchayath offices, of mortality registries, and of the Trivandrum population-based cancer registry.
References
- 1.Rogers RG, Wofford S. Life expectancy in less developed countries: socioeconomic development or public health? J Biosoc Sci. 1989;21:245–52. doi: 10.1017/s0021932000017934. [DOI] [PubMed] [Google Scholar]
- 2.United Nations. Demographic Yearbook, historical supplement. United Nations Publications. 2008. [accessed on February 20, 2008]. Available from: http://unstats.un.org/unsd/demographic/products/dyb/DYBHist/HistTab09a.pdf .
- 3.WHO. WHO Statistical Information System. 2007. [accessed on February 27, 2008]. Available from: http://www.who.int/whosis/database/core/core_select_process.cfm .
- 4.Franke RW, Chasin BH. Kerala State, India: radical reform as development. Int J Health Serv. 1992;22:139–56. doi: 10.2190/HMXD-PNQF-2X2L-C8TR. [DOI] [PubMed] [Google Scholar]
- 5.Kannan KP, Thankappan KR, Ramankutty V, Aravindan KP. Kerala: a unique model of development. Health Millions. 1991;17:30–3. [PubMed] [Google Scholar]
- 6.Kutty VR. Historical analysis of the development of health care facilities in Kerala State, India. Health Policy Plan. 2000;15:103–9. doi: 10.1093/heapol/15.1.103. [DOI] [PubMed] [Google Scholar]
- 7.Sen A. Health: perception versus observation. BMJ. 2002;324:860–1. doi: 10.1136/bmj.324.7342.860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kerala Government. Vital Statistics. Government of Kerala. 2008. [accessed on February 29, 2008]. Available from: www.kerala.gov.in/statistical/vitalstatistics/vitalstatistics_index.htm .
- 9.Census of India. Office of the Registrar General & Census Commissioner, India. 2008. [accessed on March 1, 2008]. Available from: http://www.censusindia.gov.in/Census_Data_2001/India_at_glance/literates1.aspx .
- 10.Kutty VR, Thankappan KR, Kannan KP, Aravindan KP. How socioeconomic status affects birth and death rates in rural Kerala, India: results of a health study. Int J Health Serv. 1993;23:373–86. doi: 10.2190/9N4P-F1L2-13HM-CQVW. [DOI] [PubMed] [Google Scholar]
- 11.Ministry of Health and Family Welfare, Government of India. 2005-2006 National Family Health Survey (NFHS-3): National Fact Sheet Kerala. International Institute for Population Sciences, Deonar, Mumbai. 2008. [accessed on February 29, 2008]. Available from: www.nfhsindia.org .
- 12.Ministry of Health and Family Welfare Government of India. 2005-2006 National Family Health Survey (NFHS-3): National Fact Sheet India. International Institute for Population Sciences, Deonar, Mumbai. 2008. [accessed on February 29, 2008]. Available from: www.nfhsindia.org .
- 13.Mohindra KS. A report on women Self Help Groups (SHGs) in Kerala state, India: a public health perspective. Department of Social Medicine and Prevention, University of Montreal. 2003. Mar, [accessed on March 1, 2008]. Available from: http://www.cacis.umontreal.ca/Katia_rapport_final.pdf .
- 14.Franke RW. Is there a Kerala model? World Malayalee Convention '95. 1995. Jul 1, Available from: www.chss.montclair.edu/anthro/julypap.html .
- 15.Nag M. The Kerala formula. World Health Forum. 1988;9:258–62. [PubMed] [Google Scholar]
- 16.Nath I, Reddy KS, Dinshaw KA, Bhisey AN, Krishnaswami K, Bhan MK, et al. Country profile: India. Lancet. 1998;351:1265–75. doi: 10.1016/s0140-6736(98)03010-4. [DOI] [PubMed] [Google Scholar]
- 17.Kunhikannan TP, Aravindan KP. Changes in the Health Status of Kerala 1987-1997. Kerala Research Programme on Local Level Development, Centre for Development Studies, Thiruvananthapuram. 2000. [accessed on February 28, 2008]. Available from: http://www.krpcds.org/kunhikannan.pdf .
- 18.Sauvaget C, Ramadas K, Fayette JM, Thomas G, Thara S, Sankaranarayanan R. Completed suicide in adults of rural Kerala: Rates and determinants. Nat Med J India. 2009;22:228–33. [PubMed] [Google Scholar]
- 19.Baru RV, Sivaramakrishnan K. The Commission on Social Determinants of Health: mainstreaming social inequalities in public health education in India. Natl Med J India. 2009;22:33–4. [PubMed] [Google Scholar]
- 20.Nayar KR. Social exclusion, caste & health: a review based on the social determinants framework. Indian J Med Res. 2007;126:355–63. [PubMed] [Google Scholar]
- 21.Kurkure AP, Yeole BB. Social inequalities in cancer with special reference to South Asian countries. Asian Pac J Cancer Prev. 2006;7:36–40. [PubMed] [Google Scholar]
- 22.Sankaranarayanan R, Ramadas K, Thomas G, Muwonge R, Thara S, Mathew B, et al. Effect of screening on oral cancer mortality in Kerala, India: a cluster-randomised controlled trial. Lancet. 2005;365:1927–33. doi: 10.1016/S0140-6736(05)66658-5. [DOI] [PubMed] [Google Scholar]
- 23.Sankaranarayanan R, Mathew B, Jacob BJ, Thomas G, Somanathan T, Pisani P, et al. Early findings from a community-based, cluster-randomized, controlled oral cancer screening trial in Kerala, India. Cancer. 2000;88:664–73. [PubMed] [Google Scholar]
- 24.Soleman N, Chandramohan D, Shibuya K. Verbal autopsy: current practices and challenges. Bull World Health Organ. 2006;84:239–45. doi: 10.2471/blt.05.027003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.International Statistical Classification of Diseases and Health Related Problems (The) ICD-10. 1st ed. Geneva: World Health Organization; 1996. World Health Organization. [Google Scholar]
- 26.SAS/STAT user's guide, version 9.3.1. Cary, USA: NC: SAS Institute Inc; 2002. SAS Institute Inc. [Google Scholar]
- 27.Beland F, Birch S, Stoddart G. Unemployment and health: contextual-level influences on the production of health in populations. Soc Sci Med. 2002;55:2033–52. doi: 10.1016/s0277-9536(01)00344-6. [DOI] [PubMed] [Google Scholar]
- 28.Bassuk SS, Berkman LF, Amick BC., III Socioeconomic status and mortality among the elderly: findings from four US communities. Am J Epidemiol. 2002;155:520–33. doi: 10.1093/aje/155.6.520. [DOI] [PubMed] [Google Scholar]
- 29.Davey SG, Hart C, Hole D, MacKinnon P, Gillis C, Watt G, et al. Education and occupational social class: which is the more important indicator of mortality risk? J Epidemiol Community Health. 1998;52:153–60. doi: 10.1136/jech.52.3.153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Hurt LS, Ronsmans C, Saha S. Effects of education and other socioeconomic factors on middle age mortality in rural Bangladesh. J Epidemiol Community Health. 2004;58:315–20. doi: 10.1136/jech.2003.007351. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pappas G, Queen S, Hadden W, Fisher G. The increasing disparity in mortality between socioeconomic groups in the United States, 1960 and 1986. N Engl J Med. 1993;329:103–9. doi: 10.1056/NEJM199307083290207. [DOI] [PubMed] [Google Scholar]
- 32.Smith GD, Bartley M, Blane D. The Black report on socioeconomic inequalities in health 10 years on. BMJ. 1990;301:373–7. doi: 10.1136/bmj.301.6748.373. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Subramanian SV, Davey SG, Subramanyam M. Indigenous health and socioeconomic status in India. PLoS Med. 2006;3:e421. doi: 10.1371/journal.pmed.0030421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Wilkinson RG. Socioeconomic determinants of health.Health inequalities: relative or absolute material standards? BMJ. 1997;314:591–5. doi: 10.1136/bmj.314.7080.591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Subramanian SV, Nandy S, Irving M, Gordon D, Lambert H, Davey SG. The mortality divide in India: the differential contributions of gender, caste, and standard of living across the life course. Am J Public Health. 2006;96:818–25. doi: 10.2105/AJPH.2004.060103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Chacko S. Health care in transition in Kerala. Lancet. 1989;2:620. doi: 10.1016/s0140-6736(89)90739-3. [DOI] [PubMed] [Google Scholar]
- 37.Gupte MD, Ramachandran V, Mutatkar RK. Epidemiological profile of India: historical and contemporary perspectives. J Biosci. 2001;26:437–64. doi: 10.1007/BF02704746. [DOI] [PubMed] [Google Scholar]
- 38.Antony GM, Rao KV. A composite index to explain variations in poverty, health, nutritional status and standard of living: use of multivariate statistical methods. Public Health. 2007;121:578–87. doi: 10.1016/j.puhe.2006.10.018. [DOI] [PubMed] [Google Scholar]


