Abstract
BACKGROUND
Empirical evidence has only weakly supported antidepressant treatment for patients with co-occurring depression and alcohol dependence. While some studies have demonstrated that antidepressants reduce these patients’ depressive symptoms, most studies have not found antidepressants helpful in reducing excessive drinking in these patients. We provide results from a double blind, placebo-controlled trial that evaluated the efficacy of combining approved medications for depression (sertraline) and alcohol dependence (naltrexone) for treating patients with both disorders.
METHODS
170 depressed, alcohol-dependent patients were randomized for 14 weeks to sertraline (200mg/day), naltrexone (100mg/day), the combination, or placebo, while receiving weekly cognitive behavioral therapy.
RESULTS
The sertraline + naltrexone combination produced a higher alcohol abstinence rate (53.7%; p = .001; odds ratio = 3.7), and a longer delay before relapse to heavy drinking (98 median days; p = .003; d = .54), than the other treatments: naltrexone (21.3% abstinent, 29 days), sertraline (27.5% abstinent, 23 days), or placebo (23.1% abstinent, 26 days). There also was a trend for more patients in the medication combination group not to be depressed by the end of treatment (83.3%; p = .014; odds ratio = 3.6), compared to the other treatments. The serious adverse event rate was 25.9%, with fewer reported by the medication combination group (11.9%; p < .02) than the other treatments.
CONCLUSION
More depressed, alcohol-dependent patients taking the sertraline + naltrexone combination achieved abstinence from alcohol, delayed relapse to heavy drinking, reported fewer serious adverse events, and tended not to be depressed by the end of treatment.
Keywords: combining medications, depression, alcohol, sertraline, naltrexone, clinical trial
A Double Blind, Placebo-Controlled Trial that Combines Sertraline and Naltrexone for Treating Co-Occurring Depression and Alcohol Dependence
Empirical data that support effective pharmacotherapy for the frequent combination of depression and alcohol dependence are long overdue (1–3). Each disorder carries a significant risk for the development of the other (2–5), and high severity in one disorder is associated with high severity in the other (4, 5); alcohol dependence prolongs the course of depression (6, 7); and the persistence of depression during abstinence from alcohol is a risk factor for relapse to heavy drinking (6, 8–10). Thus, logic dictates that both disorders be identified and managed when treating these patients.
Antidepressant Treatment for Depressed Patients with Alcohol Dependence
Empirical evidence for the efficacy of antidepressants for alleviating depressive symptoms in depressed, alcohol-dependent patients is limited and results are contradictory across the few existing studies. That is, there are fewer than a dozen well-controlled antidepressant trials with depressed, alcohol-dependent patients, and only one is a large multi-site study (11). Findings from the multi-site trial were that a selective serotonin reuptake inhibitor (SSRI), sertraline, prescribed at 50 to 150mg /day for 10 weeks, provided no advantage over placebo for reducing depressive symptoms, nor did it reduce drinking. This finding challenged two independent reviews of the other controlled trials, which reported that antidepressants alleviated depression, but had little impact on reducing drinking (12, 13). Pettinati and colleagues’ (13) review of the controlled studies concluded that an antidepressant alleviated depressive symptoms in 75% of studies, but reduced drinking in only 38% of studies.
Treating Depressed and Alcohol-Dependent Patients with Combination Medications
Because antidepressants do not appear to affect drinking in depressed alcohol-dependent patients, a medication that directly impacts drinking may be necessary for successful treatment. In an open-label study (14), 14 depressed, alcohol-dependent patients were given naltrexone (50mg/day), added to an SSRI. After 12 weeks, these patients decreased their drinking and showed additional mood improvement. One comparable, but placebo-controlled, study did not find an advantage in adding naltrexone to sertraline to further reduce drinking in 74 sertraline-treated depressed, alcohol-dependent older adults (15).
The present study is a single-site study that evaluated combining two FDA-approved medications, one for depression (sertraline) and one for alcohol dependence (naltrexone), to treat patients with both disorders. An important aim was to compare mood and drinking outcomes of this medication combination compared to placebo and treatments where each medication is prescribed. Sertraline was selected because most controlled studies investigating medications for co-occurring depression and alcohol dependence have prescribed an SSRI. Naltrexone, an opioid receptor antagonist, was selected for targeting drinking because it is well known to reduce heavy drinking in alcohol-dependent patients (16). We predicted that patients treated with the medication combination (an opiate antagonist and antidepressant) would achieve more abstinence, avoid relapse to heavy drinking, and reduce depressive symptoms than patients treated alternatively with naltrexone or sertraline or a placebo.
2. Methods
2.1 Patients
Patients were 170 men and women, 21 to 75 years, with current DSM-IV major depression and alcohol dependence diagnoses. Patients also have had to drink on average 12 or more alcoholic drinks per week and had a drink on 40% or more days in the 90 days before treatment. Patients had to have 3 consecutive abstinent days just before starting medication, and score 10 or higher on the Hamilton Rating Scale of Depression (HRSD) (17) at randomization. Patients were excluded if they had substance dependence besides alcohol or nicotine, or had bipolar-affective, schizophrenic, other psychotic, or organic mental disorders; were regularly taking an antidepressant; needed psychiatric medications other than an antidepressant; had a significant medical disease; or were pregnant or breastfeeding. The University of Pennsylvania’s Institutional Review Board approved the study, and all patients provided informed consent.
2.2 Patient Flow, Screening, and Treatment Initiation
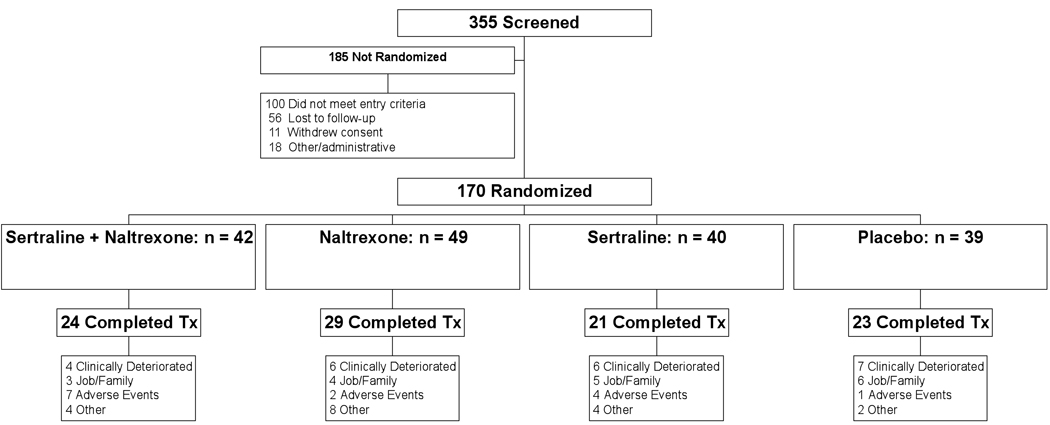
There were 355 patients screened and 170 were randomized to one of four medication conditions: naltrexone (100mg/day) and sertraline (200mg/day) (n = 42); naltrexone (100mg/day) and placebo (n = 49); sertraline (200mg/day) and placebo (n = 40); or double placebo (n = 39). Approximately 43% of the patients prematurely discontinued treatment because of: clinical deterioration (13.5%), job or family (10.6%), adverse events (8.2%), or other (10.6%). Clinical deterioration was defined as an escalation of depression and/or drinking necessitating medication and a clinical referral. There were no differences in the number of patients by reasons across groups. (See Figure 1.)
Figure 1.
Study Profile
Patients learned of the study from newspaper advertisements, local professionals, or friends and family, and after an initial telephone screening were invited for evaluation at the Treatment Research Center, a research-sponsored outpatient substance abuse treatment facility. Consenting patients went through baseline screening (1 week) and a 14-week medication trial. Urn randomization was used to evenly distribute patients across groups using four pre-treatment variables: gender, regular smoker ( > 5 cigarettes/week), randomization HRSD score: 10–20 vs. ≥ 21, and drinking frequency: fewer vs. ≥ 68% days drinking in past 90 days.
Treatment included weekly, individual cognitive-behavioral therapy (CBT) using the National Institute on Alcohol Abuse and Alcoholism Project MATCH manual (18), adapted to also treat depression.
Study medication was dispensed weekly in blister cards. At randomization, patients took 50 mg/day of naltrexone or placebo for 4 days and then added 50 mg/day of same for 3 days to the maximum naltrexone dose of 100mg/day. In the next week, patients added 50 mg/day of sertraline or placebo and were titrated up, adding 50 mg/day of same every third day, to the maximum sertraline dose of 200mg/day. Medical clinicians could exercise flexibility in dosing patients who could not tolerate maximum daily doses. Patients continued with treatment until the 13th week, when naltrexone was reduced to 50 mg/day while maintaining sertraline at 200mg/day. In the 14th week, naltrexone was continued at 50 mg/day and sertraline was reduced to 100mg/day. Medications were completed by the last treatment day.
While the FDA-recommended daily dose of sertraline for depression starts at 50mg/day, to give the maximum therapeutic benefits we chose a higher target dose, 200mg/day, because higher SSRI doses have been commonly prescribed in published studies for reducing drinking. Similarly, the FDA-recommended daily dose of naltrexone is 50mg/day, but we chose a target dose of 100mg/day because this higher dose was effective in the COMBINE study, the largest pharmacotherapy study for alcohol dependence (19). Also, some preclinical work suggested that naltrexone doses higher than 50mg/day might result in better outcomes (20).
2.3 Measures
Psychiatrically-trained clinicians (graduate degree) derived DSM-IV diagnoses using the Structured Clinical Interview for DSM–IV (SCID) (21). The SCID-IV is a 60-minute, semi-structured interview that yields current and lifetime DSM-IV psychiatric Axis I diagnoses, based on patient responses and clinician judgment. Patients had to have at least three of seven alcohol dependence symptoms in the past year, with evidence of the disorder in the past month. Patients had to have at least five of nine depression symptoms for 2 weeks in the past month with one symptom being depressed mood or loss of interest or pleasure. We primarily targeted alcohol-dependent patients with major or independent depression. Independent depression is: 1) less common than substance-induced depression with alcohol dependence (22); 2) less likely to dissipate with abstinence (23); and 3) more likely to respond to antidepressant treatment, although some have reported that these patients’ prognoses with pharmacotherapy can be similar in independent vs. substance-induced depression (24, 25). Additional SCID questions were asked to determine whether the depression was independent versus substance-induced.
A medical practitioner completed the medical history, physical exam, and pretreatment laboratory testing. Breathalyzer readings occurred at each visit to ensure data were collected when patients were abstinent. Adverse events were measured with the Systematic Assessment for Treatment Emergent Effects (26).
The Addiction Severity Index (27), a 45-minute semi-structured interview, was conducted at the screening visit to collect demographic information and clinical characteristics of patients before receiving treatment.
The depression outcome measure was the 24-item, symptom-based Hamilton Rating Scale of Depression (HRSD) (17). It is a semi-structured interview that was given by a psychiatrically-trained (graduate degree) clinician. The HRSD score was determined on the day of randomization, and weekly in-trial.
The drinking outcome measure was the Timeline Followback method (28). This is a semi-structured interview that uses memorable life events and a personalized calendar to prompt recall of drinking quantities per day during up to 90 days. The Timeline Followback method was administered in screening to record drinking in the past 90 days, and weekly in-trial. While the Timeline Followback is based on patient self-report, it has been shown repeatedly to be a reliable measure of drinking (28–29).
2.4 Statistical Analysis
Patients were compared on demographic, pre-treatment clinical characteristics, treatment attendance, medication adherence, and presence of adverse events with chi-square (χ2) tests for categorical characteristics, and 1-way analysis of variance (ANOVAs) for continuous characteristics. Medication adherence was defined as the percentage of prescribed pills taken while in treatment. The outcome analyses were intention-to-treat with two primary outcome measures for each of two outcome dimensions -- drinking and depression.
The two primary drinking outcomes were: 1) Total abstinence, and 2) Time to relapse. Total abstinence was defined as the percentage of patients who were abstinent on all days of the 14-week treatment period. Time to relapse was defined as the median number of days in treatment before a heavy drinking day. A heavy drinking day was defined as consuming in a day 5 or more drinks for men or 4 or more drinks for women.
Missing drinking data: Most patients (84.1%) provided drinking reports that were 100% complete, and the few missing reports were distributed evenly across groups. Because there were relatively few missing drinking reports, drinking outcome analyses were run on the unadjusted data.
The two primary depression outcomes were: 1) No depression at end of treatment (last 3 weeks), and 2) the HRSD in the last treatment week. No depression was defined by a 9 or lower score on the last HRSD in the final 3 treatment weeks. For the last treatment week analysis, mean HRSD scores were compared across groups.
Missing depression data: The proportion of patients providing HRSD scores in the last 3 treatment weeks was modest (67.1%) compared to the missing drinking report rate, and, thus, missing values tests were applied to HRSD scores (SPSS, v16). Results determined that non-existent HRSD data were missing completely at random (MCAR); i.e., there was no relationship between the fact that these data are missing and the value of these data (Little’s MCAR p values > 0.05) (30). These findings justified conducting the depression outcome analyses with unadjusted data.
For the primary drinking and depression outcomes, categorical data applied chi-square tests, time-to-event analyses applied Cox proportional hazards regression models, and continuous variables applied ANOVAs. The alpha was set to 0.01 to adjust for the overall group comparisons per four primary outcome variables. The alpha was fixed at 0.01 for a priori hypothesized planned subgroup contrasts, limited to comparing the two-medication group to the other three treatment groups combined. That is, the a priori study plan had determined that n=40 in the medication combination group and n=120 in the other three treatment groups combined, the study could detect moderate effect sizes between the two groups with 80% power while controlling for alpha = 0.01. Effect size estimates were computed with odds ratios for categorical outcomes and Cohen’s d statistic (31) for continuous outcomes.
Two secondary drinking outcomes were independently evaluated to determine support for the two primary drinking outcomes, and to allow for comparison with published drinking measures: percentage of patients not drinking heavily, and time to return to any drinking. These secondary analyses modeled the two primary drinking analyses with alpha set at 0.01.
3. Results
3.1 Demographic and Pre-Treatment Clinical Characteristics
The total sample’s average age was 43.4 years. Most were Caucasian (64.7%), male (62.4%), with a high school education (14.2 years), and were not currently married (78.8%). Most reported a family history of alcohol or drug problems (75.3%); approximately half reported a family history of depression (49.4%). Patients reported having alcohol problems for 21.1 years, and had received prior treatment 2.4 times. In the month before treatment, drinking occurred on 75.2 % days and heavy drinking on 68% days. Patients averaged 12.4 drinks per drinking day. The mean HRSD rating at randomization was 23.1. Table 1 provides pre-treatment information for the four treatment groups, and there were no differences for these variables among the groups.
Table 1.
Patient demographics and clinical characteristics, expressed as means, mean percentages or percent of patients
| Sertraline + Naltrexone | Naltrexone | Sertraline | Placebo | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Subjects (N=170) | (n=42) | (n=49) | (n=40) | (n=39) | ||||||||
| DEMOGRAPHICS | M or % | N | SD | M or % | N | SD | M or % | N | SD | M or % | N | SD |
| Age (years) | 43.4 | 10.2 | 42.9 | 8.1 | 43.9 | 11.5 | 43.4 | 8.9 | ||||
| Education (years) | 14.8 | 3.0 | 13.8 | 2.7 | 13.8 | 2.1 | 14.5 | 2.7 | ||||
| Sex (% male) | 57.1% | 24 | 67.3% | 33 | 67.5% | 27 | 56.4% | 22 | ||||
| Race (% Caucasian) | 73.8% | 31 | 65.3% | 32 | 55.0% | 22 | 64.1% | 25 | ||||
| Married (%) | 31.0% | 13 | 18.4% | 9 | 12.5% | 5 | 23.1% | 9 | ||||
| Smokers (% >5 cigarettes/day) | 33.3% | 14 | 34.7% | 17 | 40.0% | 16 | 51.3% | 20 | ||||
| SES (% mid-upper) | 78.6% | 33 | 71.4% | 35 | 65.0% | 26 | 71.8% | 28 | ||||
| Family Hx alcohol (%) | 59.5% | 25 | 67.3% | 33 | 72.5% | 29 | 76.9% | 30 | ||||
| Family Hx alcohol or drug (%) | 64.3% | 27 | 77.6% | 38 | 77.5% | 31 | 82.1% | 32 | ||||
| Family Hx depression (%) | 45.2% | 19 | 59.2% | 29 | 42.5% | 17 | 51.3% | 20 | ||||
| CLINICAL CHARACTERISTICS | ||||||||||||
| Years alcohol problem use | 22.2 | 10.5 | 21.3 | 8.3 | 21.7 | 10.6 | 19.3 | 10.1 | ||||
| Prior Drug and Alcohol Txs | 3.2 | 15.4 | 2.7 | 6.5 | 1.6 | 1.8 | 1.8 | 2.8 | ||||
| In past 30 days: | ||||||||||||
| Mean % days drinking | 71.0% | 23.6 | 77.3% | 22.9 | 73.4% | 21.7 | 79.0% | 21.3 | ||||
| Mean % days heavy drinking | 63.0% | 25.0 | 72.5% | 24.4 | 66.9% | 24.4 | 69.1% | 28.0 | ||||
| Drinks/drinking day | 12.8 | 9.2 | 13.6 | 6.9 | 12.4 | 5.6 | 10.5 | 5.9 | ||||
| Hamilton Rating Depression Scale | 23.7 | 6.7 | 22.3 | 5.7 | 23.4 | 6.0 | 22.9 | 7.0 | ||||
| Gamma-Glutamyl Transferase | 82.2 | 133.5 | 79.6 | 127.4 | 78.6 | 92.5 | 80.4 | 109.7 | ||||
M = Mean; SD = Standard Deviation; SES = Socioeconomic Status; Hx = History; Txs = Treatments
NOTE: There were no significant differences among the four groups on any of the variables listed in Table 1.
3.2 Treatment Attendance and Medication Adherence
Over the 14-week trial, patients attended 8.2 CBT sessions (59% of 14 possible sessions), and 3.4 support group meetings. The modal daily dosage, averaged across patients, was naltrexone = 91mg/day, and sertraline = 169.5mg/day. There were no significant group differences for any of these variables. The medication adherence rate for the total sample was 87%, and there were no differences among groups: sertraline + naltrexone = 90.9%; naltrexone = 84.9%; sertraline = 82.1%; and placebo = 90.5%. Most patients (73.5%) took at least 80% of their medications, and there were no differences in naltrexone versus sertraline adherence rates.
3.3 Adverse Events
No deaths or serious medical conditions occurred. The rate of serious adverse events was 25.9%, with the most frequent being inpatient detoxification and/or rehabilitation. The serious adverse event rate was significantly lower for sertraline + naltrexone patients (11.9%) than the other groups combined (χ2 = 5.7, df=1, p < 0.02; naltrexone=26.5%, sertraline=37.5%, placebo=28.2%). Adverse events ranged from mild to very severe. The most frequent adverse events reported as severe or very severe were anxiety/irritability (29%), fatigue (25%), decreased sexual desire (18%), headache (14%), nausea (8.2%), and orgasmic difficulty (11%). There were no statistical group differences in these rates. The numbers of patient discontinuations from an adverse event were: sertraline + naltrexone = 7, naltrexone = 2, sertraline = 4, and placebo = 1. While there were no statistical group differences, the sertraline + naltrexone group had 6 more patients discontinue treatment than the placebo group.
3.4 Primary Outcome Analyses
Table 2 presents the primary drinking and depression outcome results. Values are presented for each of the treatment groups, and the planned comparisons between the sertraline + naltrexone group and the alternative treatments combined.
Table 2.
In-trial patient outcomes for drinking and depression, expressed as percentage of patients or means
| Patients (N=170) | Sertraline + Naltrexone |
Naltrexone | Sertraline | Placebo | Sertraline + Naltrexone group vs. other groups combined |
|||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
P rimary Outcomes - Drinking and Depression |
% or M |
N | SD |
% or M |
N | SD |
% or M |
N | SD |
% or M |
N | SD |
χ2 or t |
p |
Odds Ratio or Cohen's d |
95% CI |
| Total Abstinence in Tx (% patients) |
53.7% (n=41) |
22 | 21.3% (n=47) |
10 | 27.5% (n=40) |
11 | 23.1% (n=39) |
9 | 12.9 | 0.001 | OR = 3.7 | 1.8 – 7.8 | ||||
| Time (days) to Relapse to Heavy Drinking (≥5 drinks/drink day--men; ≥4 drinks/drink day--women) |
Md=98 63.6 (n=41) |
40.8 | Md=29 45.2 (n=47) |
38.9 | Md=23 39.9 (n=40) |
38.3 | Md=26 41.7 (n=39) |
38.0 | 3.0 | 0.003 | d = 0.54 | .19 – .89 | ||||
| Not Depressed at Tx End (% patients w/Hamilton depression rating ≤ 9 in Last 3 Tx Weeks) |
83.3% (n=30) |
25 | 68.8% (n=32) |
22 | 48.1% (n=27) |
13 | 56% (n=25) |
14 | 6.1 | 0.014 | OR = 3.6 | 1.2 – 10.2 | ||||
| Hamilton Rating of Depression at Tx End |
6.9 (n=27) |
6.1 | 8 (n=29) |
7.0 | 11.7 (n=26) |
7.3 | 10.2 (n=21) |
8.0 | 2.1 | 0.042 | d = 0.44 | .02 – .87 | ||||
M = Mean; SD = Standard Deviation; CI = Confidence Interval; Tx = Treatment; OR = Odds Ratio; Md = Median; d = Cohen's statistic
3.4.1 Primary Drinking Outcome Analyses
For total abstinence, there was a significant difference among the four groups (χ2 = 13.3, df = 3, p = 0.004), and more sertraline + naltrexone patients were abstinent from alcohol for the 14 treatment weeks (53.7%), than the other treatments combined (23.8%; χ2 = 12.9, df = 1, p = 0.001). A secondary analysis determined that the percent of patients not drinking heavily differed among the groups (χ2 = 13.2, df = 3, p = 0.004), and there were more sertraline + naltrexone (63.4%) patients who were not drinking heavily compared to the other treatments combined (34.1%; χ2 = 10.9, df = 1, p = 0.001).
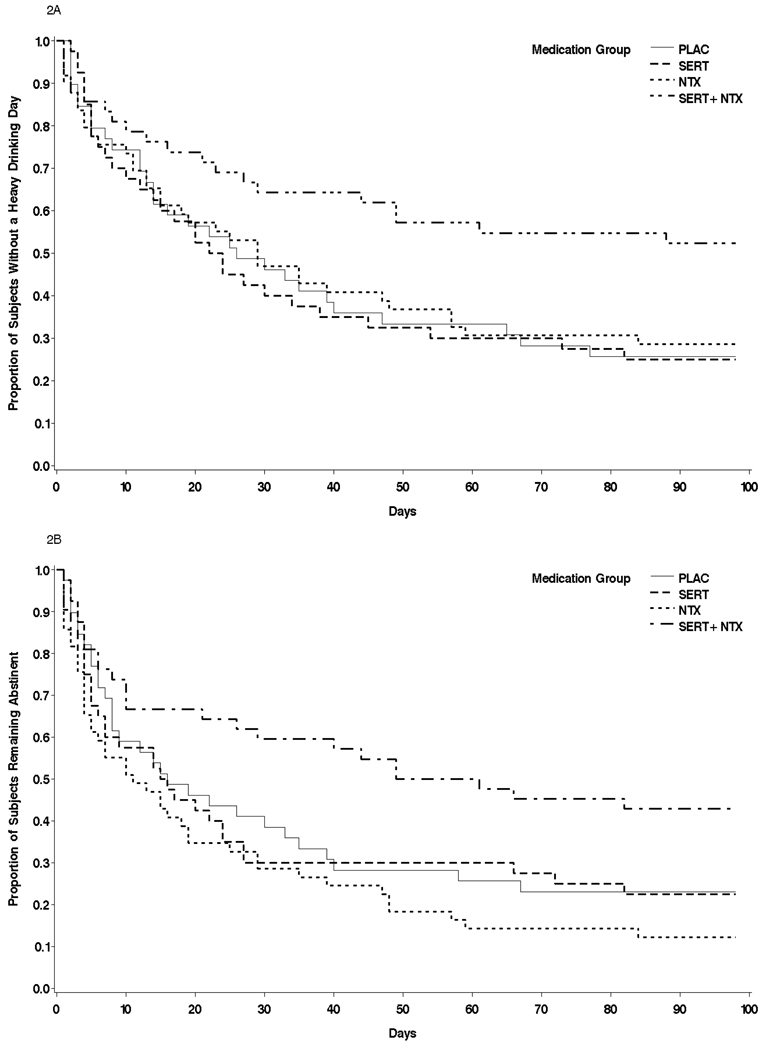
Survival analyses revealed that the time to return to heavy drinking approached significance among the groups: Cox proportional hazards = 8.29, df = 3, p = 0.04; and the a priori contrast revealed that the sertraline + naltrexone group went longer before relapsing to heavy drinking (median = 98 days), compared to the other treatments combined (26 days; t = 3.0, df = 165, p = 0.003). This finding was supported by a secondary outcome measure, return to any drinking, which revealed significant differences among the groups for any drinking: Cox proportional hazards = 11.55, df = 3, p = 0.01, and the sertraline + naltrexone group went longer before there was any drinking (median = 61 days), than the other treatments combined (15 days; t = 3.5, df = 165, p = 0.001). Figure 2 illustrates the two survival analyses.
Figure 2.
Time to First Heavy Drinking Day (Figure 2a – top panel), and Time to First Drinking Day (Figure 2b – bottom panel) for four medication conditions tested for treating co-occurring depression and alcohol dependence
3.4.2 Primary Depression Outcome Analyses
Table 2 provides the results for the primary depression outcomes: Percent of patients not depressed in the last 3 treatment weeks, and the Mean end-of-treatment HRSD depression rating. There were 67.1% patients with a HRSD score in the last 3 treatment weeks (71.4% sertraline + naltrexone; 67.5% sertraline; 65.3% naltrexone; 64.1% placebo; p = 0.90). “Not depressed” patients meant having a final HRSD score ≤ 9. The percent of non-depressed patients across the treatment groups at the end of treatment did not reach statistical significance with alpha corrected for multiple comparisons (χ2 = 8.9, df=3, p = 0.03), but the a priori comparison of non-depressed sertraline + naltrexone patients (83.3%) versus the other treatments combined clearly approached statistical significance (alpha level of 0.01 required) (58.3%; χ2 = 6.1, df=1, p = 0.014).
There were 60.6% patients who provided a HRSD score in the last week of the 14-week trial (64.3% sertraline + naltrexone; 65.0% sertraline; 59.2% naltrexone; 53.8% placebo; p = 0.72). The mean HRSD difference among the four groups in the last treatment week was not significant (F= 2.5, df=3, p = 0.06). The last treatment week mean HRSD of 6.9 in the sertraline + naltrexone group versus the other treatments combined (HRSD = 9.9), while in the predicted direction, also fell short of the 0.01 alpha level requirement (t = 2.1, df=1, p = 0.04).
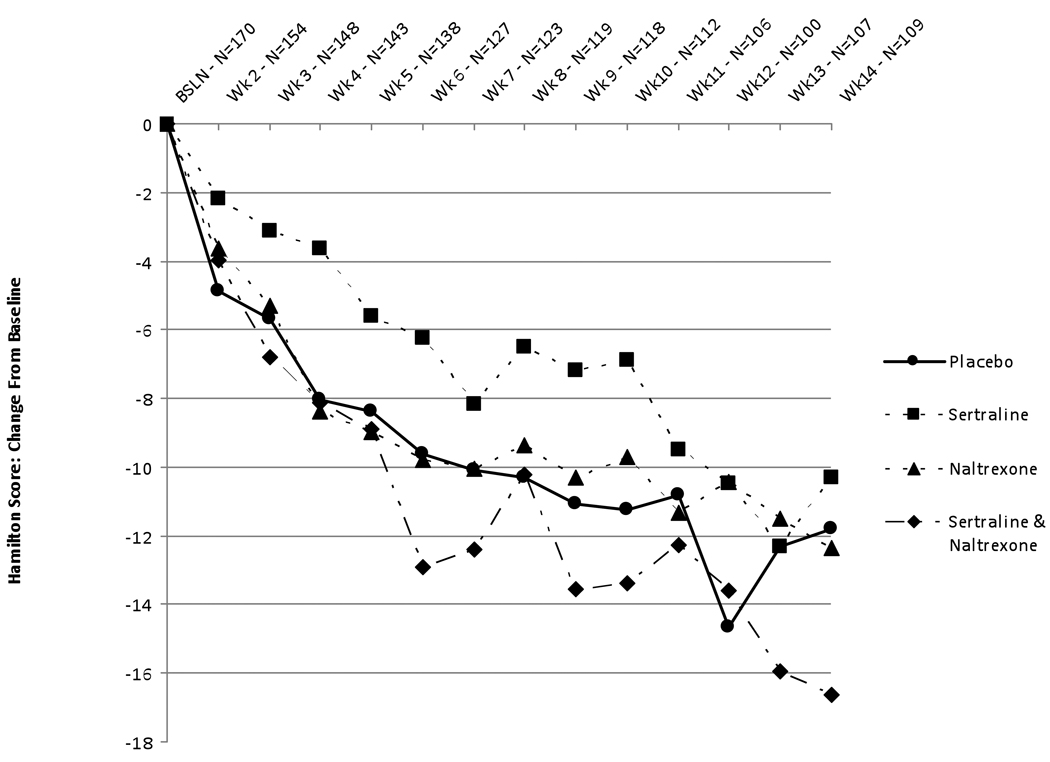
Figure 3 illustrates the weekly mean HRSD change from pre-treatment for each medication group. While there were no statistical differences among the groups across the 14 weeks, the sertraline + naltrexone group appeared to have lower HRSD scores on selected weeks, and the sertraline group appeared to have higher HRSD scores on selected weeks, compared to the other groups.
Figure 3.
Change in scores on the Hamilton Rating Scale of Depression across treatment weeks for four medication conditions tested for treating co-occurring depression and alcohol dependence
4. Discussion
Findings indicate that patients with co-occurring major depression and alcohol dependence might be optimally treated with combination pharmacotherapies that address each condition.
In the present study, more depressed, alcohol-dependent patients treated with the combination of sertraline (200mg/day) and naltrexone (100mg/day) achieved complete abstinence with treatment and significantly delayed relapse to heavy drinking, compared to a group taking single-medication treatments, namely, naltrexone, sertraline, or placebo. Secondary drinking analyses (no heavy drinking; time to first drink) supported primary drinking outcome results. There were also fewer serious adverse event reports in the medication combination group, essentially indicating that fewer patients required hospitalizations for alcohol detoxification or rehabilitation.
Also, Figure 2 illustrated that the time to relapse to heavy drinking, and to any drinking, portray relatively dramatic response differences early in treatment between the medication combination treatment versus the other three treatment groups. While a medication response before 2 weeks is inconsistent with the typical time it takes to observe an antidepressant mood response, little is known about the time it may take for drinking behavior to respond to an antidepressant in depressed, alcohol-dependent patients.
While all patient groups showed a clinical reduction in depressive symptoms, there was a trend for more patients to not be depressed in the last 3 treatment weeks if they had received the medication combination (sertraline and naltrexone), than if they were in the group of single-medication treatments, namely, naltrexone, sertraline, or placebo. The depression outcome findings were surprising in light of selected prior literature that reported that depressed, alcohol-dependent patients had a more robust reduction in depressive symptoms with an antidepressant than placebo. However, this study found no advantage for sertraline alone in depressive symptom reduction, and, potentially, portrayed a tendency for sertraline to have a slower mood improvement rate over the 14 weeks compared to the other treatment groups. A tentative observation from our depression outcome results, which do support those of the published multi-site sertraline study (11), is that there may be relatively little advantage in prescribing an antidepressant alone for depressed patients who are also alcohol dependent. Nonetheless, all patients had clinically significant reductions in depressive symptoms, which could be attributable to all patients receiving weekly CBT sessions. Alternatively, this study’s clinical sample might have had less of a problem with depression than with drinking, which is not easily captured by the measures we use to assess patients’ pre-treatment profiles.
Study limitations are that patients agreed to participate in a research study, and, may be different from non-research, clinical patients. Additionally, the treatment setting is an outpatient substance dependence treatment facility, and it is likely that depressed, alcohol-dependent patients who seek treatment at this type of facility are different from those who seek treatment at a general psychiatric or specialty depression clinic. Also, these study patients’ responses to sertraline and/or naltrexone cannot be generalized to other antidepressants or to other medications approved for treating alcohol dependence. Finally, we do not know if the ameliorative, short-term effects of our treatments are sustainable. Both of these disorders can be life-long illnesses.
In summary, the co-occurrence of depression and alcohol dependence is highly prevalent and difficult to treat successfully. This study’s findings suggest that these patients would benefit from a combination of an antidepressant and a medication for alcohol dependence. More medication-combination patients achieved abstinence from alcohol in treatment compared to a patient group taking single-medication or placebo treatments. Also, the medication-combination patients were not depressed at the end of treatment. These findings require replication before recommending changes in current clinical practices for treating co-occurring depression and alcohol dependence.
Acknowledgements
This study was funded by the National Institute on Alcohol Abuse and Alcoholism, grant #R01-AA09544-10 (Pettinati, PI). Pfizer Pharmaceuticals donated sertraline and matching placebo. These agencies had no role in the design, conduct or reporting of this study. We extend our appreciation to the many project staff and study participants. We thank Drs. Kevin Lynch, Robert Stout, and Jennifer Plebani for their advice in evaluating the results. We also thank Lauren Gent and Donna Giles for technical assistance.
Footnotes
A portion of this paper was presented at an invited symposium conducted at the 2009 annual meeting of the American Psychiatric Association, San Francisco, California.
References
- 1.Hesselbrock MN, Meyer RE, Keener JJ. Psychopathology in hospitalized alcoholics. Arch Gen Psychiatry. 1985;42(11):1050–1055. doi: 10.1001/archpsyc.1985.01790340028004. [DOI] [PubMed] [Google Scholar]
- 2.Kessler RC, Crum RM, Warner LA, Nelson CB, Schulenberg J, Anthony JC. Lifetime co-occurrence of DSM-III-R alcohol abuse and dependence with other psychiatric disorders in the National Comorbidity Survey. Arch Gen Psychiatry. 1997;54(4):313–321. doi: 10.1001/archpsyc.1997.01830160031005. [DOI] [PubMed] [Google Scholar]
- 3.Regier DA, Farmer ME, Rae DS, Locke BZ, Keith SJ, Judd LL, Goodwin FK. Comorbidity of mental disorders with alcohol and other drug abuse. Results from the Epidemiologic Catchment Area (ECA) Study. JAMA. 1990;264(19):2511–2518. [PubMed] [Google Scholar]
- 4.Gilman SE, Abraham HD. A longitudinal study of the order of onset of alcohol dependence and major depression. Drug Alcohol Depend. 2001;63(3):277–286. doi: 10.1016/s0376-8716(00)00216-7. [DOI] [PubMed] [Google Scholar]
- 5.Grant BF, Harford TC. Comorbidity between DSM-IV alcohol use disorders and major depression: Results of a national survey. Drug Alcohol Depend. 1995;39(3):197–206. doi: 10.1016/0376-8716(95)01160-4. [DOI] [PubMed] [Google Scholar]
- 6.Hasin DS, Tsai WY, Endicott J, Mueller TI, Coryell W, Keller M. Five-year course of major depression: Effects of comorbid alcoholism. J Affect Disord. 1996;41(1):63–70. doi: 10.1016/0165-0327(96)00068-7. [DOI] [PubMed] [Google Scholar]
- 7.Mueller TI, Lavori PW, Keller MB, Swartz A, Warshaw M, Hasin D, Coryell W, Endicott J, Rice J, Akiskal H. Prognostic effect of the variable course of alcoholism on the 10-year course of depression. Am J Psychiatry. 1994;151(5):701–706. doi: 10.1176/ajp.151.5.701. [DOI] [PubMed] [Google Scholar]
- 8.Greenfield SF, Weiss RD, Muenz LR, Vagge LM, Kelly JF, Bello LR, Michael J. The effect of depression on return to drinking: A prospective study. Arch Gen Psychiatry. 1998;55(3):259–265. doi: 10.1001/archpsyc.55.3.259. [DOI] [PubMed] [Google Scholar]
- 9.Hasin DS, Grant BF. Major depression in 6050 former drinkers: Association with past alcohol dependence. Arch Gen Psychiatry. 2002;59(9):794–800. doi: 10.1001/archpsyc.59.9.794. [DOI] [PubMed] [Google Scholar]
- 10.Kranzler HR, Del Boca FK, Rounsaville BJ. Comorbid psychiatric diagnosis predicts three-year outcomes in alcoholics: A posttreatment natural history study. J Stud Alcohol. 1996;57(6):619–626. doi: 10.15288/jsa.1996.57.619. [DOI] [PubMed] [Google Scholar]
- 11.Kranzler HR, Mueller T, Cornelius J, Pettinati HM, Moak D, Martin PR, Anthenelli R, Brower KJ, O'Malley S, Mason BJ, Hasin D, Keller M. Sertraline treatment of co-occurring alcohol dependence and major depression. J Clin Psychopharmacol. 2006;26(1):13–20. doi: 10.1097/01.jcp.0000194620.61868.35. [DOI] [PubMed] [Google Scholar]
- 12.Nunes EV, Levin FR. Treatment of depression in patients with alcohol or other drug dependence: A meta-analysis. JAMA. 2004;291(15):1887–1896. doi: 10.1001/jama.291.15.1887. [DOI] [PubMed] [Google Scholar]
- 13.Pettinati HM. Antidepressant treatment of co-occuring depression and alcohol dependence. Biol Psychiatry. 2004;56:785–792. doi: 10.1016/j.biopsych.2004.07.016. [DOI] [PubMed] [Google Scholar]
- 14.Salloum IM, Cornelius JR, Thase ME, Daley DC, Kirisci L, Spotts C. Naltrexone utility in depressed alcoholics. Psychopharmacol Bull. 1998;34(1):111–115. [PubMed] [Google Scholar]
- 15.Oslin DW. Treatment of late-life depression complicated by alcohol dependence. Am J Geriatr Psychiatry. 2005;13(6):491–500. doi: 10.1176/appi.ajgp.13.6.491. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Pettinati HM, O'Brien CP, Rabinowitz AR, Wortman SP, Oslin DW, Kampman KM, Dackis CA. The status of naltrexone in the treatment of alcohol dependence: Specific effects on heavy drinking. J Clin Psychopharmacol. 2006;26(6):610–625. doi: 10.1097/01.jcp.0000245566.52401.20. [DOI] [PubMed] [Google Scholar]
- 17.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Project MATCH Research Group. Matching Alcoholism Treatments to Client Heterogeneity: Project MATCH posttreatment drinking outcomes. J Stud Alcohol. 1997;58(1):7–29. [PubMed] [Google Scholar]
- 19.Anton RF, O'Malley SS, Ciraulo DA, Couper D, Donovan DM, Gastfriend DR, Hosking JD, Johnson BA, Locastro JS, Longabaugh R, Mason BJ, Mattson ME, Miller WR, Pettinati HM, Randall CL, Swift RM, Weiss RD, Williams LD, Zweben A. Combined pharmacotherapies and Behavioral Interventions for alcohol dependence. The COMBINE study: A randomized controlled trial. JAMA. 2006;295(17):2003–2017. doi: 10.1001/jama.295.17.2003. [DOI] [PubMed] [Google Scholar]
- 20.McCaul M, Wand G, Sullivan J, Mumford G, Quigley J. Beta-naltrexol level predicts alcohol relapse (abstract) Alcohol Clin Exp Res. 1997;21(3s) [Google Scholar]
- 21.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM IV Axis I Disorders - Patient Edition (SCID-I/P, Version 2.0). New York State Psychiatric Institute. New York: Biometrics Research Department; 1995. [Google Scholar]
- 22.Schuckit MA, Smith TL, Danko GP, Pierson J, Trim R, Nurnberger JI, Kramer J, Kuperman S, Bierut LJ, Hesselbrock V. A comparison of factors associated with substance-induced versus independent depressions. J Stud Alcohol Drugs. 2007 Nov;68(6):805–812. doi: 10.15288/jsad.2007.68.805. [DOI] [PubMed] [Google Scholar]
- 23.Schuckit MA. Comorbidity between substance use disorders and psychiatric conditions. Addiction. 2006 Sep;101 Suppl 1:76–88. doi: 10.1111/j.1360-0443.2006.01592.x. [DOI] [PubMed] [Google Scholar]
- 24.Mason BJ. Dosing Issues in the Pharmacotherapy of Alcoholism. Alcohol Clin Exp Res. 1996;20(s7):10A–16A. doi: 10.1111/j.1530-0277.1996.tb01184.x. [DOI] [PubMed] [Google Scholar]
- 25.Mason BJ, Kocsis JH. Desipramine treatment of alcoholism. Psychopharmacol Bull. 1991;27(2):155–161. [PubMed] [Google Scholar]
- 26.Rabkin JG, Markowitz JS, Ocepek-Welikson K, Wager SS. General versus systematic inquiry about emergent clinical events with SAFTEE: Implications for clinical research. J Clin Psychopharmacol. 1992;12:3–10. doi: 10.1097/00001573-199202000-00002. [DOI] [PubMed] [Google Scholar]
- 27.McLellan AT, Kushner H, Metzger D, Peters R, Smith I, Grissom G, Pettinati HM, Argeriou M. The Fifth Edition of the Addiction Severity Index. J Subst Abuse Treat. 1992;9(3):199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- 28.Sobell L, Sobell M. Timeline follow-back: A technique for assessing self-reported alcohol consumption. In: Allen LA, editor. Measuring Alcohol Consumption. Totowa, NJ: The Humana Press; 1992. [Google Scholar]
- 29.Sobell LC, Sobell MB, Leo GI, Cancilla A. Reliability of a timeline method: assessing normal drinkers' reports of recent drinking and a comparative evaluation across several populations. Br J Addict. 1988;83(4):393–402. doi: 10.1111/j.1360-0443.1988.tb00485.x. [DOI] [PubMed] [Google Scholar]
- 30.Little RJA, Rubin DB. Statistical analysis with missing data. New York: John Wiley & Sons, Inc.; 1987. [Google Scholar]
- 31.Cohen J. Statistical power analysis for the behavioral sciences. Hillsdale, NJ: Erlbaum; 1988. [Google Scholar]