Abstract
Objective:
Primary care asthma management is often not compatible with national evidence-based guidelines. The objective of this study was to assess the feasibility and impact of the Asthma APGAR tools to enhance implementation of asthma guideline-compatible management in primary care practices.
Subjects:
Twenty-four primary care practices across the US.
Methods:
This is a mixed methods study. Quantitative data were used to assess changes in guideline recommended asthma management including use of daily controller therapy, planned care visits, and education and information documentation before and after implementation of the Asthma APGAR. Qualitative data from focus group sessions were used to assess health care professional and patient perceived usability and value of the Asthma APGAR tools during office visits for asthma.
Results:
Implementing the Asthma APGAR tools in the 24 practices was associated with enhanced asthma visit-related medical record documentation including significant increases in recording of activity limitations due to asthma and asthma symptom frequency, asthma medication nonadherence, asthma triggers, and the patients’ perceived response to therapy (p < 0.01 for each item). Some care processes also increased significantly including assessment of inhaler technique and prescribing of daily controller therapy among patients with persistent asthma. Focus groups of patients and of clinical staff reported that the Asthma APGAR tools were easy to use, “made sense” and “improved care” was given and received.
Conclusions:
The Asthma APGAR tools are feasible to implement in primary care practices and their implementation is associated with increased guideline-compliant asthma management.
Keywords: asthma, guidelines, implementation, quality improvement, asthma control, mixed methods studies, qualitative research, primary care
Introduction
Asthma is a common chronic illness that results in significant burden for patients, families, and the health care system as well as significant preventable asthma morbidity and mortality (Yawn 2003; Savage-Brown et al 2005; Kelley et al 2005; Canino et al 2006; Yawn et al 2007). Among primary care practices, implementation of the national and international asthma guidelines has been shown to lower emergency health care resource utilization while improving patient outcomes (Bateman et al 2001, 2002). However, several barriers continue to slow the implementation of asthma guidelines into daily primary care practice (Cabana et al 2000; Diette et al 2001; Finkelstein et al 2002) including failure to document some very basic asthma-related information. Basic information such as symptom frequency, frequency of missed or modified activities due to those symptoms and information on triggers and therapy adherence appear in less than 40% of primary care medical record notes for asthma visits (Cabana et al 2000, 2005; Yawn et al 2005; Yawn and Yawn 2005; Diette et al 2007). Without this basic information it is difficult if not impossible to assess the effectiveness of current asthma control or reasons for failure to achieve asthma control (Vollmer 2004; Stoloff and Boushey 2006; Yawn et al 2006).
Some tools have been developed that facilitate collection of symptoms, activity, and use of rescue medications (Juniper et al 1999; Vollmer et al 2002; Nathan et al 2004; Skinner et al 2004; Quality Metrics 2005; Pinnock et al 2005; Michele & Amegavie 2005; Lenoir et al 2006; EPR Update 2007; Schatz et al 2006, 2007). While helpful in determining the level of control, these tools do not collect the crucial information required to identify potential reasons for poor control: trigger exposure, lack of adherence to prescribed therapy, and patient failure to see value in their asthma therapy.
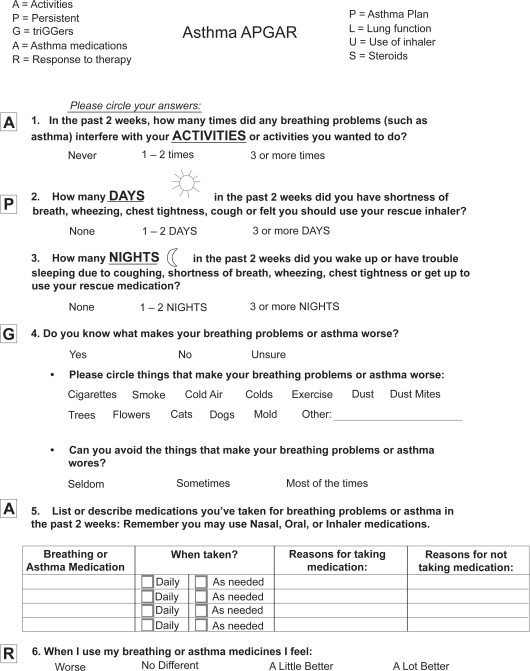
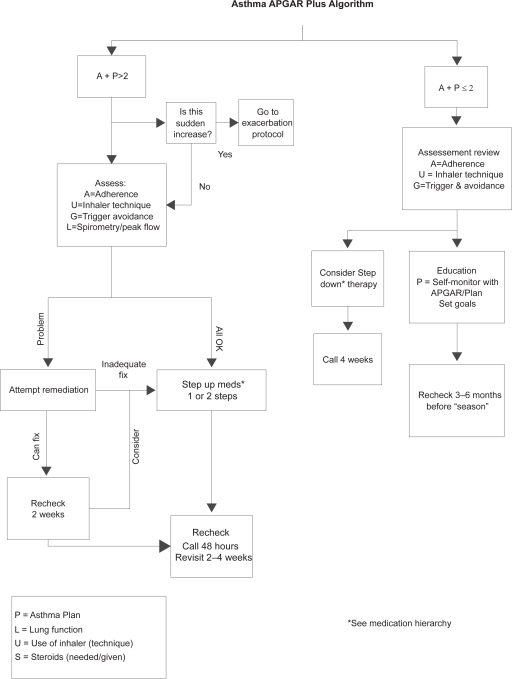
The Asthma APGAR was developed specifically to improve implementation of asthma guidelines in family medicine practices. The Asthma APGAR tools include a patient survey to collect the same information on found on control scores but adds patient reported information on asthma triggers, adherence to prescribed medications, and the patient’s perception of asthma relief from therapy. The cueing is intended to help physicians move beyond medication management to comprehensive asthma management. The second part of the Asthma APGAR is an asthma management algorithm that incorporates recommendations for asthma education, dealing with patient adherence to therapy, assessing and teaching proper inhaler technique, and employing follow-up visits for monitoring of asthma management as outlined in the 2007 NHLBI asthma guidelines (EPR Update 2007). The Asthma APGAR tools were developed by the authors in collaboration with practicing primary care physicians (Yawn 2004) thereby assuring that the tools are practical and have face validity for primary care physicians (Figures 1 and 2).
Figure 1.
Asthma APGAR – patient questions.
Figure 2.
Care algorithm.
This study presents data on the feasibility and impact of implementation of the Asthma APGAR tools in a network of primary care practices with emphasis on the processes of asthma management. The combination of qualitative and quantitative methodology allows the asthma care process results to be put in the context of patient and health care professional perceptions of the value of these tools in everyday asthma care.
Methods
This is a mixed methods study completed in US community based primary care practices (Westfall et al 2007). Quantitative data from medical record review were supplemented by qualitative data from patient and from health care professional focus groups.
After receiving approval from the Institutional Review Board of the Olmsted Medical Center and all 24 sites involved in the study, the Asthma APGAR tools were introduced into each of the 24 practices. The process was led by a physician/nurse team from each practice who attended a six hour training session (either face to face or by telephone conference call) during which the development and intended use of Asthma APGAR tools were explained. The tools of the Asthma APGAR include a practice assessment (Table 1), a patient (parent) completed Asthma APGAR survey (Figure 1), and the Asthma APGAR care algorithm (Figure 2). Attendees were given an update on asthma management based on asthma control and suggestions on how to introduce the Asthma APGAR tools to their practice colleagues.
Table 1.
Asthma APGAR practice audit questions
| Asthma APGAR Tool for practice assessment score: For each question: Y = yes present, N = not documented, and U = unsure. | ||
|---|---|---|
| 1. Activity: Was the number of missed activity days in the past 2 wks noted? | ||
| Y | N | U |
| 2. Persistence | ||
| a. Was the number of days with symptoms in the past 2 wks noted? | ||
| Y | N | U |
| b. Was the number of nights with symptoms in the past 2 wks noted? | ||
| Y | N | U |
| 3. TriGGers: Were triggers noted as being discussed? | ||
| Y | N | U |
| 4. Adherence to asthma medications: Were the type and frequency of asthma medications taken in the past 2 weeks noted? | ||
| Y | N | U |
| 5. Response to therapy: Was the patient’s response to therapy noted? | ||
| Y | N | U |
Within each enrolled practice, the lead physician and nurse completed the practice self-assessment by reviewing the medical records of 15 people who had been seen for an asthma visit (a visit with 493.xx as the first diagnostic code) during the previous six months. The records were reviewed from the date of most recent asthma visit retrospectively to identify documentation of the Asthma APGAR elements (Table 1). Review of multiple visits was allowed since not all information may be recorded at a single visit. This relatively simple practice self-assessment was used to help motivate the practice by providing information on current asthma care and gaps in that care suggested by the audit elements (Cabana et al 2005; Diette et al 2007; Solberg 2007).
In each practice, the lead physician and nurse used their practice’s audit data to facilitate an all-practice discussion of apparent strengths and gaps in current asthma management. Each of the practices agreed that data currently recorded in the medical record was inadequate to determine the level of asthma control. Furthermore, without knowing what the patient was actually taking (versus what was prescribed), and information on triggers, it was not possible to know how to modify currently used asthma therapies.
Based on identified practice gaps, review of the new asthma guidelines and introduction of the Asthma APGAR tools, each practice agreed to try implementing the Asthma APGAR tools as a practice change stimulus. During any identified asthma visit the patient (parent) would complete the Asthma APGAR survey that would be scored and linked to the care algorithm to direct asthma management. Specifically the frequency of daytime symptoms, the frequency of nighttime symptoms and the frequency of missed or modified activities as reported by the patient (parent) are each scored with a 0, 1, or 2 and then totaled (Figure 1). Any total score of 2 or greater (possible range 0 to 6) is consistent with “inadequate control” and directs the physician to the left side of the care management algorithm (Figure 2). For scores of 0 and 1, the user is directed to the “adequate control” or right side of the care algorithm. Both sides address issues such as inhaler technique demonstration and observation, asthma education and planned care visits, eg, follow-up visits at times other than during an exacerbation. The inadequate control side also includes assessment of adherence, trigger knowledge, and avoidance plus possible changes in medication therapy.
Both quantitative and qualitative data were collected to assess the impact of the Asthma APGAR tools. Quantitative data were collected from medical record review by experienced research nurse abstractors from the central site and included all the Asthma APGAR elements (Table 1) plus information on the presence of documentation regarding assessment or demonstration of inhaler technique, notation of any asthma education or of a nonacute asthma visit (planned care visit). Adherence was considered use of at least of 80% of the doses of prescribed medications being reported as taken. Data were collected from 40 patients per practice, 20 before, and another 20 nine months after Asthma APGAR implementation, half of which were children less than age 16. This data collection was completely separate from the practice audits done by the lead physician and nurse at each site. Patients were selected randomly from a list of all those making asthma visits in the six months prior to the review. The same patients were not used for before and after assessment since people make only 1.2 asthma visits per year on average (Yawn et al 2007) and therefore only the patients with the most severe asthma are likely to be seen during both the before and the after period of this study. Including only these patients would likely result in selection bias for more severe or more difficult to control cases of asthma.
Seven sites, selected for the greatest geographic (Pennsylvania, Washington State, Connecticut, and Minnesota) and practice type diversity (single and multi-specialty rural and suburban sites), held two focus groups per site (one with patients and one with health professionals) to supplement the quantitative information. Topics discussed in the focus groups included Asthma APGAR readability, ease of answering, as well as perceived relevance and value for the patient’s asthma care. A complete list of the focus group questions is available from the authors. Focus groups were led by two of the authors: BY took notes and SB asked the questions. For the patient focus group, the two authors were introduced as interested parties but not as the study principal investigator and study coordinator.
The Asthma APGAR practice assessment tools and patient survey were developed by one of the authors (BY) based on her previous research and the work of others that included the review of hundreds of medical record notations from asthma visits written by primary care physicians (Yawn 2004; Yawn et al 2007). The care management algorithm is based on information from existing national and international asthma guidelines (NAEPP and GINA) as well as in-depth review of the asthma management literature. Prior to the initiation of this study, several community-based family physicians reviewed, tested, and modified the Asthma APGAR tools used in this study (Yawn 2004).
To assess continued use of the Asthma APGAR system after study completion, we called all 24 sites to ask the lead physician, lead nurse, or the nursing supervisor whether the Asthma APGAR was still being used in practice. All follow-up was done at least 24 months after completion of the study.
Data analysis
Very simple statistical assessment was done to simulate what might be available for practice quality improvement activities. The before and after audit data were compared using Chi-squared statistics for each site, but are presented in aggregate since the direction and relative size of change were the same for all practices. Rates of change in the use of controller medications was based only on the care of the patients whose medical recorded were used to collect the “after” data. Current use of controller medication was compared to use of a controller medication at the latest visit made prior the practice’s implementation of the Asthma APGAR tools.
Qualitative data were analyzed using the editing method with both BY and SB reviewing all focus group data and identifying themes from each group and then for all patient groups and all health professional groups collectively (Crabtree 1999).
Results
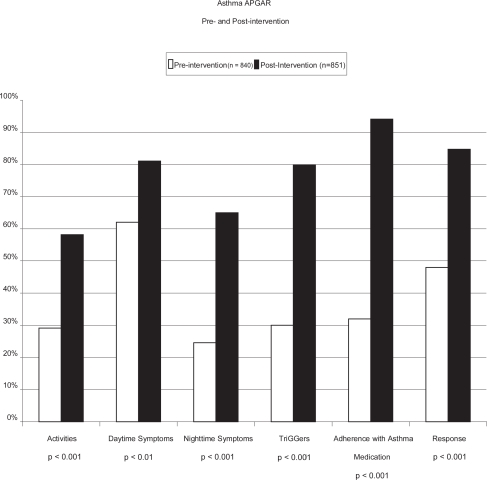
The 24 sites that participated in this study included 194 physicians plus 17 other clinicians. All but 5 practices were single specialty family medicine practices (Table 2). From the 24 sites, the medical records of 840 people with asthma were audited for baseline or before data and the medical records of 851 people with asthma were audited nine months following implementation of the Asthma APGAR.
Table 2.
Demographics of clinics, and clinician health professionals
| Clinic size N = 24 | n | Type of clinic N = 24 | n | MD N | NP/PA N | Location (States) | N | Male Clinicians % | Average age Yrs. |
|---|---|---|---|---|---|---|---|---|---|
| <3 MDs | 3 | MN | 20 | ||||||
| 3 to 8 MDs | 16 | PA | 1 | ||||||
| 9 to 15 MDs | 3 | One specialty | 13 | 194 | 17 | WA | 1 | 74 | 47 |
| Multispecialty | 11 | ||||||||
| >15 MDs | 2 | IL | 1 | range (28–68) | |||||
| WI | 1 |
Abbreviations: MD, medical doctor; IL, Illinois; MN, Minnesota; PA, Pennsylvania; WA, Washington; WI, Wisconsin.
Comparison of the before and after medical record documentation data is shown in Figure 3. Improvement occurred in all areas of medical record documentation that were assessed. For example, from the aggregate assessment, documentation of activity modification due to asthma increased by 100% from 29% to 58%, symptom frequency documentation increased by 30% from 62% to 81%, and nighttime symptom frequency documentation increased by 152% from 25% to 63%. Documentation of nonsymptom issues also increased by large relative percents; trigger information by 167% from 30% to 80%, adherence by 200% from 31% to 93%, and comments on response to therapy increased by 71% from 49% to 84%. Patient’s answers to one or more of the Asthma APGAR questions were specifically mentioned in an average of 81% (689 of 851) of the “after” medical records reviewed.
Figure 3.
Histogram for before and after documentation of asthma information in the medical records.
Other process measures also suggest increased compliance with asthma guidelines. The prescribing of a daily antiinflammatory medication increased by 204% from 24% before use of the Asthma APGAR tools to 73% after (p < 0.001). Documentation of nurse or physician observation of patient’s inhaler technique increased by 145% from 22% before to 54% after Asthma APGAR implementation (p = 0.001). The percent of patients who had a nonurgent asthma care visit in the six months prior to medical record abstraction increased by 425%, from 4% in the “before” to 21% after (p < 0.001). Medical record documentation of asthma education increased by 575% from 8% before to 54% after (p < 0.0001) introduction of the Asthma APGAR tools.
The seven health professional focus groups (one per site) were attended by a total of 72 staff members, including physicians (n = 38), nurses (n = 8), medical assistants (n = 20), receptionists (n = 4), and clinic administrators (n = 2). A total of 71 patients and parents attended the seven patient focus groups including eight child patient-parent pairs and two spouse-patient pairs.
During the focus groups health professional comments regarding the Asthma APGAR centered around 3 themes; ease of use, value of the information, and efficiency of asthma visits. Physicians that used the system (78% of all eligible) reported that when the patient completed the Asthma APGAR, it captured all of the preliminary data they needed for asthma assessment, and thereby streamlined the visit. The visit time could be used to ask more detailed questions, or provide education or develop solutions related to problems such as frequent symptoms, poor adherence, or newly identified triggers. Overall the health professionals felt that the Asthma APGAR tools saved time and improved the quality of the asthma visit. Physicians said that they usually scored the APGAR and usually followed the medication portion of the algorithm. The nurses used the portion of the algorithm related to adherence, especially the reminders about assessing inhaler technique, asking about asthma education needs, and making referrals to asthma education resources. Nursing staff often used the patient questionnaire sheet to facilitate recording asthma medications in the medical record by documenting what the patient was actually taking rather than what had been prescribed. Receptionists reported that they usually gave the patients the Asthma APGAR survey to complete and that patients who had received the questions during a previous visit sometimes ask for the “asthma” sheet when they came for their next asthma visit.
The physicians in the practices either initially liked and used the Asthma APGAR system regularly (78%, n = 56 [all within practices]) or refused to even consider using the system (22%, n = 16 [physicians]). Those physicians initially refusing to use the APGAR system did attend the last review of the progress before study completion and after hearing the responses of their physician colleagues to the benefit and limited time burden for use of the APGAR, 12 of the 16 said they would like to try using the Asthma APGAR. They were especially interested in its time-saving aspects.
Patient comments during the focus groups also centered on three domains; providing new information to their physician (specifically information about triggers, symptom frequency, and lack of adherence), improving self-efficacy (taking charge of asthma visit and self assessment), and receiving better care. The patients and parents reported that the Asthma APGAR patient questionnaire was easy to complete, requiring 5 minutes or less. None of the patient attendees had problems reading the Asthma APGAR questions and all agreed that the questions made sense. Several attendees noted that the Asthma APGAR questions covered topics they had not previously discussed with their physician or nurse, especially frequency of problems, adherence, and triggers. Patients reported that they did not mind completing the form at each asthma visit since asthma problems changed from visit to visit. Three attendees reported that they and their physicians had identified new asthma triggers after completing the Asthma APGAR. One attendee stated that completing the Asthma APGAR was the first time she had told her doctor she could not afford her medications and was not getting her prescriptions filled. She was able to apply for a medication support program at that visit. A mother said that the Asthma APGAR allowed her 8-year-old daughter to begin to take responsibility for her asthma when they took a copy home to use as part of her asthma action plan. Three adult attendees from different sites reported that they used the Asthma APGAR at home and felt they were now in control of their asthma.
Discussion
Use of the Asthma APGAR was associated with enhanced documentation in medical record notations for asthma visits and increased prescribing of daily controller medications, inhaler technique education and nonurgent asthma visits. In this “before” and “after” study design, it is not possible to demonstrate that the practice changes were due to use of the Asthma APGAR tools. However, the consistency in the direction and size of the practice change, the temporal relation to implementation of the Asthma APGAR tools and the much larger than expected change in asthma process measures suggests that at least part of the practice change is associated with the Asthma APGAR (Bateman et al 2001; Finkelstein et al 2002; Sin et al 2004; Mangione-Smith et al 2005; Wroth and Boals 2005).
Increasing medical records documentation is an important practice change. Without documentation of the asthma data assessed in this study, health professionals are unable to determine levels of asthma control or to select appropriate next steps in asthma management (Diette et al 2001; Fuhlbrigge 2004; Cabana et al 2005; Yawn et al 2005; Stoloff and Boushey 2006; EPR Update 2007; GINA Guidelines 2008). The Asthma APGAR also facilitated collection of information that could influence levels of control. The increase in the prescribing of daily controller medications suggests that documentation and use of the Asthma APGAR tools was associated with increased compliance with guideline recommended care. Other primary care investigators have also identified the importance of using the patient perspective in assessing asthma control (Horne et al 2007). In addition, focus group responses from both health professionals and patients reported Asthma APGAR provided more information then usually obtained during an asthma care visit.
Since the Asthma APGAR is intended as a practice change and guideline implementation tool, its value was assessed by usability, perceived value, and impact on the delivery of guideline compliant asthma care. This type of in-practice validation is most appropriate for implementation tools as opposed to assessment tools that require a different type of validation and different outcome measures. In-practice evaluation should be required of all practice implementation tools before they are recommended for widespread use in primary care.
By providing information on triggers and medication adherence, the Asthma APGAR can and did appear to facilitate exploration of factors known to affect control (Wark et al 2001; Weiss et al 2001; Mo et al 2003; EPR Update 2007). Adherence to medical therapy is a major problem in asthma (Fiese et al 2005; Bender 2006; Horne 2006; Marceau et al 2006). By asking patients to record exactly what they are currently using, physicians or nurses can focus on solutions rather than adherence assessment that may be perceived as confrontational or judgmental (Wark et al 2001; Yawn 2003; Horne 2006). In the focus group sessions patients reported that including a place to explain deviations from prescribed medication allowed them to be honest with the physician and nurse while focusing on problem solving rather than incriminations. Future studies need to assess whether documenting this information results in improving adherence rates.
Others have also suggested the importance of asking patients about their perception of response to current asthma therapy could facilitate discussion and education related to the important and specific role of each type of therapy (Horne et al 2007). Two of the focus group attendees stated that this question led to clarification of which medication was to be used for quick relief and which was the antiinflammatory medication for longer term control (Boushey et al 2005; EPR Update 2007). Both patients and staff reported that the Asthma APGAR questions helped the patient feel “more like a partner instead of a patient” for asthma management.
The Asthma APGAR care management flow sheet combines aspects from many different sections of the 2007 NHLBI asthma guidelines: assessment, monitoring, education, and treatment as well as medication step therapy (EPR Update 2007). The Asthma APGAR care algorithm recommends adherence assessment, trigger avoidance assessment, inhaler technique review, asthma education, and when needed, objective lung function testing in conjunction with the medication management.
Our results must be viewed in the context of the study’s limitations. No direct patient outcomes were collected and the sites that participated volunteered to do so. It is possible that other sites that were less interested would have less change in the process measures evaluated. Currently no studies report successful methods to work with practices that have no interest in care improvement. All of the physicians and most of the patients included in this study were Caucasian, so that it is not possible to know if the Asthma APGAR is useful in more racially diverse practices. The attendees at the focus groups may not be representative of all socioeconomic groups within practices although 25% of all attendees reported that they had some type of insurance that included government support. Future studies must assess the impact of the Asthma APGAR on longer term patient outcomes. It is these measures rather than comparison with expert opinion, lung function, or future health care utilization that will justify use of the Asthma APGAR tools in primary care practice. While we did include medical record confirmed episodes of asthma education, prescribing of controller medications to patients with persistent asthma and active review of inhaler technique, we did not include other measures of asthma care that are not discussed in the patient survey or in the care algorithm. We have only self-reports to confirm that 22 of the 24 practices continued to use all or part of the Asthma APGAR system 24 months after completion of the study.
Implementation of the Asthma APGAR tools was feasible in diverse types of primary care practices, was associated with changes in asthma care, and was reported to be acceptable and valuable by patients and health care professionals. In these practices, the Asthma APGAR tools became the basis of an asthma chronic care system motivated by a practice self-assessment and facilitated by use of tools developed in primary care to enhance asthma care content and activate patients.
Footnotes
Disclosure
This work was support by grants from the Agency for HealthCare Research and Quality (R03-HS014476) and The American Academy of Family Physicians Foundation. The authors report no conflicts of interest in this work.
References
- Bateman ED, Bousquet J, Braunstein GL. Is overall asthma control being achieved? A hypothesis-generating study. Eur Respir J. 2001;17:589–95. doi: 10.1183/09031936.01.17405890. [DOI] [PubMed] [Google Scholar]
- Bateman ED, Frith LF, Braunstein GL. Achieving guideline-based asthma control: does the patient benefit. Eur Respir J. 2002;20:588–95. doi: 10.1183/09031936.02.00294702. [DOI] [PubMed] [Google Scholar]
- Bender BG. Risk taking, depression, adherence, and symptom control in adolescents and young adults with asthma. Am J Respir Crit Care Med. 2006;173:953–7. doi: 10.1164/rccm.200511-1706PP. [DOI] [PubMed] [Google Scholar]
- Boushey HA, Sorkness CA, King TS, et al. Daily versus as-needed corticosteroids for mild persistent asthma. N Engl J Med. 2005;352:1519–28. doi: 10.1056/NEJMoa042552. [DOI] [PubMed] [Google Scholar]
- Cabana MD, Rand CS, Becher OJ, et al. Reasons for pediatrician nonadherence to asthma guidelines. Arch Pediatr Adolesc Med. 2000;155:1057–62. doi: 10.1001/archpedi.155.9.1057. [DOI] [PubMed] [Google Scholar]
- Cabana MD, Slish KK, Nan B, et al. Asking the correct questions to assess asthma symptoms. Clin Pediatr. 2005;44:319–25. doi: 10.1177/000992280504400406. [DOI] [PubMed] [Google Scholar]
- Canino G, Koinis-Mitchell D, Ortega AN, et al. Asthma disparities in the prevalence, morbidity, and treatment of Latino children. Soc Sci Med. 2006;63:2926–37. doi: 10.1016/j.socscimed.2006.07.017. [DOI] [PubMed] [Google Scholar]
- Crabtree BF, Miller W, editors. Doing Qualitative Research. New York, NY: Sage Publications, Inc; 1999. [Google Scholar]
- Diette GB, Skinner EA, Markson LE, et al. Consistency of care with national guidelines for children with asthma in managed care. J Pediatr. 2001;138:59–64. doi: 10.1067/mpd.2001.109600. [DOI] [PubMed] [Google Scholar]
- Diette GB, Patino CM, Merriman B, et al. Patient factors that physicians use to assign asthma treatment. Arch Intern Med. 2007;167:1360–6. doi: 10.1001/archinte.167.13.1360. [DOI] [PubMed] [Google Scholar]
- EPR-Update . Bethesda, MD: US Department of Health and Human Services: National Institutes of Health; National Heart, Lung, and Blood Institute: National Asthma Education and Prevention Program; 2007. Aug, 2007. Expert Panel Report 3 (EPR 3): Guidelines for the Diagnosis and Management of Asthma. NIH Prepublication copy No. 08-4051. [online]. Accessed on April 5, 2008. URL: http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.htm. [Google Scholar]
- Fiese BH, Wamboldt FS, Anbar RD. Family asthma management routines: connections to medical adherence and quality of life. J Pediatr. 2005;146:171–6. doi: 10.1016/j.jpeds.2004.08.083. [DOI] [PubMed] [Google Scholar]
- Finkelstein JA, Lozano P, Streiff KA, et al. Clinical effectiveness research in managed-care systems: lessons from the Pediatric Asthma Care PORT. Patient Outcomes Research Team. Health Serv Res. 2002;37:775–89. doi: 10.1111/1475-6773.00048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fuhlbrigge AL. Asthma severity and asthma control: symptoms, pulmonary function, and inflammatory markers. Curr Opin Pulm Med. 2004;10:1–6. doi: 10.1097/00063198-200401000-00002. [DOI] [PubMed] [Google Scholar]
- GINA Guidelines Welcome to the GINA Guidelines: the Global Initiative for Asthma. 2008. Guidelines and Resources [online]. Accessed on April 4, 2008. URL: http://www.ginasthma.com/GuidelinesResources.asp?l1=2&l2=0.
- Horne R. Compliance, adherence, and concordance: implications for asthma treatment. Chest. 2006;130(1 Suppl):65S–72S. doi: 10.1378/chest.130.1_suppl.65S. [DOI] [PubMed] [Google Scholar]
- Horne R, Price D, Cleland J, et al. Can asthma control be improved by understanding the patient’s perspective? BMC Pulm Med. 2007;7:8–12. doi: 10.1186/1471-2466-7-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Juniper EF, O’Byrne PM, Guyatt GH, et al. Development and validation of a questionnaire to measure asthma control. Eur Respir J. 1999;14:902–7. doi: 10.1034/j.1399-3003.1999.14d29.x. [DOI] [PubMed] [Google Scholar]
- Kelley CF, Mannino DM, Homa DM, et al. Asthma phenotypes, risk factors, and measures of severity in a national sample of US children. Pediatrics. 2005;115:726–31. doi: 10.1542/peds.2004-0529. [DOI] [PubMed] [Google Scholar]
- Lenoir M, Williamson A, Stanford RH, et al. Assessment of asthma control in a general population of asthmatics. Curr Med Res Opin. 2006;22:17–22. doi: 10.1185/030079905X74925. [DOI] [PubMed] [Google Scholar]
- Mangione-Smith R, Schonlau M, Chan KS, et al. Measuring the effectiveness of a collaborative for quality improvement in pediatric asthma care: does implementing the chronic care model improve processes and outcomes of care? Ambul Pediatr. 2005;5:75–82. doi: 10.1367/A04-106R.1. [DOI] [PubMed] [Google Scholar]
- Marceau C, Lemiere C, Berbiche D, et al. Persistence, adherence, and effectiveness of combination therapy among adult patients with asthma. J Allergy Clin Immunol. 2006;118:574–81. doi: 10.1016/j.jaci.2006.06.034. [DOI] [PubMed] [Google Scholar]
- Michele J, Amegavie L. Developing a paediatric asthma review pro forma. Nurs Stand. 2005;19:33–40. doi: 10.7748/ns2005.02.19.22.33.c3803. [DOI] [PubMed] [Google Scholar]
- Mo F, Robinson C, Choi BC, et al. Analysis of prevalence, triggers, risk factors and the related socio-economic effects of childhood asthma in the Student Lung Health Survey (SLHS) database, Canada 1996. Int J Adolesc Med Health. 2003;15:349–58. doi: 10.1515/ijamh.2003.15.4.349. [DOI] [PubMed] [Google Scholar]
- Nathan RA, Sorkness CA, Kosinski M, et al. Development of the asthma control test: a survey for assessing asthma control. J Allergy Clin Immunol. 2004;113:59–65. doi: 10.1016/j.jaci.2003.09.008. [DOI] [PubMed] [Google Scholar]
- Pinnock H, Juniper EF, Sheikh A. Concordance between supervised and postal administration of the Mini Asthma Quality of Life Questionnaire (MiniAQLQ) and Asthma Control Questionnaire (ACQ) was very high. J Clin Epidemiol. 2005;58:809–14. doi: 10.1016/j.jclinepi.2005.01.010. [DOI] [PubMed] [Google Scholar]
- QualityMetrics Inc Childhood Asthma Control Test for children with asthma 4 to 11 years old [online] 2005. Accessed on April 4, 2008. URL: http://www.asthmacontrol.com/AsthmaControlTestChild.html.
- Savage-Brown A, Mannino DM, Redd SC. Lung disease and asthma severity in adults with asthma: data from the Third National Health and Nutrition Examination. J Asthma. 2005;42:519–23. doi: 10.1081/JAS-67605. [DOI] [PubMed] [Google Scholar]
- Schatz M, Sorkness CA, Li JT, et al. Asthma Control Test: reliability, validity, and responsiveness in patients not previously followed by asthma specialists. J Allergy Clin Immunol. 2006;117:549–56. doi: 10.1016/j.jaci.2006.01.011. [DOI] [PubMed] [Google Scholar]
- Schatz M, Mosen D, Kosinski M, et al. Validity of the Asthma Control Test completed at home. Am J Manage Care. 2007;13:661–7. [PubMed] [Google Scholar]
- Sin DD, Bell NR, Man SF. Effects of increased primary care access on process of care and health outcomes among patients with asthma who frequent emergency departments. Am J Med. 2004;117:479–83. doi: 10.1016/j.amjmed.2004.04.011. [DOI] [PubMed] [Google Scholar]
- Skinner EA, Diette GB, Algatt-Bergstrom PJ, et al. The Asthma Therapy Assessment Questionnaire (ATAQ) for children and adolescents. Dis Manag. 2004;7:305–13. doi: 10.1089/dis.2004.7.305. [DOI] [PubMed] [Google Scholar]
- Solberg LI. Improving medical practice: a conceptual framework. Ann Fam Med. 2007;5:251–6. doi: 10.1370/afm.666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stoloff SW, Boushey HA. Severity, control, and responsiveness in asthma. J Allergy Clin Immunol. 2006;117:544–8. doi: 10.1016/j.jaci.2006.01.005. [DOI] [PubMed] [Google Scholar]
- Vollmer WM, Markson LE, O’Connor E, et al. Association of asthma control with health care utilization: a prospective evaluation. Am J Respir Crit Care Med. 2002;165:195–9. doi: 10.1164/ajrccm.165.2.2102127. [DOI] [PubMed] [Google Scholar]
- Vollmer WM. Assessment of asthma control and severity. Ann Allergy Asthma Immunol. 2004;93:409–13. doi: 10.1016/S1081-1206(10)61406-8. [DOI] [PubMed] [Google Scholar]
- Wark PA, Gibson PG, Johnston SL. Exacerbations of asthma: addressing the triggers and treatments. Monaldi Arch Chest Dis. 2001;56:429–35. [PubMed] [Google Scholar]
- Weiss ST, Horner A, Shapiro G, et al. The prevalence of environmental exposure to perceived asthma triggers in children with mild-to-moderate asthma: data from the Childhood Asthma Management Program (CAMP) J Allergy Clin Immunol. 2001;107:634–40. doi: 10.1067/mai.2001.113869. [DOI] [PubMed] [Google Scholar]
- Westfall JM, Mold J, Fagnan L. Practice-based research – “Blue Highways” on the NIH roadmap. JAMA. 2007;297:403–6. doi: 10.1001/jama.297.4.403. [DOI] [PubMed] [Google Scholar]
- Wroth TH, Boals JC. Application of quality-improvement methods in a community practice: the Sandhills Pediatrics Asthma Initiative. N C Med J. 2005;66:218–20. [PubMed] [Google Scholar]
- Yawn BP. The impact of childhood asthma on daily life of the family. Prim Care Respir J. 2003;12:82–5. doi: 10.1038/pcrj.2003.52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yawn BP. Participatory research in rural primary care. MN Med. 2004;87:52–4. [PubMed] [Google Scholar]
- Yawn BP, Yawn RA. Measuring asthma quality in primary care: Can we develop better measures? Respir Med. 2005;100:26–33. doi: 10.1016/j.rmed.2005.04.010. [DOI] [PubMed] [Google Scholar]
- Yawn BP, van der Molen T, Humbert M. Asthma management: are GINA guidelines appropriate for daily clinical practice? Prim Care Respir J. 2005;14:294–302. doi: 10.1016/j.pcrj.2005.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yawn BP, Brenneman SK, Allen-Ramey FC, et al. Assessment of asthma severity and asthma control in children. Pediatrics. 2006;118:322–9. doi: 10.1542/peds.2005-2576. [DOI] [PubMed] [Google Scholar]
- Yawn B, Wollan P, Bertram S, et al. Asthma treatment in a population based cohort: Putting step-up and step-down in context. Mayo Clin Proc. 2007;82:414–21. doi: 10.4065/82.4.414. [DOI] [PubMed] [Google Scholar]