Hypoglycemia, a frequent occurrence during modern intensive insulin therapy, remains the major limiting factor in achieving optimal glucose control in type 1 diabetic patients as well as in patients with long-standing type 2 diabetes. This has been a challenge for clinicians and investigators since several large population-based studies such as the Diabetes Control and Complications Trial and UK Prospective Diabetes Study established the long-term benefits of tight glycemic control many years ago (1,2). More recently, studies of intensive glucose control in patients with diabetes of several years duration have—to the surprise to many—been either terminated because of increased mortality in the intensive control arm or because worse outcomes were revealed in regard to the clinical end points (3,4). In a parallel development, we have gone, over the course of 10 years, from embracing stringent inpatient glucose control via insulin infusion protocols in the intensive care setting (5) to realizing that not everybody may benefit equally from such an intervention, since the increased incidence of profound hypoglycemia is the limiting factor (6). In fact, a recent systematic review of 21 trials of intensive insulin therapy by Kansagara et al. (7) found a sixfold higher risk of severe hypoglycemic events in patients undergoing such therapy. Faced with a clinical dilemma of such proportion, it appears that we may need to readdress our hypotheses, and we need to conduct mechanistic studies that allow us to identify therapies that are effective but minimize the exposure of patients to the heightened risk of hypoglycemia. Understanding the regulation of glucose metabolism in the brain and how it responds to hypoglycemia in this context is of particular relevance because of the brain’s exquisite dependence on glucose as an energy substrate and its integrative function in whole body fuel homeostasis (8).
The brain poses particular challenges because, due to limited glucose transport activity in the blood brain barrier and high rates of cellular glucose metabolism, the concentrations of glucose in human brain interstitial fluid are only about a fifth of those in plasma, making the brain highly vulnerable to a drop in glucose supply (9). Magnetic resonance spectroscopy (MRS), which allows monitoring of glucose and other substrate metabolism in vivo offers the unique opportunity to study glucose metabolism behind the blood brain barrier in real time. Using the stable 13C isotope as a tracer, labeled glucose or other substrates are infused and label appearance in the metabolite pools of glutamate and glutamine can be observed over time. Fitting of these data with a mathematical model of metabolism allows calculation of substrate-specific metabolism as well as compartmentation of metabolism between the two major brain cell types, neurons and glia (Fig. 1).
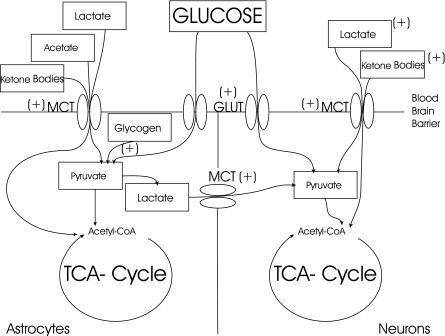
FIG. 1.
Two-compartment model of brain metabolic fluxes along with pathways that have been proposed to be upregulated in intensively treated type 1 diabetes. Both astrocytes and neurons are dependent on glucose as a metabolic substrate, but neurons to a higher degree than astrocytes—particularly under hypoglycemia. Storage of glycogen allows astrocytes to provide neurons with an energy reserve that can be quickly mobilized and transferred during times of intense activity as well as during hypoglycemia; whether its levels are increased in type 1 diabetes still remains unclear (17). Monocarboxylic acid transporters (MCTs) along the blood brain barrier allow uptake of acetate, lactate, and ketone bodies and may be upregulated in type 1 diabetes (18,24) allowing increased alternate fuel consumption during hypoglycemia (indicated by +). Glucose transporters (GLUT) may be upregulated in a similar fashion in type 1 diabetes (20).
To test whether moderate hypoglycemia can reduce human brain energy production, van de Ven et al. (10) used 13C MRS to study glucose metabolism in healthy control subjects during euglycemia and hypoglycemia using a hyperinsulinemic clamp to maintain stable glycemia. Eight subjects served as their own controls and were studied at a glucose level of 5 mM and at 3 mM, thereby reducing the confounding influence of interindividual variability. Interestingly, the authors were not able to detect a difference between tricarboxylic acid (TCA) cycle activity under euglycemic and hypoglycemic conditions. They suggest that oxidative brain metabolism was not impaired in a way that would have resulted in decreased production of ATP further downstream, in seeming contradiction with results showing impaired cortical function in control subjects at similar levels of hypoglycemia (11,12).
There are several potential explanations for the paradoxical results of van de Ven et al. (10), including the brain region observed and a switch of cerebral metabolism to alternate substrates. An important point to keep in mind is that most current MRS studies are focused on the brain tissue most adjacent to the nuclear magnetic resonance (NMR) coil, the occipital cortex. Because we know from animal studies and human positron emission tomography studies (13) that metabolic activity can vary substantially from region to region and change when local activity is stimulated (14), we must ask ourselves how the current observations can be applied from the occipital cortex to other areas of the brain. Several human studies using functional magnetic resonance imaging, which uses blood oxygen tension differences as a surrogate of regional activation, support the notion that changes in the activation patterns of the brain under acute hypoglycemia do occur (15,16). It is therefore likely that with the advent of more localized NMR spectroscopy we will be able to further delineate regional differences of metabolism.
We must also take into consideration that energy substrates other than glucose may increase their contribution to TCA cycle activity, which in the brain is composed of separate and cooperative glial and neuronal compartments. For a schematic representation of these changes, see Fig. 1. Astrocytes (a form of glial cell predominant in the cerebral cortex) have emerged as playing a potentially important role by temporarily supplying neurons with fuel derived from stored glycogen, which could provide extra substrate during a hypoglycemic period (17). A reduction of astrocytic glucose metabolism to spare glucose for the neuron is also possible, and changes in the balance between neuronal and astrocyte glucose oxidation in animal models during hypoglycemia have been reported by our group (18). An alternative possibility is that there was an increase in the metabolism of lactate derived from the circulation, which increased by 50% under hypoglycemia. It has been reported that an infusion of lactate given to subjects during a comparable clamp study was able to alleviate cognitive dysfunction (19). We note that based on MRS measurements of glucose transport activity (20,21), the reduction in net glucose transport at 3 mmol/L plasma glucose levels would reduce glucose uptake on the order of 5–10%. Although van de Ven et al. indirectly calculate an up to 5% contribution of lactate, direct measurement of lactate metabolism by 13C MRS (22) as well as arteriovenous difference methods (23) suggest that at the lactate levels achieved in the hypoglycemia portion of the study by van de Ven et al. the contribution of lactate oxidation is most likely greater and can support close to 10% of neuronal metabolic needs.
A more comprehensive understanding of the adaptations of brain fuel metabolism to acute and recurrent hypoglycemia will likely serve as the foundation for the development of more specific therapeutic interventions that avert the negative impact of neuroglycopenia in patients receiving insulin therapy.
ACKNOWLEDGMENTS
No potential conflicts of interest relevant to this article were reported.
Footnotes
See accompanying original article, published in Diabetes 2011;60:1467–1473.
REFERENCES
- 1.The Diabetes Control and Complications Trial Research Group The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993;329:977–986 [DOI] [PubMed] [Google Scholar]
- 2.UK Prospective Diabetes Study (UKPDS) Group Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet 1998;352:837–853 [PubMed] [Google Scholar]
- 3.Gerstein HC, Miller ME, Genuth S, et al. ; ACCORD Study Group Long-term effects of intensive glucose lowering on cardiovascular outcomes. N Engl J Med 2011;364:818–828 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Yakubovich N, Gerstein HC. Serious cardiovascular outcomes in diabetes: the role of hypoglycemia. Circulation 2011;123:342–348 [DOI] [PubMed] [Google Scholar]
- 5.van den Berghe G, Wouters P, Weekers F, et al. Intensive insulin therapy in the critically ill patients. N Engl J Med 2001;345:1359–1367 [DOI] [PubMed] [Google Scholar]
- 6.Finfer S, Chittock DR, Su SY, et al. ; NICE-SUGAR Study Investigators Intensive versus conventional glucose control in critically ill patients. N Engl J Med 2009;360:1283–1297 [DOI] [PubMed] [Google Scholar]
- 7.Kansagara D, Fu R, Freeman M, Wolf F, Helfand M. Intensive insulin therapy in hospitalized patients: a systematic review. Ann Intern Med 2011;154:268–282 [DOI] [PubMed] [Google Scholar]
- 8.Cryer PE. Hypoglycemia in type 1 diabetes mellitus. Endocrinol Metab Clin North Am 2010;39:641–654 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Abi-Saab WM, Maggs DG, Jones T, et al. Striking differences in glucose and lactate levels between brain extracellular fluid and plasma in conscious human subjects: effects of hyperglycemia and hypoglycemia. J Cereb Blood Flow Metab 2002;22:271–279 [DOI] [PubMed] [Google Scholar]
- 10.van de Ven KCC, de Galan BE, van der Graaf M, et al. Effect of acute hypoglycemia on human cerebral glucose metabolism measured by 13C magnetic resonance spectroscopy. Diabetes 2011;60:1467–1473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sommerfield AJ, Deary IJ, McAulay V, Frier BM. Moderate hypoglycemia impairs multiple memory functions in healthy adults. Neuropsychology 2003;17:125–132 [PubMed] [Google Scholar]
- 12.Kodl CT, Seaquist ER. Cognitive dysfunction and diabetes mellitus. Endocr Rev 2008;29:494–511 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Cranston I, Reed LJ, Marsden PK, Amiel SA. Changes in regional brain (18)F-fluorodeoxyglucose uptake at hypoglycemia in type 1 diabetic men associated with hypoglycemia unawareness and counter-regulatory failure. Diabetes 2001;50:2329–2336 [DOI] [PubMed] [Google Scholar]
- 14.Wang J, Jiang L, Jiang Y, Ma X, Chowdhury GM, Mason GF. Regional metabolite levels and turnover in the awake rat brain under the influence of nicotine. J Neurochem 2010;113:1447–1458 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Anderson AW, Heptulla RA, Driesen N, et al. Effects of hypoglycemia on human brain activation measured with fMRI. Magn Reson Imaging 2006;24:693–697 [DOI] [PubMed] [Google Scholar]
- 16.Driesen NR, Goldberg PA, Anderson AW, et al. Hypoglycemia reduces the blood-oxygenation level dependent signal in primary auditory and visual cortex: a functional magnetic resonance imaging study. J Neurosci Res 2007;85:575–582 [DOI] [PubMed] [Google Scholar]
- 17.Herzog RI, Chan O, Yu S, Dziura J, McNay EC, Sherwin RS. Effect of acute and recurrent hypoglycemia on changes in brain glycogen concentration. Endocrinology 2008;149:1449–1504 [DOI] [PMC free article] [PubMed]
- 18.Jiang L, Herzog RI, Mason GF, et al. Recurrent antecedent hypoglycemia alters neuronal oxidative metabolism in vivo. Diabetes 2009;58:1266–1274 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Maran A, Cranston I, Lomas J, Macdonald I, Amiel SA. Protection by lactate of cerebral function during hypoglycaemia. Lancet 1994;343:16–20 [DOI] [PubMed] [Google Scholar]
- 20.Gruetter R, Novotny EJ, Boulware SD, et al. Direct measurement of brain glucose concentrations in humans by 13C NMR spectroscopy. Proc Natl Acad Sci USA 1992;89:1109–1112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.de Graaf RA, Mason GF, Patel AB, Rothman DL, Behar KL. Regional glucose metabolism and glutamatergic neurotransmission in rat brain in vivo. Proc Natl Acad Sci USA 2004;101:12700–12705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Boumezbeur F, Petersen KF, Cline GW, et al. The contribution of blood lactate to brain energy metabolism in humans measured by dynamic 13C nuclear magnetic resonance spectroscopy. J Neurosci 2010;30:13983–13991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.van Hall G, Strømstad M, Rasmussen P, et al. Blood lactate is an important energy source for the human brain. J Cereb Blood Flow Metab 2009;29:1121–1129 [DOI] [PubMed] [Google Scholar]
- 24.Mason GF, Petersen KF, Lebon V, Rothman DL, Shulman GI. Increased brain monocarboxylic acid transport and utilization in type 1 diabetes. Diabetes 2006;55:929–934 [DOI] [PMC free article] [PubMed] [Google Scholar]