Abstract
Objective
To study whether traditionally vulnerable populations have worse geographic access to trauma centers.
Design
A cross-sectional analysis using data from the American Hospital Association Annual Survey from 2005 linked with zip code–level data from the US Census. We used a multinomial logit model to examine the odds of having difficult as opposed to easy access to trauma centers for a given subgroup of vulnerable populations.
Setting and Participants
Population in rural and urban communities as defined by zip codes in the United States.
Main Outcome Measures
Each community’s distance to the nearest trauma center (levels I–III).
Results
In urban areas, 67% of the population had easy access to trauma centers and 12% had difficult access compared with 24% and 31% in rural areas, respectively. Areas with higher shares of the following vulnerable population groups had higher risks (odds ratios) of facing difficult access to trauma center services in 2005: foreign born in urban areas (1.65 for a medium share and 2.18 for a high share [both P < .01]); African American in urban and rural areas (1.25 for a medium share and 1.35 for a high share, respectively [both P < .05]); and near-poor in urban and rural areas (1.52 [P < .05] and 1.69 [P < .01] for a high share, respectively).
Conclusions
A significant segment of the US population (representing 38.4 million people) does not have access to trauma care within 1 hour of driving time. Moreover, certain vulnerable groups are at higher risk than others for worse access to trauma centers. Stakeholders and health care planners should consider these factors in the development of trauma systems because a mismatch of potential need and access could signal inefficiencies in the delivery of care.
Trauma centers are a key component of the infrastructure of the US health care system because they have been shown to decrease morbidity and mortality for injured patients of all age ranges, from children to the elderly.1–3 However, as highlighted in the media and in scholarly literature, trauma centers are more likely to be safety-net hospitals, are often underfunded, and are more likely to be poorly or not reimbursed for their provision of lifesaving but expensive care.4–6 These financial hardships are cited as contributing to the increasing closures of trauma centers in the United States and are part of the growing national crisis in access to emergency care.6–9
Associated with the increasing closures of trauma centers is the growing concern regarding disparity in trauma access. Several studies have highlighted that access to trauma centers is not even for all populations, especially rural and urban groups.10 Another important aspect of access that has been less studied but suggested as a possible area for intervention is that of socioeconomic disparities in system-level access to care, specifically, race/ethnicity, income, and age.11,12
There are no studies, to our knowledge, that describe system-level disparities in geographic access to trauma care that may be experienced by vulnerable populations. Most of the literature focuses on the reimbursement mechanisms that support the high costs of trauma care,8,13,14 effectiveness of trauma centers,3,15,16 and regionalization, 17 without attention to populations that may be at higher risk of being further away from trauma centers.
Knowledge of these patterns is crucial to the future of providing equitable access to care and the development and management of trauma centers. Certain disadvantaged groups have been shown to be at higher risk for injury,18 and, at the same time, certain racial/ethnic groups have been shown to have poorer outcomes.19 A critical knowledge gap exists as to whether these poorer outcomes are due to individual treatment biases by physicians or other individual-level factors as opposed to system-level factors, such as access to care. Because timely access to care is closely linked to the benefits provided by trauma centers, it is crucial to know whether vulnerable populations have decreased availability of these services on a population level.
From the patient’s perspective, there are various types of access barriers to trauma care that may be faced, such as geographical, financial, or cultural barriers. Our study analyzed whether there are disparities in access by examining geographic proximity of trauma care in 2005, with a particular focus on vulnerable population groups (racial/ethnic minority, foreign born, elderly, and economically disadvantaged). Results from our study provide a new cross-sectional view of access to trauma care on a systems level.
METHODS
DATA SOURCES
We used the 2000 US census results20 (the most recently available) to obtain data on communities at the zip code level. We linked the census data with longitude and latitude coordinates of each zip code’s population center using Mailer software. 21 For trauma center availability, we used service data from the 2005 American Hospital Association annual survey. This survey included all general, acute, short-stay hospitals and indicated whether a trauma center was available. We chose to look at only trauma center levels I through III (level I being the most comprehensive) based on previous literature.22 The survey also included hospital characteristics, such as the size, ownership, and teaching status of the hospital, and allowed us to construct hospital market characteristics. Finally, we obtained the longitude and latitude coordinates of the trauma center’s location (identified from the heliport, if one exists, or from the zip code) to calculate the distance between each community and its nearest trauma center.23
VARIABLES AND METHODS OF MEASUREMENT
Outcome Measures
Our outcome measure in this study was each zip code community’s distance to its nearest trauma center in 2005. We calculated spherical distance using longitude and latitude information between each zip code’s population center and the hospital’s location according to information included in the survey database. The distance calculation based on longitude and latitude coordinates has been shown to be highly correlated with actual driving distance, especially for urban areas.24,25
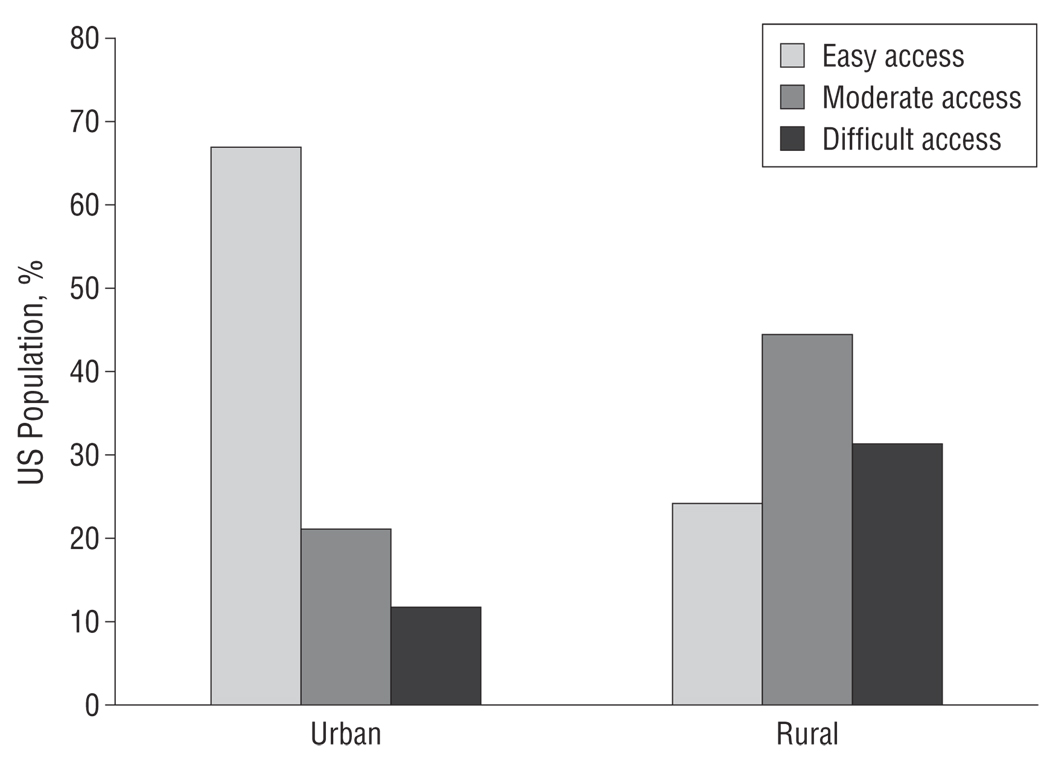
We distributed distance into the following 3 discrete categories of access: those with access to trauma centers less than 10 miles (16 km) away (reference group); those with access within 10 to 30 miles (16 to 48 km); and those with access greater than 30 miles (48 km) away. For ease of comprehension, we converted these distances into driving times using a validated method by Phibbs and Luft25 by which these distances correlated with estimated travel times of less than 20 minutes, 20 to 60 minutes, and greater than 60 minutes, respectively. We categorized these thresholds into easy, moderate, and difficult access on the basis of previous literature,10 in which prehospital times of greater than 60 minutes (known as the golden hour of trauma)26 have been associated with a significant increase in the risk of death. The Figure shows the distribution of the 2005 access categories.
Figure.
Population access to trauma services in 2005. Access groups are described in the “Variables and Methods of Measurement” subsection of the “Methods” section.
Vulnerable Populations
Because our focus in this report consisted of traditionally disadvantaged populations, the key predictor variables we chose were based on previous literature as follows: race/ethnicity, foreign born, economically disadvantaged, and the elderly. We divided the communities into 3 categories according to distributions of a given subpopulation. For example, a zip code was classified as having a high share of African American population if the percentage was at the upper one-third of the entire African American population distribution, a medium share if its percentage of African American population fell in the middle one-third of the distribution, and a low share if the percentage fell in the lower one-third. The categorical variables allow for easier presentation of the multinomial logit results when we discuss odds ratios (ORs). We classified the 3 share groups of each underserved population separately for urban and rural areas. The set of vulnerable population categories are as follows:
Race/ethnicity. Based on standard US Census Bureau measures, we analyzed African American, white Hispanic (or Latino), and other nonwhite (American Indian or Alaskan Native, Asian, Native Hawaiian or other Pacific Islander, and other race, all self-classified according to categories defined by the US Census Bureau20) populations. We defined the reference group as the standard non-Hispanic (or non-Latino) white population.
Foreign born. Because foreign-born populations have been shown to have poorer health and more limited access to health care,27–29 we included the share of foreign-born population to capture this potentially vulnerable population.
Economically disadvantaged. We defined the economically disadvantaged population by the traditional measure of poverty and by unemployment. Similar to previous research on access and use, we categorized income in the following 3 ways: the poor (< 100% of the federal poverty line), the near-poor (100%–200% of the federal poverty line), and the nonpoor (the reference group, >200% of the federal poverty line).30,31 We also used the census measurements of the percentage of unemployed, divided into 3 quantiles, as a separate category.32,33
Elderly. We considered elderly populations as defined by the US Census Bureau to be individuals older than 65 years.
CONTROL VARIABLES
To take into account other confounders, we controlled for zip code–level population characteristics, in particular, population size and wealth, by including total population and per capita income. To control for hospital market characteristics that could be related to trauma center availability, we followed previous literature and defined hospital market as a 15-mile (24-km) radius. 25,34 We included the percentage of beds within the same hospital market with different ownership (for-profit and government, omitting not-for-profit) and that belong to teaching hospitals.
STATISTICAL METHODS
Our unit of analysis was the community, as defined by zip codes in 2005, and all analyses were performed separately for urban and rural areas. We first conducted descriptive analyses comparing population characteristics between communities with easy and difficult access to trauma centers. We omitted the comparison between easy and moderate access to enhance the clarity of our presentation, but results are available from the authors on request. We then used a multinomial logit model to examine the odds of having difficult or moderate access to trauma centers as opposed to having easy access for a given subgroup of vulnerable population. The dependent variable in the multinomial logit model consisted of the 3 aforementioned discrete categories of access (distances of <10 miles [<16 km], 10–30 miles [16–48 km], and >30 miles [>48 km]). Urban and rural areas were defined by whether the zip code was in a metropolitan statistical area. All models were estimated using commercially available software (Stata, version 10.0; StataCorp, College Station, Texas). This study was approved by the Committee on Human Research at the University of California, San Francisco.
RESULTS
CHARACTERISTICS OF URBAN AND RURAL AREAS BY ACCESS TO TRAUMA CENTERS
As shown in the Figure, 67% of the urban population had easy access to trauma centers, whereas only 24% of the rural population lived within 10 miles (a 20-minute drive) of a trauma center. On the other hand, 12% of urban communities lived more than 30 miles away (>60-minute drive) from the nearest trauma center (representing 25 million people), whereas close to one-third of the rural population (13 million people [31%]) had difficult access to trauma centers.
We included 24 447 zip codes in our sample. More than half (56%) were urban (n=13 578) and 44% were rural (n=10 869). In terms of population size, our analysis covered more than an estimated 265 million residents in the United States, with the distribution heavily weighted toward urban residents (221 million) compared with rural residents (44 million). Table 1 shows the descriptive statistics of population and health care market characteristics in the urban and rural areas. Looking at the whole sample (the first and third columns of Table 1), there were lower proportions of all minority (African American, Hispanic, and other nonwhite) and foreign-born populations in rural areas compared with urban areas, as expected. Not surprisingly, health care resources were much more meager in rural areas compared with urban areas, as evidenced by fewer hospitals and a lower percentage of beds belonging to teaching hospitals.
Table 1.
Descriptive Statistics of Population and Health Care Market Characteristics by Trauma Services Access Categoriesa
| Urban Communities | Rural Communities | |||||
|---|---|---|---|---|---|---|
| Access in 2005 | Access in 2005 | |||||
| Whole Sample |
Easy Access |
Difficult Access |
Whole Sample |
Easy Access |
Difficult Access |
|
| Zip code population characteristics from 2000 census | ||||||
| Total population | 31 941 (18 914) | 34 168 (18 800) | 31 834 (19 169)b | 14 719 (12 265) | 18 603 (12 127) | 14 700 (12 463)b |
| Per capita income, $ | 22 814 (9766) | 23 018 (10 496) | 22 157 (9294)b | 17 067 (3746) | 17 430 (4016) | 16 964 (3977)b |
| African American population | 0.13 (0.20) | 0.15 (0.22) | 0.11 (0.17)b | 0.09 (0.15) | 0.09 (0.15) | 0.09 (0.16) |
| Hispanic population | 0.14 (0.20) | 0.15 (0.21) | 0.18 (0.22)b | 0.05 (0.12) | 0.08 (0.15) | 0.05 (0.11)b |
| Other nonwhite population (including Asian) | 0.14 (0.15) | 0.15 (0.15) | 0.17 (0.17)b | 0.06 (0.10) | 0.07 (0.10) | 0.07 (0.11) |
| Elderly population (age >65 y) | 0.07 (0.03) | 0.06 (0.03) | 0.07 (0.04)b | 0.08 (0.03) | 0.08 (0.02) | 0.09 (0.03)b |
| Foreign-born population | 0.13 (0.13) | 0.15 (0.14) | 0.16 (0.16)b | 0.03 (0.05) | 0.04 (0.06) | 0.03 (0.05)b |
| Unemployed | 0.03 (0.02) | 0.03 (0.02) | 0.03 (0.02) | 0.03 (0.01) | 0.03 (0.01) | 0.03 (0.01)b |
| Family below FPL | 0.12 (0.09) | 0.12 (0.09) | 0.12 (0.08) | 0.14 (0.07) | 0.14 (0.07) | 0.14 (0.06) |
| Near poor (100%–200% of FPL) | 0.16 (0.07) | 0.16 (0.08) | 0.17 (0.07)b | 0.21 (0.05) | 0.20 (0.05) | 0.21 (0.05)b |
| County-level health care market characteristics in 2000 | ||||||
| Total No. of physicians per 1000 people | 2.88 (1.77) | 3.17 (1.80) | 2.47 (1.70) | 1.26 (0.99) | 1.53 (1.35) | 1.21 (0.79) |
| Total No. of general physicians per 1000 people | 0.23 (0.09) | 0.22 (0.09) | 0.23 (0.08) | 0.28 (0.15) | 0.29 (0.14) | 0.28 (0.15) |
| ≥1 FQHC present in the county | 0.70 (0.46) | 0.75 (0.44) | 0.73 (0.44) | 0.29 (0.46) | 0.30 (0.46) | 0.35 (0.48) |
| 15-Mile radius hospital market characteristics in 2005, No. | ||||||
| Hospitals | ||||||
| All | 11.50 (13.92) | 13.65 (14.95) | 12.31 (14.27)b | 1.48 (0.78) | 1.51 (0.88) | 1.37 (0.69)b |
| For profit | 2.31 (3.99) | 2.48 (3.97) | 4.02 (5.92) | 0.23 (0.48) | 0.20 (0.43) | 0.28 (0.52) |
| Government | 1.11 (1.83) | 1.30 (2.00) | 1.21 (1.74)c | 0.38 (0.58) | 0.42 (0.61) | 0.34 (0.55) |
| Not for profit | 8.08 (11.08) | 9.87 (12.23) | 7.08 (9.57) | 0.87 (0.85) | 0.90 (0.93) | 0.75 (0.73) |
| Teaching | 2.50 (5.23) | 3.25 (5.92) | 1.71 (3.93) | 0.01 (0.14) | 0.03 (0.21) | 0.00 (0.05) |
| Trauma centers | 3.55 (4.07) | 4.57 (4.26) | 2.14 (3.62) | 0.45 (0.61) | 1.15 (0.43) | 0.00 (0.01) |
| Beds, % | ||||||
| In for-profit hospitals | 0.16 (0.23) | 0.15 (0.20) | 0.24 (0.27)b | 0.15 (0.32) | 0.11 (0.28) | 0.19 (0.37)b |
| In government hospitals | 0.12 (0.20) | 0.11 (0.16) | 0.15 (0.25)b | 0.28 (0.42) | 0.30 (0.44) | 0.26 (0.42)b |
| In teaching hospitals | 0.22 (0.25) | 0.27 (0.25) | 0.12 (0.19)b | 0.01 (0.08) | 0.01 (0.10) | 0.00 (0.02)b |
| No. of zip codes | 13 578 | 7156 | 1685 | 10 869 | 1906 | 3350 |
| Population size | 221 467 156 | 151 768 389 | 25 217 669 | 44 174 337 | 12 417 135 | 13 248 769 |
Abbreviations: FQHC, federally qualified health center; FPL, federal poverty line.
SI conversion factor: To convert miles to kilometers, multiply by 1.6.
Unless otherwise indicated, data are expressed as mean (SD).
P<.01.
P<.05.
For urban areas (Table 1), communities with difficult access were slightly less populated compared with those with easy access, with slightly higher proportions of Hispanic, nonwhite, and foreign-born populations and lower proportions of African American population (P < .01 for all). Areas with difficult access had fewer hospitals (12.31 vs 13.65 in easy access areas [P < .01]) within the 15-mile hospital market radius. In addition, areas with difficult access to trauma centers had a higher share of for-profit hospital beds (0.24 vs 0.15 in easy access areas [P < .01]).
For rural areas (Table 1), there were few large differences between the communities with difficult access vs easy access except for a smaller proportion of Hispanics in communities with difficult access (5% vs 8% of Hispanics in easy access areas [P < .01]). As in urban areas, rural communities with difficult access also had fewer overall health care resources available.
RISK FACTORS FOR DIFFICULT ACCESS TO THE NEAREST TRAUMA CENTER
We report the results from the multinomial logit regressions in Table 2. For clarity of presentation, we report only the ORs of communities with difficult access relative to those with easy access and omit the results comparing those with moderate and easy access (the moderate access group was included in the model, and the results are available from the authors on request). When we compared communities with a low and a medium share of African American population, for example, the OR of 1.25 (P < .05) was the odds of a community with a medium share of African American population having difficult access as opposed to easy access to trauma centers relative to the same odds for a community with a low share of African American population (the reference group).
Table 2.
Multinomial Logit Regression Results on Static Access to Trauma Services in 2005a
| Difficult Access, RR (95% CI) | ||
|---|---|---|
| Urban Communities | Rural Communities | |
| Vulnerable population | ||
| African American | ||
| Low share | 1.00 [Reference] | 1.00 [Reference] |
| Medium share (middle 1/3) | 1.25 (1.02–1.52)b | 1.04 (0.81–1.34) |
| High share (upper 1/3) | 1.18 (0.95–1.47) | 1.35 (1.02–1.80)b |
| Hispanic | ||
| Low share | 1.00 [Reference] | 1.00 [Reference] |
| Medium share | 0.87 (0.67–1.13) | 1.09 (0.83–1.44) |
| High share | 1.17 (0.82–1.68) | 1.22 (0.82–1.81) |
| Other nonwhite | ||
| Low share | 1.00 [Reference] | 1.00 [Reference] |
| Medium share | 0.46 (0.35–0.60)c | 1.12 (0.86–1.47) |
| High share | 0.38 (0.26–0.55)c | 0.86 (0.61–1.21) |
| Elderly | ||
| Low share | 1.00 [Reference] | 1.00 [Reference] |
| Medium share | 0.72 (0.58–0.89)c | 1.05 (0.80–1.38) |
| High share | 0.84 (0.69–1.03) | 1.17 (0.90–1.52) |
| Foreign-born | ||
| Low share | 1.00 [Reference] | 1.00 [Reference] |
| Medium share | 1.65 (1.29–2.12)c | 0.76 (0.58–1.01)d |
| High share | 2.18 (1.55–3.05)c | 0.88 (0.61–1.27) |
| Unemployed | ||
| Low share | 1.00 [Reference] | 1.00 [Reference] |
| Medium share | 1.01 (0.80–1.37) | 0.73 (0.57–0.94)b |
| High share | 1.05 (0.80–1.37) | 1.01 (0.77–1.34) |
| Below FPL | ||
| Low share | 1.00 [Reference] | 1.00 [Reference] |
| Medium share | 1.07 (0.82–1.39) | 0.82 (0.61–1.09) |
| High share | 0.90 (0.62–1.31) | 0.71 (0.49–1.03)d |
| Near-poor (100%–200% FPL) | ||
| Low share | 1.00 [Reference] | 1.00 [Reference] |
| Medium share | 1.25 (0.95–1.65) | 1.29 (0.96–1.73)d |
| High share | 1.52 (1.04–2.23)b | 1.69 (1.19–2.38)c |
| Other zip code–level population characteristics | ||
| Log (population) | 0.78 (0.71–0.87)c | 0.73 (0.65–0.82)c |
| Log (per capita income) | 1.34 (0.94–1.92) | 1.00 (0.50–2.03) |
| 15-Mile radius hospital market characteristics | ||
| Beds that belong to FP hospitals, % | ||
| Low share | 1.00 [Reference] | 1.00 [Reference] |
| Medium share | 0.94 (0.74–1.19) | |
| High share | 1.30 (1.09–1.56)c | 1.47 (1.11–1.94)c |
| Beds that belong to GOV hospitals, % | ||
| Low share | 1.00 [Reference] | 1.00 [Reference] |
| Medium share | 1.32 (0.98–1.77)d | 0.51 (0.15–1.70) |
| High share | 1.06 (0.90–1.26) | 0.76 (0.61–0.96)b |
| Beds that belong to teaching hospitals, % | ||
| Low share | 1.00 [Reference] | 1.00 [Reference] |
| Medium share | 0.54 (0.45–0.66)d | |
| High share | 0.16 (0.12–0.20)d | 0.09 (0.02–0.33)c |
Abbreviations: CI, confidence interval; FQHC, federally qualified health center; FP, for-profit; FPL, federal poverty line; GOV, government; RR, relative risk.
SI conversion factor: To convert miles to kilometers, multiply by 1.6.
Comparisons were to groups with easy access (reference group). Numbers of observations (zip codes) in the analysis were 13 564 for urban communities and 10758 for rural communities. To convert miles to kilometers, multiply by 1.6.
P<.05.
P<.01.
P<.10.
As Table 2 shows, communities with medium and high shares of foreign-born population also appeared to have a higher odds of more difficult access relative to communities with low shares of foreign-born population (OR, 1.65 for medium share and 2.18 for high share [both P < .01]). Finally, areas with high shares of near-poor families had 1.52-higher odds (P < .05) of having difficult access compared with areas with low shares of nearpoor families.
Similar to urban areas, rural communities with higher shares of African American population had a higher odds (OR, 1.35 [P < .05]) of having difficult access as opposed to easy access compared with communities with a low share of African American population. Likewise, communities with medium and high shares of near-poor families had higher odds of having difficult access compared with areas with low shares of near-poor families (OR, 1.29 for a medium share [P < .10] and 1.69 for a high share [P < .01]).
Although not the main focus of this study, several findings deserve mention. In urban and rural analyses, areas with higher shares of for-profit hospital beds were associated with more difficult access to trauma centers (OR, 1.30 for urban areas [P < .01] and 1.47 for rural areas [P < .01]). This is not surprising given that for-profit hospitals tend to be smaller and are not likely to operate trauma services because of their size. This is also interesting in light of the potentially complementary finding that areas with a stronger presence of teaching hospitals were associated with a lower likelihood of poor access to trauma centers in urban and rural contexts.
COMMENT
In this study, we examined whether vulnerable population groups faced more difficult geographical access to trauma centers in 2005. Our findings from this cross-sectional analysis highlight that, in addition to the disparities in treatment care noted in the 2003 Institute of Medicine report,35 certain vulnerable groups appear to face system-level disparities of poorer geographical access to trauma centers in rural and urban areas. In particular, we found that areas with a higher proportion of certain groups, such as African American and near-poor populations in urban and rural areas and foreign-born population in urban areas, were at higher risk of having difficult access to trauma centers or, in other words, were farther away from trauma centers.
Our study has several limitations. First, the zip code–level census data are only available every 10 years. Therefore, it is possible that there will be measurement errors of our key independent variables because our dependent variable was based on 2005 data. However, given the unlikely occurrence of large shifts in zip code composition in 5 years, we do not believe that these slight deviations would significantly alter our results.
Second, although we used a previously described method to calculate distances and correlated this to travel time, driving times may be more variable, especially in rural areas.
Third, we used driving time to the nearest trauma center to define geographic access. It is important to remember that rural communities may have established relationships with aeromedical transport to urban trauma centers, and we may have overestimated the difficulty to access trauma services in those rural communities because we cannot account for aeromedical transport. However, it is unclear how many rural areas have negotiated agreements with other trauma centers for airlifting trauma patients. In addition, even in certain rural settings, the benefit of helicopter transport for most patients (especially those of lower severity) has been questioned36,37; some literature suggests that the current “hub-and-spoke” model of air transport may be the best model for severely injured patients,38 especially when ground transport distance is greater than 45 miles (72 km).39,40 It is crucial to recognize that providing aeromedical transport and building a trauma center are expensive endeavors. Although more extensive discussion of these issues is beyond the scope of this study, it is important for future research to compare the cost-effectiveness of expanding the aerial transport network vs establishing trauma centers (which could include lower level trauma centers).
Finally, we examined only 1 type of access, namely, geographical access to the trauma centers. There are other barriers to care that we cannot address in this study, such as financial and cultural barriers in obtaining trauma care when needed. Persons in communities with easy geographical access to trauma centers still would face disparity in care if they are unable to overcome other types of barriers to care. For example, although we do not find that communities with a high share of Hispanic population face more difficult geographical access to trauma centers, language and cultural barriers still might prevent this population from obtaining timely access to the critical care. Likewise, although communities with high shares of families below the federal poverty line do not have a higher odds of living far away from trauma centers, they are likely to face financial barriers.
Overall, our findings point to a significant segment of the US population (representing 38.4 million people) who do not have access to trauma care within 30 miles (equivalent to 1 hour of driving). Moreover, access is uneven across communities, and certain vulnerable groups are at higher risk than others for worse access to trauma centers. The separate analyses for urban and rural areas show that the types of vulnerable subpopulations facing more difficult access are not identical between urban and rural communities. These findings suggest that there may be fractures in access to care on a system level and that evaluation of trauma center availability should take this type of disparity into consideration. Our research should not be interpreted to mean that trauma centers should be built in every small town across the United States, but rather that access in urban and rural settings is diminished for areas with higher proportions of minority populations and the poor, who may experience a higher burden of injury. Therefore, stakeholders and health care planners should therefore consider these factors in the development of trauma systems because a mismatch of potential need and access could signal inefficiencies in the delivery of care.
Acknowledgments
Funding/Support: This study was supported in part by grant 63974 from the Robert Wood Johnson Foundation’s Health Care Financing and Organization Initiative and the Graduate School of Business and Public Policy Direct Funded Research Program (Dr Shen); and by grant KL2 RR024130 from the National Institutes of Health/National Center for Research Resources/OD University of California–San Francisco-Clinical and Translational Science Institute and a grant under the Robert Wood Johnson Foundation Physician Faculty Scholars Program (Dr Hsia).
Role of the Sponsors: None of the funders had any role in the design and conduct of the study; collection, management, analysis, and interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Author Contributions: Both authors have full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. Study concept and design: Hsia and Shen. Acquisition of data: Shen. Analysis and interpretation of data: Hsia and Shen. Drafting of the manuscript: Hsia and Shen. Critical revision of the manuscript for important intellectual content: Hsia and Shen. Statistical analysis: Shen. Obtained funding: Hsia and Shen. Administrative, technical, and material support: Hsia. Study supervision: Hsia.
Financial Disclosure: None reported.
Disclaimer: The article’s contents are solely the responsibility of the authors and do not represent the official views of the funders or authors’ affiliated institutions.
REFERENCES
- 1.Hulka F, Mullins RJ, Mann NC, et al. Influence of a statewide trauma system on pediatric hospitalization and outcome. J Trauma. 1997;42(3):514–519. doi: 10.1097/00005373-199703000-00020. [DOI] [PubMed] [Google Scholar]
- 2.DeMaria EJ, Kenney PR, Merriam MA, Casanova LA, Gann DS. Aggressive trauma care benefits the elderly. J Trauma. 1987;27(11):1200–1206. doi: 10.1097/00005373-198711000-00002. [DOI] [PubMed] [Google Scholar]
- 3.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. N Engl J Med. 2006;354(4):366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 4.Gaskin DJ, Hadley J. Population characteristics of markets of safety-net and non–safety-net hospitals. J Urban Health. 1999;76(3):351–370. doi: 10.1007/BF02345673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Bazzoli GJ, Kang R, Hasnain-Wynia R, Lindrooth RC. An update on safety-net hospitals: coping with the late 1990s and early 2000s. Health Aff (Millwood) 2005;24(4):1047–1056. doi: 10.1377/hlthaff.24.4.1047. [DOI] [PubMed] [Google Scholar]
- 6.Bazzoli GJ, Meersman PJ, Chan C. Factors that enhance continued trauma center participation in trauma systems. J Trauma. 1996;41(5):876–885. doi: 10.1097/00005373-199611000-00021. [DOI] [PubMed] [Google Scholar]
- 7.Eastman AB, Bishop GS, Walsh JC, Richardson JD, Rice CL. The economic status of trauma centers on the eve of health care reform. J Trauma. 1994;36(6):835–846. [PubMed] [Google Scholar]
- 8.Eastman AB, Rice CL, Bishop G, Richardson JD. An analysis of the critical problem of trauma center reimbursement. J Trauma. 1991;31(7):920–926. doi: 10.1097/00005373-199107000-00007. [DOI] [PubMed] [Google Scholar]
- 9.Shen YC, Hsia RY, Kuzma K. Understanding the risk factors of trauma center closures: do financial pressure and community characteristics matter? Med Care. 2009;47(9):968–978. doi: 10.1097/MLR.0b013e31819c9415. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Branas CC, MacKenzie EJ, Williams JC, et al. Access to trauma centers in the United States. JAMA. 2005;293(21):2626–2633. doi: 10.1001/jama.293.21.2626. [DOI] [PubMed] [Google Scholar]
- 11.Institute of Medicine. Hospital-Based Emergency Care: At the Breaking Point. Washington, DC: Institute of Medicine; 2007. [Google Scholar]
- 12.Institute of Medicine. America’s Health Care Safety Net: Intact but Endangered. Washington, DC: National Academies Press; 2000. [PubMed] [Google Scholar]
- 13.Taheri PA, Butz DA, Lottenberg L, Clawson A, Flint LM. The cost of trauma center readiness. Am J Surg. 2004;187(1):7–13. doi: 10.1016/j.amjsurg.2003.06.002. [DOI] [PubMed] [Google Scholar]
- 14.Taheri PA, Butz DA, Watts CM, Griffes LC, Greenfield LJ. Trauma services: a profit center? J Am Coll Surg. 1999;188(4):349–354. doi: 10.1016/s1072-7515(99)00021-6. [DOI] [PubMed] [Google Scholar]
- 15.Champion HR, Sacco WJ, Copes WS. Improvement in outcome from trauma center care. Arch Surg. 1992;127(3):333–338. doi: 10.1001/archsurg.1992.01420030107020. [DOI] [PubMed] [Google Scholar]
- 16.Nathens AB, Jurkovich GJ, Maier RV, et al. Relationship between trauma center volume and outcomes. JAMA. 2001;285(9):1164–1171. doi: 10.1001/jama.285.9.1164. [DOI] [PubMed] [Google Scholar]
- 17.Sampalis JS, Denis R, Lavoie A, et al. Trauma care regionalization: a process-outcome evaluation. J Trauma. 1999;46(4):565–581. doi: 10.1097/00005373-199904000-00004. [DOI] [PubMed] [Google Scholar]
- 18.Overpeck MD, Jones DH, Trumble AC, Scheidt PC, Bijur PE. Socioeconomic and racial/ethnic factors affecting non-fatal medically attended injury rates in US children. Inj Prev. 1997;3(4):272–276. doi: 10.1136/ip.3.4.272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Haider AH, Chang DC, Efron DT, Haut ER, Crandall M, Cornwell EE., III Race and insurance status as risk factors for trauma mortality. Arch Surg. 2008;143(10):945–949. doi: 10.1001/archsurg.143.10.945. [DOI] [PubMed] [Google Scholar]
- 20.US Census Bureau. United States Census 2000. [Accessed September 10, 2009]; http://www.census.gov/main/www/cen2000.html.
- 21.MelissaDATA. Mailing and Data Management Software. [Accessed January 10, 2009]; http://www.MelissaData.com/software.htm.
- 22.MacKenzie EJ, Hoyt DB, Sacra JC, et al. National inventory of hospital trauma centers. JAMA. 2003;289(12):1515–1522. doi: 10.1001/jama.289.12.1515. [DOI] [PubMed] [Google Scholar]
- 23.Horwitz JR, Nichols A. What do nonprofits maximize? nonprofit hospital service provision and market ownership mix. [Accessed September 17, 2009];National Bureau of Economic Research Working Paper Series 13246. 2007 http://www.nber.org/authors/jill_horwitz.
- 24.Love RF, Morris JG. Mathematical models of road travel distances. Manage Sci. 1979;25(4):130–139. [Google Scholar]
- 25.Phibbs CS, Luft HS. Correlation of travel time on roads versus straight line distance. Med Care Res Rev. 1995;52(4):532–542. doi: 10.1177/107755879505200406. [DOI] [PubMed] [Google Scholar]
- 26.Lerner EB, Moscati RM. The golden hour: scientific fact or medical “urban legend”? Acad Emerg Med. 2001;8(7):758–760. doi: 10.1111/j.1553-2712.2001.tb00201.x. [DOI] [PubMed] [Google Scholar]
- 27.Lucas JW, Barr-Anderson DJ, Kington RS. Health status of non-Hispanic U.S.-born and foreign-born black and white persons: United States, 1992–95. Vital Health Stat. 2005;10(226):1–20. [PubMed] [Google Scholar]
- 28.Singh GK, Hiatt RA. Trends and disparities in socioeconomic and behavioural characteristics, life expectancy, and cause-specific mortality of native-born and foreign-born populations in the United States, 1979–2003. Int J Epidemiol. 2006;35(4):903–919. doi: 10.1093/ije/dyl089. [DOI] [PubMed] [Google Scholar]
- 29.Thamer M, Richard C, Casebeer AW, Ray NF. Health insurance coverage among foreign-born US residents: the impact of race, ethnicity, and length of residence. Am J Public Health. 1997;87(1):96–102. doi: 10.2105/ajph.87.1.96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Shen YC, Zuckerman S. The effect of Medicaid payment generosity on access and use among beneficiaries. Health Serv Res. 2005;40(3):723–744. doi: 10.1111/j.1475-6773.2005.00382.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zuckerman S, Shen YC. Characteristics of occasional and frequent emergency department users: do insurance coverage and access to care matter? Med Care. 2004;42(2):176–182. doi: 10.1097/01.mlr.0000108747.51198.41. [DOI] [PubMed] [Google Scholar]
- 32.O’Hare WP. Poverty in America: trends and new patterns. Popul Bull. 1985;40(3):1–44. [PubMed] [Google Scholar]
- 33.O’Toole TP, Gibbon JL, Seltzer D, Hanusa BH, Fine MJ. Urban homelessness and poverty during economic prosperity and welfare reform: changes in self-reported comorbidities, insurance, and sources for usual care, 1995–1997. J Urban Health. 2002;79(2):200–210. doi: 10.1093/jurban/79.2.200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shen YC. The effect of financial pressure on the quality of care in hospitals. J Health Econ. 2003;22(2):243–269. doi: 10.1016/S0167-6296(02)00124-8. [DOI] [PubMed] [Google Scholar]
- 35.Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2003. [PubMed] [Google Scholar]
- 36.Shepherd MV, Trethewy CE, Kennedy J, Davis L. Helicopter use in rural trauma. Emerg Med Australas. 2008;20(6):494–499. doi: 10.1111/j.1742-6723.2008.01135.x. [DOI] [PubMed] [Google Scholar]
- 37.Greengross P. Effects of helicopter service on survival after trauma: service is part of a continuum of care. BMJ. 1995;311(7013):1164–1165. doi: 10.1136/bmj.311.7013.1164b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Gearhart PA, Wuerz R, Localio AR. Cost-effectiveness analysis of helicopter EMS for trauma patients. Ann Emerg Med. 1997;30(4):500–506. doi: 10.1016/s0196-0644(97)70010-6. [DOI] [PubMed] [Google Scholar]
- 39.Diaz MA, Hendey GW, Bivins HG. When is the helicopter faster? a comparison of helicopter and ground ambulance transport times. J Trauma. 2005;58(1):148–153. doi: 10.1097/01.ta.0000124264.43941.41. [DOI] [PubMed] [Google Scholar]
- 40.Diaz MA, Hendey GW, Winters RC. How far is that by air? the derivation of an air:ground coefficient. J Emerg Med. 2003;24(2):199–202. doi: 10.1016/s0736-4679(02)00725-4. [DOI] [PubMed] [Google Scholar]