Abstract
Objectives
We analyze whether hazard rates of shutting down trauma centers are higher due to financial pressures or in areas with vulnerable populations (such as minorities or the poor).
Materials and Methods
This is a retrospective study of all hospitals with trauma center services in urban areas in the continental US between 1990 and 2005, identified from the American Hospital Association Annual Surveys. These data were linked with Medicare cost reports, and supplemented with other sources, including the Area Resource File. We analyze the hazard rates of trauma center closures among several dimensions of risk factors using discrete-time proportional hazard models.
Results
The number of trauma center closures increased from 1990 to 2005, with a total of 339 during this period. The hazard rate of closing trauma centers in hospitals with a negative profit margin is 1.38 times higher than those hospitals without the negative profit margin (P < 0.01). Hospitals receiving more generous Medicare reimbursements face a lower hazard of shutting down trauma centers (ratio: 0.58, P < 0.01) than those receiving below average reimbursement. Hospitals in areas with higher health maintenance organizations penetration face a higher hazard of trauma center closure (ratio: 2.06, P < 0.01). Finally, hospitals in areas with higher shares of minorities face a higher risk of trauma center closure (ratio: 1.69, P < 0.01). Medicaid load and uninsured populations, however, are not risk factors for higher rates of closure after we control for other financial and community characteristics.
Conclusions
Our findings give an indication on how the current proposals to cut public spending could exacerbate the trauma closure particularly among areas with high shares of minorities. In addition, given the negative effect of health maintenance organizations on trauma center survival, the growth of Medicaid managed care population should be monitored. Finally, high shares of Medicaid or uninsurance by themselves are not independent risk factors for higher closure as long as financial pressures are mitigated. Targeted policy interventions and further research on the causes, are needed to address these systems-level disparities.
Emergency departments and trauma centers are key players of the health care safety net for all patients, especially the underserved. Trauma centers, in particular, have been shown to significantly reduce both morbidity and mortality in numerous studies, and are important public health institutions given that injury is the most important cause of lost years of life in the United States.1–5 Trauma centers, however, are not without costs; they have traditionally been viewed as unprofitable, and have been shown to serve higher proportions of Medicaid and uninsured patients compared with nontrauma centers and sustain greater losses for the care they provide.6,7 Specific concerns have been voiced by the Institute of Medicine (IOM) and other stakeholders regarding the underfunding of and uneven access to trauma centers, which are seen as particularly vulnerable to closure because of the high costs of care.7–11
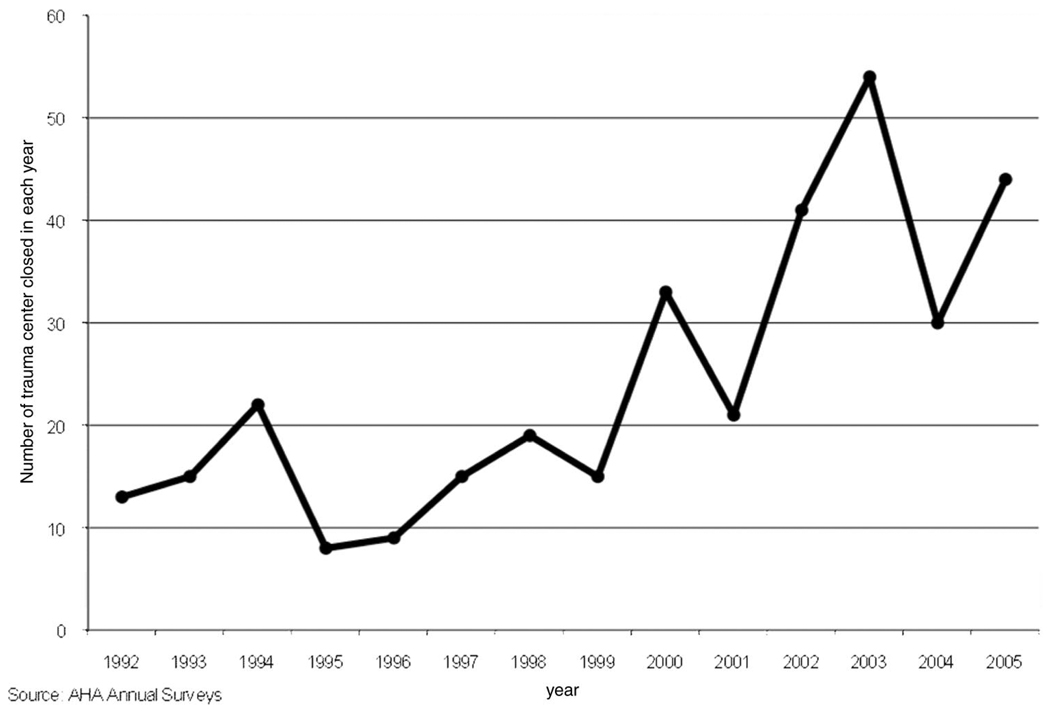
One of the areas that has been relatively unexplored in trauma service studies is the identification of system-level risk factors of trauma center closures. Although there are, on average, an increasing number of trauma centers in the United States, the pattern of openings and closures has been very unstable. One of the few studies looking at closures in the past decade found approximately 60 trauma centers dropped their trauma designation from 1981 to 1991.12 The rate of closures has accelerated, with over 300 trauma centers closing in urban areas between 1990 and 2005.
Current literature in this field is mainly descriptive data on the trends and characteristics of trauma centers.6,10,11,12–19 Although some works document the financial characteristics of trauma centers,6,12,13,18,20–22 to our knowledge, no study has conducted multivariate analysis examining the institutional risk factors of trauma center closures.
Alongside financial considerations, however, it is also important to identify if these exits occur differentially in areas with higher shares of vulnerable populations (eg, poor, minority, uninsured) requiring this service. Although there are some outcomes-based studies documenting racial disparities in trauma care on a patient-level,23–26 no study investigates whether there is a differential closure rate of trauma centers among areas with varying shares of vulnerable populations.
In this study, we aim to extend the work of this field by conducting a multivariate analysis of trauma center closures that occurred between 1990 and 2005. Specifically, we estimate the hazard rates of shutting down these trauma centers along several dimensions of risk factors, particularly: (1) whether financial pressure increases the risks of trauma center closure, holding other characteristics constant; and (2) whether vulnerable populations (such as minority or poor population) are more likely to be in areas with higher risks of trauma center closures.
METHODS
Data and Sample Criteria
The analytical sample includes all general, acute, short-stay hospitals in Metropolitan Statistical Areas (MSA) that have ever offered trauma center services anytime between 1990 and 2005. We limit the sample to hospitals in MSAs because rural hospitals are often designated as critical access hospitals and behave differently from those in urban areas. Last, we exclude a handful of Kaiser Foundation hospitals because they serve exclusively their plan enrollees. It is important to note that only hospitals that have ever offered a trauma center service are included in the analytical sample. This sampling frame contains 1132 hospitals with complete information for a total of 9566 hospital-year observations.
Hospital data primarily come from the American Hospital Association (AHA) Annual Surveys and the Medicare hospital cost reports by Centers for Medicare and Medicaid Services. We further supplement the hospital data with other information to capture relevant market characteristics. Overall health maintenance organizations (HMO) penetration rates at the MSA level were provided by Laurence Baker of Stanford University.27 County population characteristics were obtained from the Area Resource File (ARF). State-level Medicaid payment generosity index is obtained from published reports of the Urban Institute and Lewin Group (see the 3 references at the end). A wage index (a proxy for the cost of living) was obtained from the PPS Impact File, and a patient-flow based hospital competition measure (Herfindahl index) was provided by Glenn Melnick of USC.
We rely on the AHA surveys to identify the existence of trauma centers. The technical definitions of a trauma center have changed over time, but broadly speaking, the definitions provided by the American College of Surgeons/Committee on Trauma (ACS) are generally accepted as the standard. Although the definitions used by the AHA and the ACS are not exactly the same, based on our calibration of data between AHA and another trauma registry based on ACS definitions for 1 year, there is little difference between the number of trauma centers that we use in our analysis, as we use levels I to III trauma centers only. (The trauma registry, maintained by the Trauma Information Exchange Program is only available after 2002.)28
Variable Definitions
Defining Trauma Center Adoption and Closure Years
To analyze the risk of trauma center closure, we also need to track when a hospital opened the trauma center. We use the adoption definition in Baker and Phibbs29 and Shen30—the adoption year is defined as the first year of the first consecutive pair of years in which the hospital reports provision of a trauma center. The closure year is defined using the following logic: (1) there must be an adoption year between 1990 and 2003; (2) closure year is the year after the last year in which the hospital indicates on the AHA survey that it has a trauma center in operation.
Determinants of Trauma Center Closures
Based on previous literature, we conceptualize that the risks of trauma center closure depend on the following set of characteristics. For ease of interpretation of the hazard models results, we use categorical variables in the proportional hazard model instead of the continuous version.
Financial Pressure Measures
Trauma care funding sources vary widely across counties and states,13,19 and the factors and funding situations for the existence of trauma centers differ greatly depending on the context of the hospital. We hypothesized that increasing financial pressure would increase the risks of closing trauma centers. As trauma centers are not a homogenous entity especially in terms of funding, we examine 4 types of financial pressures.
Operating profit margin: the ratio between the net expense (total patient revenue, including disproportionate share [DSH] payments, minus total operating cost) divided by the total operating cost. Financial information tends to be measured with considerable noise and that the decision to close a trauma service might depend on financial situation from prior years. To increase the precision of the estimation, we take the average profit margin from the prior 3 years and include 2 binary indicators to capture the hospitals’ profit status: those hospitals that earned greater than 5% profit margin (representing roughly upper quartile of the profit distribution) and those that earned less than 5% profit margin (lower quartile).
Medicare payment generosity: during the study period, Medicare implemented a series of payment changes for hospitals. We construct a Medicare payment generosity index to capture whether a hospital receives more generous Medicare payments than the average hospital based on previous studies.31–34 First, Medicare fiscal pressure is calculated as the difference between a hospital’s actual payments compared with the payments that it would have received under the new reimbursement method if the hospital did not change its behavior at all in response to the changing reimbursement policies from Medicare. The main variation in Medicare payment across hospitals primarily comes from 4 adjustment factors in the payment formula: the case-mix index, the DSH, the outlier payment, and the indirect medical education payment. The Medicare program has reduced the amount of payment for these adjustment factors throughout the 1990s, with the biggest cut coming from the Balanced Budget Act of 1997. Although the cuts in formula are uniform for all hospitals, the impact on the hospitals are different each year because each hospital has different input values (such as resident-to-bed ratios, number of Medicaid, and SSI patients) for these adjustment factors. When facing a payment cut policy, hospitals could receive higher payments if, for example, they increase their resident-to-bed ratio, in response to the reduction in indirect medical education payment component. To capture the exogenous variation in the Medicare payment, the standard practice is to fix the input values of these adjustment factors in the base year before the cut becomes effective. Second, this measure is weighted by a hospital’s Medicare share of patients so we can capture hospital’s revenue reliance on Medicare. Third, we standardize the Medicare financial index so that the average hospital in each year has the value of 1—hospitals with index above 1 receive more generous payment from Medicare compared with the average hospital. Last, we create 2 binary indicators: one that takes on the value of 1 if a hospital receives 10% higher Medicare payment than the average hospital and 0 otherwise; the other takes on the value of 1 if a hospital receives 10% lower Medicare payment than the average hospital and 0 otherwise.
Medicaid payment generosity: Medicaid programs vary greatly across states. Although we made every effort to find a measure of Medicaid payment generosity for hospitals, such data are not available for the national sample. Instead, we use the state-level Medicaid physician fee index published by the Urban Institute and the Lewin Group.35–37 Specifically, this index is the ratio between each state’s Medicaid physician fee schedule for primary care and the Medicare physician fee schedule for primary care. If a state has an index above 1, its Medicaid program is considered more generous and vice versa. Similar to the Medicare generosity index, we create 2 binary indicators: one that takes on the value of 1 if a hospital’s Medicaid generosity index is 10% higher than the average hospital and 0 otherwise; the other takes on the value of 1 if a hospital’s generosity index is 10% lower than the average hospital and 0 otherwise.
HMO penetration: the literature is well established that HMO increases the financial pressure on providers, and are generally credited for slowing down hospital cost and revenue.30,32,38 How the HMO financial pressure affects trauma survival is an empirical question. The conceptual effect of HMO on trauma closure is ambiguous. On one hand, because of economies of scale, the financial pressure from HMO is likely to drive hospitals to specialize in particular, perhaps more profitable, services. Given the scarce resources, specializing in new profitable services might come at the expense of shutting down existing less profitable services, such as trauma services. On the other hand, managed care generally pays well for trauma care, although it is unclear how large a share this revenue stream represents in the total revenue for trauma centers. We capture the financial pressure from HMOs using the HMO penetration rate, measured as the total HMO enrollment as a share of the MSA population, categorized into 3-quantiles of the HMO penetration distribution.
County Population Composition
We consider the following county population characteristics, with each categorical variable divided into low, medium, and high based on the 3-quantiles of the percent distribution of the characteristics: minority population, poverty, elderly, and uninsured. (As the percent uninsured population is available only for 2 years, 2000 and 2004, we use the average value of percent uninsured from these 2 years to construct the 3-level indicators for hospitals. We noted that there was a high correlation between the 2 years [correlation 0.89].) Other county population characteristics are population size and cost of living.
Other Hospital and Market Characteristics
Some hospitals are legally obligated to provide safety-net services whereas some not-for-profit hospitals might adopt an explicit mission to provide certain services. Although there is no direct measure to identify those core safety-net providers, we use 2 proxies to capture these providers. First, we control for hospital ownership (not-for-profit, for-profit, or government). Second, we control for whether a hospital provides a disproportionate share of Medicaid services compared with its competitors (a hospital is assigned a value of 1 if its Medicaid share of patients are twice as much as that of its competitors within the 15-mile radius).
In addition, we control for the following hospital characteristics: teaching status (if a hospital is member of Council of Teaching Hospital of the Association of American Medical Colleges), system membership, case-mix index, and relevant patient size (measured by total visits to the emergency departments). We also include the following market characteristics in the model: whether there is a presence of another trauma center within 15-mile radius, whether a hospital is in a competitive hospital market (1 if hospital Herfindhal index is <0.25), and hospital market ownership mixture (percent of for-profit and government hospitals within a 15-mile radius).
Statistical Methods
After the standard literature on service adoption and exit, we use discrete-time proportional hazard models.29–31,39 The nonparametric proportional hazard framework is the natural choice to examine service survival. All hospitals that already had a trauma center by 1990 enter the model in 1990. If a hospital did not open a trauma center until 1994, then it does not enter the hazard model until 1994. If a hospital never had a trauma center, then it is not included in the model.
In the proportional hazard framework, we define 14 intervals during which we can observe service exit. Suppose a hospital opens a trauma center in year t0, then intervals (t0, t2), (t2, t3), (t3, t4), and so on capture a hospital that offers the trauma center in the initial year of that interval but drops the service by the end year of the interval. Hospitals that continue offering trauma center service at the end of 2005 are censored at 2005. The probability that hospital i drops its trauma center given that the service was offered up until time t is described by the following hazard function, λi(t):
| (1) |
where λ0(t) = the baseline hazard rate, which differs by the 4 census regions;
Financiali = the 3 types of financial pressure measures described earlier (profit margin, Medicare payment generosity, and HMO penetration level);
Pop_Characit = the set of county population composition measures as described earlier (percent minority, percent population under the poverty line, etc.);
Xit = a vector of other hospital and market characteristics.
In our results section later, we report results from equation (1). We estimate 3 additional models to test the sensitivity of our results. The second model adds an indicator for early adopter (ie, those that had a trauma center since 1990). If the timing of adoption varies systematically across hospitals, the hazard of shutting down trauma center might depend on the time of adoption. The early adopter indicator allows us to test whether the results are sensitive to this assumption. The third model re-estimates equation (1) using Cox proportional hazard model to test the stability of our hazard ratio estimates. (Cox proportional hazard models allow for a more flexible model specification, but assumes that the researcher can observe closures as it happened instead of only on a yearly basis.) The fourth model excludes profit margin variables to examine whether the effect of the policy variables (Medicare and Medicaid payment generosity) in the main model is biased because profit margin is driven partly by the payments received from the government. In all models, we estimate the robust standard errors to account for the fact that many of our population characteristics are measured at the aggregated level. We use Stata 10 to estimate our models.
RESULTS
Characteristics of Hospitals With and Without Trauma Closures
Table 1 presents the descriptive statistics of hospitals and market characteristics by the trauma center closure status between 1990 and 2005. The first column presents average values of characteristics of the whole sample (ie, hospitals that have ever offered a trauma center at any time between 1990 and 2005). The second column represents the average characteristics of hospitals that did not shut down their trauma center by 2005 (ie, hospitals that had existing or opened trauma centers after 1990). The third column includes hospitals that closed the trauma center at any time between 1992 and 2005 and reports the average characteristics of the 3 years before the trauma center was closed. As Table 1 indicates, there are 1125 hospitals that offer a trauma center at any time during the study period, of which 339 were closed by 2005. We present the number of closures in each year in Figure 1.
TABLE 1.
Descriptive Statistics of Hospital and Market Characteristics By Trauma Center Closure Status: 1990 to 2005
| Standard Deviations in Parentheses | Whole Sample All Hospitals With Trauma Center at Some Point |
By Trauma Closure Status |
|
|---|---|---|---|
| No Trauma Center Closure (All-yr Average) |
Trauma Center Closed (3-yr Average Before Closure)* |
||
| Financial pressure measures | |||
| Hospital with <−5% profit margin | 0.22 (0.42) | 0.22 (0.41) | 0.27† (0.44) |
| Hospital with >5% profit margin | 0.19 (0.39) | 0.19 (0.39) | 0.20 (0.40) |
| Hospital received less generous Medicare reimbursement than average | 0.29 (0.46) | 0.30 (0.46) | 0.30 (0.46) |
| Hospital received more generous Medicare reimbursement than average | 0.27 (0.44) | 0.28 (0.45) | 0.17† (0.38) |
| Hospital in states with below average Medicaid physician payment | 0.29 (0.45) | 0.28 (0.45) | 0.31‡ (0.46) |
| Hospital in states with above average Medicaid physician payment | 0.31 (0.46) | 0.32 (0.47) | 0.29‡ (0.45) |
| Medium HMO markets | 0.37 (0.48) | 0.37 (0.48) | 0.39 (0.49) |
| High HMO markets | 0.27 (0.44) | 0.25 (0.44) | 0.30† (0.46) |
| County population characteristics | |||
| Share of minority population | 0.19 (0.15) | 0.19 (0.15) | 0.20‡ (0.15) |
| Share of population below poverty line | 0.13 (0.05) | 0.13 (0.05) | 0.13 (0.05) |
| Share of elderly population | 0.12 (0.03) | 0.12 (0.03) | 0.12 (0.03) |
| Share of uninsured population in 2000 | 0.14 (0.04) | 0.14 (0.04) | 0.14 (0.04) |
| Population size | 1020762 (1658642) | 1004954 (1693202) | 974536 (1472033) |
| Cost of living (log transformed) | 1.03 (0.16) | 1.02 (0.15) | 1.03 (0.16) |
| Hospital characteristics | |||
| For-profit hospital | 0.10 (0.30) | 0.08 (0.27) | 0.20† (0.40) |
| Government hospital | 0.17 (0.37) | 0.18 (0.39) | 0.12† (0.32) |
| Teaching hospital | 0.27 (0.44) | 0.30 (0.46) | 0.12† (0.33) |
| Member of a system | 0.64 (0.48) | 0.63 (0.48) | 0.69† (0.46) |
| Case-mix index | 1.50 (0.23) | 1.53 (0.23) | 1.41† (0.23) |
| Total outpatient visits to ED | 43135 (28362) | 46025 (29261) | 34333† (25534) |
| Hospital market characteristics | |||
| Presence of another trauma center within 15-mile radius | 0.76 (0.43) | 0.76 (0.43) | 0.73§ (0.44) |
| Share of Medicaid discharges twice as much as the average competitor within 15-mile radius | 0.09 (0.28) | 0.09 (0.29) | 0.08 (0.27) |
| Hospital Herfindahl index | 0.35 (0.11) | 0.35 (0.11) | 0.33† (0.10) |
| Percent for-profit hospitals within 15-mile radius | 0.13 (0.18) | 0.14 (0.19) | 0.13‡ (0.18) |
| Percent government hospitals within 15-mile radius | 0.07 (0.12) | 0.07 (0.12) | 0.08† (0.12) |
| No. hospitals | 1125 | 786 | 339 |
| Observations | 9555 | 7117 | 1100 |
Differences between hospitals with and without trauma closures are significant at the following level:
significant at 1%,
significant at 5%,
significant at 10%.
FIGURE 1.
Trend in trauma center closures: 1992 to 2005.
We find several notable differences between hospitals that continue trauma center services and those that discontinue these services by 2005. Hospitals that shut down their trauma centers, in general, face greater financial pressures, with 27% reporting a negative profit margin during the 3 years preceding the closure time (compared with 22% of hospitals in the control sample, P < 0.01). Hospitals that discontinue their trauma centers are also less likely to receive more generous Medicare reimbursement or locate in states with more generous Medicaid generosity index compared with those continuing operation. Thirty percent of hospitals with trauma center closure are located in areas with high levels of HMO penetration (as opposed to 25% of hospitals that continue trauma center operation, P < 0.01). Trauma center closures tend to occur more in hospitals that are for-profit or belong to a system, and less in government and teaching hospitals. There are no noticeable differences in terms of population and hospital market characteristics between the 2 groups of hospitals.
Effects of Financial Pressure on the Risks of Trauma Center Closures
Table 2 presents the estimated effect of the aforementioned risk factors on the hazard of trauma center shut down based on equation (1). We report the hazard ratios instead of the actual coefficients for easier interpretation. Using the comparison between hospitals with negative profit margin (those with <−5% margin) and the reference group (those with profit margin between −5 and 5%, henceforth “break-even” hospitals) as an example, the hazard ratio is the ratio of the hazard rate between hospitals with negative profit margin and those in the reference group, where the hazard rate is the probability that if trauma center has not been dropped in year t, it will be dropped in year t + 1. The reference group has a hazard ratio of 1 by default. A statistically significant hazard ratio above one indicates a higher risk of trauma center closure in hospitals with negative profit margin relative to the reference group.
TABLE 2.
Discrete-Time Proportional Hazard Models on Trauma Center Closures Between 1990 and 2005
| Hazard Ratio | (95% CI) | P | ||
|---|---|---|---|---|
| Financial pressure measures | ||||
| Profit margin | ||||
| Hospital with (−5, 5)% margin | 1.000 | — | — | — |
| Hospital with < −5% profit margin | 1.384‡ | 1.055 | 1.815 | 0.02 |
| Hospital with >5% profit margin | 1.010 | 0.753 | 1.355 | 0.95 |
| Medicare payment generosity | ||||
| Receive average reimbursement | 1.000 | — | — | — |
| Received less generous Medicare reimbursement than average | 1.024 | 0.751 | 1.397 | 0.88 |
| Received more generous Medicare reimbursement than average | 0.578* | 0.374 | 0.892 | 0.01 |
| Medicaid payment generosity | ||||
| Hospitals in states with average Medicaid physician payment | 1.000 | — | — | — |
| Hospitals in states with below average Medicaid physician payment | 1.237 | 0.867 | 1.766 | 0.24 |
| Hospitals in states with above average Medicaid physician payment | 0.939 | 0.697 | 1.264 | 0.68 |
| HMO penetration level | ||||
| Low HMO markets | 1.000 | — | — | — |
| Medium HMO markets | 1.628* | 1.167 | 2.270 | 0.00 |
| High HMO markets | 2.059* | 1.416 | 2.994 | 0.00 |
| County population characteristics | ||||
| Minority population | ||||
| Low share (lower 1/3) | 1.000 | — | — | — |
| Medium share | 1.213 | 0.873 | 1.685 | 0.25 |
| High share | 1.693* | 1.173 | 2.444 | 0.01 |
| Population under poverty line | ||||
| Low share (lower 1/3) | 1.000 | — | — | — |
| Medium share | 1.048 | 0.743 | 1.479 | 0.79 |
| High share | 1.352 | 0.869 | 2.104 | 0.18 |
| Elderly population | ||||
| Low share (lower 1/3) | 1.000 | — | — | — |
| Medium share | 1.122 | 0.825 | 1.525 | 0.46 |
| High share | 1.278 | 0.908 | 1.800 | 0.16 |
| Uninsured population in 2000 | ||||
| 15% or lower | 1.000 | — | — | — |
| Greater than 15% | 0.908 | 0.653 | 1.262 | 0.57 |
| Other population characteristics | ||||
| Population (log transformed) | 1.034 | 0.894 | 1.197 | 0.65 |
| Cost of living (log transformed) | 0.656 | 0.197 | 2.187 | 0.49 |
| Hospital characteristics | ||||
| For-profit hospital | 1.975* | 1.421 | 2.745 | 0.00 |
| Government hospital | 0.856 | 0.575 | 1.275 | 0.45 |
| Teaching hospital | 0.444* | 0.286 | 0.690 | 0.00 |
| Member of a system | 1.276† | 0.982 | 1.660 | 0.07 |
| Case-mix index (log transformed) | 0.108* | 0.042 | 0.277 | 0.00 |
| Total visits to ED (log transformed) | 0.848* | 0.778 | 0.924 | 0.00 |
| Hospital market characteristics | ||||
| Presence of another trauma center within 15-mile radius | 0.833 | 0.630 | 1.102 | 0.20 |
| Share of Medicaid discharges twice as much as the average competitor within 15-mile radius | 0.840 | 0.531 | 1.327 | 0.45 |
| Competitive hospital market (hospital Herfindahl index <0.25) | 0.703‡ | 0.500 | 0.990 | 0.04 |
| Percent for-profit hospitals within 15-mile radius | 1.092 | 0.488 | 2.443 | 0.83 |
| Percent government hospitals within 15-mile radius | 1.561 | 0.616 | 3.958 | 0.35 |
| Observations | 9555 | |||
Census region and year indicators are included.
Significant at 1%,
significant at 10%,
significant at 5%.
The first panel of Table 2 reports the hazard ratios of the financial pressure variables. Relative to the break-even hospitals, the hazard rate of shutting down trauma center is 1.38 times higher in hospitals with a large negative profit margin (P < 0.01). The converse is not true: hospitals with a large positive profit margin are no different from the reference group in their risks of trauma center shutdown. Medicare payment generosity also plays a role: hospitals receiving more generous Medicare reimbursement have a lower hazard rate of shutting down trauma center than those that receive below average reimbursement (hazard ratio 0. 58, P < 0.01), although there is no difference in survival rates between hospitals that receive average or below average reimbursement. Last, higher HMO market share also has a negative effect on trauma center survival: medium and high HMO markets have, respectively, 1.63 and 2.06 times higher hazard rates of shutting down trauma centers compared with hospitals in low HMO market (both P < 0.01).
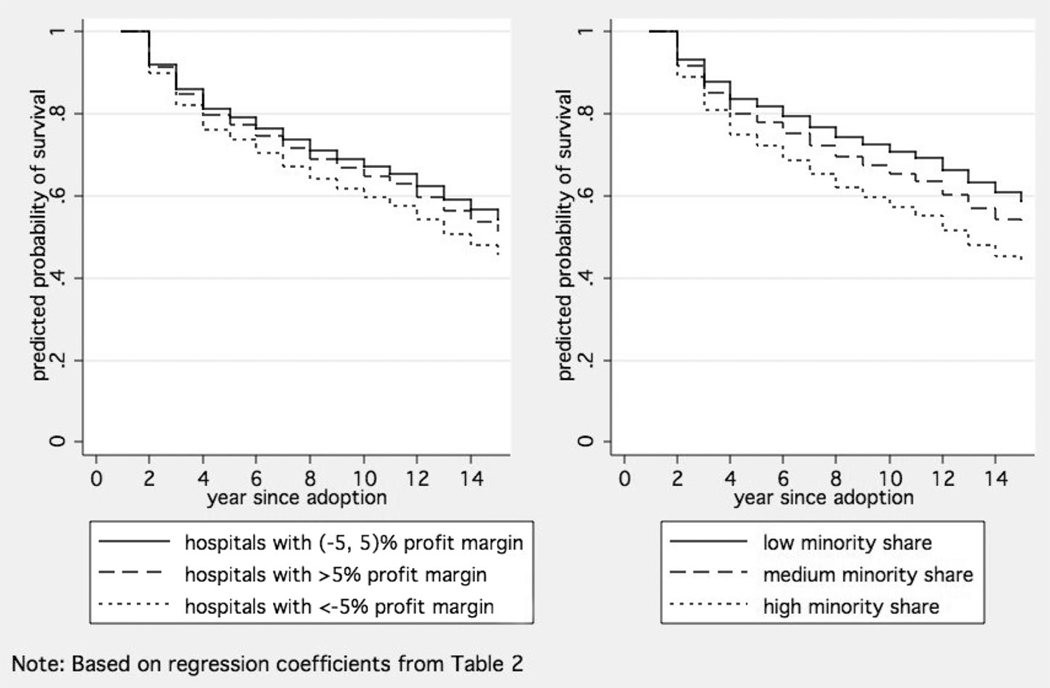
We show the predicted survival probabilities of trauma center by levels of profit margin in Figure 2 (left panel). In the graph, we hold all other characteristics at their average values; therefore, the gaps between the survival curves in the 3 categories of profit margin can be solely attributed to the differences in levels of profit margin. Relative to the breakeven hospitals (solid line), hospitals with negative profit margin (dotted line) clearly show a lower survival rate. By the end of the study period, the cumulative predicted survival probability of trauma center is less than 50% among hospitals with negative profit margin.
FIGURE 2.
Predicted survival probability of trauma centers: by profit margin and by minority share.
County Population Composition and the Risks of Trauma Center Closures
The second panel of Table 2 reports the hazard ratios on the population composition characteristics. There is a strong association between the share of minorities and trauma center closures: hospitals in counties with a high share of minorities (average 36%) face a 1. 69 higher hazard rate (P < 0.01) of shutting down trauma centers than hospitals in counties with a small share of minorities (average 5%). To illustrate this effect, the right panel of Figure 2 shows the predicted survival curves by levels of minority share, holding all other characteristics at the average values. In an alternative model, we separate the minority share into Black and Hispanic share (data available for 1990 and 2000 only; other minority groups, such as Asian, are not available). It seems that the minority results are mainly driven by high shares of black population and not by the Hispanic population (results available on request). Similarly, hospitals in counties with a high share of the population below poverty and a high share of elderly also have a higher hazard of shutting down trauma centers compared with their respective reference groups, although the standard errors are fairly large due to the robust standard error adjustment. However, once we control for all these characteristics, the percentage of uninsured does not matter.
Sensitivity Analysis and Results of Other Variables
The results of various hazard ratios reported earlier are fairly consistent across the 3 models we examined (results of alternative models are included in the Appendix Table A1). Not surprisingly, early adopters of trauma center services have a lower hazard rate of shutting down trauma center (model 2). We obtain remarkably similar coefficients when we use the Cox proportional hazard model (model 3) instead of the discrete-time proportional hazard model. Coefficients on the policy variables remain similar to equation (1) when we exclude profit margin from the analysis (model 4).
APPENDIX TABLE 1.
Estimation Results From Alternative Models on Trauma Center Closures Between 1990 to 2005
| Model 2 (Include Early Adopter Indicator) |
Model 3 (Cox Proportional Hazard) |
Model 4 (Exclude Profit Margin) |
Model 5 (Standard SE) |
|||||
|---|---|---|---|---|---|---|---|---|
| Hazard Ratio |
P | Hazard Ratio |
P | Hazard Ratio |
P | Hazard Ratio |
P | |
| Financial pressure measures | ||||||||
| Profit margin | ||||||||
| Hospital with (−5, 5)% margin | 1.000 | — | 1.000 | — | 1.000 | — | ||
| Hospital with < − 5% profit margin | 1.295* | 0.07 | 1.391† | 0.01 | — | — | 1.384† | 0.00 |
| Hospital with >5% profit margin | 0.971 | 0.85 | 1.048 | 0.73 | — | — | 1.010 | 0.88 |
| Medicare payment generosity | ||||||||
| Receive average reimbursement | 1.000 | — | 1.000 | — | — | — | 1.000 | — |
| Received less generous Medicare reimbursement than average | 0.984 | 0.92 | 1.021 | 0.89 | 1.002 | 0.99 | 1.024 | 0.72 |
| Received more generous Medicare reimbursement than average | 0.555† | 0.01 | 0.629† | 0.02 | 0.614‡ | 0.03 | 0.578† | 0.00 |
| Medicaid payment generosity | ||||||||
| Hospitals in states with average Medicaid physician payment | 1.000 | 1.000 | — | — | — | 1.000 | — | |
| Hospitals in states with below average Medicaid physician payment | 1.439* | 0.05 | 1.127 | 0.50 | 1.231 | 0.25 | 1.237† | 0.00 |
| Hospitals in states with above average Medicaid physician payment | 0.998 | 0.99 | 0.935 | 0.64 | 0.928 | 0.62 | 0.939 | 0.33 |
| HMO penetration level | ||||||||
| Low HMO markets | 1.000 | 1.000 | — | — | — | 1.000 | — | |
| Medium HMO markets | 1.581† | 0.01 | 1.618† | 0.00 | 1.622† | 0.00 | 1.628† | 0.00 |
| High HMO markets | 1.953† | 0.00 | 2.012† | 0.00 | 2.064† | 0.00 | 2.059† | 0.00 |
| County population characteristics | ||||||||
| Minority population | ||||||||
| Low share (lower 1/3) | 1.000 | — | 1.000 | — | — | — | 1.000 | — |
| Medium share | 1.176 | 0.34 | 1.226 | 0.19 | 1.218 | 0.24 | 1.213† | 0.01 |
| High share | 1.587† | 0.01 | 1.694† | 0.00 | 1.693† | 0.01 | 1.693† | 0.00 |
| Population under poverty line | ||||||||
| Low share (lower 1/3) | 1.000 | — | 1.000 | — | — | — | 1.000 | — |
| Medium share | 1.058 | 0.75 | 1.078 | 0.63 | 1.059 | 0.74 | 1.048 | 0.51 |
| High share | 1.339 | 0.20 | 1.303 | 0.20 | 1.352 | 0.18 | 1.352† | 0.00 |
| Elderly population | ||||||||
| Low share (lower 1/3) | 1.000 | — | 1.000 | — | — | — | 1.000 | — |
| Medium share | 1.134 | 0.43 | 1.124 | 0.43 | 1.129 | 0.44 | 1.122* | 0.08 |
| High share | 1.321 | 0.11 | 1.321* | 0.08 | 1.305 | 0.13 | 1.278† | 0.00 |
| Uninsured population in 2000 | ||||||||
| 15% or lower | 1.000 | — | 1.000 | — | — | — | 1.000 | — |
| Greater than 15% | 0.933 | 0.68 | 0.908 | 0.55 | 0.902 | 0.54 | 0.908 | 0.18 |
| Other population characteristics | ||||||||
| Population (log transformed) | 1.015 | 0.84 | 1.028 | 0.70 | 1.038 | 0.61 | 1.034 | 0.29 |
| Cost of living (log transformed) | 1.199 | 0.78 | 0.696 | 0.53 | 0.616 | 0.43 | 0.656 | 0.10 |
| Hospital characteristics | ||||||||
| For-profit hospital | 1.846† | 0.00 | 1.895† | 0.00 | 1.944† | 0.00 | 1.975† | 0.00 |
| Government hospital | 0.847 | 0.42 | 0.876 | 0.50 | 0.892 | 0.57 | 0.856* | 0.07 |
| Teaching hospital | 0.502† | 0.00 | 0.417† | 0.00 | 0.438† | 0.00 | 0.444† | 0.00 |
| Member of a system | 1.261* | 0.09 | 1.250* | 0.07 | 1.271* | 0.07 | 1.276† | 0.00 |
| Case-mix index (log transformed) | 0.132† | 0.00 | 0.114† | 0.00 | 0.097† | 0.00 | 0.108 | 0.00 |
| Total visits to ED (log transformed) | 0.846† | 0.00 | 0.856† | 0.00 | 0.844† | 0.00 | 0.848† | 0.00 |
| Hospital market characteristics | ||||||||
| Presence of another trauma center within 15-mile radius | 0.857 | 0.29 | 0.807 | 0.11 | 0.849 | 0.26 | 0.833† | 0.00 |
| Share of Medicaid discharges twice as much as the average competitor within 15-mile radius | 0.810 | 0.37 | 0.854 | 0.44 | 0.882 | 0.59 | 0.840* | 0.09 |
| Competitive hospital market (hospital Herfindahl index <0.25) | 0.765 | 0.13 | 0.734* | 0.06 | 0.720* | 0.06 | 0.703† | 0.00 |
| Percent for-profit hospitals within 15-mile radius | 1.055 | 0.90 | 1.103 | 0.79 | 1.066 | 0.88 | 1.092 | 0.59 |
| Percent government hospitals within 15-mile radius | 1.634 | 0.31 | 1.512 | 0.37 | 1.594 | 0.33 | 1.561† | 0.03 |
| Early adopter indicator | ||||||||
| = 1 if provide trauma center service since 1990 | 0.485† | 0.00 | — | — | — | — | — | |
| Observations | — | 9555 | — | 9555 | — | 9555 | — | 9555 |
Significant at 1%;
significant at 10%;
significant at 5%.
Census region and year indicators are included.
In our main model, we report our findings using robust standard errors to account for potential clustering of the data at MSA levels and thus should be interpreted as conservative, since only the HMO variables are measured at the MSA level. Accordingly, some of our findings achieve statistical significance only at the alpha = 0.1 level. The last model (model 5) we present in the appendix reports the conventional standard errors (note the hazard ratios are identical to that of Table 2), where the coefficients of the vulnerable population (such as medium and high share of minority population, high share of population under poverty line, and high share of elderly population) achieve statistical significance at the alpha = 0.01 level.
One concern with the main model is that the decision to close the trauma center might have taken place a year or 2 before the closure. To test the sensitivity of our results to this assumption, we re-estimate our model using 2-year lagged values for the independent variables. Our main results remain stable (results available on request). Our analytical samples include hospitals that offer levels I to III trauma services according to AHA surveys. One concern might be that level III trauma centers are sometimes not considered true trauma centers. In another sensitivity analysis, therefore, we exclude level III trauma centers from our model (this reduces the sample size by 15%), and our results remain stable with one exception: the hazard ratio for high minority share is smaller compared with the main model (1.45, P value 0.06).
The results of several hospital and market characteristics, though not the focus of this article, are worth highlighting (third and fourth panels of Table 2). For-profit hospitals have a much higher hazard of closing down trauma center (1.98, P < 0.01) relative to not-for-profit hospitals. However, hospitals with higher Medicaid patient load compared with neighbor hospitals have comparable risks of shutting down trauma centers compared with those who do not have substantial Medicaid patient loads. The presence of another trauma center within 15-mile radius also is not associated with trauma closure. Not surprisingly, teaching hospitals have a much lower hazard of shutting down trauma center (0.46, P < 0.01).
DISCUSSION
The first set of findings from our study provides empirical evidence from a multivariate context that financial pressure is indeed associated with a higher risk of trauma center closure. The results on high HMO penetration is particularly notable because large managed care organizations pay relatively well for trauma care and would actually make the presence of HMOs look better than it should, and yet we still find that they are associated with higher risks of closure. This finding supports the economy of scale argument that the financial pressure from HMOs might drive hospitals to specialize in more profitable services and shut down unprofitable ones such as trauma center. In addition, our results indicate that the relationship between profit margin and trauma center survival is not linear—a higher positive profit margin does not necessarily reduce the risks of trauma center shutdown while negative profit increases the risks of closures. This finding implies that a uniform injection of financial resources into the trauma center system as a whole would not have the desirable effect of curtailing the trauma center closures. Rather, a targeted policy that evaluates the financial pressure faced by each individual hospital and the population they serve would be more effective.
The IOM has reported various disparities in care between white and minority populations.40,41 Our second set of findings supplement that literature by showing that, on the systems level, minorities are also in danger of decreased access to trauma centers. This is particularly concerning given that we already control for financial pressures.
Finally, given the reported size of underpayment from uncompensated care and Medicaid,6,12,13,20,42 our findings are somewhat contrary to the prevailing idea that high shares of Medicaid or uninsured clients within the trauma system are associated with higher risks of closure. Previous studies have shown that trauma centers have higher proportions of uninsured and underinsured patients,11,12,18 and they incur greater financial losses to trauma centers.6 Our study is unique in establishing that once we control for the financial pressures and community characteristics, a hospital with a higher share of Medicaid than its competitors, or serving a community with a high share of uninsured, has comparable risks of shutting down trauma centers compared with others. In other words, the mechanism by which uninsurance and Medicaid load affects trauma center closure is through financial means, and our study includes financial pressure measures as a way to further define these relationships. Taken together with prior studies, our findings indicate that Medicaid or uninsurance by themselves are not independent risk factors for higher closure as long as financial pressures are mitigated. In addition, as we indicated in our methods section, this measure of patient population may reflect a hospital’s status in the community as a core safety-net provider.
We are aware that there are numerous other factors that affect trauma center closure or removal of trauma designation status. We investigated these factors to the fullest extent possible. For example, closure of trauma centers might be influenced by state or local regulations. On review of regulations pertaining to trauma centers, however, we did not find any regulations preventing withdrawal from designation (though some states prohibit hospitals from self-designating themselves as trauma centers). In addition, we control for regional differences in the underlying baseline hazard in our model, which further mitigate potential bias in our estimated results. Even with a carefully chosen set of control variables, however, there might still be some omitted variable bias, so our results are best interpreted as establishing association and not necessarily pointing at a causal relationship.
With these caveats in mind, our findings of the financial pressure effects on trauma center closures have important implications regarding current proposals on public programs (not only federal such as Medicare and Medicaid, but also local mechanisms such as municipal taxes) that may influence the availability of trauma centers. Although we find that a more generous Medicare payment can improve trauma center survival, the reality is that Medicare funding will be cut by $556 billion over the next 10 years.43 Medicaid is under similar pressure, with a proposed $12 billion in cuts over the next 5 years, 47% of which will result in reduced reimbursement to safety-net hospitals.44 All these changes are likely to erode hospitals’ profit margin and exacerbate the trauma closure particularly among areas with high shares of minority.
In addition to monitoring how the proposed cuts might affect trauma center access, attention should be paid to the recent growth of Medicaid managed care, which now represents 60% of the Medicaid population. Given the negative association between HMO penetration level and trauma center survivals, it would be important to monitor the growth of Medicaid managed care population and whether that translates to increased pressure on trauma center closures.
Overall, by refining the understanding of the associations between financial pressures and trauma center survival, our study highlights the importance of robust and targeted financial mechanisms to decrease the risk of trauma center closure especially in areas with high shares of minorities, as well as the continued need to address systematic disparities that exist in trauma center closure for vulnerable populations. Further research should elucidate the reasons behind these disparities and develop interventions to address these systems disparities.
REFERENCES
- 1.Celso B, Tepas J, Langland-Orban B, et al. A systematic review and meta-analysis comparing outcome of severely injured patients treated in trauma centers following the establishment of trauma systems. J Trauma. 2006;60:371–378. doi: 10.1097/01.ta.0000197916.99629.eb. discussion 8. [DOI] [PubMed] [Google Scholar]
- 2.MacKenzie EJ. Review of evidence regarding trauma system effectiveness resulting from panel studies. J Trauma. 1999;47:S34–S41. doi: 10.1097/00005373-199909001-00008. [DOI] [PubMed] [Google Scholar]
- 3.MacKenzie EJ, Rivara FP, Jurkovich GJ, et al. A national evaluation of the effect of trauma-center care on mortality. New Engl J Med. 2006;354:366–378. doi: 10.1056/NEJMsa052049. [DOI] [PubMed] [Google Scholar]
- 4.Nathens AB, Jurkovich GJ, Cummings P, et al. The effect of organized systems of trauma care on motor vehicle crash mortality. JAMA. 2000;283:1990–1994. doi: 10.1001/jama.283.15.1990. [DOI] [PubMed] [Google Scholar]
- 5.Rhodes M, Aronson J, Moerkirk G, et al. Quality of life after the trauma center. J Trauma. 1988;28:931–938. doi: 10.1097/00005373-198807000-00005. [DOI] [PubMed] [Google Scholar]
- 6.Eastman AB, Rice CL, Bishop G, et al. An analysis of the critical problem of trauma center reimbursement. J Trauma. 1991;31:920–925. doi: 10.1097/00005373-199107000-00007. discussion 5–6. [DOI] [PubMed] [Google Scholar]
- 7.Zuckerman S, Bazzoli G, Davidoff A, et al. How did safety-net hospitals cope in the 1990s? Health Aff (Millwood) 2001;20:159–168. doi: 10.1377/hlthaff.20.4.159. [DOI] [PubMed] [Google Scholar]
- 8.Institute of Medicine. America’s Health Care Safety Net: Intact but Endangered. Washington, DC: National Academy Press; 2000. [PubMed] [Google Scholar]
- 9.Bazzoli GJ, Kang R, Hasnain-Wynia R, et al. An update on safety-net hospitals: coping with the late 1990s and early 2000s. Health Aff (Millwood) 2005;24:1047–1056. doi: 10.1377/hlthaff.24.4.1047. [DOI] [PubMed] [Google Scholar]
- 10.Branas CC, MacKenzie EJ, Williams JC, et al. Access to trauma centers in the United States. JAMA. 2005;293:2626–2633. doi: 10.1001/jama.293.21.2626. [DOI] [PubMed] [Google Scholar]
- 11.MacKenzie EJ, Hoyt DB, Sacra JC, et al. National inventory of hospital trauma centers. JAMA. 2003;289:1515–1522. doi: 10.1001/jama.289.12.1515. [DOI] [PubMed] [Google Scholar]
- 12.Dailey JT, Teter H, Cowley RA. Trauma center closures: a national assessment. J Trauma. 1992;33:539–546. discussion 46–47. [PubMed] [Google Scholar]
- 13.Bazzoli GJ, Meersman PJ, Chan C. Factors that enhance continued trauma center participation in trauma systems. J Trauma. 1996;41:876–885. doi: 10.1097/00005373-199611000-00021. [DOI] [PubMed] [Google Scholar]
- 14.Bazzoli GJ, Madura KJ, Cooper GF, et al. Progress in the development of trauma systems in the United States: results of a national survey. JAMA. 1995;273:395–401. [PubMed] [Google Scholar]
- 15.Eastman AB, Lewis FR, Jr, Champion HR, et al. Regional trauma system design: critical concepts. Am J Surg. 1987;154:79–87. doi: 10.1016/0002-9610(87)90294-7. [DOI] [PubMed] [Google Scholar]
- 16.Goldberg J, Levy PS, Gelfand HM, et al. Factors affecting trauma center utilization in Illinois. Med Care. 1981;19:547–566. doi: 10.1097/00005650-198105000-00006. [DOI] [PubMed] [Google Scholar]
- 17.Mullner R, Goldberg J. An evaluation of the Illinois trauma system. Med Care. 1978;16:140–151. doi: 10.1097/00005650-197802000-00006. [DOI] [PubMed] [Google Scholar]
- 18.Selzer D, Gomez G, Jacobson L, et al. Public hospital-based level I trauma centers: financial survival in the new millennium. J Trauma. 2001;51:301–307. doi: 10.1097/00005373-200108000-00012. [DOI] [PubMed] [Google Scholar]
- 19.Bazzoli GJ, MacKenzie EJ. Trauma centers in the United States: identification and examination of key characteristics. J Trauma. 1995;38:103–110. doi: 10.1097/00005373-199501000-00026. [DOI] [PubMed] [Google Scholar]
- 20.Eastman AB, Bishop GS, Walsh JC, et al. The economic status of trauma centers on the eve of health care reform. J Trauma. 1994;36:835–844. discussion 44–46. [PubMed] [Google Scholar]
- 21.Fath J, Ammon A, Cohen MM. Urban trauma care is threatened by inadequate reimbursement. Am J Surg. 1999;177:371–374. doi: 10.1016/s0002-9610(99)00065-3. [DOI] [PubMed] [Google Scholar]
- 22.Taheri PA, Butz DA, Lottenberg L, et al. The cost of trauma center readiness. Am J Surg. 2004;187:7–13. doi: 10.1016/j.amjsurg.2003.06.002. [DOI] [PubMed] [Google Scholar]
- 23.Arthur M, Hedges JR, Newgard CD, et al. Racial disparities in mortality among adults hospitalized after injury. Med Care. 2008;46:192–199. doi: 10.1097/MLR.0b013e31815b9d8e. [DOI] [PubMed] [Google Scholar]
- 24.Chang DC, Britt LD, Cornwell EE. Racial disparities in emergency surgical care. Med Clin North Am. 2005;89:945–948. doi: 10.1016/j.mcna.2005.05.005. 947. [DOI] [PubMed] [Google Scholar]
- 25.Krause JS, Broderick LE, Saladin LK, et al. Racial disparities in health outcomes after spinal cord injury: mediating effects of education and income. J Spinal Cord Med. 2006;29:17–25. doi: 10.1080/10790268.2006.11753852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Shafi S, Marquez de la Plata C, Diaz-Arrastia R, et al. Racial disparities in long-term functional outcome after traumatic brain injury. J Trauma. 2007;63:1263–1268. doi: 10.1097/TA.0b013e31815b8f00. discussion 8–70. [DOI] [PubMed] [Google Scholar]
- 27.Baker L. The effect of HMOs on fee-for-service health care expenditures: evidence from Medicare. J Health Econ. 1997;16:453–481. doi: 10.1016/s0167-6296(96)00535-8. [DOI] [PubMed] [Google Scholar]
- 28.Available at: http://www.amtrauma.org/tiep/index.html.
- 29.Baker L, Phibbs C. Managed care, technology adoption, and health care: the adoption of neonatal intensive care. Rand J Econ. 2002;33:524–548. [PubMed] [Google Scholar]
- 30.Shen Y. Do HMO and its for-profit expansion jeopardize the survival of hospital safety net services? Health Econ. 2009;18:305–320. doi: 10.1002/hec.1366. [DOI] [PubMed] [Google Scholar]
- 31.Cutler D, McClellan M. NBER Working Paper 5751. Cambridge, MA: National Bureau of Economic Research Inc; 1996. The determinants of technological change in heart attack treatment. [Google Scholar]
- 32.Morrisey MA. Competition in hospital and health insurance markets: a review and research agenda. Health Serv Res. 2001;36:191–221. [PMC free article] [PubMed] [Google Scholar]
- 33.Shen Y. The effect of financial pressure on the quality of care in hospitals. J Health Econ. 2004;22:243–269. doi: 10.1016/S0167-6296(02)00124-8. [DOI] [PubMed] [Google Scholar]
- 34.Wu V. Managed Care’s Price Bargaining With Hospitals; Academy Health Annual Research Meeting; June 3, 2005; Cambride, MA. [Google Scholar]
- 35.Menges J, Park C, Babcock J, et al. Comparing Physician and Dentist Fees Among Medicaid Programs. Washington, DC: The Lewin Group; 2001. [Google Scholar]
- 36.Norton S, Zuckerman S. Trends in Medicaid physician fees, 1993–1998. Health Aff (Millwood) 2000;19:222–232. doi: 10.1377/hlthaff.19.4.222. [DOI] [PubMed] [Google Scholar]
- 37.Zuckerman S, McFeeters J, Cunningham P, et al. Changes in Medicaid physician fees, 1998–2003: implications for physician participation. Health Aff (Millwood) 2004 suppl doi: 10.1377/hlthaff.w4.374. W4–374–W4–384. [DOI] [PubMed] [Google Scholar]
- 38.Shen Y, Melnick GA. Forum of Health Economics and Policy. Vol 9. Frontiers in Health Policy Research; 2007. Is managed care still an effective cost containment device? Article 3. [Google Scholar]
- 39.Prentice R, Gloeckler L. Regression analysis of grouped survival data with application to breast cancer data. Biometrics. 1978;34:57–67. [PubMed] [Google Scholar]
- 40.Institute of Medicine. Crossing the Quality Chasm: A New Health System for the 21st Century. Washington, DC: National Academy Press; 2001. [PubMed] [Google Scholar]
- 41.Institute of Medicine. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care. Washington, DC: National Academy Press; 2003. [PubMed] [Google Scholar]
- 42.Hsia RY, MacIsaac D, Baker LC. Decreasing reimbursements for outpatient emergency department visits across payer groups from 1996 to 2004. Ann Emerg Med. 2008;51:265–274. doi: 10.1016/j.annemergmed.2007.08.009. 274, e1–e5. [DOI] [PubMed] [Google Scholar]
- 43.Budget OoMa. Fiscal Year 2009 Budget. US Government Printing Office; 2008. p. 22. [Google Scholar]
- 44.Rudowitz R. Kaiser Commission on Medicaid and the Uninsured. Washington, DC: Kaiser Family Foundation; 2008. Medicaid: overview and impact of new regulations. [Google Scholar]