Abstract
Objective
To study the relationship between sex differences among men and women in the response to pain and the effect on satisfaction with quality of life (QOL) in poststroke patients approximately 90 days after discharge from inpatient medical rehabilitation.
Design
Cross-sectional design.
Setting
Community based.
Participants
The sample included 1724 patients (877 men, 847 women) aged 40 years and older with a history of stroke, according to information obtained from the IT HealthTrack database. The average age was 68.7 years; 79.3% were non-Hispanic white.
Interventions
Not applicable.
Main Outcome Measure
Satisfaction with QOL.
Results
Pain ratings for both the men and the women were significant and inversely associated with satisfaction with QOL after adjustments for possible confounding factors. However, among men with stroke, each 1-point increase in pain rating was associated with an 18% decreased odds of being satisfied with QOL (odds ratio [OR], .81; 95% confidence interval [CI], .77–.86). Conversely, among women with stroke, each 1-point increase in pain rating was associated with an 11% decreased odds of being satisfied with QOL (OR=.89; 95% CI, .84–.95).
Conclusions
Our data indicate that pain after stroke is significantly associated with reduced satisfaction with QOL, particularly among men. Increased awareness and treatment of pain may improve satisfaction with QOL. Our findings suggest that sex differences and pain response are clinically important factors in examining satisfaction with QOL in the poststroke population.
Keywords: Pain, Quality of life, Rehabilitation, Sex, Stroke
THE AMERICAN HEART ASSOCIATION1 estimates that 4.8 million Americans currently live with the effects of stroke, and each year an additional 700,000 persons suffer a new or recurrent stroke. In the coming decades, the number of people with stroke will likely increase, due in part to the rapid aging of the U.S. population and to ongoing advances in stroke management and therapies.1
Clinical and research interests in medical rehabilitation have typically focused on functional outcomes, though more recently subjective outcomes, including those related to quality of life (QOL), have emerged as primary areas of interest. The Institute of Medicine's Enabling America: Assessing the Role of Rehabilitation Science and Engineering2 characterizes QOL as an interaction between the person's external contexts (eg, economic, cultural, environmental, and political) and his/her subjective evaluations and judgments of well-being. Accreditation agencies such as the Joint Commission on Accreditation of Healthcare Organizations3 and the Commission on Accreditation of Rehabilitation Facilities (CARF)4 consider patient QOL an important indicator of outcome assessment and a necessary component when indicators of health care outcomes are evaluated.5 Rehabilitation programs that show improved QOL for their patients after discharge will have clear advantages in the health care marketplace.6
The importance of satisfaction with QOL as a measure of health outcome in rehabilitation medicine may be limited if linkages cannot be made with common modifiable clinical factors. One common and clinically relevant consequence of stroke is pain, with a typical onset within the first 6 weeks after stroke.7 Pain after stroke slows the recovery process, increases health care costs, results in lost wages, and increases dissatisfaction with working life.8 At present, little is known about the relationship between sex differences on the experience of pain and its overall effect on satisfaction with QOL after stroke. The only available data are from a population-based study that evaluated sex differences in the experience of chronic pain and the impact of chronic pain on QOL,9 in which men in chronic pain reported having a poorer QOL compared with women. To our knowledge, no U.S.-based study has factored in differences between the sexes in the response to pain and its overall effect on satisfaction with QOL in a stroke rehabilitation sample.
The present study examines the association between pain and satisfaction with QOL in men and women with stroke, controlling for sociodemographic characteristics and functional status. We hypothesized that higher levels of pain would be associated with less satisfaction with QOL and that the association would differ based on the sex of the patient.
METHODS
Sources of Data
Data were examined from the IT HealthTrack database for the year 2001 to 2002. The IT HealthTrack collects rehabilitation outcomes and follow-up information for 130 rehabilitation facilities across the United States. This database contains information clinically relevant to the subscribing hospitals and contains demographic factors, clinical diagnosis (International Classification of Diseases, 9th Revision, Clinical Modification, codes), discharge setting, functional status, length of stay, living arrangements, vocational status, hospitalizations, follow-up therapy, quality indicators, and general pain ratings. Follow-up information was collected approximately 90 days (range, 80–180d) after patients were discharged from the medical rehabilitation facility.
Study Population
Follow-up data were available for 1724 patients with stroke (877 men, 847 women) aged 40 years and older (case-mix group [CMG] impairment codes 1.1–1.4, 1.9) who had complete information at the follow-up assessment, approximately 90 days after discharge from inpatient medical rehabilitation. Five main stroke groups were included: left body involvement (44.8%; CMG impairment code 1.1); right body involvement (39.6%; CMG impairment code 1.2); bilateral involvement (3.0%; CMG impairment code 1.3); nonparesis (6.7%; CMG impairment code 1.4); and other stroke (5.9%; CMG impairment code 1.9). The institutional review board of each participating rehabilitation facility granted approval of the data collection.
The characteristics of this stroke population were similar to those in the Centers for Medicare and Medicaid Services (CMS).10,11 We compared the sociodemographic and functional status ratings for IT HealthTrack patient records included in this investigation with the descriptive characteristics of patients 65 years and older with stroke in recent CMS reports.10,12 We found no significant differences in demographic variables, patient characteristics, or FIM instrument ratings for the subset of IT HealthTrack records compared with the CMS data.
Outcome Measure
Patients were asked at follow-up interview to “Please rate your satisfaction with your quality of life.” Responses were coded using a 4-point ordinal scale (1, very dissatisfied; 2, somewhat dissatisfied; 3, somewhat satisfied; 4, very satisfied). For analytical purposes, the 4-level satisfaction measure was dichotomized. To do this, we combined those who stated they were very and somewhat satisfied and those who were very or somewhat dissatisfied to reflect the proportion of satisfied versus dissatisfied patients.13,14 Estimates from surveys using this type of single-item scale have shown intraclass correlation coefficients of .82.15
Main Independent Measure
Patients were asked at the follow-up interview to rate their current level of pain. Responses were coded using an 11-point scale ranging from no pain (score, 0) to worst pain possible (score, 10). This single-item measure of pain intensity is the most widely used rating scale in clinical studies. Huskisson16 reports correlations ranging from .71 to .78 between analog pain scales and 4- and 5-point descriptive pain scales. Previous research has also established the psychometric properties of a 0 to 10 pain rating scale.16 For analytical purposes, the pain measure was used as a continuous (0–10) variable.
Covariates
Variables included as covariates in the statistical models were chosen based on their relevance to our poststroke rehabilitation sample.17 Demographic covariates included age (continuous); sex (0, men; 1, women); marital status (1, married; 0, not married); ethnicity (0, non-Hispanic white; 1, non-Hispanic black; 2, Hispanic); and living arrangements (0, living with family/relatives/friends/other; 1, living alone). Rehabilitative covariates included currently receiving therapy (0, none; 1, outpatient/home based/inpatient/long-term care/day treatment) and functional status. Functional status was assessed at follow-up using the FIM items from the Inpatient Rehabilitation Facilities–Patient Assessment Instrument (IRF-PAI).16 The IRF-PAI measures functional status using 18 items covering 6 domains: self-care, sphincter control, transfers, locomotion, communication, and social cognition. The IRF-PAI FIM items include 2 subscales: motor and cognitive. The motor subscale includes the first 4 domains (13 items), and the cognitive subscale includes communication and social cognition (5 items). The instrument is scored by using a 7-level rating where the lowest possible score per item is 1 (most dependent) and the highest possible score is 7 (most independent). The reliability, validity, and responsiveness of the FIM instrument items and subscales have been widely investigated, and consistently produced correlation and statistical values greater than .85.18 The interrater reliability and stability of the collected FIM follow-up information has yielded intraclass correlation coefficients ranging from .86 to .99.19
Statistical Analysis
In the cross-sectional analysis, we examined demographic and functional status variables for patients with stroke using descriptive and univariate statistics for continuous variables and contingency tables for categorical variables. First we assessed the interaction between sex differences and the response to pain in unadjusted and adjusted models, and obtained significant results. Using these results, we proceeded to stratify our univariate and multivariate analyses between men and women. Logit models assessed the association between men and women's pain ratings (continuous) and their overall satisfaction with QOL (dichotomous), adjusting for relevant risk factors. Each reported odds ratio (ORs) (and 95% confidence intervals [CIs]) for the logit models is interpreted as the effect of the pain variable on the odds of being in a higher satisfaction level rather than in a lower satisfaction level with and without adjustment for relevant risk factors. Model fit was evaluated through Pearson goodness-of-fit test statistics; all reported models fit the data (ie, P>.15). Statistical analyses were performed using SAS.20,a
RESULTS
Table 1 presents the demographic characteristics and health-related factors for the sample. The mean age ± standard deviation was 68.7±14.1 years (range, 40–99y); most subjects were non-Hispanic white (79.3%), followed by non-Hispanic black (15.1%), and Hispanic (5.6%); 16.4% lived alone, and 42.0% received therapy at follow-up; mean FIM instrument rating at discharge was 89.3±20.1. Approximately one third of the sample reported pain (score >0). Overall, men and women reported similar mean pain scores (1.57±2.67 vs 1.55±2.66; range, 0–10) and similar satisfaction with QOL rating (very satisfied: 41.7% of men and 46.6% of women).
Table 1.
Selected Characteristics of Patients with Stroke by Sex (N = 1724)
| Variable | Total | Men | Women |
|---|---|---|---|
| n | 1724 | 877 | 847 |
| Mean age ± SD (y) | 68.7±14.1 | 67.5±14.1 | 69.8±13.9 |
| Ethnicity, n (%) | |||
| White | 1368 (79.3) | 707 (80.6) | 661 (78.0) |
| Black | 260 (15.1) | 120 (13.7) | 140 (16.5) |
| Hispanic | 96 (5.6) | 50 (5.7) | 46 (5.5) |
| Living arrangements, n (%) | |||
| Alone | 283 (16.4) | 92 (10.5) | 191 (22.5) |
| Other | 1441 (83.6) | 785 (89.5) | 656 (77.5) |
| Receiving therapy, n (%) | |||
| Yes | 724 (42.0) | 378 (43.1) | 501 (59.1) |
| No | 1000 (58.0) | 499 (56.9) | 346 (40.9) |
| Mean pain ± SD | 1.56±2.66 | 1.57±2.67 | 1.55±2.66 |
| Satisfaction with QOL, n (%) | |||
| Very dissatisfied | 86 (5.0) | 45 (5.1) | 41 (4.8) |
| Somewhat dissatisfied | 242 (14.0) | 133 (15.2) | 109 (12.9) |
| Somewhat satisfied | 364 (36.9) | 333 (38.0) | 302 (35.7) |
| Very satisfied | 761 (44.1) | 366 (41.7) | 395 (46.6) |
| Mean discharge FIM ± SD | 89.3±20.1 | 89.3±20.0 | 89.5±20.3 |
Abbreviation: SD, standard deviation.
We first tested the association between time of follow-up assessment (80–180d) and pain scores and satisfaction with QOL ratings independently to determine the need to control for time of follow-up assessment in our analyses. The results of Pearson product-moment correlations (not shown) showed weak and nonsignificant associations between QOL and time of assessment and pain scores and time of assessment, indicating no need to control for time of assessment in the models.
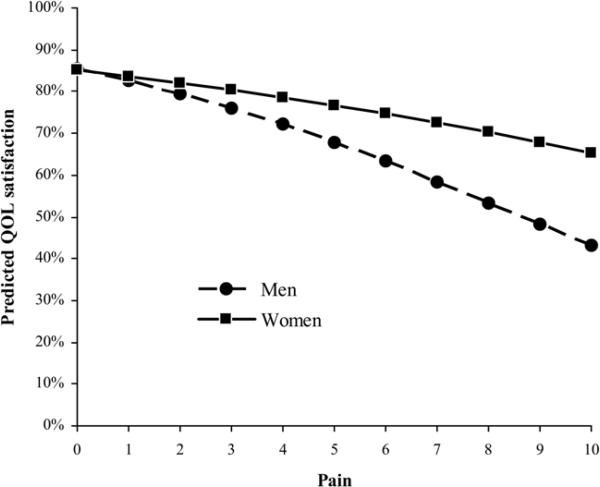
Next, we tested interaction effects between pain and sex differences on QOL. Significant results were found for the unadjusted model (OR=1.09; 95% CI, 1.02–1.19; P<.02). Figure 1 shows the sex-specific effect on the association between pain and QOL. As pain score increased, satisfaction with QOL decreased, though the trend was stronger for men than for women, that is, compared with men at higher levels of pain, women reported greater satisfaction with QOL.
Fig 1.
Pain and satisfaction with quality of life by sex.
Based on these results, we re-examined the effects of pain on QOL stratified by sex. Table 2 shows the association between the continuous pain score and satisfaction with QOL. Models 1 and 3 show the unadjusted effect of pain on satisfaction with QOL for men and women, respectively. Each 1-point increase in pain score was associated with a 19% decreased odds of being satisfied with QOL for men (OR=.81; 95% CI, .77–.86) and with an 11% decreased odds of being satisfied with QOL for women (OR=.89; 95% CI, .84–.95). Models 2 and 4 adjusted for age, ethnicity, living arrangements, current therapy, and discharge FIM ratings. Adding these variables to the models did not change pain scores as a significant predictor of satisfaction with QOL for both men and women.
Table 2.
Logit Models Assessing Associations Between Continuous Pain Scores and Satisfaction With QOL for Patients With Stroke (N = 1724)
| Men (n=877) |
Women (n=847) |
|||
|---|---|---|---|---|
| Variable | Model 1* OR (95% CI) | Model 2† OR (95% CI) | Model 3* OR (95% CI) | Model 4† OR (95% CI) |
| Pain (0–10) | 0.81 (0.77–0.86) | 0.81 (0.77–0.86) | 0.89 (0.84–0.95) | 0.89 (0.84–0.95) |
| Age (continuous) | NE | 1.00 (0.99–1.01) | NE | 1.00 (0.98–1.01) |
| Non-Hispanic white (vs other) | NE | 1.14 (0.73–1.77) | NE | 0.86 (0.56–1.33) |
| Living arrangements (alone) | NE | 0.67 (0.34–1.30) | NE | 0.44 (0.24–0.78) |
| Receiving therapy (yes) | NE | 0.70 (0.48–1.00) | NE | 0.82 (0.56–1.20) |
| Discharge FIM | 1.02 (1.01–1.03) | 1.02 (1.01–1.02) | ||
| R 2 | 0.10 | 0.15 | 0.02 | 0.10 |
Abbreviation: NE, variable not entered into the model.
Unadjusted model.
Adjusted model.
DISCUSSION
The current study assessed the association between pain and satisfaction with QOL in patients with stroke approximately 90 days after discharge from inpatient medical rehabilitation. To increase the clinical applicability of our findings, we used the CMG impairment codes (1.1–1.4, 1.9). The results confirmed an inverse association between pain and satisfaction with QOL. Most interestingly, men and women reported similar levels of satisfaction with QOL in the absence of pain or at low levels of pain (ie, pain scores ≤2); however, as levels of pain increased, men's satisfaction with QOL decreased more than women's.
The differential effect of pain on satisfaction with QOL among men and women is an important finding, given the limited research in this area in medical rehabilitation.21 Our results support those of population-based studies and studies in cancer patients which have found sex differences in the report of pain and its association with QOL.22,23 Rustoen et al9 suggest that women's greater satisfaction with QOL in the presence of pain has several reasons: first, women are more proactive in seeking help to alleviate pain and, second, women are more likely than men to adhere to analgesic treatments. Myers et al23 add that men tend to underreport pain and have a stoic attitude toward pain. Collectively, these studies suggest the need for further research to better understand the role of sex differences in the experience of pain and its impact on overall well-being.
Previous research has showed discrepancies in pain assessment between patients and clinical staff, indicating the importance of the patient's evaluation and judgment of the relation between pain and well-being.24 Government and other accrediting agencies now recognize the importance of assessing patients’ perceptions regarding QOL. CARF4 has indicated that rehabilitation programs are in a new era of evidence-based accreditation, where patient-focused outcomes, including assessments of QOL, are important indicators of program excellence.6 More recently, the Institute of Medicine25 has recommended the implementation of a patient-centered model to develop new clinical guidelines for patient care. Given that patient's self-reports are linked to health, the challenge for rehabilitation providers is to understand how to effectively intervene to improve patients’ QOL.
The current study found low overall levels of general post-stroke pain in the sample. The average pain rating for the overall sample was 1.5 (range, 0–10) with 32% of persons with stroke reporting some level of pain. In a subanalysis (data not shown) conducted on those who reported pain, however, findings indicated an average pain rating of 4.7. This result was comparable with those by Jönsson et al,26 who report that about one third of persons with stroke experience pain 4 months after the stroke with an average pain rating of 50 on a scale from 1 to 100. Because pain is a well-known condition after a stroke,8 and with the high prevalence of stroke in the United States and the disability that follows, additional studies are needed to explore variations in occurrence in different populations.
The current study contributes to the understanding of sex differences in the evaluation of QOL among clinical populations. The value of our findings is strengthened by the large well-defined sample using CMG impairment codes, the consistency of data collection procedures, and the time to follow-up.
Study Limitations
The study does have some limitations. First, satisfaction with QOL as well as pain was assessed by a single-item measure, which was an original component of the standard interview process of the collection of follow-up information by the IT HealthTrack. Single-item measures have the advantage that they can be administered and scored easily,27 and have showed good response stability.28,29 On the other hand, single-item measures do not allow for examination of different dimensions of a construct and offer a small range of responses that might not capture small differences. The use of a more comprehensive measure of pain, for example, may have provided important information on specific types of pain experienced by patients poststroke (eg, neurogenic, central poststroke, nociceptive, or tension-type headache) and their association with QOL, thus increasing the generalizability of the results. A second limitation of the study was that the explained variance of the models was relatively low; however, the goal of the study was not to build a prediction model, but to provide accurate estimates that would reflect the association between pain and satisfaction with QOL across sex.30 Finally, the current sample may not be representative or generalize to other persons with stroke, although we compared the sociodemographic characteristics of the current stroke sample with CMS data31 and found it was similar.
CONCLUSIONS
In this secondary analysis of men and women with stroke, pain appeared to be a sex-specific determinant of satisfaction with QOL after inpatient medical rehabilitation. These results may aid rehabilitation professionals focus on the importance of sex differences in designing treatment modalities.
Acknowledgments
Supported by the National Institute on Aging (grant no. K02 AG019736), the National Center for Medical Rehabilitation Research (grant no. K01 HD046682), and the American Heart Association (grant no. 027045N).
Footnotes
No commercial party having a direct financial interest in the results of the research supporting this article has or will confer a benefit upon the author(s) or upon any organization with which the author(s) is/are associated.
SAS Institute Inc, 100 SAS Campus Dr, Cary, NC 27513.
References
- 1.American Heart Association . Heart disease and stroke statistics— 2005 update. American Heart Association; Dallas: 2004. [Google Scholar]
- 2.Brandt EM, Pope A. Enabling America: assessing the role of rehabilitation science and engineering. Natl Acad Pr; Washington (DC): 1997. [PubMed] [Google Scholar]
- 3.Joint Commission on Accreditation of Healthcare Organizations . Guidelines for establishing and evaluating outcomes in clinical settings. JCAHO; Washington (DC): 1994. [Google Scholar]
- 4.CARF . 2003 medical rehabilitation standards manual. CARF; Tucson: 2002. [Google Scholar]
- 5.The Medicare health outcomes survey program: overview, context, and near-term prospects. Health Qual Life Outcomes. 2004;2:33. doi: 10.1186/1477-7525-2-33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wilkerson D, Shen D, Duhaime M. Performance indicators for rehabilitation programs. Rehabilitation Accreditation Commission (CARF); Tucson: 1998. Version 1.1. [Google Scholar]
- 7.Langhorne P, Stott DJ, Robertson L, et al. Medical complications after stroke: a multicenter study. Stroke. 2000;31:1223–9. doi: 10.1161/01.str.31.6.1223. [DOI] [PubMed] [Google Scholar]
- 8.Andersen G, Vestergaard K, Ingemannielsen M, Jensen TS. Incidence of central poststroke pain. Pain. 1995;61:187–93. doi: 10.1016/0304-3959(94)00144-4. [DOI] [PubMed] [Google Scholar]
- 9.Rustoen T, Wahl AK, Hanestad BR, Lerdal A, Paul S, Miaskowski C. Gender differences in chronic pain—findings from a population-based study of Norwegian adults. Pain Manag Nurs. 2004;5:105–17. doi: 10.1016/j.pmn.2004.01.004. [DOI] [PubMed] [Google Scholar]
- 10.Carter GM, Buntin MB, Hayden O, et al. Analysis for the initial implementation of the inpatient rehabilitation facility prospective payment system. Rand Corp; Santa Monica: 2002. No. MR-1500-CMS. [Google Scholar]
- 11.Medicare Payment Advisory Commission . A data book: healthcare spending and the Medicare program. MedPAC; Washington (DC): 2005. [Google Scholar]
- 12.Carter GM, Paddock SM. Preliminary analysis of changes in coding and case mix under the inpatient rehabilitation facility prospective payment system. Rand Corp; Santa Monica: 2004. [Google Scholar]
- 13.Hall JA, Dornan MC. Meta-analysis of satisfaction with medical care: description of research domain and analysis of overall satisfaction levels. Soc Sci Med. 1988;27:637–44. doi: 10.1016/0277-9536(88)90012-3. [DOI] [PubMed] [Google Scholar]
- 14.Tooth LR, Ottenbacher KJ, Smith PM, et al. Effect of functional gain on satisfaction with medical rehabilitation after stroke. Am J Phys Med Rehabil. 2003;82:692–9. doi: 10.1097/01.PHM.0000083672.01300.47. quiz 700-1, 715. [DOI] [PubMed] [Google Scholar]
- 15.McDowell I, Newell C. Measuring health: a guide to rating scales and questionnaires. Oxford Univ Pr; New York: 1996. [Google Scholar]
- 16.Huskisson EC. Measurement of pain. Lancet. 1974;2:1127–31. doi: 10.1016/s0140-6736(74)90884-8. [DOI] [PubMed] [Google Scholar]
- 17.Bhandari VK, Kushel M, Price L, Schillinger D. Racial disparities in outcomes of inpatient stroke rehabilitation. Arch Phys Med Rehabil. 2005;86:2081–6. doi: 10.1016/j.apmr.2005.05.008. [DOI] [PubMed] [Google Scholar]
- 18.Ottenbacher KJ, Hsu Y, Granger CV, Fiedler RC. The reliability of the functional independence measure: a quantitative review. Arch Phys Med Rehabil. 1996;77:1226–32. doi: 10.1016/s0003-9993(96)90184-7. [DOI] [PubMed] [Google Scholar]
- 19.Smith PM, Illig SB, Fiedler RC, Hamilton BB, Ottenbacher KJ. Intermodal agreement of follow-up telephone functional assessment using the Functional Independence Measure in patients with stroke [published erratum appears in Arch Phys Med Rehabil 1996;77:784]. Arch Phys Med Rehabil. 1996;77:431–5. doi: 10.1016/s0003-9993(96)90029-5. [DOI] [PubMed] [Google Scholar]
- 20.SAS Institute . SAS/STAT user's guide. SAS Institute Inc; Cary: 2004. Version 9. [Google Scholar]
- 21.Widar M, Ahlstrom G, Ek AC. Health-related quality of life in persons with long-term pain after a stroke. J Clin Nurs. 2004;13:497–505. doi: 10.1046/j.1365-2702.2003.00815.x. [DOI] [PubMed] [Google Scholar]
- 22.Thome B, Hallberg IR. Quality of life in older people with cancer—a gender perspective. Eur J Cancer Care (Engl) 2004;13:454–63. doi: 10.1111/j.1365-2354.2004.00471.x. [DOI] [PubMed] [Google Scholar]
- 23.Myers CD, Riley JL III, Robinson ME. Psychosocial contributions to sex-correlated differences in pain. Clin J Pain. 2003;19:225–32. doi: 10.1097/00002508-200307000-00005. [DOI] [PubMed] [Google Scholar]
- 24.Idler EL, Angel RJ. Self-rated health and mortality in the NHANES-I Epidemiologic Follow-up Study. Am J Public Health. 1990;80:446–52. doi: 10.2105/ajph.80.4.446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Institute of Medicine . Crossing the quality chasm: a new health system for the 21st century. Natl Acad Pr; Washington (DC): 2001. [PubMed] [Google Scholar]
- 26.Jönsson AC, Lindgren I, Norrving B, Lindgren A. Prevalence and intensity of pain after stroke: a population based study focusing on patient's perspectives. J Neurol Neurosurg Psychiatry. 2006;77:590–5. doi: 10.1136/jnnp.2005.079145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ottenbacher KJ, Gonzales VA, Smith PM, Illig SB, Fiedler RC, Granger CV. Satisfaction with medical rehabilitation in patients with cerebrovascular impairment. Am J Phys Med Rehabil. 2001;80:876–84. doi: 10.1097/00002060-200112000-00002. [DOI] [PubMed] [Google Scholar]
- 28.Cleary PD, McNeil BJ. Patient satisfaction as an indicator of quality care. Inquiry. 1988;25:25–36. [PubMed] [Google Scholar]
- 29.Steiber SR, Krowinski WJ. Measuring and managing patient satisfaction. American Hospital Publisher; Chicago: 1990. [Google Scholar]
- 30.Muller KE, Fetterman BA. Regression and ANOVA. SAS Publishing; Cary: 2002. [Google Scholar]
- 31.Carter GM, Relles DA, Buchanan JL, et al. A classification system for inpatient rehabilitation patients: a review and proposed revisions to the Functional Independence Measure-Function Related Groups. Rand Corp; Santa Monica: 1997. No. PM-682-HCFA. [Google Scholar]