Abstract
Although most studies find low socioeconomic status (SES) to be associated with prevalence of schizophrenia, incidence studies do not generally support this, and some even report an inverse association. The objective of the current historical prospective study was to examine the relationship between SES, cognitive functioning, and risk of hospitalization for schizophrenia in a population-based sample of Israeli adolescents. Subjects were 811 487 adolescents, assessed by the Israeli military draft board for socio-demographic factors and cognitive functioning. Data on later hospitalization for schizophrenia were obtained from a population-based hospitalization registry. Findings indicated that when simply examining SES and schizophrenia, lower SES was associated with greater risk of hospitalization for schizophrenia (Hazard Ratio [HR] = 1.193, 95% CI = 1.091–1.303). When dividing the cohort into low, average, and high cognitive functioning, SES did not influence the risk for schizophrenia among individuals with high and average cognitive functioning, whereas among individuals with low cognitive functioning, high SES was found to slightly increase the risk for schizophrenia (HR = 1.21, 95% CI = 1.03–1.42). One possible explanation for this finding might be that among individuals from low socioeconomic backgrounds, low IQ may reflect decreased opportunities related to SES, whereas among individuals from high SES backgrounds, low IQ might reflect risk for later psychopathology.
Keywords: socioeconomic status, cognition, psychotic illness
Introduction
Previous research on the association between socioeconomic status (SES) and risk for schizophrenia has yielded mixed results. Although studies examining patients' SES have generally agreed that low SES is associated with higher risk for schizophrenia, studies examining parental or childhood SES have been inconclusive.1,2 While some studies have indicated that growing up in a low SES environment is associated with increased risk for schizophrenia,3–9 others have found no such effect,10–14 and still others have reported that growing up in a high SES environment may be associated with higher risk for schizophrenia15–18 (see table 1 for a summary of previous studies which examined childhood SES). The objective of the current study was to address this controversial issue by examining the association between SES and risk of hospitalization for schizophrenia in a large population-based sample of Israeli adolescents assessed by the Israeli military draft board before the onset of illness, then followed for later hospitalization for schizophrenia using a national psychiatric hospitalization registry. Furthermore, given that lower cognitive functioning is a core feature of the illness often present before the onset of psychosis22,23 and that low SES is associated with low cognitive functioning,24,25 an additional goal of this study was to explore the relationship between cognitive functioning, childhood SES, and risk for schizophrenia.
Table 1.
Previous Studies on the Association Between Childhood SES and Risk for Schizophrenia in Adulthood
| Author | Year | Country | N | Measures of SES | Central Findings |
| Goldberg et al10 | 1963 | United Kingdom | 369 | Paternal occupation | Paternal SES was similar to that in the general population. |
| Turner et al4 | 1967 | United States | 214 | Paternal occupation | Lower paternal occupational prestige during childhood was associated with higher rates of schizophrenia in offspring. |
| Grünfeld et al11 | 1968 | Norway | 186 (85 with schizophrenia diagnosis) | Paternal occupation | Paternal SES was similar to that in the general population. |
| Hare et al12 | 1972 | United Kingdom | 624 (175 with schizophrenia diagnosis) | Paternal occupation | Paternal SES was similar to that in the general population. |
| Wiersma et al13 | 1983 | Netherlands | 83 (34 with schizophrenia diagnosis) | Paternal occupation | Only 38% of the schizophrenic patients in the study came from low SES backgrounds. |
| Malama et al15 | 1988 | Greece | 486 | Paternal education | Greater paternal education was associated with higher risk for schizophrenia. |
| Dohrenwend et al19 | 1992 | Israel | 4914 | Ethnicity | Advantaged ethnic status (European origins) was associated with higher rates of schizophrenia than disadvantaged ethnic status (North African origins). |
| Castle et al7 | 1993 | United Kingdom | 256 | Place of birth and paternal occupation | Patients with schizophrenia were more likely to have been born in a low SES area and to have fathers who worked in manual labor. |
| Dauncey et al8 | 1993 | United Kingdom | 67 | Place of birth | Rates of schizophrenia were higher among participants born in low SES areas. |
| Jones et al14 | 1994 | United Kingdom | 5362 | Paternal occupation and place of birth | No association was found between childhood SES and risk for schizophrenia. |
| Mäkikyrö et al16 | 1997 | Finland | 11 017 | Paternal occupation | Higher SES was associated with greater risk for schizophrenia. |
| Timms17 | 1998 | Sweden | 15 117 | Parental occupation | Higher SES was associated with greater risk for schizophrenia. |
| Mulvany et al18 | 2001 | Ireland | 704 | Paternal occupation | Risk of schizophrenia was slightly higher among participants with high SES. However, these findings may be associated with the younger age of participants in the high SES group. |
| Harrison et al9 | 2001 | United Kingdom | 280 | Paternal occupation and maternal place of residence at birth | Risk of schizophrenia was higher among those with low SES. |
| Eaton et al1 | 2001 | — | Review | Paternal occupation | Three out of the five studies indicated that high SES was associated with higher risk for schizophrenia. In one study, the risk was nonsignificantly associated with SES and in one study low SES was associated with higher risk. |
| Byrne et al20 | 2004 | Denmark | 200 294 | Parents' occupation, education, income, wealth | Increased risk was associated with parental unemployment and low income. Increased risk was not associated with parental wealth, but was associated with greater parental education. |
| Wicks et al3 | 2005 | Sweden | 2.1 million | Parental occupation, social welfare benefits, unemployment, single-parenthood, and housing type | Higher risk for schizophrenia was associated with lower SES, as well as cumulatively (the greater the number of risk factors) |
| Saraceno et al21 | 2005 | Review | — | Various measures | While the majority of studies do not support the association between childhood SES and later risk for schizophrenia, a number of studies have found lower childhood SES to be associated with greater risk. |
| Werner et al6 | 2007 | Israel | 71 165 | Individual SES: parents' education and occupational status | Lower individual and community SES were associated with greater risk for schizophrenia. |
| Community SES: residential area | |||||
| Corcoran et al5 | 2009 | Israel | 88 829 | Paternal occupation at birth | No linear association was found between SES and risk for schizophrenia. However, an increased risk for schizophrenia was found among the lowest SES group. |
Note: SES, socioeconomic status.
Methods
Israeli Draft Board Registry
All adolescents in Israel undergo a mandatory predraft screening at ages 16–17 years in order to evaluate their eligibility to participate in military service. This screening assesses socio-demographic characteristics as well as physical, social, and cognitive functioning. The cognitive assessment includes 4 tests: (1) a modified Otis-type verbal intelligence test, appraising ability to understand and execute verbal instructions; (2) verbal analogies, a modified version of the “similarities” subtest of the Wechsler Intelligence Scales, measuring verbal abstraction and categorization; (3) mathematical knowledge, assessing mathematical reasoning, concentration, and concept manipulation; and (4) nonverbal analogies, a modified version of Raven’s Progressive Matrices that evaluates nonverbal abstract reasoning and visual–spatial problem-solving abilities. The tests become progressively more difficult as subjects complete the different sections and are time-limited. Scores are based on the number of correct answers. The sum of the scores for the 4 tests forms a validated measure of general cognitive abilities,23,26 scored on a 9-point scale (scaled between 10 and 90, with a 10-point increment at each score). These scores were computed into standardized scores prior to analysis. In this study, we used the sum score as a composite measure of cognitive functioning.
Israeli Central Bureau of Statistics
This study used an index of neighborhood SES, which was developed and validated by The Israeli Central Bureau of Statistics.27 The country is divided into 1559 “geographical units,” which are areas with approximately 2000 residents, who are as homogeneous as possible in terms of ethnic background, culture, and income. Small villages with fewer residents were not included. Each area is given an ordinal ranking from 1 to 20 based on information on a wide range of factors, including demographic information, education, standard of living, employment, and social benefits.28
Israeli Psychiatric Hospitalization Case Registry
The Israeli Psychiatric Hospitalization Case Registry is a complete listing of all International Classification of Diseases (ICD–10) discharge diagnoses assigned by a board-certified psychiatrist at the reporting facility. All psychiatric hospitals, day hospitals, and psychiatric units in general hospitals are required by law to report all admissions and discharges to this registry. From the registry, we identified patients with a last discharge diagnosis of schizophrenia (ICD–10 codes F20.0–F20.9). Because the first psychotic episode is associated with cognitive decline, we only included data on those patients who had a first hospitalization, which occurred 1 year or more after the draft board assessment (1961 cases, 0.2% of the sample).
Study Population
After receiving approval from the Internal Review Boards both of the Israel Defense Forces Medical Corps and the Chaim Sheba Medical Center, the file containing data on SES by residential address at the time of the draft board assessment was linked to the draft board file, which contains results of the board’s assessments for all adolescents in the country. This file was then linked to the Israeli National Psychiatric Hospitalization Case Registry, using national identification numbers (equivalent to the US social security number). Before the merged file was returned to the investigators for analysis, in order to preserve confidentiality, the national identification numbers were removed, leaving the participants unidentifiable. From this file, we excluded adolescents who were hospitalized prior or within a year of the draft board assessment and adolescents with missing data on the study variables (gender, SES, and cognitive functioning, n = 162 603, 16.66% of the overall sample), leaving 811 487 adolescents consecutively assessed by the draft board at ages 16–17 years, among whom 1961 (0.2%; the same percentage as those with missing data) had a discharge diagnosis of schizophrenia. There was a follow-up of 1–15 years (mean 5.47 years, SD 3.26 years) between the draft board assessment and psychiatric hospitalization. Fifty-nine point four per cent of the sample was male and 40.6% was female. The average cognitive functioning score was 53.12 (SD = 18.28; range: 10–90). The median SES score was 12 (range: 1–20).
Statistical Analysis
Cross-tabulation and chi-square analyzes were first conducted between SES and hospitalization for schizophrenia. SES was then divided into high (n = 431 743, participants with an SES score equal to or above the median, 53.2% of the sample) and low (n = 381 705, participants with an SES score below the median; 47.0% of the sample). Cognitive functioning was divided into low (1 SD or more below the mean, n = 131 516, 16.21% of the sample), average (between 1 SD above and below the mean, n = 564 175, 69.52% of the sample), and high (1 SD or more above the average, n = 117 757, 14.51% of the sample). This was done to make interpretation of the results more intuitive and to enable the identification of a possible nonlinear relationship between SES, cognitive functioning, and risk of hospitalization for schizophrenia. Cox regressions were conducted (taking into account the time between assessment of cognitive functioning at the draft board and later hospitalization) predicting hospitalization for schizophrenia by SES and by cognitive functioning, while controlling for gender. The proportional hazards assumption was satisfied (examined through the log-minus-log survival plot). Finally, the relationship between cognitive functioning, SES, and risk for schizophrenia was examined by dividing the sample according to cognitive functioning (high, average, and low). Cox regression analyzes assessing risk for hospitalization for schizophrenia were preformed separately for each cognitive level, separated into high and low SES. Cognitive functioning and SES were not entered into the same regression because they are fundamentally associated with one another, hence cannot be examined together as predictors of hospitalization for schizophrenia.29
Results
Association Between SES and Later Hospitalization for Schizophrenia
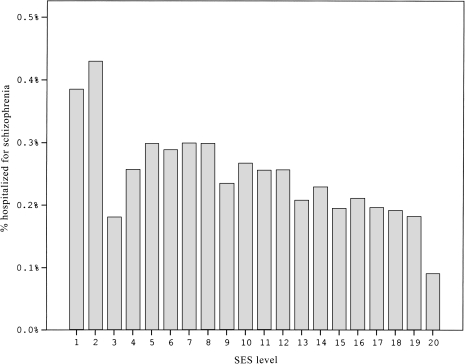
Cross-tabulation between SES and hospitalization for schizophrenia can be seen in figure 1, indicating that there is a slight, though significant, decline in risk with increasing SES (χ2 = 53.925, df = 19, P for trend < .001). Similarly, low SES was associated with significantly higher risk of hospitalization for schizophrenia (HR = 1.193, 95% CI = 1.091–1.303) in comparison with high SES.
Fig. 1.
Percentage of individuals hospitalized for schizophrenia within each socioeconomic status level.
Association Between Cognitive Functioning and Later Hospitalization for Schizophrenia
In comparison with participants with high cognitive functioning, those with low cognitive functioning had almost 5 times the risk of being hospitalized for schizophrenia (HR = 4.98, 95% CI = 4.13–6.00) and those with average cognitive functioning had approximately 2 times the risk of hospitalization (HR = 2.15, 95% CI = 1.80–2.58).
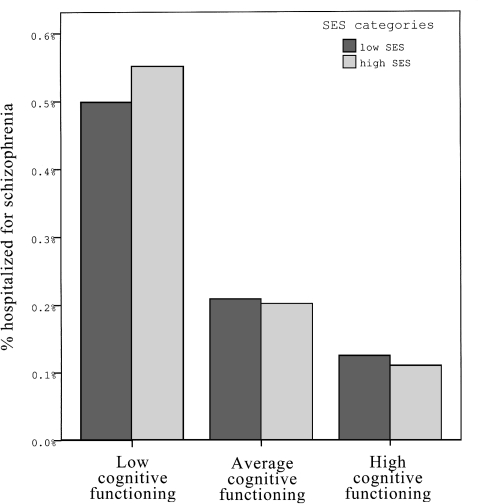
Relationship Between SES, Cognitive Functioning, and Hospitalization for Schizophrenia
Since SES and cognitive functioning are correlated with each other (r = .336, P < .001), additional analyzes were conducted to examine the relationship between SES, cognitive functioning, and risk for hospitalization for schizophrenia. Findings indicated that among individuals with average and high cognitive functioning, SES was not a significant risk factor for hospitalization for schizophrenia (average cognitive functioning: HR = 1.05, 95% CI = 0.93–1.17; high cognitive functioning HR = 0.88, 95% CI = 0.60–1.27). In contrast, among individuals with low cognitive functioning, high SES was significantly associated with hospitalization for schizophrenia (HR = 1.21, 95% CI = 1.03–1.42; figure 2).
Fig. 2.
Percentage of individuals hospitalized for schizophrenia according to socioeconomic status level (divided by median) and cognitive functioning level (divided according to SD, low: below −1 SD, average: −1 to +1 SD, high: above +1 SD).
Discussion
When simply examining the association between SES and schizophrenia, lower SES was found to be associated with greater risk of hospitalization for schizophrenia as has been found in a number of previous studies.3–9 However, this current study shows that the relationship between these 2 variables is influenced by cognitive functioning, and this complexity might be the source of the previous inconsistent findings on this topic. We found a relationship between SES, cognitive functioning, and risk for later schizophrenia: among individuals with high and average cognitive functioning, SES did not influence risk for schizophrenia, whereas among individuals with low cognitive functioning, high SES was found to slightly increase the risk for schizophrenia. One possible explanation for this finding might be that among individuals from low socioeconomic backgrounds, low cognitive functioning may reflect decreased opportunities related to SES, whereas among individuals from high SES backgrounds, low cognitive functioning might reflect greater neuro-developmental problems, influencing later risk for later psychopathology. A finding somewhat similar to these data was reported in a study, which studied risk for suicide and cognitive functioning among inductees into the Swedish army30 and reported that the greatest risk was found among poorly performing offspring of well-educated parents. Similarly, an additional possibility relates to Cognitive Reserve Theory.31 Namely, persons with low cognitive functioning may have low cognitive reserve and the high cognitive demands characteristic of high SES environments may lead to the manifestation of clinical deficits, such as schizophrenia. Another possibility is that among individuals from high SES backgrounds, having low cognitive functioning may lead to social defeat to a greater extent than among individuals from low SES backgrounds because of the greater gap between the individual's abilities and those expected in high SES environments. This possibility has been addressed previously by Selten and Cantor-Graae32 who suggested than social defeat may mediate the association between disadvantage (eg, low IQ, migration, low SES) and higher risk of schizophrenia.
Limitations
One of the limitations of the study is that we were unable to control for parents' mental illness. Namely, among participants' whose parents also have schizophrenia, it is probable that their increased risk for schizophrenia results from genetic factors rather than resulting from parents' low SES. However, as the prevalence of schizophrenia in the population is relatively low, this potential bias is not likely to be the cause of the observed findings.
Furthermore, the diagnosis of psychotic disorders in this study was drawn from a hospitalization case registry. This could be of limited value if a large proportion of individuals with psychosis were never hospitalized. However, data from a different study currently conducted by our group (data not shown) indicates that 93% of patients with schizophrenia are hospitalized at least once during their lifetime. A similar study on nonhospitalized schizophrenics from England33 showed that 93.3% of patients with schizophrenia are eventually hospitalized at least once over their lifetime. In addition, although the registry diagnoses are clinical, not research, diagnoses, they are assigned by board-certified psychiatrists who had the benefit of observing the patients throughout one or more hospitalizations and had been trained and retrained in the use of the diagnostic criteria of the ICD-10 and Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Studies that compared clinical diagnoses of schizophrenia assigned in state hospitals34 with research diagnoses have shown a high degree of concordance, and a previous study by our group comparing registry diagnoses to research diagnostic criteria (RDC) diagnoses found that the sensitivity of the registry diagnosis of nonaffective psychotic disorders was 0.89 and of schizophrenia 0.8735.
In conclusion, low SES was slightly associated with increased risk for later schizophrenia. In persons with poor cognitive functioning, those with high SES had slightly higher risk compared with those with lower SES. A possible explanation for this interesting finding might be that among individuals from low socioeconomic backgrounds, low IQ may reflect decreased opportunities related to SES, whereas among individuals from high SES backgrounds, low IQ might reflect risk for later psychopathology. The results of this study should be interpreted with caution until future studies replicate these reported associations between SES, IQ, and risk for schizophrenia.
Acknowledgments
The Authors have declared that there are no conflicts of interest in relation to the subject of this study.
References
- 1.Eaton W, Harrison G. Life chances, life planning, and schizophrenia: a review and interpretation of research on social deprivation. Int J Ment Health. 2001;30:58–81. [Google Scholar]
- 2.Muntaner C, Eaton WW, Miech R, O'Campo P. Socioeconomic position and major mental disorders. Epidemiol Rev. 2004;26:53–62. doi: 10.1093/epirev/mxh001. [DOI] [PubMed] [Google Scholar]
- 3.Wicks S, Hjern A, Gunnell D, Lewis G, Dalman C. Social adversity in childhood and the risk of developing psychosis: a national cohort study. Am J Psychiatry. 2005;162:1652–1657. doi: 10.1176/appi.ajp.162.9.1652. [DOI] [PubMed] [Google Scholar]
- 4.Turner RJ, Wagenfeld MO. Occupational mobility and schizophrenia: an assessment of the social causation and social selection hypotheses. Am Sociol Rev. 1967;32:104–113. [PubMed] [Google Scholar]
- 5.Corcoran C, Perrin M, Harlap S, et al. Effect of socioeconomic status and parents’ education at birth on risk of schizophrenia in offspring. Soc Psychiatry Psychiatr Epidemiol. 2009;44:265–271. doi: 10.1007/s00127-008-0439-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Werner S, Malaspina D, Rabinowitz J. Socioeconomic status at birth is associated with risk of schizophrenia: population-based multilevel study. Schizophr Bull. 2007;33:1373–1378. doi: 10.1093/schbul/sbm032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Castle DJ, Scott K, Wessely S, Murray RM. Does social deprivation during gestation and early life predispose to later schizophrenia? Soc Psychiatry Psychiatr Epidemiol. 1993;28:1–4. doi: 10.1007/BF00797825. [DOI] [PubMed] [Google Scholar]
- 8.Dauncey K, Giggs J, Baker K, Harrison G. Schizophrenia in Nottingham: lifelong residential mobility of a cohort. Br J Psychiatry. 1993;163:613–619. doi: 10.1192/bjp.163.5.613. [DOI] [PubMed] [Google Scholar]
- 9.Harrison G, Gunnell D, Glazebrook C, Page K, Kwiecinski R. Association between schizophrenia and social inequality at birth: case—control study. Br J Psychiatry. 2001;179:346–350. doi: 10.1192/bjp.179.4.346. [DOI] [PubMed] [Google Scholar]
- 10.Goldberg EM, Morrison SL. Schizophrenia and social class. Br J Psychiatry. 1963;109:785–802. doi: 10.1192/bjp.109.463.785. [DOI] [PubMed] [Google Scholar]
- 11.Grünfeld B, Salvesen C. Functional psychoses and social status. Br J Psychiatry. 1968;114:733–737. doi: 10.1192/bjp.114.511.733. [DOI] [PubMed] [Google Scholar]
- 12.Hare EH, Price JS, Slater E. Parental social class and psychiatric patients. Br J Psychiatry. 1972;121:515–524. doi: 10.1192/bjp.121.5.515. [DOI] [PubMed] [Google Scholar]
- 13.Wiersma D, Giel R, De Jong A, Slooff CJ. Social class and schizophrenia in a Dutch cohort. Psychol Med. 1983;13:141–150. doi: 10.1017/s0033291700050145. [DOI] [PubMed] [Google Scholar]
- 14.Jones P, Rodgers B, Murray R, Marmot M. Child developmental risk factors for adult schizophrenia in the British 1946 birth cohort. Lancet. 1994;344:1398–1402. doi: 10.1016/s0140-6736(94)90569-x. [DOI] [PubMed] [Google Scholar]
- 15.Malama IM, Papaioannou DJ, Kaklamani EP, Katsouyanni KM, Koumantaki IG, Trichopoulos DV. Birth order sibship size and socio-economic factors in risk of schizophrenia in Greece. Br J Psychiatry. 1988;152:482–486. doi: 10.1192/bjp.152.4.482. [DOI] [PubMed] [Google Scholar]
- 16.Mäkikyröa T, Isohanni M, Moring J, et al. Is a child's risk of early onset schizophrenia increased in the highest social class? Schizophr Res. 1997;23:245–252. doi: 10.1016/s0920-9964(96)00119-3. [DOI] [PubMed] [Google Scholar]
- 17.Timms D. Gender, social mobility and psychiatric diagnoses. Soc Sci Med. 1998;46:1235–1247. doi: 10.1016/s0277-9536(97)10052-1. [DOI] [PubMed] [Google Scholar]
- 18.Mulvany F, O'Callaghan E, Takei N, Byrne M, Fearon P, Larkin C. Effect of social class at birth on risk and presentation of schizophrenia: casecontrol study. BMJ. 2001;323:1398–1401. doi: 10.1136/bmj.323.7326.1398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dohrenwend BP, Levav I, Shrout PE, et al. Socioeconomic status and psychiatric disorders: the causation-selection issue. Science. 1992;255:946–952. doi: 10.1126/science.1546291. [DOI] [PubMed] [Google Scholar]
- 20.Byrne M, Agerbo E, Eaton WW, Mortensen PB. Parental socio-economic status and risk of first admission with schizophrenia: a Danish national register based study. Soc Psychiatry Psychiatr Epidemiol. 2004;39:87–96. doi: 10.1007/s00127-004-0715-y. [DOI] [PubMed] [Google Scholar]
- 21.Saraceno B, Levav I, Kohn R. The public mental health significance of research on socio-economic factors in schizophrenia and major depression. World Psychiatry. 2005;4:181–185. [PMC free article] [PubMed] [Google Scholar]
- 22.Burdick K, Gunawardane N, Woodberry K, Malhotra A. The role of general intelligence as an intermediate phenotype for neuropsychiatric disorders. Cognit Neuropsychiatry. 2009;14:299–311. doi: 10.1080/13546800902805347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Davidson M, Reichenberg A, Rabinowitz J, et al. Behavioral and intellectual markers for schizophrenia in apparently healthy male adolescents. Am J Psychiatry. 1999;156:1328–1335. doi: 10.1176/ajp.156.9.1328. [DOI] [PubMed] [Google Scholar]
- 24.Hart SA, Petrill SA, Deater Deckard K, Thompson LA. SES and CHAOS as environmental mediators of cognitive ability: a longitudinal genetic analysis. Intelligence. 2007;35:233–242. doi: 10.1016/j.intell.2006.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Rindermann H, Flores-Mendoza C, Mansur-Alves M. Reciprocal effects between fluid and crystallized intelligence and their dependence on parents' socioeconomic status and education. Learn Individ Differ. 2010;20:544–548. [Google Scholar]
- 26.Reichenberg A, Weiser M, Rabinowitz J, et al. A population-based cohort study of premorbid intellectual, language, and behavioral functioning in patients with schizophrenia, schizoaffective disorder, and nonpsychotic bipolar disorder. Am J Psychiatry. 2002;159:2027–2035. doi: 10.1176/appi.ajp.159.12.2027. [DOI] [PubMed] [Google Scholar]
- 27.Burck L, Feinstein Y. Characterization and Classification of Geographical Units by the Socioeconomic Level of the Population. Jerusalem, Israel: Central Bureau of Statistics; 2000. [Google Scholar]
- 28.Central Bureau of Statistics. Demographic Characteristics of the Population in Localities and Statistical Areas. Jerusalem, Israel: Ministry of the Interior, 1995. [Google Scholar]
- 29.Miller GA, Chapman JP. Misunderstanding analysis of covariance. J Abnorm Psychol. 2001;110:40–48. doi: 10.1037//0021-843x.110.1.40. [DOI] [PubMed] [Google Scholar]
- 30.Gunnell D, Magnusson PKE, Rasmussen F. Low intelligence test scores in 18 year old men and risk of suicide: cohort study. BMJ. 2005;330:167. doi: 10.1136/bmj.38310.473565.8F. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stern Y. What is cognitive reserve? Theory and research application of the reserve concept. J Int Neuropsychol Soc. 2002;8:448–460. [PubMed] [Google Scholar]
- 32.Selten JP, Cantor-Graae E. Social defeat: risk factor for schizophrenia. Br J Psychiatry. 2005;187:101–102. doi: 10.1192/bjp.187.2.101. [DOI] [PubMed] [Google Scholar]
- 33.Geddes JR, Kendell RE. Schizophrenic subjects with no history of admission to hospital. Psychol Med. 1995;25:859–868. doi: 10.1017/s003329170003511x. [DOI] [PubMed] [Google Scholar]
- 34.Pulver AE, Carpenter WT, Adler L, McGrath J. Accuracy of the diagnoses of affective disorders and schizophrenia in public hospitals. Am J Psychiatry. 1988;145:218–220. doi: 10.1176/ajp.145.2.218. [DOI] [PubMed] [Google Scholar]
- 35.Weiser M, Kanyas K, Malaspina D, et al. Sensitivity of ICD-10 diagnosis of psychotic disorders in the Israeli National Hospitalization Registry compared with RDC diagnoses based on SADS-L. Compr Psychiatry. 2005;46:38–42. doi: 10.1016/j.comppsych.2004.07.016. [DOI] [PMC free article] [PubMed] [Google Scholar]