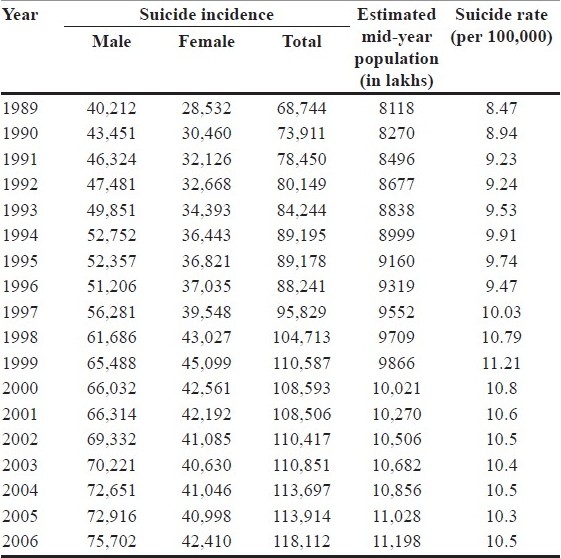
Indian union health ministry estimates state that 1.2 lakh people commit suicide every year in India. Also, over 4 lakh people attempt suicide.On World Suicide Prevention Day 2008, WHO claimed that Japan, China and India might account for about 40% of the world suicides. Most people who commit suicide in India (37.8%) are below 30 years of age. The percentage of suicides committed by those below 44 years is 71% [Figure 1]. Experts opine that 60% of suicides may not have occurred if proper intervention was undertaken. Ministry officials state that majority of those commiting suicide suffer from depression or other emotional disorders. Over 7.5% of Indians are facing some sort of emotional disorder. Out of these, more than 1.75% (16 million) need institutional intervention. Out of every three cases of suicide reported every 15 minutes in India, one is committed by a youth in the age group of 15–29 years. Kerala, the country's first fully literate state, has the highest number of suicides. Some 32 people commit suicide in Kerala every day. In the United States, the overall rate is approximately 20 suicidal deaths per 100,000 persons, which is almost twice as much as the 10.5 reported in India [Table 1].
Figure 1.
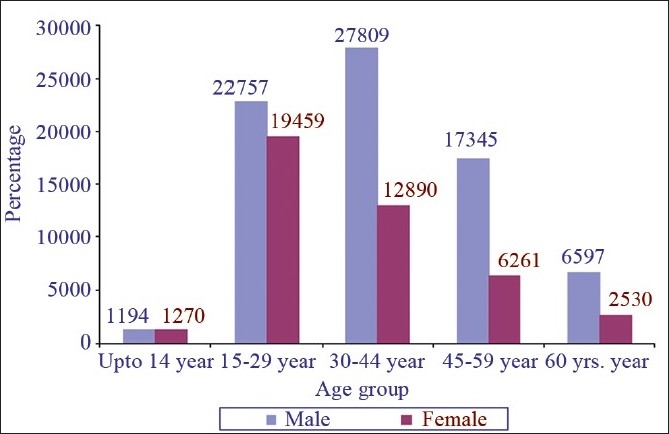
Suicide victims by sex and age-group during 2006
Table 1.
Incidence and rate of suicidal deaths in India (1989–2006)
According to the WHO, every year, almost 1 million people die from suicide, a "global" mortality rate of 16 per 100,000, or one death every 40 seconds. Suicide is among the three leading causes of death among those aged 15–44 years in some countries and the second leading cause of death in the 10–24 years age group; these figures do not include suicide attempts which are up to 20 times more frequent than completed suicide.
Although traditionally, suicide rates have been highest among the male elderly, rates among young people have been increasing to such an extent that they are now the group at highest risk in a third of countries, in both developed and developing countries. Mental disorders (particularly depression and alcohol use disorders) are a major risk factor for suicide in Europe and North America; however, in Asian countries, impulsiveness plays an important role. Suicide is complex with psychological, social, biological, cultural and environmental factors involved.
Although global rates are shown in Figure 2, there are marked differences between individual countries with Belarus and Lithuania topping the list, while India ranks 43rd, thus having a much lower suicide rate than many developed countries [Figure 3]. Within the country, suicide rates vary between 8.1 and 58.3/100,000 population for different parts of India.
Figure 2.
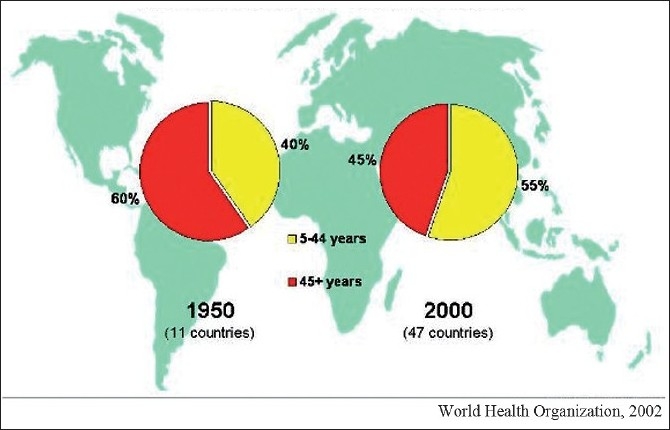
Changes in the age distribution of cases of suicide between 1950 and 2000
Figure 3.
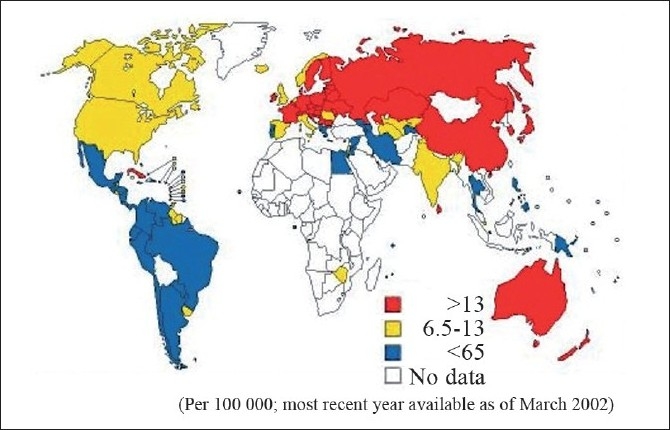
Internationally suicidal rates
S. Mohanty and colleagues found that in India, the largest number of victims were found in the age group of 21–30 years. Majority of the victims were mentally sound, married and were from rural background. Victims were mostly drawn from low socioeconomic status (48%). Less educated or illiterates were usually the victims. Suicidal note was detected in 5% of cases. Suicidal tendency and alcohol intake could not be encountered in most of the cases. Financial burden (37%) and marital disharmony (35%) were some of the main reasons for the suicide.
Andhra Pradesh, the fourth largest state in India, is responsible for more than 11% of these. Unfortunately, most suicides are under-reported and there are scant data on attempted suicides. Using Patient Care Record (PCR) forms of all emergencies serviced by 108 (Emergency Ambulance Service), an analysis of all cases was done in one study which found that a total of 1007 cases were recorded as confirmed suicides in the year 2007. Hanging and insecticide poisoning (72%) were the most common methods used. Males preferred hanging and insecticide poisoning, while females preferred self-immolation and hanging as the common methods. Self-immolation and insecticide poisoning had the highest mortality (41.6%). Estimates of attempted suicides for the year 2008 revealed a mean of 3.2–3.8 per 1000 population for males, 3.3–3.7 per 1000 population for females and 6.4–7.6 per 1000 population combined.
SUICIDE RISK AND MENTAL ILLNESS
All major psychiatric disorders carry an increased risk of suicide. However, 90% of suicides can be traced to depression, linked either to bipolar disorder, major depressive disorder, schizophrenia or personality disorders, particularly borderline personality disorder. Comorbidity of mental disorders increases suicide risk, especially anxiety or panic attacks.
Schizophrenia
The long-term suicide rate for people with schizophrenia was estimated in a recent meta-analysis, which showed that 4.9% of schizophrenics will commit suicide during their lifetimes, usually near the illness onset. Risk factors for suicide among people with schizophrenia include a history of previous suicide attempts, the degree of illness severity, comorbid depression or post-psychotic depression, social isolation, and male gender. The risk is higher for the paranoid subtype of schizophrenia and is highest in the time immediately after discharge from hospital. Command hallucinations, in schizophrenia and psychotic depressions, in which one hears voices telling one to kill oneself, have traditionally been felt to carry particular risk.
Mood disorders
While the lifetime suicide risk for mood disorders in general is around 1%, long-term follow-up studies of people who have been hospitalized for severe depression show a suicide risk of up to 13%. People with severe depression are 20 times more likely and people with bipolar disorder are 15 times more likely to die from suicide than members of the general population. Depressed people with agitation, severe insomnia, anxiety symptoms, and comorbid anxiety disorders are particularly at risk.
Anorexia nervosa has a particularly strong association with suicide; the rate of suicide is 40 times greater than the general population. The lifetime risk of suicide was 18% in one study, and in another study 27% of all deaths related to anorexia nervosa were due to suicide.
Personality disorders
People with a diagnosis of a personality disorder, particularly borderline, antisocial or narcissistic personality disorders, are at a high risk of suicide. In this group, elevated suicide risk is associated with younger age, comorbid drug addiction and major mood disorders, a history of childhood sexual abuse, impulsive and antisocial personality traits, and recent reduction of psychiatric care, such as recent discharge from hospital. While some people with personality disorders may make manipulative or contingent suicide threats, the threat is likely to be non-contingent when the person is silent, passive, withdrawn, hopeless, and making few demands. A tendency toward impulsivity appears to be the common denominator relating suicidal tendencies in personality disorders.
Substance abuse
A history of alcohol abuse and alcohol dependence is common among people who commit suicide, and alcohol intoxication at the time of the suicide attempt is a common pattern.
Medical illnesses
Coexistent medical conditions also increase the risk for suicide. This is particularly so for chronic, painful conditions. Malignant diseases also increase the risk.
METHODS OF SUICIDE
Some of the common methods of committing suicide include:
Bleeding: Wrist cutting
Drowning
Suffocation
Hypothermia
Electrocution
Jumping from a height
Firearms
Hanging
Vehicular impact – rail, traffic collisions, etc.
Poisoning – pesticide, drug overdose, etc.
Immolation
According to the WHO, national studies on suicide indicate that suicidal behavior and, in particular, the preferred suicide method, varies between countries. While numerous factors contribute to the choice of a suicide method, societal patterns of suicide can be understood from basic concepts such as the social acceptability of the method (i.e. culture and tradition) and its availability (i.e. opportunity). Hanging was the predominant method of suicide in most countries.
In India, S. Mohanty and colleagues found that hanging and poisoning constituted the two major modes of suicides (63%).
As might be expected, firearm suicide was the most common method in the United States, but was also prevalent in Argentina, Switzerland and Uruguay, although only men used this method in Switzerland. The use of firearms accounts for 54% of all suicides in America.
Jumping from a height plays an important role in small, predominantly urban societies such as Hong Kong.
In contrast, in rural Latin American countries, Asian countries and also in Portugal, poisoning with pesticides was a major problem. Poisoning with drugs was common in Canada and the United Kingdom.
Violent and highly lethal methods such as firearm suicide and hanging are more frequent among men, whereas women often choose poisoning or drowning, which are less violent and less lethal.
Three methods – hanging, pesticide suicide and firearm suicide – dominate country-specific suicide patterns.
This indicates that hanging is the main suicide method when no other major method is available. The proportion of hangings typically decreases as either pesticide suicide or firearm suicide increases. Readily available poisons and firearms facilitate unplanned suicide acts, which are typical of impulsive suicide. This probably explains why the proportion of firearm suicides in individuals with a background of severe mental illness is distinctly below average.
Each method of suicide has its own particular obstacles. Typically, the greater the obstacles, the lower the acceptability of the method and the greater the proportion of suicides associated with psychosis and other severe mental disorder.
ASSESSMENT OF LETHALITY
There is no single cause for suicide and no two suicides can be understood to result from exactly the same constellation of factors. Therefore, the effectiveness of any measures designed to screen for suicide will depend upon the degree to which causal factors have been identified, the strengths of the causal relationships and suicide, and their prevalence in the specific population.
Three domains related to the lethality of suicidal ideation include predisposing factors, risk factors, and protective factors. Predisposing factors are long-term factors that are variable, while risk factors are the more acute symptoms, stressors, or conditions. Protective factors can increase or decrease a person's risk level.
Some risk factors that may lead the practitioner to believe it is unsafe for a patient to be alone include feelings of hopelessness, a definite suicide plan, a recent suicide attempt, severe depression, psychotic symptoms, a recent discharge from a psychiatric unit, the use of alcohol and/or street drugs, homelessness, or medical illness.
ASSESSMENT OF SUICIDE RISK
A suicide risk assessment requires nonjudgmental, open-ended questions aimed at gaining knowledge and insight into the person's thoughts and feelings. There are many elements to consider such as current suicidal thoughts, intent, plans, history of attempts, family history of suicide, history of violence, intensity of depressive systems, previous or current treatment regimens and response, recent or concurrent life stressors, alcohol and drug abuse patterns, psychotic symptoms, and the person's current living situation and social supports.
Suicidal patients with a history of depression can be categorized into three groups to help better determine lethality and treatment options: patients with suicidal ideation, a plan, and intent to harm themselves; patients with suicidal ideation and a plan, but without intent; and thirdly, patients with suicidal ideation but no plan or intent to harm themselves.
When patients deny suicidal ideation, or endorse suicidal ideation but state that they would not act on it, they should also be asked about deterrents against suicide (e.g., religious beliefs, fear of disapproval, concerns about their legacy if death is by suicide). Further, family members or friends should be asked whether the patient is giving warnings or clues such as giving property away. If a patient reports suicidal ideation with a plan and lethal means are available, hospitalization is required. However, the clinician should not say that hospitalization is necessary to prevent suicide; rather, the patient should be assured that hospitalization is necessary for treatment by trained professionals and that it is hoped the hospitalization will make the patient feel better while providing for their safety.
FORMAL ASSESSMENT OF SUICIDE RISK
While acknowledging that administering a tool to determine suicide risk is the only one aspect of the broader aspect of risk assessment, a number of scales are available.
Suicide Behaviors Questionnaire-Revised (SBQ-R)
The Positive and Negative Suicide Ideation Inventory (PANSI)
Suicidal Behaviors Questionnaire (SBQ)
Beck Scale for Suicide Ideation (BSS)
Risk-Rescue Rating (of Weisman and Worden for Suicide Assessment)
Modified SAD PERSONS Scale of Hockberger and Rothstein
The SAD PERSONS Scale for assessing the risk of suicide
Reasons for Living Scale (long form: 72 items, short form: 48 items)
The Reasons for Living Inventory for Adolescents (RFL-A)
The Reasons for Living Inventory for Young Adults (RFL-YA)
The Suicide Resilience Inventory-25 (SRI-25)
DRUGS AFFECTING SUICIDE RATES
Antidepressants and suicide
The status of antidepressants in suicide is controversial. Several meta-analyses of adult studies on antidepressant use and suicide found no significant difference (neither an increase nor a decrease) in risk of suicide attempt or suicide death in adults exposed to active antidepressants compared with those exposed to placebo. In some studies, antidepressants have been linked with suicide, stating that people on antidepressant have the tendency to commit suicide after 10–14 days of commencement of antidepressant (Healy 2009).
Studies in children and adolescents have shown that antidepressants can increase the suicidal thoughts. However, other studies have shown that the overall risk of attempting suicide goes down after starting the antidepressant medication.
Different findings in pediatric and adult studies are not the only source of complexity and potential confusion. Recent evidence suggests that effects on suicidality may differ across antidepressants. Venlafaxine was the only individual drug for which the increase in risk was statistically significant. Two meta-analyses of adult paroxetine studies suggest an increased risk of suicidal behavior or suicide attempt. One meta-analysis of adult sertraline studies found no increase in risk of suicidal ideation or behavior.
It is unlikely that additional randomized trials will provide a final answer to this question, either for adolescents or for adults. Observational studies may have confounding factors, e.g., the finding by Gibbons and colleagues that counties with higher antidepressant use tend to have lower suicide rates may simply mean that suicide rates are lower in areas with more progressive attitudes toward mental health care. Conversely, the finding by Olfson and colleagues that suicide attempters were more often using antidepressants than non-attempters may simply mean that use of antidepressants is a marker for more severe depression.
Despite these limitations, observational studies can provide some reassurance. The risk of serious suicide attempt during the first 6 months of antidepressant treatment is less than 1 per 1000 for adults and less than 1 in 300 for adolescents. Increasing use of newer antidepressants (compared across time or place) has been accompanied by lower rates of suicide mortality in adolescents and in adults. Average risk of suicide attempt actually declines after starting the antidepressant treatment, but this may reflect the natural history of help-seeking than a protective effect of medication.
Finally, it is likely that effects of antidepressants on suicidal ideation or suicide risk differ across individuals. The Food and Drug Administration requires a warning that antidepressant medications can sometimes cause or increase thoughts of suicide.
Lithium and suicide
Tondo and colleagues reviewed and analyzed 22 studies and found that the data indicate substantially lower suicide risk in patients with bipolar disorders, or in mixed affective disorders in patients who remained on long-term lithium maintenance treatment. Similar differences were also found in the same individual during and after discontinuing treatment. Overall, crude suicide rates during lithium treatment were 5.5 times lower than without such treatment. Despite the lower crude suicide rates with lithium maintenance treatment, these rates still greatly exceeded the average suicide rates reported in international general populations by atleast 10-fold. It is not clear if the lower suicide rates observed with lithium maintenance treatment reflect simply the mood-stabilizing effect of lithium or if other effects also contribute. Relevant associated benefits of lithium treatment include improvements in overall emotional stability, interpersonal relationships and close clinical follow-up, vocational functioning, self-esteem and perhaps reduced comorbid substance abuse.
Clozapine and suicide
According to International Suicide Prevention Trial (InterSePT) (a multicenter, randomized, international 2-year study) clozapine therapy demonstrated to be superior to olanzapine therapy in preventing suicide attempts in patients with schizophrenia and schizoaffective disorder, at high risk for suicide. Use of clozapine in this population should lead to a significant reduction in suicidal behavior.
In contrast, Sernyak and colleagues evaluated clozapine's effect on the rate of death due to suicide and found that while overall death rates of patients exposed to clozapine were lower, there were no significant differences in rates of suicidal or accidental deaths.
FOR FURTHER READING
Mitchell AM, Garand L, Dean D, Panzak G, Taylor M. Suicide Assessment in Hospital Emergency Departments: Implications for Patient Satisfaction and Compliance. Top Emerg Med 2005;27:302-12.
Assessment and Management of People at Risk of Suicide. 2003.
Aursnes I, Tvete IF, Gaasemyr J, Natvig B. Suicide attempts in clinical trials with paroxetine randomised against placebo. BMC Med 2005;3:14.
Bryan CJ, Rudd MD. Advances in the assessment of suicide risk. J Clin Psychol 2006;62:185-200.
Conwell Y, Rotenberg M, Caine ED. Completed suicide at age 50 and over. J Am Geriatr Soc 1990;38:640-4.
Fawcett J. Acute risk factors for suicide: Anxiety severity as a treatment modifiable risk factor. Chapter 4 in Tatarelli et al. (eds) (2007)
Fried LP. Health promotion and disease prevention. In: Hazzard WR, Andres R, Bierman EL, Blass JP, editors. Principles of Geriatric Medicine and Gerontology. New York: McGraw-Hill, Inc; 1990.
Frierson RL, Melikian M, Wadman PC. Principles of suicide risk assessment. How to interview depressed patients and tailor treatment. Postgrad Med 2002;112:65-6.
Gibbons RD, Hur K, Bhaumik DK, Mann JJ. The relationship between antidepressant medication use and rate of suicide. Arch Gen Psychiatry 2005;62:165-72.
Simon GE. How can we know whether antidepressants increase suicide risk? Am J Psychiatry 2006;163:1861-3.
Gunnell D, Saperia J, Ashby D. Selective serotonin reuptake inhibitors (SSRIs) and suicide in adults: meta-analysis of drug company data from placebo controlled, randomised controlled trials submitted to the MHRA's safety review. BMJ 2005;330:385.
Hammad TA, Laughren T, Racoosin J. Suicidality in pediatric patients treated with antidepressant drugs. Arch Gen Psychiatry 2006;63:332-9.
Hammad TA, Laughren TP, Racoosin JA. Suicide rates in short-term randomized controlled trials of newer antidepressants. J Clin Psychopharmacol 2006;26:203-7.
Khan A, Khan S, Kolts R, Brown WA. Suicide rates in clinical trials of SSRIs, other antidepressants, and placebo: analysis of FDA reports. Am J Psychiatry 2003;160:790-2.
Lambert M. Suicide risk assessment and management: focus on personality disorders. Current opinion in psychiatry 16:71-6.
Tondo L, Hennen J, Baldessarini RJ. Lower suicide risk with long-term lithium treatment in major affective illness: a meta-analysis. Acta Psychiatr Scand 2001;104:163-72.
Meltzer HY, Alphs L, Green AI, Altamura AC, Anand R, Bertoldi A, et al. Clozapine treatment for suicidality in schizophrenia: International Suicide Prevention Trial (InterSePT). Arch Gen Psychiatry 2003;60:82-91.
Sernyak MJ, Desai R, Stolar M, Rosenheck R. Impact of clozapine on completed suicide. Am J Psychiatry 2001;158:931-7.
Montross LP, Zisook S, Kasckow J. Suicide among patients with schizophrenia: a consideration of risk and protective factors. Ann Clin Psychiatry 2005;17:173-82.
Olfson M, Marcus SC, Shaffer D. Antidepressant drug therapy and suicide in severely depressed children and adults: A case-control study. Arch Gen Psychiatry 2006;63:865-72
Olfson M, Shaffer D, Marcus SC, Greenberg T. Relationship between antidepressant medication treatment and suicide in adolescents. Arch Gen Psychiatry 2003;60:978-82.
Palmer BA, Pankratz VS, Bostwick JM. The lifetime risk of suicide in schizophrenia: a reexamination. Arch Gen Psychiatry 2005;62:247-53.
Saddichha S, Prasad MN, Saxena MK. Attempted suicides in India: a comprehensive look. Arch Suicide Res 2010;14:56-65.
Federico S. Suicide Explained. A Neuropsychological Approach. 2007.
Simon GE, Savarino J, Operskalski B, Wang PS. Suicide risk during antidepressant treatment. Am J Psychiatry 2006;163:41-7.
Søndergård L, Kvist K, Andersen PK, Kessing LV. Do antidepressants precipitate youth suicide?: a nationwide pharmacoepidemiological study. Eur Child Adolesc Psychiatry 2006;15:232-40.
Vanderburg D, Batzar E, Fogel I, Kremer C. Possibly suiciderelated adverse events in placebo-controlled, short-term studies of sertraline in adult patients. American Psychiatric Association Annual Meeting.
Ajdacic-Gross V, Weiss MG, Ring M, Hepp U, Bopp M, Gutzwiller F, et al. Methods of suicide: international suicide patterns derived from the WHO mortality database. Bull World Health Organ 2008;86:726-32.
WHO SUPRE (Suicide Prevention)


