Abstract
The large and growing number of viral and bacterial pathogens responsible for respiratory infections poses a challenge for laboratories seeking to provide rapid and comprehensive pathogen identification. We evaluated a novel application of the TaqMan low-density array (TLDA) cards for real-time PCR detection of 21 respiratory-pathogen targets. The performance of the TLDA was compared to that of individual real-time PCR (IRTP) assays with the same primers and probes using (i) nucleic acids extracted from the 21 pathogen strains and 66 closely related viruses and bacteria and (ii) 292 clinical respiratory specimens. With spiked samples, TLDA cards were about 10-fold less sensitive than IRTP assays. By using 292 clinical specimens to generate 2,238 paired individual assays, the TLDA card exhibited 89% sensitivity (95% confidence interval [CI], 86 to 92%; range per target, 47 to 100%) and 98% specificity (95% CI, 97 to 99%; range per target, 85 to 100%) overall compared to IRTP assays as the gold standard with a threshold cycle (CT) cutoff of 43. The TLDA card approach offers promise for rapid and simultaneous identification of multiple respiratory pathogens for outbreak investigations and disease surveillance.
INTRODUCTION
Despite the high prevalence of acute respiratory infections (ARI), no etiologic agent is identified in approximately 50% of cases tested in studies of community-acquired pneumonia (CAP) (20). In addition, mounting evidence indicates that bacterial and viral coinfections can play a major role in both CAP and ARI (9–11, 13, 17). Accurate and rapid diagnosis of etiologic agents in respiratory illness can be challenging, particularly during investigations of respiratory disease outbreaks of unknown etiology, when there is an urgent need for identification of a causative pathogen. While viral and bacterial culture, serology, immunoassays, and molecular diagnostics can be employed to detect the presence of coinfections in respiratory illness, these techniques can be both costly and time-consuming. More-efficient diagnostic tools are needed that can provide rapid results for a number of pathogens without compromising sensitivity or specificity.
In recent years, a number of multiple-pathogen detection systems have been developed and evaluated on respiratory clinical specimens. These systems use multiplex PCR assays combined with various detection systems, including mass spectroscopy, bead sorting, dye-labeled probes, and microarray technology (1, 3, 18, 19). One drawback shared by all of the technologies based on multiplex PCR is that each change to existing primers or each addition of new primer pairs and probes necessitates reevaluation of the sensitivity and specificity of the entire tool. As new sequence data and other information on known pathogens become available, specific quantitative PCR (qPCR) primers and probes may need to be altered or added, but revalidation of an entire multiple-pathogen detection assay is difficult and costly. Although not previously applied to infectious-pathogen detection, a novel microfluidic-technology format, the TaqMan low-density array (TLDA) (Life Technologies, Carlsbad, CA), may provide a useful platform for multiple-pathogen detection. TLDA is based on singleplex qPCR assays and has been used extensively in cancer research for multiple gene expression and micro-RNA expression analyses (8, 21, 22).
In this study, we evaluated the TLDA format for rapid and simultaneous singleplex detection of multiple viral and bacterial respiratory pathogens. The advantage of the TLDA platform is that it is a closed system incorporating validated singleplex PCR methodology, which allows the flexibility to add new primers and probes without recalibration of the others already incorporated on the cards. Since the reagents for each assay are preallocated to the reaction wells, this format is easy to use, and the sample needs to be added only once. The TLDA card is designed to run 24 duplicate assays, each providing a real-time semiquantitative readout: one internal positive control (IPC), two nucleic acid quality controls, and 21 pathogen assays. Our evaluation of the TLDA card, developed to detect both DNA and RNA from respiratory viruses and bacteria, includes results from both analytical and clinical evaluations of specificity and sensitivity relative to individual real-time PCR (IRTP) assays.
MATERIALS AND METHODS
Strains and clinical specimens.
All viral and bacterial isolates used in this study were obtained from Centers for Disease Control and Prevention (CDC) collections. Nasopharyngeal/oropharyngeal (NP/OP) swabs (n = 272), lung tissue samples (n = 15), and sputum samples (n = 5) in these specialized collections were obtained through routine surveillance and/or from respiratory illness outbreaks from 1990 to 2009 by the CDC in Atlanta, GA, as well as by the CDC surveillance, research, and outbreak response platform in Nairobi, Kenya (based at the Kenya Medical Research Institute [KEMRI]).
TNA extraction.
Total nucleic acids (TNA) were extracted from viral isolates, bacterial isolates, and specimens (lung tissue or sputum specimens for assays used for Legionella; NP/OP specimens for all others) using the InviMag Bacteria DNA kit (Invitek, Germany) and the KingFisher ML extraction platform (Thermo Scientific, Waltham, MA) using the InviMag Viral settings. Despite the name, the InviMag Bacteria kit extracts both DNA and RNA from both viruses and bacteria (27). The procedure was performed according to the manufacturer's instructions unless otherwise stated. Briefly, 200 μl of viral transport medium (VTM) containing NP swabs was incubated in a lysis buffer that includes a proprietary mix of digestive enzymes for 10 min at 65°C, followed by 10 min at 95°C. Approximately 30 mm3 of lung tissue or 125 mm3 of sputum was lysed in the same lysis buffer, but the incubation at 65°C was increased to overnight. Lysed samples were extracted using the KingFisher ML platform as recommended by the manufacturer with an elution volume of 260 μl (this is a deviation from a standard elution in 120 μl to accommodate the large volume required for performing many IRTPs). The samples were centrifuged for 1 min at maximum speed to collect leftover beads in the bottom of each tube. Isolated TNA were stored at −80°C.
Genomic DNA extraction and quantification.
Genomic DNA, required for genome equivalent calculations, was purified from bacterial isolates using the Qiagen Genomic-tip 20/G according to the manufacturer's instructions (Qiagen, Germany). Approximately 4.5 × 109 bacterial cells were pelleted and lysed in the presence of lysozyme and proteinase K for 30 min at 37°C, followed by 30 min at 50°C. These lysates were loaded onto the equilibrated Qiagen Genomic-tip 20/G. The samples were allowed to run through the column by gravity flow. The captured genomic DNA was washed three times with buffer QC (Qiagen, Germany) and was eluted with 1 ml of buffer QF (Qiagen, Germany) twice. The DNA in the eluate was precipitated with isopropanol and was pelleted by centrifugation at 14,000 × g. The pellet was washed and allowed to dissolve in elution buffer at room temperature overnight with shaking. The DNA was quantified using a NanoDrop spectrophotometer (Thermo Scientific, Wilmington, DE).
IRTP.
All individual real-time PCRs (IRTPs) were performed on the Applied Biosystems 7900HT real-time PCR platform in a 96-well format using the AgPath-ID One-Step kit (Applied Biosystems, Foster City, CA) (28). Each reaction mixture contained 1× reverse transcription-PCR (RT-PCR) buffer, 1× RT-PCR enzyme, 1× primer and probe mix, and 5 μl of TNA in a total volume of 25 μl. Primers and probes for each assay were premixed, aliquoted, and stored at −20°C until use. All master mixes for reactions were prepared and aliquoted into 96-well plates in a clean room to limit the possibility of contamination with the template or PCR products. The template was subsequently added to the prealiquoted master mix in another room. The plates were sealed, centrifuged at 750 × g for 2 min, and placed in the thermal cycler. The following cycling conditions were used for all IRTP applications: 45°C for 10 min, 94°C for 10 min, and 45 cycles of 94°C for 30 s followed by 60°C for 1 min.
TLDA card design.
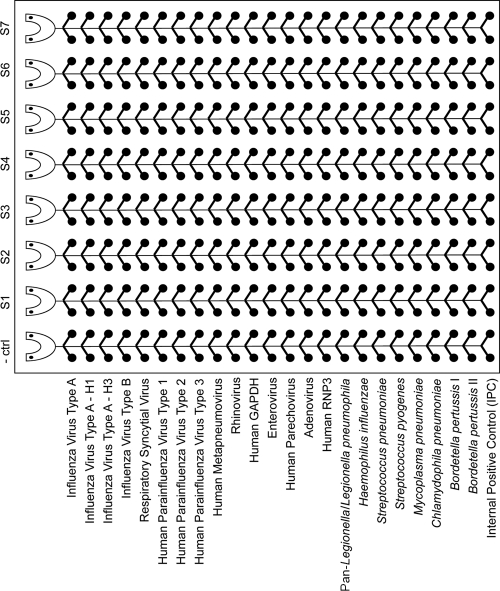
TaqMan low-density array (TLDA) cards (Applied Biosystems, Foster City, CA) are 384-well microfluidic cards with eight ports, each containing 48 connected wells (Fig. 1). The primers and probe for each assay are preloaded and dried onto the designated duplicate wells. All probes used on our card are conjugated to 6-carboxyfluorescein (FAM) except for the Legionella pneumophila probe, which is conjugated to hexachlorofluorescein (HEX). Black hole quencher 1 (BHQ1) was used as a quencher for all probes (28). The TLDA respiratory-pathogen card is designed to run seven samples and a negative-control sample on one card. Alternatively, a positive control can be added to one port, allowing six samples to be run per card. Each port tests against 13 viral targets and 8 bacterial targets in duplicate. All the assays and their respective target genes are listed in Table 1. The card also features three control assays, including the internal positive control (IPC) and two specimen quality control assays, for the glyceraldehyde 3-phosphate dehydrogenase (GAPDH) and RNase P (RNP3) genes.
Fig. 1.
TaqMan low-density array (TLDA) card layout including the respiratory pathogens. TLDA cards were customized to include singleplex real-time PCR assays for 13 viruses and 8 bacteria known to cause acute respiratory infections. These microfluidic cards contain 384 individual wells separated into eight loading ports with 48 assay wells each (− ctrl, negative control; S1 to S7, samples 1 through 7). This format allows for easy loading of eight specimens and for the performance of each assay in duplicate. Upon completion of specimen loading, all wells are sealed individually for singleplex reactions. Each CDC respiratory panel TLDA card has built-in controls, including the internal positive control (IPC) and two human DNA/RNA controls, GAPDH and RNP3, respectively.
Table 1.
Primers and probes used in this study
| Assaya | Target geneb | Primer/probe sequence (5′ to 3′)c | Final concn (nM) | Source or reference |
|---|---|---|---|---|
| Influenza virus type A | M | Biosearch Technologies | ||
| Influenza virus type A subtype H1 | HA | Biosearch Technologies | ||
| Influenza virus type A subtype H3 | HA | Biosearch Technologies | ||
| Influenza virus type B | NS | Biosearch Technologies | ||
| Respiratory syncytial virus | M | F, GGC AAA TAT GGA AAC ATA CGT GAA | 500 | 4 |
| R, TCT TTT TCT AGG ACA TTG TAY TGA ACA G | 250 | |||
| P, FAM-CTG TGT ATG TGG AGC CTT CGT GAA GCT | 50 | |||
| Human parainfluenza virus type 1 | HN | F, AGT TGT CAA TGT CTT AAT TCG TAT CAA T | 500 | Internal, unpublished |
| R, TCG GCA CCT AAG TAA TTT TGA GTT | 500 | |||
| P, FAM-ATA GGC CAA AGA “T”TG TTG TCG AGA CTA TTC CAA | 50 | |||
| Human parainfluenza virus type 2 | HN | F, GCA TTT CCA ATC TAC AGG ACT ATG A | 750 | Internal, unpublished |
| R, ACC TCC TGG TAT AGC AGT GAC TGA AC | 750 | |||
| P, FAM-CCA TTT ACC “T”AA GTG ATG GAA TCA ATC GCA AA | 50 | |||
| Human parainfluenza virus type 3 | HN | F, TGG YTC AAT CTC AAC AAC AAG ATT TAA G | 750 | Internal, unpublished |
| R, TAC CCG AGA AAT ATT ATT TTG CC | 500 | |||
| P, FAM-CCC RTC TG“T” TGG ACC AGG GAT ATA CTA CAA A | 200 | |||
| Human metapneumovirus | F | F, CAA GTG TGA CAT TGC TGA YCT RAA | 600 | Internal, unpublished |
| R, ACT GCC GCA CAA CAT TTA GRA A | 600 | |||
| P, FAM-TGG CYG TYA GCT TCA GTC AAT TCA ACA GA | 100 | |||
| Rhinovirus | 5′ NCR | F, CPA GCC TGC GTG GC | 1,000 | 14 |
| R, GAA ACA CGG ACA CCC AAA GTA | 1,000 | |||
| P, FAM-TCC TCC GGC CCC TGA ATG YGG C | 100 | |||
| Enterovirus | 5′ NTR | F, CCT GAA TGC GGC TAA TCC | 400 | 12 |
| R, TTG TCA CCA TWA GCA GYC A | 400 | |||
| P, FAM-CCG ACT ACT TTG GGW GTC CGT GT | 200 | |||
| Human parechovirus | 5′ NTR | F, GTA ACA SWW GCC TCT GGG SCC AAA AG | 400 | 16 |
| R, GGC CCC WGR TCA GAT CCA YAG T | 400 | |||
| P, FAM-CCT RYG GGT ACC TYC WGG GCA TCC TTC | 200 | |||
| Pan-adenovirus | Hexon | F, GCC CCA GTG GTC TTA CAT GCA CAT C | 500 | 7 |
| R, GCC ACG GTG GGG TTT CTA AAC TT | 500 | |||
| P, FAM-TGC ACC AGA CCC GGG CTC AGG TAC TCC GA | 100 | |||
| Pan-Legionella/Legionella pneumophila | 5S-23S | F, GTA CTA ATT GGC TGA TTG TCT TGA CC | 200 | 26 |
| R, CCT GGC GAT GAC CTA CTT TCG | 400 | |||
| P1, FAM-ATC GTG TAA ACT CTG AC“T” CTT TAC CAA ACC TGT GG | 200 | |||
| P2, HEX-ATC TCG AAC TCA GAA GTG AAA C | 200 | |||
| Haemophilus influenzae | bexA | F, TGC GGT AGT GTT AGA AAA TGG TAT TAT G | 600 | 24 |
| R, GGA CAA ACA TCA CAA GCG GTT A | 600 | |||
| P, FAM-ACA AAG CGT ATC AA“T” ACT ACA ACG AGA CGC AAA AA | 100 | |||
| Streptococcus pneumoniae | lytA | F, ACG CAA TCT AGC AGA TGA AGC A | 500 | 2 |
| R, TCG TGC GTT TTA ATT CCA GCT | 500 | |||
| P, FAM-TGC CGA AAA CGC TTG ATA CAG GGA G | 100 | |||
| Streptococcus pyogenes | spy1258 | F, GCA CTC GCT ACT ATT TCT TAC CTC AA | 300 | CDC, Streptococcus Laboratory Protocolsd |
| R, GTC ACA ATG TCT TGG AAA CCA GTA AT | 300 | |||
| P, FAM-CCG CAA CTC ATC AAG GAT TTC TGT TAC CA | 100 | |||
| Mycoplasma pneumoniae | ATPase | F, AAG AAG CTT ATG GTA CAG GTT GGT TAA | 300 | Internal, unpublished |
| R, TGG AGG TTG GTA GCT AAG TAA GCA | 900 | |||
| P, FAM-TGA CTG GAA GGA “T”GT TAA GCA GGA CAA CAA ATT T | 150 | |||
| Chlamydophila pneumoniae | MOMP | F, GGG CTA TAA AGG CGT TGC TTT | 500 | 15 |
| R, AGA CTT TGT TCC AGT AGC TGT TGC T | 500 | |||
| P, FAM-CCT TGC CAA CAG ACG CTG GCG | 100 | |||
| Bordetella pertussis target I | IS481a | F, CAA GGC CGA ACG CTT CAT | 300 | 23 |
| R, GAG TTC TGG TAG GTG TGA GCG TAA | 300 | |||
| P, FAM-CAG TCG GCC TTG CGT GAG TGG G | 300 | |||
| Bordetella pertussis target II | PtxS1 | F, CGC CAG CTC GTA CTT C | 700 | 23 |
| R, GAT ACG GCC GGC ATT | 700 | |||
| P, FAM-AAT ACG TCG ACA CTT ATG GCG A | 300 |
The rhinovirus, enterovirus, and Mycoplasma pneumoniae assays have been updated and will be replaced on future cards. For the Mycoplasma pneumoniae assay, see reference 25.
NCR, noncoding region; NTR, nontranslated region; MOMP, major outer membrane protein.
F, forward primer; R, reverse primer; P, probe. Quotation marks around a letter indicate an internal quencher. Underlining and boldface indicate a locked nucleic acid.
TLDA card processing.
All TLDA cards were run on the Applied Biosystems 7900HT real-time PCR platform using the AgPath-ID One-Step kit (Applied Biosystems, Foster City, CA). The master mix for each TLDA card was prepared in a clean room, and it included 1× RT-PCR buffer and 1× RT-PCR enzyme in a final volume of 80 μl per port. Twenty microliters of TNA was added to the master mix, resulting in the same primer-probe and template concentrations as those for the IRTPs. Each reaction was mixed by pipetting and was dispensed into loading wells on the TLDA card. The final volume in each TLDA well is approximately 1 μl. The excess volume was necessary for proper loading of small microfluidic ports. Each run included at least one negative control. The cards were centrifuged twice at 336 × g for 1 min each time, sealed, and placed in the thermal cycler. The following cycling conditions were used for all TLDA applications: 45°C for 10 min, 94°C for 10 min, and 45 cycles of 94°C for 30 s followed by 60°C for 1 min.
Analysis of the reproducibility of the TLDA assays.
Samples of total nucleic acids from all bacteria and viruses represented on the card were pooled, aliquoted, and stored at −80°C. One aliquot was loaded into all seven wells of one TLDA card, for a total of 14 separate reactions per target. Finally, additional aliquots of the nucleic acid pool were run on two additional days in either one or two ports per day for a total of five different TLDA cards.
Analytical specificity.
The analytical specificity of the assays was tested in two stages. First, TNA from all viruses and bacteria from the card were loaded into individual wells and were tested for cross-reactivity between the pathogens present on the card. Second, 20-ng portions of TNA from representative isolates of commensal flora and viral pathogens not represented on the card were analyzed for cross-reactivity (see Table 3).
Table 3.
Cross-reactivity panel used to assess the analytical specificity of the TLDA assay
| Organism | Bacterial species | No. of species tested |
|---|---|---|
| Bacterial genera | ||
| Legionellaa | L. lansingensis, L. erythra, L. oakridgensis, L. jordanis, L. wadsworthii, L. maceachernii, L. birminghamensis, L. sainthelensi, L. tucsonensis, L. dumoffii, L. longbeachae, L. bozemanae, L. gormanii, L. micdadei, L. feeleii, L. anisa, L. hackeliae, L. parisiensis, L. rubrilucens, L. nautarum, L. cincinnatiensis, L. worsleiensis, L. shakespearei | 23 |
| Streptococcus | S. pseudopneumoniae, S. agalactiae, S. oralis, S. mitis, S. cristatus, S. gordonii, S. sanguinis, S. parasanguinis, S. vestibularis, S. salivarius, S. peroris, S. australis, S. oligofermentans, S. infantis, S. sinensis, S. dysgalactiae | 16 |
| Chlamydia | C. trachomatis, C. psittaci | 2 |
| Mycoplasma | M. salivarium, M. fermentans, M. orale, M. genitalium | 4 |
| Haemophilus | H. haemolyticus, H. parainfluenzae | 2 |
| Neisseria | N. subflava, N. lactamica | 2 |
| Bordetellab | B. bronchiseptica, B. parapertussis, B. holmesii, B. petrii, B. avium, B. hinzii, B. trematum | 7 |
| Staphylococcus | S. aureus, S. epidermidis | 2 |
| Escherichia | E. coli | 1 |
| Klebsiella | K. pneumoniae | 1 |
| Pseudomonas | P. aeruginosa | 1 |
| Total | 61 | |
| Viruses | ||
| Human herpes simplex virus | 1 | |
| Human parainfluenza virus 4A | 1 | |
| Human coronavirus 229E | 1 | |
| Severe acute respiratory syndrome coronavirus | 1 | |
| MMR vaccinec | 1 | |
| Total | 5 |
The pan-Legionella assay recognized all of the species, as expected. No species other than L. pneumophila cross-reacted with the L. pneumophila assay.
B. parapertussis and B. bronchiseptica were amplified only by the BP2 assay, as expected. B. holmesii was amplified only by the BP1 assay, as expected.
MMR, measles, mumps, and rubella.
Analytical sensitivity.
Two different sets of experiments were performed to test for analytical sensitivity: comparative analytical-sensitivity experiments and comparative limit-of-detection (LOD) experiments. First, a 10-fold serial dilution of the pooled template mixture was performed, and each dilution was aliquoted and frozen at −80°C. Each member of the dilution series was analyzed in quadruplicate using two TLDA cards, and the highest dilution at which at least three out of four replicates tested positive was considered the lowest detectable concentration for that assay. For comparison, the appropriate IRTPs were performed on the serial dilution series in quadruplicate to determine the lowest dilution at which at least three out of four replicates were positive.
The limit of detection was determined for each target by comparing TLDA cards and the corresponding IRTPs. Different methods of determining the lower limit of detection were used for different assays. The 50% egg infectious dose (EID50) per milliliter was used for all influenza assays; quantified transcripts were used for human parechovirus (HPeV) and enterovirus (EV); quantified armored RNA was used for respiratory syncytial virus (RSV), human parainfluenza virus types 1 to 3 (HPIV1 to HPIV3), human metapneumovirus (HMPV), and rhinovirus (RV); and genome equivalents were used for adenovirus and all bacterial assays. Ten-fold serial dilutions of each viral and bacterial strain were analyzed for the lowest detectable concentration range where at least three out of four replicates tested positive. Although this is a relatively low number of replicates for determination of the LOD, the main goal was to compare TLDA and IRTP performance on the same set of dilutions.
Clinical validation.
Samples were processed in groups of seven, and both TLDA cards and IRTPs were run on the same day without a freeze-thaw cycle in between. IRTPs were run in duplicate to match the format of the TLDA cards. A TLDA or IRTP result was considered positive if it passed internal positive controls, had an exponential growth curve, and had at least one run less than or equal to the threshold cycle (CT) cutoff value.
Study design.
The study design was a paired-specimen evaluation where matched results by TLDA and IRTP for a range of 21 pathogens were compared in terms of sensitivity and specificity. Each specimen was tested on a TLDA card for the 21 targets described above using cards manufactured in the same batch. Specimens were handled in “analysis groups” or “collections” of about 30 specimens to accommodate efficient processing, especially of the IRTP assays. From an available collection of 292 specimens, a random sample of 79 specimens was selected for complete paired testing for each of the 21 pathogens by both the TLDA and IRTPs. Additional specimens were selected for testing by both assays. These were any specimens that were positive by TLDA but were not tested by IRTP. Selection of specimens with a positive TLDA result ensured additional data points for analysis. In addition, due to the large number of positive results obtained for Streptococcus pneumoniae by the TLDA, all specimens were analyzed by IRTP assay for S. pneumoniae.
Statistical analysis.
The performance of the TLDA was analyzed for reproducibility and in comparison to IRTP. Reproducibility experiments were performed on four TLDA cards within the same batch to determine if there was a statistically significant difference in results within the seven ports of a card and between cards. The clinical sensitivity and specificity of TLDA were determined by comparison to the IRTP as the “gold standard,” i.e., assuming that the IRTP was 100% sensitive and specific. We performed all clinical sensitivity and specificity analyses using CT cutoffs of 43 and 35.
RESULTS
Reproducibility of the TLDA.
The reproducibility of the CT values within one card or between different cards from the same production lot was based on 828 total observations with a P value of ≤0.0001 by analysis of variance (ANOVA). Within individual pathogens and across four cards, the highest coefficient of variance (CV) was 4.7% (HPeV), the lowest CV was 0.46% (Mycoplasma pneumoniae), and 13/22 (59%) pathogens exhibited CVs under 1% (Table 2). Within individual cards, for a given pathogen, the median CV was 0.51% and the mean was 0.80%. There were only two instances of CVs above 4%, both for HPeV, on cards 3 (6.1%) and 4 (4.1%) (Table 2 and data not shown). Among all four cards and all pathogens, 95% of the within-card and within-pathogen CVs were below 2.91%.
Table 2.
TLDA reproducibility
| Assaya | Within-card reproducibility (n = 14)b |
Reproducibility between cards (n = 22) |
||
|---|---|---|---|---|
| CT | % CV | CT | % CV | |
| Flu A | 21.09 | 0.69 | 21.04 | 1.05 |
| Flu A–H1 | 25.31 | 0.96 | 25.23 | 0.94 |
| Flu A–H3 | 22.88 | 1.52 | 23.02 | 1.83 |
| Flu B | 19.29 | 0.95 | 19.28 | 0.85 |
| RSV | 26.18 | 0.47 | 26.14 | 0.56 |
| HPIV1 | 24.87 | 0.36 | 24.75 | 0.69 |
| HPIV2 | 24.90 | 0.54 | 24.71 | 0.73 |
| HPIV3 | 26.62 | 0.52 | 26.61 | 0.71 |
| HMPV | 25.78 | 0.76 | 25.70 | 1.18 |
| RV | 22.77 | 0.67 | 22.69 | 0.87 |
| EV | 31.23 | 1.78 | 31.47 | 1.95 |
| HPeV | 29.72 | 4.13 | 30.19 | 4.73 |
| Pan-AdV | 21.54 | 0.96 | 21.49 | 1.13 |
| Pan-Legionella | 20.37 | 1.88 | 20.41 | 1.93 |
| L. pneu | 20.54 | 0.93 | 20.45 | 0.97 |
| H. influ | 23.25 | 0.50 | 23.24 | 0.52 |
| S. pneumo | 27.74 | 0.68 | 27.81 | 0.64 |
| S. pyo | 26.03 | 0.82 | 26.20 | 0.88 |
| M. pneumo | 17.55 | 0.34 | 17.49 | 0.46 |
| C. pneumo | 25.59 | 0.60 | 25.47 | 0.67 |
| B. pert I | 23.92 | 1.52 | 23.99 | 1.76 |
| B. pert II | 25.25 | 0.95 | 25.35 | 1.03 |
Flu A, influenza virus type A; Flu A–H1, influenza virus type A subtype H1; RSV, respiratory syncytial virus; HPIV1, human parainfluenza virus type 1; HMPV, human metapneumovirus; RV, rhinovirus; EV, enterovirus; HPeV, human parechovirus; pan-AdV, pan-adenovirus; L. pneu, Legionella pneumophila; H. influ, Haemophilus influenzae; S. pneumo, Streptococcus pneumoniae; S. pyo, Streptococcus pyogenes; M. pneumo, Mycoplasma pneumoniae; C. pneumo, Chlamydophila pneumoniae; B. pert I, Bordetella pertussis target I.
n, number of replicates; CT, threshold cycle; % CV, percent coefficient of variance.
Analytical specificity and sensitivity of the TLDA.
All assays on the TLDA card showed high specificity when testing was performed on bacterial and viral isolates and the near-neighbor panel. By design, some assays detected multiple species or subtypes; these included the influenza virus type A (unpublished data), pan-Legionella/L. pneumophila (26), and Bordetella pertussis assays (23). Specimens positive for influenza virus type A were also further subtyped by the TLDA into H1 or H3. Any influenza virus type A specimens negative for both the H1 and H3 epitopes were characterized as unsubtypeable. The pan-Legionella assay (26) was designed to amplify all Legionella species, and all species listed in Table 3 were amplified, as expected. On the other hand, the Legionella pneumophila (all serogroups) assay was specific for this species, as expected. By design, the B. pertussis target I assay amplified Bordetella pertussis and Bordetella holmesii, while the B. pertussis target II assay amplified B. pertussis, Bordetella parapertussis, and Bordetella bronchiseptica (23). Only one cross-reaction was discovered during the analytical validation: the rhinovirus assay nonspecifically amplified characterized enterovirus type strain TNA on TLDA cards and in the IRTP assays. None of the 61 commensal flora and closely related bacteria and none of the 5 viruses were detected by the TLDA respiratory panel (Table 3).
The LOD was determined for all viruses and bacteria on the TLDA respiratory-panel card and was compared to the LOD for the respective IRTP (Table 4). Highly purified, quantified genomic DNA was used for these experiments. Some assays exhibited the same LOD for the TLDA and the IRTP, including the HPIV2, HMPV, Haemophilus influenzae, B. pertussis target I, and B. pertussis target II assays. Assays that were 10-fold less sensitive by the TLDA included the influenza virus type A, influenza virus type A subtype H1, influenza virus type A subtype H3, influenza virus type B, HPIV1, HPIV3, RV, EV, and HPeV assays, the pan-adenovirus assay tested by adenovirus 11, and the pan-Legionella, L. pneumophila, S. pneumoniae, Streptococcus pyogenes, and M. pneumoniae assays. A few assays exhibited a 100-fold reduction in analytical sensitivity, specifically, the RSV assay, the pan-adenovirus assay tested by adenovirus 15, and the Chlamydophila pneumoniae assay.
Table 4.
Limits of detection of the TLDA and IRTP assays
| Assay and targeta | LOD range |
Unit of measureb | Fold decrease in TLDA LOD | |
|---|---|---|---|---|
| IRTP assay | TLDA | |||
| Flu A | ||||
| Template A | 0.6–6 | 6–60 | EID50/ml (H1) | 10 |
| Template B | 6–60 | 60–600 | EID50/ml (H3) | 10 |
| Flu A–H1 | 0.6–6 | 6–60 | EID50/ml | 10 |
| Flu A–H3 | 6–60 | 60–600 | EID50/ml | 10 |
| Flu B | 0.6–6 | 6–60 | EID50/ml | 10 |
| RSV | 0.6–6 | 60–600 | Transcripts/μl | 100 |
| HPIV1 | 60–600 | 600–6000 | Transcripts/μl | 10 |
| HPIV2 | 6–60 | 6–60 | Transcripts/μl | 1 |
| HPIV3 | 6–60 | 60–600 | Transcripts/μl | 10 |
| HMPV | 600–6000 | 600–6000 | Transcripts/μl | 1 |
| RV | 0.6–6 | 6–60 | Transcripts/μl | 10 |
| EV | 6–60 | 60–600 | Transcripts/μl | 10 |
| HPeV | 0.6–6 | 6–60 | Transcripts/μl | 10 |
| Pan-AdV | ||||
| AV11 | 0.6–6 | 6–60 | GE/μl (AV11) | 10 |
| AV15 | 6–60 | 600–6000 | GE/μl (AV15) | 100 |
| Pan-Legionella spp. | 0.06–0.6 | 0.6–6 | GE/μl | 10 |
| L. pneu | 0.06–0.6 | 0.6–6 | GE/μl | 10 |
| H. influ | 0.6–6 | 0.6–6 | GE/μl | 1 |
| S. pneumo | 0.6–6 | 6–60 | GE/μl | 10 |
| S. pyo | 6–60 | 60–600 | GE/μl | 10 |
| M. pneumo | 0.06–0.6 | 0.6–6 | GE/μl | 10 |
| C. pneumo | 0.04–0.4 | 4–40 | IFU/ml | 100 |
| B. pert I | 6–60 | 6–60 | GE/μl | 1 |
| B. pert II | 6–60 | 6–60 | GE/μl | 1 |
Flu A, influenza virus type A; Flu A–H1, influenza virus type A subtype H1; RSV, respiratory syncytial virus; HPIV1, human parainfluenza virus type 1; HMPV, human metapneumovirus; RV, rhinovirus; EV, enterovirus; HPeV, human parechovirus; pan-AdV, pan-adenovirus; AV11, adenovirus 11; L. pneu, Legionella pneumophila; H. influ, Haemophilus influenzae; S. pneumo, Streptococcus pneumoniae; S. pyo, Streptococcus pyogenes; M. pneumo, Mycoplasma pneumoniae; C. pneumo, Chlamydophila pneumoniae; B. pert I, Bordetella pertussis target I.
EID50, 50% egg infectious dose; GE, genome equivalents; IFU, inclusion-forming units.
Clinical sensitivity and specificity of TLDA.
Clinical validation of the TLDA cards was performed on 292 clinical specimens obtained retrospectively from CDC frozen-specimen collections. Of these, 14 were excluded from the analysis because they gave negative results for both human controls (RNP3 and GAPDH) on the TLDA. Of the remaining 278 samples, all tested positive for at least one pathogen by either the IRTP assay or the TLDA card. Exactly 50% (146/292) of the specimens were positive for more than one pathogen. Forty-two percent (61/146) of these were positive for three or more pathogens. None of the 44 negative controls gave a positive test result for any of the pathogens.
We first analyzed the performance of the TLDA card compared to the IRTP assay as the “gold standard” by using a CT cutoff of 43. This cutoff was chosen as a liberal definition of “positive” and was applied to both the TLDA and IRTP assays. Table 5 shows the number of specimens analyzed for each pathogen and the corresponding sensitivity and specificity of the TLDA card at this CT cutoff. Although the sample sizes for some pathogens were small and confidence intervals were wide, the overall performance of the TLDA card fell within 10% of that of the combined IRTPs. The card was most sensitive for 10 of the 21 pathogens, detecting ≥95% of IRTP-positive influenza virus type A subtype H1, RSV, HPIV1, HPIV3, HMPV, RV, HPeV, pan-adenovirus, H. influenzae, and S. pyogenes samples. The pathogens for which the TLDA card had the lowest sensitivity (≤75%) were M. pneumoniae, C. pneumoniae, and B. pertussis target II. The TLDA card was comparable in specificity to the IRTP assays for most pathogens, ranging from 92 to 100%, except for S. pneumoniae, for which it had a specificity of 85%.
Table 5.
Sensitivity and specificity of TLDA assays compared to individual real-time PCR assays using a CT cutoff of 43
| Targeta | No. of results |
Sensitivity (%) (95% CIb) | Specificity (%) (95% CI) | ||||
|---|---|---|---|---|---|---|---|
| True positive | False positive | False negative | True negative | Total | |||
| Flu A | 22 | 1 | 2 | 77 | 102 | 92 (80–100) | 99 (96–100) |
| Flu A–H1 | 6 | 0 | 0 | 94 | 100 | 100 (100–100) | 100 (100–100) |
| Flu A–H3 | 15 | 1 | 3 | 83 | 102 | 83 (65–100) | 99 (96–100) |
| Flu B | 14 | 0 | 0 | 72 | 86 | 100 (100–100) | 100 (100–100) |
| RSV | 30 | 2 | 0 | 75 | 107 | 100 (100–100) | 97 (94–100) |
| HPIV1 | 7 | 0 | 0 | 74 | 81 | 100 (100–100) | 100 (100–100) |
| HPIV2 | 11 | 2 | 3 | 74 | 90 | 79 (55–100) | 96 (92–100) |
| HPIV3 | 21 | 0 | 1 | 73 | 95 | 95 (86–100) | 100 (100–100) |
| HMPV | 19 | 1 | 1 | 74 | 95 | 95 (85–100) | 99 (96–100) |
| RV | 41 | 6 | 1 | 69 | 117 | 98 (93–100) | 91 (84–97) |
| EV | 13 | 6 | 0 | 73 | 92 | 100 (100–100) | 92 (86–98) |
| HPeV | 1 | 0 | 0 | 79 | 80 | 100 (100–100) | 100 (100–100) |
| Pan-AdV | 28 | 0 | 1 | 81 | 110 | 97 (90–100) | 100 (100–100) |
| Pan-Legionella spp. | 19 | 1 | 6 | 76 | 102 | 77 (60–94) | 99 (96–100) |
| L. pneu | 19 | 1 | 6 | 76 | 102 | 77 (60–94) | 99 (96–100) |
| H. influ | 15 | 3 | 0 | 75 | 93 | 100 (100–100) | 96 (92–100) |
| S. pneumo | 135 | 10 | 11 | 55 | 211 | 92 (88–97) | 85 (76–94) |
| S. pyo | 3 | 0 | 0 | 78 | 81 | 100 (100–100) | 100 (100–100) |
| M. pneumo | 8 | 0 | 9 | 84 | 101 | 50 (25–75) | 100 (100–100) |
| C. pneumo | 16 | 0 | 8 | 78 | 102 | 67 (47–87) | 100 (100–100) |
| B. pert I | 10 | 1 | 0 | 93 | 104 | 100 (100–100) | 99 (97–100) |
| B. pert II | 7 | 0 | 3 | 74 | 84 | 70 (38–100) | 100 (100–100) |
| Total | 460 | 35 | 56 | 1,687 | 2,238 | 89 (86–92) | 98 (97–99) |
Flu A, influenza virus type A; Flu A–H1, influenza virus type A subtype H1; RSV, respiratory syncytial virus; HPIV1, human parainfluenza virus type 1; HMPV, human metapneumovirus; RV, rhinovirus; EV, enterovirus; HPeV, human parechovirus; pan-AdV, pan-adenovirus; L. pneu, Legionella pneumophila; H. influ, Haemophilus influenzae; S. pneumo, Streptococcus pneumoniae; S. pyo, Streptococcus pyogenes; M. pneumo, Mycoplasma pneumoniae; C. pneumo, Chlamydophila pneumoniae; B. pert I, Bordetella pertussis target I.
CI, confidence interval.
For a more conservative definition of a positive result, we lowered the CT cutoff from 43 to 35, which resulted in a small net gain in TLDA card sensitivity without changes in specificity relative to the IRTP assay, although the performance by pathogen differed greatly (data not shown). The TLDA card showed higher sensitivity for eight pathogens, lower sensitivity for nine, and unchanged sensitivity for four at this threshold. The most notable differences with the cutoff of 35 were the M. pneumoniae and C. pneumoniae results, which increased in sensitivity by 33%. The change in the specificity of the TLDA card was less notable, with results differing 0 to 9% from their values at the CT cutoff of 43.
DISCUSSION
Viruses and bacteria are responsible for a large number of community-acquired pneumonia and upper respiratory tract infection cases on a global level, both as independent infections and as coinfections (5, 10, 11, 13). In this study, we evaluated the sensitivity and specificity of the TaqMan low-density array (TLDA) cards for the identification of 21 respiratory-pathogen targets compared to individual real-time PCRs (IRTPs) using the same extraction techniques and the same primers and probes.
The TLDA card format offers several advantages over IRTP. First, it allows for the detection of multiple pathogens simultaneously, thereby eliminating the need to transport, register, aliquot, and process clinical specimens for different pathogens sequentially. This reduces the amount of handling required and the chance for human error. In an outbreak investigation, one laboratory technician can complete the detection of 21 pathogens from multiple patient samples within 3 h, whereas running IRTP assays would take significantly longer. Second, the TLDA card requires a much smaller amount of nucleic acids than an IRTP; more than 210 μl of TNA is required for the detection of 21 pathogens using individual assays in duplicate, but only 20 μl of TNA is needed for the TLDA. This allows for the testing of multiple pathogens even when the available clinical sample is small, obviating the need to choose between suspected pathogens. In addition, the TLDA card offers a singleplex, preformulated panel that helps to avoid extensive assay optimization and to minimize cross-contamination.
In analytical studies, we found that TLDA cards require somewhat higher concentrations of nucleic acids than IRTPs (i.e., 10-fold more RNA or DNA; range, 1 to 1,000), although this difference was not reflected in the detection of most pathogens after evaluation of clinical specimens. One of the limitations of this experiment was a low number of replicates. However, the goal was not validation of individual assays but comparison of TLDA and IRTP performance. We selected four replicates based on available resources. For the same reason, we did not exceed seven 10-fold serial dilutions in comparative LOD determinations; however, more frequent dilutions would have decreased the discrepancy between TLDA and IRTP LODs.
We evaluated TLDA performance on clinical specimens at CT cutoffs of 35 and 43 for both the TLDA and IRTP assays. These cutoffs were chosen to evaluate TLDA performance under both conservative and liberal definitions of positive results and to allow for various specimen concentrations in different samples, such as would occur in a real-world scenario. Under both liberal and conservative conditions, the overall specificity of the TLDA compared to the IRTP was unchanged, while the sensitivity was 4% lower at the CT cutoff of 43. This decrease in sensitivity seen with the TLDA at higher CT levels is consistent with the more sensitive LODs of IRTP assays found in the analytical validation. Concordance with TLDA results improved with a CT cutoff of 35, because specimens that were considered positive with IRTP values between 35 and 43 were recategorized as negative. The TLDA card consistently showed the lowest sensitivity for two pathogens, M. pneumoniae and C. pneumoniae, possibly due to sample quality and the prior dilution status of the clinical specimens available for these specific pathogens, indicated by high CT values for IRTP assays (≥35). The sensitivity of the TLDA for these pathogens increased by 33% when the CT cutoff was lowered to 35.
In total, less than 3% (56/2,238) of assays performed by both the TLDA and IRTP gave false-negative results at a CT cutoff of 43. In a normal outbreak or surveillance setting, clinical specimens would be eluted in a 120-μl or smaller volume; however, in order to perform 48 IRTPs in addition to the TLDA, the samples were eluted in 260 μl for this study. This specimen dilution step may have led to the TLDA missing some clinical specimens that would otherwise have tested positive, which could potentially explain some of the false-negative results on TLDA cards. In this study, we were unable to perform IRTP testing on many specimens for which TLDA results were negative for a given pathogen. The decision to test only a subset of negative results was based on available resources, since complete testing of all specimens would have required performing approximately 7,000 additional IRTP assays. We believe this limitation introduced a minor bias against the IRTP assays.
False-positive TLDA results were seen in less than 1.6% (35/2,238) of TLDA assay reactions at a CT cutoff of 43. One explanation for this may be that each 25-μl IRTP mixture contained the nucleic acid equivalent of 7.5 μl of the original clinical specimen, while each 1-μl TLDA reaction mixture contained only a 0.2-μl nucleic acid equivalent of the original clinical specimen. Forty-five cycles at 94°C may have caused this small reaction volume to evaporate over time, potentially modifying PCR chemistry enough to prevent proper amplification and to introduce nonspecific amplicons.
Another factor that may have impacted the sensitivity and specificity of the TLDA was the need to use a single extraction method, real-time PCR chemistry, and cycling conditions for all reactions. Some pathogens might be detected better using assays optimized under individualized conditions, but we used a method likely to give the best overall results for this combination of RNA and DNA targets. The IRTPs used in this study were run under this unified set of conditions. However, the ability to use the same chemistry for the identification of both viruses and bacteria makes our respiratory-pathogen card possible.
Despite these limitations, our results show that the sensitivity and specificity of the TLDA card are close to those of IRTP assays. These findings suggest that the TLDA card would be a useful tool for pathogen detection, particularly in surveillance and outbreak settings, where results can be interpreted in a broader context than with individual clinical care. As with any multiple-pathogen detection tool, special consideration must be given to situations in which more than one pathogen has a positive result, and clinical judgment is important for distinguishing between carriage and disease. More experience with the assay is essential to determine if the level of detection is appropriate for clinical care. The TLDA card is an efficient tool for rapid screening of many respiratory pathogens when the etiology of respiratory disease is not known or multiple pathogens are suspected, which gives it an advantage over most currently used diagnostics. Further evaluation of the TLDA is needed to assess its performance in a clinical context, including distinguishing between carriage and disease and determining whether the level of detection is appropriate for clinical care. Multiple pathogens were frequently detected using TLDA technology. It is not clear whether all these multiple pathogens were responsible for the patients' illnesses. It is likely that carriage is responsible for the presence of some multiple pathogens. For example, S. pneumoniae carriage is commonly detected in nasopharyngeal swabs and may be present in as many as 50% of some populations (6). One of the challenges of utilizing the TLDA technology will be to develop algorithms to determine which pathogens are primarily responsible for disease, which pathogens can work synergistically to produce disease, and which pathogens represent carriage. TLDA cards could have useful applications to various syndromes beyond respiratory infections, such as diarrhea, sepsis, and meningitis/encephalitis, where a variety of pathogens could be causing similar symptoms.
ACKNOWLEDGMENT
The findings and the conclusions in this report are those of the authors and do not necessarily represent the official position of the Centers for Disease Control and Prevention.
Footnotes
Published ahead of print on 6 April 2011.
REFERENCES
- 1. Briese T., et al. 2005. Diagnostic system for rapid and sensitive differential detection of pathogens. Emerg. Infect. Dis. 11:310–313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Carvalho M. D. G. S., et al. 2007. Evaluation and improvement of real-time PCR assays targeting lytA, ply, and psaA genes for detection of pneumococcal DNA. J. Clin. Microbiol. 45:2460–2466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Dominguez S. R., et al. 2008. Multiplex MassTag-PCR for respiratory pathogens in pediatric nasopharyngeal washes negative by conventional diagnostic testing shows a high prevalence of viruses belonging to a newly recognized rhinovirus clade. J. Clin. Virol. 43:219–222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Fry A. M., et al. 2010. The burden of hospitalized lower respiratory tract infection due to respiratory syncytial virus in rural Thailand. PLoS One 5:e15098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Hamano-Hasegawa K., et al. 2008. Comprehensive detection of causative pathogens using real-time PCR to diagnose pediatric community-acquired pneumonia. J. Infect. Chemother. 14:424–432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Hammitt L. L., et al. 2006. Indirect effect of conjugate vaccine on adult carriage of Streptococcus pneumoniae: an explanation of trends in invasive pneumococcal disease. J. Infect. Dis. 193:1487–1494 [DOI] [PubMed] [Google Scholar]
- 7. Heim A., Ebnet C., Harste G., Pring-Akerblom P. 2003. Rapid and quantitative detection of human adenovirus DNA by real-time PCR. J. Med. Virol. 70:228–239 [DOI] [PubMed] [Google Scholar]
- 8. Hui A. B., et al. 2009. Robust global micro-RNA profiling with formalin-fixed paraffin-embedded breast cancer tissues. Lab. Invest. 89:597–606 [DOI] [PubMed] [Google Scholar]
- 9. Jacoby P., et al. 2007. Modelling the co-occurrence of Streptococcus pneumoniae with other bacterial and viral pathogens in the upper respiratory tract. Vaccine 25:2458–2464 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Johansson N., Kalin M., Tiveljung-Lindell A., Giske C. G., Hedlund J. 2010. Etiology of community-acquired pneumonia: increased microbiological yield with new diagnostic methods. Clin. Infect. Dis. 50:202–209 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Johnstone J., Majumdar S. R., Fox J. D., Marrie T. J. 2008. Viral infection in adults hospitalized with community-acquired pneumonia: prevalence, pathogens, and presentation. Chest 134:1141–1148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kilpatrick D. R., et al. 2009. Rapid group-, serotype-, and vaccine strain-specific identification of poliovirus isolates by real-time reverse transcription-PCR using degenerate primers and probes containing deoxyinosine residues. J. Clin. Microbiol. 47:1939–1941 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kleemola M., et al. 2006. Is there any specific association between respiratory viruses and bacteria in acute otitis media of young children? J. Infect. 52:181–187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Lu X., et al. 2008. Real-time reverse transcription-PCR assay for comprehensive detection of human rhinoviruses. J. Clin. Microbiol. 46:533–539 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Mitchell S. L., Budhiraja S., Thurman K. A., Lanier Thacker W., Winchell J. M. 2009. Evaluation of two real-time PCR chemistries for the detection of Chlamydophila pneumoniae in clinical specimens. Mol. Cell. Probes 23:309–311 [DOI] [PubMed] [Google Scholar]
- 16. Nix W. A., et al. 2008. Detection of all known parechoviruses by real-time PCR. J. Clin. Microbiol. 46:2519–2524 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Oosterheert J. J., et al. 2005. Impact of rapid detection of viral and atypical bacterial pathogens by real-time polymerase chain reaction for patients with lower respiratory tract infection. Clin. Infect. Dis. 41:1438–1444 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Pabbaraju K., Tokaryk K. L., Wong S., Fox J. D. 2008. Comparison of the Luminex xTAG respiratory viral panel with in-house nucleic acid amplification tests for diagnosis of respiratory virus infections. J. Clin. Microbiol. 46:3056–3062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Reijans M., et al. 2008. RespiFinder: a new multiparameter test to differentially identify fifteen respiratory viruses. J. Clin. Microbiol. 46:1232–1240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Reimer L. G., Carroll K. C. 1998. Role of the microbiology laboratory in the diagnosis of lower respiratory tract infections. Clin. Infect. Dis. 26:742–748 [DOI] [PubMed] [Google Scholar]
- 21. Sánchez-Espiridión B., et al. 2009. A TaqMan low-density array to predict outcome in advanced Hodgkin's lymphoma using paraffin-embedded samples. Clin. Cancer Res. 15:1367–1375 [DOI] [PubMed] [Google Scholar]
- 22. Steg A., et al. 2006. Multiple gene expression analyses in paraffin-embedded tissues by TaqMan low-density array: application to hedgehog and Wnt pathway analysis in ovarian endometrioid adenocarcinoma. J. Mol. Diagn. 8:76–83 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Tatti K. M., et al. 2008. Development and evaluation of dual-target real-time polymerase chain reaction assays to detect Bordetella spp. Diagn. Microbiol. Infect. Dis. 61:264–272 [DOI] [PubMed] [Google Scholar]
- 24. Wang X., et al. 2011. Detection of bacterial pathogens in Mongolia meningitis surveillance with a new real-time PCR assay to detect Haemophilus influenzae. Int. J. Med. Microbiol. 301:303–309 [DOI] [PubMed] [Google Scholar]
- 25. Winchell J. M., Thurman K. A., Mitchell S. L., Thacker W. L., Fields B. S. 2008. Evaluation of three real-time PCR assays for detection of Mycoplasma pneumoniae in an outbreak investigation. J. Clin. Microbiol. 46:3116–3118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Yang G., et al. 2010. Dual detection of Legionella pneumophila and Legionella species by real-time PCR targeting the 23S–5S rRNA gene spacer region. Clin. Microbiol. Infect. 16:255–261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Yang G., et al. 2011. Comparison of commercial systems for extraction of nucleic acids from DNA/RNA respiratory pathogens. J. Virol. Methods 171:195–199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Yang G. P., Erdman D. D., Tondella M. L., Fields B. S. 2009. Evaluation of tetramethylrhodamine and black hole quencher 1 labeled probes and five commercial amplification mixes in TaqMan real-time RT-PCR assays for respiratory pathogens. J. Virol. Methods 162:288–290 [DOI] [PubMed] [Google Scholar]