Abstract
Despite progress in our understanding of the growth factors that support the progressive maturation of the various cell lineages of the hematopoietic system, less is known about factors that govern the self-renewal of hematopoietic stem and progenitor cells (HSPCs), and our ability to expand human HSPC numbers ex vivo remains limited. Interest in stem cell expansion has been heightened by the increasing importance of HSCs in the treatment of both malignant and nonmalignant diseases, as well as their use in gene therapy. To date, most attempts to ex vivo expand HSPCs have used hematopoietic growth factors but have not achieved clinically relevant effects. More recent approaches, including our studies in which activation of the Notch signaling pathway has enabled a clinically relevant ex vivo expansion of HSPCs, have led to renewed interest in this arena. Here we briefly review early attempts at ex vivo expansion by cytokine stimulation followed by an examination of our studies investigating the role of Notch signaling in HSPC self-renewal. We will also review other recently developed approaches for ex vivo expansion, primarily focused on the more extensively studied cord blood–derived stem cell. Finally, we discuss some of the challenges still facing this field.
Introduction
The hierarchical development of the hematopoietic system has become progressively better understood over the past few decades, aided in part by significant advances in identifying and isolating hematopoietic stem cells (HSCs) and their progeny.1 Although advances have been made in understanding the hematopoietic growth factors that support the progressive maturation of the various cell lineages, less is known about factors that govern the self-renewal of hematopoietic stem cells and multipotent progenitor cells (MPPs) that consist of short-term repopulating stem cells and give rise to the different cell lineages, thereby impacting the ability to expand HSC and MPP (hematopoietic stem and progenitor cell [HSPC]) numbers ex vivo. Initial attempts at ex vivo expansion of HSCs focused on the use of soluble cytokines known to support lineage committed cells with the expectation that some of these factors also supported HSC proliferation.2 These studies were based on the belief that cell lineage determination was a stochastic process combined with positive and negative cytokine-mediated regulatory responses controlling survival and expansion of the stem cell population.3 More recently, recognition of factors critical for embryologic development as well as discovery of other novel pathways that may influence HSC self-renewal have led to renewed interest in ex vivo expansion, which has been heightened by the increasing importance of HSPCs in the treatment of both malignant and nonmalignant diseases as well as their use in gene therapy.
To date, most attempts to expand HSPC ex vivo for enhanced in vivo engraftment in patients have been clinically unsuccessful because of generation of insufficient cell numbers or improper differentiation of the HSPC starting cell population. However, more recent approaches, including our studies using activation of endogenous Notch signaling, have enabled clinically relevant ex vivo expansion of HSPC. Here, we briefly review early attempts at ex vivo expansion by cytokine stimulation followed by a more in-depth examination of our studies investigating the role of Notch signaling in HSPC self-renewal. We also review other recent approaches under investigation and will discuss opportunities and challenges facing this field.
This review focuses on cord blood (CB) expansion, as these attempts have generally been more successful than those with adult bone marrow (BM) or mobilized peripheral blood stem cells (mPBSCs),4 perhaps related to biologic properties inherent to CB HSPCs.5 In addition, CB is an increasingly utilized source of HSCs for hematopoietic cell transplantation (HCT), primarily because of its ready availability and suitability for recipients, especially minority and mixed-race individuals, who cannot identify other HLA-matched marrow or mPBSC donors. However, the limiting cell doses provided in a single CB unit have been associated with delayed hematopoietic recovery of both neutrophils and platelets. One approach to this limited cell number problem has been the use of double cord blood transplantation (dCBT), which has improved the rate of sustained donor engraftment but has not significantly impacted the time to neutrophil recovery, with median recovery time remaining between 3 and 4 weeks.6 Furthermore, delayed neutrophil engraftment has been associated with early transplantation-related mortality primarily from infection, supporting the need for infusion of greater numbers of progenitor cells capable of providing rapid neutrophil recovery, at least transiently, for protection against posttransplantation infectious complications.7 For these reasons, there has been renewed interest in the adequate generation and clinical application of expanded CB HSPCs.
Initial expansion attempts
Preclinical studies with human BM-, mPBSC-, or CB-derived HSCs cultured with various cytokine combinations have been only moderately successful with significant expansions of committed myeloid progenitor cells but only 2- to 5-fold net increase in long-term repopulating cells after 4 to 21 days in culture.8–11 With the expectation that these committed progenitor cells would enhance absolute neutrophil count (ANC) recovery, cytokine-mediated ex vivo expansion methods have been translated to the clinic for autologous and allogeneic uses. Initial clinical trials used mPBSC- or BM-derived autologous CD34+ cells cultured ex vivo with various cytokine cocktails for 10-14 days followed by infusion of these cell products following high-dose chemotherapy. Importantly, these trials demonstrated safety of this approach but achieved either modest or no effect on time to neutrophil recovery.12–15
In a trial of cord blood transplantation (CBT) in individuals with hematologic malignancies undergoing high-dose preparative regimens, Shpall and colleagues used a 3-cytokine cocktail (stem cell factor [SCF], thrombopoietin [TPO], G-CSF) to expand a portion of single CB units where the nonmanipulated fraction was infused on day 0 and the remaining fraction was infused on day 10 of expansion.16 Although modest progenitor cell expansion (4-fold median) was achieved and no toxicities were observed, the time to neutrophil engraftment was not reduced compared with historic controls.16 On the basis of the favorable safety and feasibility data demonstrated in this trial, a dCBT randomized trial is now currently under way in which patients are randomized to receive either 2 nonmanipulated CB units or 1 nonmanipulated unit and 1 unit expanded ex vivo.17 Although interim analysis shows no significant difference in time to neutrophil engraftment overall, an effect was seen in a subset of patients who received reduced-intensity conditioning (median time to neutrophil engraftment of 7 days vs 14 days).17 Similarly, Jaroscak and colleagues cultured a portion of a single CB unit for 12 days using the Aastrom Replicell bioreactor in the presence of cytokines but failed to achieve an improvement in neutrophil or platelet engraftment.18
The above studies demonstrate that cytokine-mediated expansion methods are safe but generate only moderate increases in progenitor cell numbers with at best modest improvements in clinically relevant outcomes such as time to neutrophil recovery. These results also indicate that ex vivo enumeration of progenitor cell expansion is not predictive of in vivo behavior and that in vivo studies such as repopulating assays in immunodeficient mice are important for preclinical assessment. Furthermore, this lack of clinical success has led to a paradigm shift in current approaches to ex vivo expansion to target molecular pathways involved in stem cell self-renewal, including those that play fundamental roles in governing cell-fate decisions throughout development. Our work with the Notch signaling system is an example of one such approach.
Notch-mediated expansion and clinical translation
In the early 1990s we postulated that, as in other developing systems, hematopoietic stem cell–fate specification resulted from intercellular interactions with adjacent cells and was modulated by several families of molecules, including the Notch gene family.19 At that time, the Notch pathway was particularly well studied in invertebrate systems with clear evidence that Notch played an important role in mediating intercellular interactions affecting cell-fate decisions within the CNS, eye, mesoderm, and ovaries.20,21 In mammals, 4 Notch receptor homologs (Notch 1-4) and 5 ligands (Jagged 1 and 2 and Delta 1,3, and 4) have now been identified.22 Notch signaling is activated as a result of binding of the receptor extracellular domain (ECD) to ligand expressed by adjacent cells. This renders the receptor susceptible to a series of proteolytic cleavage events as a result of conformational changes in or removal of the ECD, which protect the transmembrane/intracellular domain (ICD) from proteolytic cleavage. This cleavage leads, in turn, to release of the constitutively active ICD of Notch, which traffics to the nucleus where it binds directly to the transcription factor CSL (CBF1/RBPJκ), converting it from a transcriptional repressor to a transcriptional activator.23 This binding results in expression of a broad group of target genes, including the transcriptional repressors HES1 and HES5, which are able to inhibit expression of genes required for B-cell and myeloid differentiation.24,25 Differential activation of Notch target genes results from selective activation of the different Notch receptors as a result of specific ligand interactions, leading to different cellular outcomes. For example, activation of Notch1 by Delta ligands 1 and 4 is required for inducing T-cell and inhibiting B-cell differentiation, whereas Notch2 activation by Jagged1 and possibly Delta1 is sufficient to induce effects on HSPCs.26–28
Initial studies to determine whether Notch was expressed in human hematopoietic precursors and might similarly play a role in HSC cell fate determination revealed the presence of at least one Notch homolog in the CD34+lineage-negative bone marrow cell population known to be enriched for hematopoietic precursors.29 This receptor, now termed Notch1, was determined identical to one cloned by Ellisen et al that was involved in a translocation associated with T-cell leukemia.30 Further studies demonstrated that overexpression in HSCs of the truncated form of this receptor inhibited B-cell differentiation while promoting T-cell differentiation and inducing T-cell leukemia.31,32 Although loss-of-function approaches failed to show an effect on the hematopoietic stem cell in adult mouse models,26,33,34 we postulated that masking of the Notch-mediated effects on HSCs occurred because of compensatory mechanisms in vivo such as those mediated by cytokines. To test this hypothesis, we used a retrovirus to express the constitutively active ICD of Notch1 in primary murine HSCs that were then cultured ex vivo. This led to the emergence of an immortalized pluripotent cytokine-dependent cell line capable of both lymphoid and myeloid repopulation in vivo, thereby demonstrating a role for Notch in HSPC self-renewal.35 Although at the time a biologic function for Notch in HSPCs was not determined, this work suggested that manipulation of the Notch signaling pathway ex vivo in primary HSCs could prove to be a novel approach for expanding HSPCs. Moreover, recent studies have helped elucidate a biologic function for Notch in hematopoiesis, where Notch2 signaling delays differentiation and enhances generation of HSPCs during marrow reconstitution (Figure 1).28
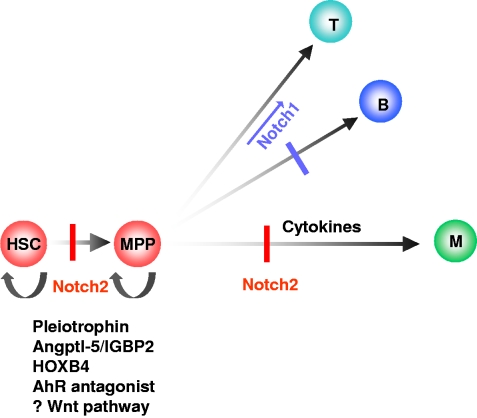
Figure 1.
Model of HSPC self-renewal and differentiation. Notch2 affects HSPC self-renewal by blocking differentiation into multipotent progenitors (MPP) and myeloid/monocytic (M) cell lineage. Notch1 promotes T-cell (T) differentiation versus B-cell (B) differentiation. Also illustrated are molecules with proposed roles in HSPC self-renewal and expansion. Factors with proposed anti-apoptotic and enhanced homing/in vivo survival effects (eg, PGE2) on HSPCs are not shown.
To avoid the potential safety concerns of retroviral transduction, we chose an approach activating endogenous Notch signaling in HSPCs during culture. We engineered Notch ligands consisting of the ECD of the Notch ligands Jagged1 and Delta1 for this purpose.36–38 Notch ligands activate their receptors by physically pulling on the ECD in vivo; thus immobilization of the ligand proved necessary to activate endogenous Notch signaling in vitro.36 Using an immobilized form of the Notch ligand Delta1, we were able to sufficiently activate endogenous receptors and induce expansion of murine stem progenitor cells capable of in vivo reconstitution similar to that seen in the retroviral-mediated Notch overexpression experiments.38 In fact, culture of murine hematopoietic precursors with the immobilized ligand Delta1 and cytokines (SCF, IL-6, IL-11, Flt-3 ligand) resulted in a several-log increase in progenitors capable of short-term lymphoid and myeloid repopulation.38,39 Although these expanded cells appeared limited to short-term and not long-term repopulating stem cells, it is possible that dilution of the HSC population occurred with the extensive expansion.
Given the clinical need for large numbers of hematopoietic progenitor cells capable of providing rapid myeloid recovery in vivo, especially in patients undergoing CBT, we extended our ex vivo expansion approach to human HSPCs, where we noted a response of CB HSPCs to Notch ligands.40,41 With further optimization, we found that incubation of CD34+ CB HSPCs with the immobilized ligand Delta1 combined with fibronectin fragments and cytokines (SCF, TPO, Flt3 ligand, IL-3, IL-6) led to a 222-fold increase in the number of CD34+ cells after 17 days in culture compared with input cell number. Furthermore, we demonstrated a nearly 16-fold increase in NOD/SCID mouse repopulating cell frequency when cultured on Delta ligand compared with uncultured cells.42 The ability of these human cells to rapidly reconstitute the myeloid compartment in immunodeficient mice indicated their potential clinical utility. In contrast to our studies using primary murine HSPCs, in vivo persistence of transplanted cells at 9 weeks and secondary transplantation studies suggested the presence of both long-term and short-term repopulating cells following culture of human CB progenitor cells on Delta ligand.
A key aspect of these studies was determination of whether the magnitude of Notch signaling played a role in the optimal generation of repopulating cells. Murine studies found that the relatively lower amount of Notch signaling induced in cells cultured with lower densities of Delta1 led to self-renewal of progenitors with primarily B-lymphoid and myeloid potential, whereas higher amounts of Notch signaling inhibited B-cell differentiation and promoted differentiation toward the T-cell lineage.43 Concurrent studies with human CB also revealed important ligand dose-dependent effects whereby relatively lower densities of immobilized ligand substantially enhanced generation of NOD/SCID repopulating cells, whereas higher ligand densities promoted differentiation toward the T-cell lineage at the expense of repopulating cells.41 This in vitro requirement for different strengths of Notch signaling presumably reflects selective in vivo usage of specific Notch receptor homologs with differing transcriptional activating strengths. For example, Notch2, which promotes HSPC self-renewal, may be a less potent transcriptional activator than Notch1, which is required for T-cell differentiation.28
On the basis of these promising preclinical studies, this methodology using an engineered Notch ligand for the ex vivo generation of increased numbers of CD34+ cells is now under clinical investigation. In an ongoing phase 1 clinical trial, patients undergoing a myeloablative CBT are receiving one nonmanipulated CB unit along with a second CB unit that has undergone Notch-mediated ex vivo expansion.42 In the first 10 patients enrolled on this trial, an average of 6 × 106 CD34+ cells/kg resulting from an average 164-fold expansion of isolated CD34+ cells were co-infused with an average 2.4 × 105 CD34+cells/kg from a second nonmanipulated unit. These cells were safely infused and led to a significant reduction in the time to neutrophil engraftment. A median time to absolute neutrophil count (ANC) ≥ 500/μL of 16 days was observed in those receiving the expanded unit compared with 26 days in a concurrent cohort of 20 patients receiving dCBT with the same conditioning and posttransplantation immunosuppressive regimen. We also demonstrated a statistically significant improvement in median time to achieve an ANC > 100 cells/μL (9 vs 19 days), a potentially important metric based on its association with improved survival after allogeneic stem cell transplantation.44 In addition, comparable overall survival and GVHD risk to those receiving nonmanipulated CB grafts was observed, with an average follow-up of 354 days. In addition, acute grade 2 GVHD was observed in all evaluable patients with the exception of acute grade 3 GVHD in one. Additionally, chronic extensive GVHD has not been observed, although 3 patients have been diagnosed with chronic limited GVHD.42 Furthermore, preliminary evaluation of time to platelet engraftment compared favorably in those receiving the expanded cell product compared with recipients of double nonmanipulated CB grafts (C.D., I.D.B., unpublished data, December 28, 2010). Interestingly, whereas peripheral blood leukocytes at 7 days were derived from the expanded units in all patients, at the time of achieving early engraftment with an ANC ≥ 500/μL only half of the patients demonstrated predominant engraftment with the expanded CB unit while the other half had engraftment derived from the nonmanipulated unit, suggesting that the expanded unit may have facilitated engraftment by the nonmanipulated unit.42
In contrast with our murine stem cell studies, it is encouraging that 2 of the 10 patients demonstrated persistence of the expanded graft 180 days after transplantation, suggesting maintenance of some longer-term repopulating progenitor cells despite ex vivo expansion. It remains unclear whether the lack of long-term engraftment from the expanded unit in the other 8 patients represents loss of stem cell self-renewal capacity after in vitro culture or is indicative of immune-mediated rejection of the expanded unit (which is devoid of T cells) in vivo. In fact, our studies have also demonstrated T cell–mediated effects to be responsible for rejection of one of two infused CB units in conventional dCBT.45 Thus it was surprising that in vivo persistence of cells derived from the expanded unit survived longer term in the 2 patients as we anticipated eventual rejection of the expanded cell graft by the T cell–containing, nonmanipulated unit. Although these preliminary studies of Notch-mediated expansion of CB repopulating cells point to the promise of expanding stem cells to achieve clinically relevant effects, phase 2 and 3 trials will be necessary to evaluate whether co-infusion of this expanded cell product decreases the occurrence of serious infection, improves survival, or affects duration of hospital stay in recipients of CB grafts.
Other emerging approaches to ex vivo expansion
We expect that our studies will be the first of many successful approaches for HSPC expansion. There are currently numerous approaches under investigation that include ones based on culture with stromal elements to provide a “niche” for stem cell self-renewal or have targeted defined molecules to achieve ex vivo expansion. In the following sections we will review multiple different approaches, beginning with those in early clinical trials followed by those with clear preclinical evidence for HSC expansion and concluding with potential future targets for expansion based on promising murine data. Direct comparisons of the multiple preclinical approaches, however, are difficult, in particular because critical data on ex vivo expansion of repopulating cells are often insufficiently quantified. However, where available, we have highlighted in vivo repopulating assay results, as these are currently the best available surrogate for possible future clinical utility.
Approaches in early clinical trials
Stromal cell–based culture
The hematopoietic microenvironment comprises HSCs as well as nonhematopoietic cells that are thought to provide many of the molecular signals necessary for directing HSC self-renewal and proliferation as well as regulating their differentiation. Coculture of HSCs with stromal cells and growth factors has been utilized in an attempt to recapitulate these interactions ex vivo to expand HSPCs. To date, mesenchymal stem cells (MSCs) have shown the most promise for use ex vivo as they are plastic adherent and seem to restore stromal interactions seen in the BM.46 Preclinical work by Shpall and others coculturing MSCs and either CB or adult progenitor cells has demonstrated modest expansion of the progenitor cell population.46,47 Using the dCBT platform and a myeloablative conditioning regimen, Shpall and colleagues are currently translating this to the clinic by combining a nonmanipulated CB unit with a unit that has been expanded for 14 days in the presence of cytokines (SCF, Flt-3 ligand, G-CSF, and TPO) on either family member donor-derived MSCs or “off-the-shelf” MSCs (Angioblast Ltd). On day 14 the cells are washed and infused following the infusion of the nonmanipulated CB unit (Elizabeth J. Shpall, University of Texas M. D. Anderson Cancer Center, oral communication, November 5, 2010).48–50 To date, they have demonstrated a median 40-fold expansion of CD34+ cells and a median time to neutrophil and platelet engraftment of 15 (range 9-42) and 40 (range 13-62) days, respectively. There were no toxicities attributable to the expanded cells. Thirty-one (97%) and 26 (81%) of all patients engrafted neutrophils and platelets, respectively, and 1 patient died before engraftment.50 These studies confirm a potential role for cell-based HSPC expansion methodologies and suggest the need for further investigation to define the molecules responsible for these effects.
Copper chelator: TEPA
On the basis of studies suggesting that cellular copper is involved in the regulation of proliferation and differentiation of the HSPC,51,52 Peled et al cultured CD34+38− CB HSPCs with the copper chelator tetraethylenepentamine (TEPA) and cytokines (TPO, Flt3 ligand, IL-6, and SCF) and found an average of 17-fold and 159-fold increase in CD34+ cells after 3 and 7 weeks in culture, respectively, compared with input cell number.53,54 More importantly, cells cultured with TEPA appeared to show improved NOD-SCID engraftment in a single analysis performed 8 weeks after transplantation, although the increase in repopulating cells was not enumerated. In a phase 1 trial, Shpall and colleagues cultured a portion of a single cord blood unit with TEPA and cytokines and co-infused these cells with the remainder of the untreated cell fraction. Although this methodology was safe and resulted in engraftment in human subjects, it did not improve the time to neutrophil or platelet engraftment compared with previous published reports.55 A phase 2/3 study is under way in more than 25 centers in the United States, Europe, and Israel, to evaluate the safety and efficacy of this approach (“StemEx”) in 100 patients with advanced hematologic malignancies. Interim results, however, are not yet available (David A. Synder, Gamida Cell Ltd, written communication, November 13, 2010).
PGE2
Using a high-throughput screen to identify novel regulators of HSC self-renewal and proliferation, North et al identified prostaglandin E2 (PGE2) as capable of enhancing HSC formation in zebrafish.56 Furthermore, when murine cells are briefly incubated (1-2 hours) ex vivo with PGE2 before transplantation, significantly higher numbers of repopulating cells are generated in a limiting-dilution transplantation model compared with uncultured control cells (3.3-fold at 6 weeks, 2.3-fold at 24 weeks).56 Although its precise mechanism of action is unknown, PGE2 has been shown to interact with the Wnt pathway by increasing β-catenin expression levels.57 In addition, PGE2 may enhance HSC homing through up-regulation of CXCR4 and survival through Survivin, a protein known to regulate survival and apoptosis through p21.58 This brief ex vivo incubation with PGE2 is currently being tested in a clinical trial in which adults with hematologic malignancies receive a nonmyeloablative conditioning regimen followed by dCBT in which 1 of 2 CB units has been incubated with 16, 16-dimethyl prostaglandin E2 before infusion (Pratik S. Multani, Fate Therapeutics, written communication, October 22, 2010).
Preclinical approaches
AhR antagonist
Also using a high-throughput screen, Boitano et al identified an aryl hydrocarbon receptor (AhR) antagonist (StemRegenin1 or SR1) capable of enhancing CD34+ cell generation from the blood of mobilized donors.59 Using CB progenitors, culture with cytokines plus SR1 led to a 669-fold increase in the number of CD34+ cells at 3 weeks and a 17 100-fold increase with longer-term culture of 5 weeks compared with input cell number. Most important, however, is that CB cells transplanted after 3 weeks in culture demonstrate a 17-fold increase in the number of cells with the ability to repopulate immunodeficient mice compared with uncultured cells or cells cultured with cytokines alone. In addition, SR1-treated cells demonstrated enhanced long-term engraftment with 12-fold improvement in repopulation capacity following secondary transplantation. Whereas it is known that the AhR is expressed on HSCs and has been implicated in pathways regulating hematopoiesis including HES-1, Pu.1, C/EBPbeta, β-catenin and others, the precise mechanism whereby an AhR inhibitor might induce HSPC self-renewal remains unknown.59
Novel cytokines
Three recently described soluble growth factors that are produced by the endothelium—Angiopoietin-like 5 (Angptl5), IGFBP2, and pleiotrophin—may significantly enhance HSPC expansion ex vivo when used in concert with conventional cytokines.60,61 Culture of CD133+ CB cells for 10 days with Angptl5 and/or IGFBP2 led to significantly improved in vivo reconstitution in NOD/SCID mice at 2 months after transplantation (0.8% vs 11.3%, 17.3%, and 39.5% human engraftment for standard cytokines vs standard cytokines plus IGFBP2, Angptl5, or both, respectively) as well as enhanced secondary transplantation, although the fold expansion of total nucleated cells in vitro did not differ significantly from cytokine alone containing cultures.60 Pleiotrophin, which has been found essential for maintenance of murine HSCs, has recently been shown to modestly enhance ex vivo human CB HSPC expansion (approximately 40-fold expansion of CD34+38− cells compared with input cell number after 7 days in culture) as well as in vivo reconstitution of immunodeficient mice with 3-fold improved human engraftment at 4 weeks and a 7-fold increase at 8 weeks after transplantation compared with uncultured control.61 This factor, which was identified initially in brain endothelial cells, may activate the PI3-Kinase/AKT and Notch pathways by alleviating activation of its receptor, receptor protein tyrosine phosphatase- β/ζ.61,62
HOXB4
Overexpression through cellular modification of the homeobox gene HOXB4, a regulator of hematopoietic differentiation, has led to expansion of murine as well as human HSPCs.63,64 To avoid genetic alteration of the HSCs, human CB CD34+ cells have been expanded by culture in the presence of a stromal cell layer expressing a HOXB4 fusion protein that is passively taken up by the CD34+ cells, resulting in a 2.5-fold increase in long-term repopulating cells compared with uncultured control.65 Future studies with continuous presentation of this relatively unstable protein or development of more stable protein forms may prove an effective strategy for ex vivo expansion.
Other potential molecular targets
A variety of other molecules known to play roles in stem cell self-renewal, development, and cell-cycle regulation have also attracted interest, although to date they have not been manipulated for significant ex vivo expansion. Forced overexpression of β-catenin, a downstream effector of Wnt signaling, results in significant ex vivo expansion of murine HSCs.66 However, the role of the Wnt pathway in stem cell self-renewal based on gain- and loss-of function studies of Wnt pathway components remains controversial.67,68 In studies with human CB progenitors, manipulation of the Wnt pathway through overexpression of Wnt5a or with glycogen synthase kinase-3B (GSK-3B) inhibitors did not augment expansion when added ex vivo to cultures but did enhance engraftment when infused in vivo after transplantation in irradiated mice.69,70 It remains unclear, however, whether these outcomes result from direct effects on HSCs or are indirectly mediated through marrow stromal interactions. Other pathways known to regulate stem cell development, including Sonic Hedgehog and BMP-4, may also prove effective for human hematopoietic stem/progenitor cell growth and self-renewal and deserve further exploration.71,72 Activation of the PI3-Kinase-AKT pathway because of inactivation of the negative regulator PTEN results in short-term HSC expansion but with long-term exhaustion of the stem cell pool.73 Inactivation of the cyclin-dependent kinase inhibitors p16Ink4a and p19Arf augments stem cell self-renewal in knockout murine models.74,75 Finally, p21, a downstream target of p53, has been implicated in stem cell quiescence as p21−/− mice demonstrate significantly impaired stem cell self-renewal.76 Thus there are compelling murine data that these molecular pathways play an important role in the regulation of HSC self-renewal and may be applicable in human studies. It is possible, however, that manipulation of these pathways, particularly those with tumor-suppressor function, may permit accumulation of mutations during stem cell culture, generating potentially oncogenic cells.
Opportunities, challenges, and future directions
Further improvements in the ex vivo generation of HSPCs will undoubtedly be forthcoming by some combination of the above-cited and yet-to-be-developed methods to manipulate different pathways supporting the proliferation, self-renewal, and survival of HSPCs. For example, whereas activation of the Notch pathway is able to inhibit HSPC differentiation, the addition of other factors that enhance proliferation and/or survival might be expected to increase the numbers of both long-term repopulating HSCs and short-term repopulating progenitors, perhaps allowing for future sole use of expanded CB in the absence of a nonmanipulated unit. Furthermore, cross-talk between pathways such as the Notch and Wnt pathways may lead to synergistic effects. In addition, provision of appropriate substrates in cultures, such as integrins,77 may further enhance HSPC self-renewal. Finally, we expect the development of approaches that will enhance the ability of ex vivo–generated HSPCs to home and survive in vivo. For example, agents that inhibit CD2678 or alter fucosylation79 increase the expression of molecules critical for homing properties (such as CXCR4) and PGE2 may both improve homing and in vivo survival. Future studies may also develop alternative sources of HSPCs, in particular embryonic stem cells or induced pluripotent stem cells, which may be amenable to many of the expansion methods described herein.
Despite the many promising approaches discussed, challenges clearly remain. A key issue is the expansion of the long-term repopulating HSCs. Abrogation of the prolonged neutropenia that occurs following high-dose chemotherapy and radiation for HSCT is the immediate goal of expanded cell therapies for clinical intent. As demonstrated in the clinical trial using Notch-mediated expansion of CB progenitors, this can be achieved through the generation of short-term repopulating progenitor cells capable of rapid, but transient, myelopoiesis. If truly transient, the generation of large numbers of short-term repopulating cells could also be applied to other non–stem cell transplantation therapies in which prolonged neutropenia causes increased risk of death because of infection, such as high-dose chemotherapy for AML or following accidental radiation exposure. However, other indications such as gene therapy still require expansion of long-term HSCs. In the transplantation setting, expansion of both long- and short-term repopulating cells would allow for infusion of expanded cells alone. This would allow for the use of single, expanded CB units that would previously have been considered too small for use and may allow patients to receive smaller, HLA-matched units who otherwise would have received mismatched grafts. Although our studies have suggested the presence of these long-term repopulating cells in Notch-expanded grafts, design of studies to definitively test this possibility will be problematic in the current clinical setting because of the requirement for infusion of a second immunocompetent unit, rendering long-term survival of the expanded cells unlikely. A related challenge is the need for better characterization and expansion of thymic repopulating cells as delayed immune reconstitution remains a major cause of CB transplantation-related morbidity and mortality. Although our studies40 and others59 have demonstrated thymic engrafting cells in immunodeficient mice, the precise cell responsible has not been determined.
Cost consideration will ultimately affect the application of stem cell expansion methodologies provided they demonstrate improved patient outcome or decreased requirement for hospitalization after transplantation. Bioprocesses involving cell selection,80 investigation of novel bioreactors that may recreate an artificial stem cell niche,81 effectively using or reusing media and cytokines, and 3-dimensional lattices allowing for maximal expansion82 will certainly contribute to better optimized, cost-effective approaches. In addition, our current studies are testing whether transient engraftment in myelosuppressed patients undergoing CB HCT or high-dose chemotherapy can be achieved using ex vivo–expanded and then cryopreserved, non-HLA matched CB HSPCs. Success with this approach would potentially make small inventories of previously expanded CB HSPCs available for universal and immediate use, in contrast to the large inventories currently required to ensure availability of HLA-matched units. This methodology, which also eliminates the need for expanding CB units in real-time and allows for the future possibility of pooling several units for processing, enables a commercially feasible approach.
Also critical to the future development of these cellular therapies is the need to ensure safety of the expanded cell products, particularly when pathways that maintain genomic integrity might be perturbed, allowing for aberrant differentiation and/or oncogenesis. New techniques for global assessment of the genome and epigenome will enable assessment of whether the genome and chromatin landscape of the expanded cell populations accurately reflect their nonmanipulated counterparts and thus are predictive of appropriate cell behavior.
During the next few years, we can expect that further development of the promising methods described herein will result in substantially enhanced generation of HSPCs for clinical application, and, importantly, the effectiveness of such approaches will be tested in randomized clinical trials. We ultimately envision utilizing expanded HSPCs to significantly improve the clinical course of patients undergoing HCT or myelosuppression from high-dose chemotherapy or radiation exposure by ameliorating the severe side effects associated with these treatments and decreasing the length of their hospital stay, thus having both a clinical and an economic impact. We also believe that success in the hematopoietic system will be followed closely by success in a wide variety of stem cell–based therapies.
Acknowledgments
We thank M. Cooke, B. Hadland, S. Heimfeld, A. Shimamura, C. Stein, and B. Varnum-Finney for their critical reading of the manuscript.
This work was supported by National Heart, Lung, and Blood Institute grants U01HL100395, R01HL080245, R01HL084205, R24HL074445, RC2HL101844, and National Institutes of Health Ruth L. Kirschstein National Research Service Award T32CA009351. C.D. is a Damon Runyon Clinical Investigator. I.D.B. is an American Cancer Society Professor.
Authorship
Contribution: All authors reviewed the literature and each wrote portions of the paper. I.D.B. had overall editorial responsibility for the manuscript.
Conflict-of-interest disclosure: The Fred Hutchinson Cancer Research Center holds a patent on “methods for immortalizing cells” that covers the use of Notch ligand for expansion of hematopoietic stem cells. I.D.B. is an inventor on this patent. The remaining authors declare no competing financial interests.
Correspondence: Irwin D. Bernstein, Fred Hutchinson Cancer Research Center, 1100 Fairview Ave N, D2-373, PO Box 19024, Seattle, WA 98109-1024; e-mail: ibernste@fhcrc.org.
References
- 1.Weissman IL. Stem cells: units of development, units of regeneration, and units in evolution. Cell. 2000;100(1):157–168. doi: 10.1016/s0092-8674(00)81692-x. [DOI] [PubMed] [Google Scholar]
- 2.Sauvageau G, Iscove NN, Humphries RK. In vitro and in vivo expansion of hematopoietic stem cells. Oncogene. 2004;23(43):7223–7232. doi: 10.1038/sj.onc.1207942. [DOI] [PubMed] [Google Scholar]
- 3.Ogawa M. Differentiation and proliferation of hematopoietic stem cells. Blood. 1993;81(11):2844–2853. [PubMed] [Google Scholar]
- 4.Noort WA, Willemze R, Falkenburg JH. Comparison of repopulating ability of hematopoietic progenitor cells isolated from human umbilical cord blood or bone marrow cells in NOD/SCID mice. Bone Marrow Transplant. 1998;22(suppl 1):S58–S60. [PubMed] [Google Scholar]
- 5.Ueda T, Yoshida M, Yoshino H, et al. Hematopoietic capability of CD34+ cord blood cells: a comparison with CD34+ adult bone marrow cells. Int J Hematol. 2001;73(4):457–462. doi: 10.1007/BF02994007. [DOI] [PubMed] [Google Scholar]
- 6.Barker JN, Weisdorf DJ, DeFor TE, et al. Transplantation of 2 partially HLA-matched umbilical cord blood units to enhance engraftment in adults with hematologic malignancy. Blood. 2005;105(3):1343–1347. doi: 10.1182/blood-2004-07-2717. [DOI] [PubMed] [Google Scholar]
- 7.Brunstein CG, Gutman JA, Weisdorf DJ, et al. Allogeneic hematopoietic cell transplantation for hematologic malignancy: relative risks and benefits of double umbilical cord blood. Blood. 2010;116(22):4693–4699. doi: 10.1182/blood-2010-05-285304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bhatia M, Bonnet D, Kapp U, Wang JC, Murdoch B, Dick JE. Quantitative analysis reveals expansion of human hematopoietic repopulating cells after short-term ex vivo culture. J Exp Med. 1997;186(4):619–624. doi: 10.1084/jem.186.4.619. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Conneally E, Cashman J, Petzer A, Eaves C. Expansion in vitro of transplantable human cord blood stem cells demonstrated using a quantitative assay of their lympho-myeloid repopulating activity in nonobese diabetic-scid/scid mice. Proc Natl Acad Sci U S A. 1997;94(18):9836–9841. doi: 10.1073/pnas.94.18.9836. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Gammaitoni L, Bruno S, Sanavio F, et al. Ex vivo expansion of human adult stem cells capable of primary and secondary hemopoietic reconstitution. Exp Hematol. 2003;31(3):261–270. doi: 10.1016/s0301-472x(02)01077-9. [DOI] [PubMed] [Google Scholar]
- 11.Ueda T, Tsuji K, Yoshino H, et al. Expansion of human NOD/SCID-repopulating cells by stem cell factor, Flk2/Flt3 ligand, thrombopoietin, IL-6, and soluble IL-6 receptor. J Clin Invest. 2000;105(7):1013–1021. doi: 10.1172/JCI8583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Bachier CR, Gokmen E, Teale J, et al. Ex-vivo expansion of bone marrow progenitor cells for hematopoietic reconstitution following high-dose chemotherapy for breast cancer. Exp Hematol. 1999;27(4):615–623. doi: 10.1016/s0301-472x(98)00085-x. [DOI] [PubMed] [Google Scholar]
- 13.Boiron J-M, Dazey B, Cailliot C, et al. Large-scale expansion and transplantation of CD34+ hematopoietic cells: in vitro and in vivo confirmation of neutropenia abrogation related to the expansion process without impairment of the long-term engraftment capacity. Transfusion. 2006;46(11):1934–1942. doi: 10.1111/j.1537-2995.2006.01001.x. [DOI] [PubMed] [Google Scholar]
- 14.McNiece I, Jones R, Bearman SI, et al. Ex-vivo expanded peripheral blood progenitor cells provide rapid neutrophil recovery after high-dose chemotherapy in patients with breast cancer. Blood. 2000;96(9):3001–3007. [PubMed] [Google Scholar]
- 15.Williams SF, Lee WJ, Bender JG, et al. Selection and expansion of peripheral blood CD34+ cells in autologous stem cell transplantation for breast cancer. Blood. 1996;87(5):1687–1691. [PubMed] [Google Scholar]
- 16.Shpall EJ, Quinones R, Giller R, et al. Transplantation of ex vivo expanded cord blood. Biol Blood Marrow Transplant. 2002;8(7):368–376. doi: 10.1053/bbmt.2002.v8.pm12171483. [DOI] [PubMed] [Google Scholar]
- 17.de Lima M, McMannis JD, Saliba R, et al. Double cord blood transplantation (CBT) with and without ex-vivo expansion (EXP): a randomized, controlled study [abstract]. Blood. 2008;112 Abstract 154. [Google Scholar]
- 18.Jaroscak J, Goltry K, Smith A, et al. Augmentation of umbilical cord blood (UCB) transplantation with ex vivo-expanded UCB cells: results of a phase I trial using the AastromReplicell system. Blood. 2003;101(12):5061–5067. doi: 10.1182/blood-2001-12-0290. [DOI] [PubMed] [Google Scholar]
- 19.Greenwald I, Rubin GM. Making a difference: the role of cell-cell interactions in establishing separate identities for equivalent cells. Cell. 1992;68(2):271–281. doi: 10.1016/0092-8674(92)90470-w. [DOI] [PubMed] [Google Scholar]
- 20.Artavanis-Tsakonas S, Rand MD, Lake RJ. Notch signaling: cell fate control and signal integration in development. Science. 1999;284(5415):770–776. doi: 10.1126/science.284.5415.770. [DOI] [PubMed] [Google Scholar]
- 21.Simpson P. Introduction: Notch signalling and choice of cell fates in development. Semin Cell Dev Biol. 1998;9(6):581–582. doi: 10.1006/scdb.1998.0265. [DOI] [PubMed] [Google Scholar]
- 22.Bray SJ. Notch signalling: a simple pathway becomes complex. Nat Rev Mol Cell Biol. 2006;7(9):678–689. doi: 10.1038/nrm2009. [DOI] [PubMed] [Google Scholar]
- 23.Radtke F, Fasnacht N, Macdonald HR. Notch signaling in the immune system. Immunity. 2010;32(1):14–27. doi: 10.1016/j.immuni.2010.01.004. [DOI] [PubMed] [Google Scholar]
- 24.Wendorff AA, Koch U, Wunderlich FT, et al. Hes1 is a critical but context-dependent mediator of canonical Notch signaling in lymphocyte development and transformation. Immunity. 2010;33(5):671–684. doi: 10.1016/j.immuni.2010.11.014. [DOI] [PubMed] [Google Scholar]
- 25.Varnum-Finney B, Dallas MH, Kato K, Bernstein ID. Notch target Hes5 ensures appropriate Notch induced T-versus B-cell choice in the thymus. Blood. 2008;111(5):2615–2620. doi: 10.1182/blood-2007-03-079855. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Radtke F, Wilson A, Stark G, et al. Deficient T cell fate specification in mice with an induced inactivation of Notch1. Immunity. 1999;10(5):547–558. doi: 10.1016/s1074-7613(00)80054-0. [DOI] [PubMed] [Google Scholar]
- 27.Han H, Tanigaki K, Yamamoto N, et al. Inducible gene knockout of transcription factor recombination signal binding protein-J reveals its essential role in T verses B lineage decision. Int Immunol. 2002;14(6):637–645. doi: 10.1093/intimm/dxf030. [DOI] [PubMed] [Google Scholar]
- 28.Varnum-Finney B, Halasz LM, Sun M, Gridley T, Radtke F, Bernstein ID. Notch2 governs the rate of generation of mouse long- and short-term repopulating stem cells [published online ahead of print February 11, 2011]. J Clin Invest. doi: 10.1172/JCI43868. doi: 10.1172/JCI43868. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Milner LA, Kopan R, Martin DIK, Bernstein ID. A human homologue of the drosophila developmental gene, Notch, is expressed in CD34+ hematopoietic precursors. Blood. 1994;83(8):2057–2062. [PubMed] [Google Scholar]
- 30.Ellisen LW, Bird J, West DC, et al. TAN-1, the human homolog of the Drosophila notch gene, is broken by chromosomal translocations in T lymphoblastic neoplasms. Cell. 1991;66(4):649–661. doi: 10.1016/0092-8674(91)90111-b. [DOI] [PubMed] [Google Scholar]
- 31.Pear WS, Aster JC, Scott ML, et al. Exclusive development of T cell neoplasms in mice transplanted with bone marrow expressing activated Notch alleles. J Exp Med. 1996;183(5):2283–2291. doi: 10.1084/jem.183.5.2283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Pui JC, Allman D, Xu L, et al. Notch1 expression in early lymphopoiesis influences B versus T lineage determination. Immunity. 1999;11(3):299–308. doi: 10.1016/s1074-7613(00)80105-3. [DOI] [PubMed] [Google Scholar]
- 33.Maillard I, Koch U, Dumortier A, et al. Canonical notch signaling is dispensable for the maintenance of adult hematopoietic stem cells. Cell Stem Cell. 2008;2(4):356–366. doi: 10.1016/j.stem.2008.02.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Mancini SJ, Mantei N, Demortier A, Suter U, MacDonald HR, Radtke F. Jagged1-dependent Notch signaling is dispensable for hematopoietic stem cell self-renewal and differentiation. Blood. 2005;105(6):2340–2342. doi: 10.1182/blood-2004-08-3207. [DOI] [PubMed] [Google Scholar]
- 35.Varnum-Finney B, Xu L, Brashem-Stein C, et al. Pluripotent, cytokine-dependent, hematopoietic stem cells are immortalized by constitutive Notch1 signaling. Nat Med. 2000;6(11):1278–1281. doi: 10.1038/81390. [DOI] [PubMed] [Google Scholar]
- 36.Varnum-Finney B, Purton LE, Yu M, et al. The Notch ligand, Jagged-1, influences the development of primitive hematopoietic precursor cells. Blood. 1998;91(11):4084–4091. [PubMed] [Google Scholar]
- 37.Varnum-Finney B, Wu L, Yu M, et al. Immobilization of Notch ligand, Delta-1, is required for induction of notch signaling. J Cell Sci. 2000;113(23):4313–4318. doi: 10.1242/jcs.113.23.4313. [DOI] [PubMed] [Google Scholar]
- 38.Varnum-Finney B, Brashem-Stein C, Bernstein ID. Combined effects of Notch signaling and cytokines induce a multiple log increase in precursors with lymphoid and myeloid reconstituting ability. Blood. 2003;101(5):1784–1789. doi: 10.1182/blood-2002-06-1862. [DOI] [PubMed] [Google Scholar]
- 39.Dallas MH, Varnum-Finney B, Martin PJ, Bernstein ID. Enhanced T-cell reconstitution by hematopoietic progenitors expanded ex vivo using the Notch ligand Delta1. Blood. 2007;109(8):3579–3587. doi: 10.1182/blood-2006-08-039842. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Ohishi K, Varnum-Finney B, Bernstein ID. Delta-1 enhances marrow and thymus repopulating ability of human CD34+38- cord blood cells. J Clin Invest. 2002;110(8):1165–1174. doi: 10.1172/JCI16167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Delaney C, Varnum-Finney B, Aoyama K, Brashem-Stein C, Bernstein ID. Dose-dependent effects of the Notch ligand Delta1 on ex vivo differentiation and in vivo repopulating ability of cord blood cells. Blood. 2005;106(9):2693–2699. doi: 10.1182/blood-2005-03-1131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Delaney C, Heimfeld S, Brashem-Stein C, Voorhies H, Manger RL, Bernstein ID. Notch-mediated expansion of human cord blood progenitor cells capable of rapid myeloid reconstitution. Nat Med. 2010;16(20):232–237. doi: 10.1038/nm.2080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Dallas MH, Varnum-Finney B, Delaney C, Kato K, Bernstein ID. Density of the Notch ligand Delta1 determines generation of B and T cell precursors from hematopoietic stem cells. J Exp Med. 2005;201(9):1361–1366. doi: 10.1084/jem.20042450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Offner F, Schoch G, Fisher LD, Torok-Storb B, Martin PJ. Mortality hazard functions as related to neutropenia at different times after marrow transplantation. Blood. 1996;88(10):4058–4062. [PubMed] [Google Scholar]
- 45.Gutman JA, Turtle CJ, Manley TJ, et al. Single-unit dominance after double-unit umbilical cord blood transplantation coincides with a specific CD8+ T-cell response against the nonengrafted unit. Blood. 2010;115(4):757–765. doi: 10.1182/blood-2009-07-228999. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McNiece I, Harrington J, Turney J, Kellner J, Shpall EJ. Ex vivo expansion of cord blood mononuclear cells on mesenchymal stem cells. Cytotherapy. 2004;6(4):311–317. doi: 10.1080/14653240410004871. [DOI] [PubMed] [Google Scholar]
- 47.Li N, Feugier P, Serrurrier B, et al. Human mesenchymal stem cells improve ex vivo expansion of adult human CD34+ peripheral blood progenitor cells and decrease their allostimulatory capacity. Exp Hematol. 2007;35(3):507–515. doi: 10.1016/j.exphem.2006.10.015. [DOI] [PubMed] [Google Scholar]
- 48.Kelly SS, Sola CBS, de Lima M, Shpall E. Ex vivo expansion of cord blood. Bone Marrow Transplant. 2009;44(10):673–681. doi: 10.1038/bmt.2009.284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.De Lima M, Robinson S, McMannis J, et al. Mesenchymal stem cell based cord blood expansion leads to rapid engraftment of platelets and neutrophils [abstract]. Blood. 2010;116 Abstract 362. [Google Scholar]
- 50.De Lima M, Robinson S, McMannis J, et al. Mesenchymal stem cell (MSC) based cord blood (CB) expansion (Exp) leads to rapid engraftment of platelets and neutrophils [abstract]. Blood. 2010;116 Abstract 362. [Google Scholar]
- 51.Peled T, Landau E, Prus E, Treves A, Nagler A, Fibach E. Cellular copper content modulates differentiation and self renewal in cultures of cord blood-derived CD34+ cells. Br J Haematol. 2002;116(3):655–661. doi: 10.1046/j.0007-1048.2001.03316.x. [DOI] [PubMed] [Google Scholar]
- 52.Peled T, Glukhman E, Hasson N, et al. Chelatable cellular copper modulates differentiation and self-renewal of cord blood-derived hematopoietic progenitor cells. Exp Hematol. 2005;33(10):1092–1100. doi: 10.1016/j.exphem.2005.06.015. [DOI] [PubMed] [Google Scholar]
- 53.Peled T, Mandel JL, Goudsmid R, et al. Pre-clinical development of cord blood-derived progenitor cell graft expanded ex vivo with cytokines and the polyamine copper chelator tetraethylenepentamine. Cytotherapy. 2004;6(4):344–355. doi: 10.1080/14653240410004916. [DOI] [PubMed] [Google Scholar]
- 54.Peled T, Landau E, Mandel J, et al. Linear polyamine copper chelator tetraethylenepentamine augments long-term ex vivo expansion of cord blood-derived CD34+ cells and increases their engraftment potential in NOD/SCID mice. Exp Hematol. 2004;32(6):547–555. doi: 10.1016/j.exphem.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 55.de Lima M, McMannis J, Gee A, et al. Transplantation of ex vivo expanded cord blood cells using the copper chelator tetraethylenepentamine: a phase I/II clinical trial. Bone Marrow Transplant. 2008;41(9):771–778. doi: 10.1038/sj.bmt.1705979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.North TE, Goessling W, Walkley CR, et al. Prostaglandin E2 regulates vertebrate haematopoietic stem cell homeostasis. Nature. 2007;447(7147):1007–1011. doi: 10.1038/nature05883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Goessling W, North TE, Loewer S, et al. Genetic interaction of PGE2 and Wnt signaling regulates developmental specification of stem cells and regeneration. Cell. 2009;136(6):1136–1147. doi: 10.1016/j.cell.2009.01.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Hoggatt J, Singh P, Sampath J, Pelus LM. Prostaglandin E2 enhances hematopoietic stem cell homing, survival and proliferation. Blood. 2009;113(22):5444–5455. doi: 10.1182/blood-2009-01-201335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Boitano AE, Wang J, Romeo R, et al. Aryl hydrocarbon receptor antagonists promote the expansion of human hematopoietic stem cells. Science. 2010;329(5997):1345–1348. doi: 10.1126/science.1191536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zhang CC, Kaba M, Iizuka S, Huynh HD, Lodish HF. Angiopoietin-like 5 and IGFBP2 stimulate ex vivo expansion of human cord blood hematopoietic stem cells as assayed by NOD/SCID transplantation. Blood. 2008;111(7):3415–3423. doi: 10.1182/blood-2007-11-122119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Himburg HA, Muramoto GG, Daher P, et al. Pleiotrophin regulates the expansion and regeneration of hematopoietic stem cells. Nat Med. 2010;16(4):475–483. doi: 10.1038/nm.2119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.HImburg HA, Daher P, Russel JL, et al. Pleiotrophin signaling is necessary and sufficient for hematopoietic stem cell self-renewal in vivo [abstract]. Blood. 2010;116 Abstract 404. [Google Scholar]
- 63.Antonchuk J, Sauvageau G, Humphries RK. HOXB4-Induced expansion of adult hematopoietic stem cell ex vivo. Cell. 2002;109(1):39–45. doi: 10.1016/s0092-8674(02)00697-9. [DOI] [PubMed] [Google Scholar]
- 64.Sauvageau G, Lansdorp PM, Eaves CJ, et al. Differential expression of homeobox genes in functionally distinct CD34+ subpopulations of human bone marrow cells. Proc Natl Acad Sci U S A. 1994;91(25):12223–12227. doi: 10.1073/pnas.91.25.12223. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Amsellem S, Pflumio F, Bardinet D, et al. Ex vivo expansion of human hematopoietic stem cells by direct delivery of the HOXB4 homeoprotein. Nat Med. 2003;9(11):1423–1427. doi: 10.1038/nm953. [DOI] [PubMed] [Google Scholar]
- 66.Reya T, Duncan AW, Ailles L, et al. A role for Wnt signalling in self-renewal of haematopoietic stem cells. Nature. 2003;423(6938):409–414. doi: 10.1038/nature01593. [DOI] [PubMed] [Google Scholar]
- 67.Cobas M, Wilson A, Ernst B, et al. beta-catenin is dispensable for hematopoiesis and lymphopoiesis. J Exp Med. 2004;199(2):221–229. doi: 10.1084/jem.20031615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Scheller M, Huelsken J, Rosenbauer F, et al. Hematopoietic stem cell and multilineage defects generated by constitutive beta-catenin activation. Nat Immunol. 2006;7(10):1037–1047. doi: 10.1038/ni1387. [DOI] [PubMed] [Google Scholar]
- 69.Murdoch B, Chadwick K, Martin M, et al. Wnt-5A augments repopulating capacity and primitive hematopoietic development of human blood stem cells in vivo. Proc Natl Acad Sci U S A. 2003;100(6):3422–3427. doi: 10.1073/pnas.0130233100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Trowbridge JJ, Xenocostas A, Moon RT, Bhatia M. Glycogen synthase kinase-3 is an in vivo regulator of hematopoietic stem cell repopulation. Nat Med. 2006;12(1):89–98. doi: 10.1038/nm1339. [DOI] [PubMed] [Google Scholar]
- 71.Bhardwaj G, Murdoch B, Wu D, et al. Sonic hedgehog induces the proliferation of primitive human hematopoietic cells via BMP regulation. Nat Immunol. 2001;2(2):172–180. doi: 10.1038/84282. [DOI] [PubMed] [Google Scholar]
- 72.Ying QL, Nichols J, Chambers I, Smith A. BMP induction of Id proteins suppresses differentiation and sustains embryonic stem cell self-renewal in collaboration with STAT3. Cell. 2003;115(3):281–292. doi: 10.1016/s0092-8674(03)00847-x. [DOI] [PubMed] [Google Scholar]
- 73.Zhang J, Grindley JC, Yin T, et al. PTEN maintains haematopoietic stem cells and acts in lineage choice and leukaemia prevention. Nature. 2006;441(7092):518–522. doi: 10.1038/nature04747. [DOI] [PubMed] [Google Scholar]
- 74.Akala OO, Park I-K, Qian D, Pihalja M, Becker MW, Clark MF. Long-term haematopoietic reconstitution by Trp53−/−p16Ink4a−/−p19Arf−/− multipotent progenitors. Nature. 2008;453(7192):228–232. doi: 10.1038/nature06869. [DOI] [PubMed] [Google Scholar]
- 75.Iwama A, Oguro H, Negishi M, et al. Enhanced self-renewal of hematopoietic stem cells mediated by the polycomb gene product Bmi-1. Immunity. 2004;21(6):843–851. doi: 10.1016/j.immuni.2004.11.004. [DOI] [PubMed] [Google Scholar]
- 76.Cheng T, Rodrigues N, Shen H, et al. Hematopoietic stem cell quiescence maintained by p21cip1/waf1. Science. 2000;287(5459):1804–1808. doi: 10.1126/science.287.5459.1804. [DOI] [PubMed] [Google Scholar]
- 77.Mei Y, Saha K, Bogatyrev SR, et al. Combinatorial development of biomaterials for clonal growth of human pluripotent stem cells. Nat Mater. 2010;9(9):768–778. doi: 10.1038/nmat2812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Campbell TB, Hangoc G, Liu Y, Pollok K, Broxmeyer HE. Inhibition of CD26 in human cord blood CD34+ cells enhances their engraftment of nonobese diabetic/severe combined immunodeficiency mice. Stem Cells Dev. 2007;16(3):347–354. doi: 10.1089/scd.2007.9995. [DOI] [PubMed] [Google Scholar]
- 79.Xia L, McDaniel JM, Yago T, Doeden A, McEver RP. Surface fucosylation of human cord blood cells augments binding to P-selectin and E-selectin and enhances engraftment in bone marrow. Blood. 2004;104(10):3091–3096. doi: 10.1182/blood-2004-02-0650. [DOI] [PubMed] [Google Scholar]
- 80.Chou S, Chu P, Hwang W, Lodish H. Expansion of human cord blood hematopoietic stem cells for transplantation. Cell Stem Cell. 2010;7(4):427–428. doi: 10.1016/j.stem.2010.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Astori G, Adami V, Mambrini G, et al. Evaluation of ex vivo expansion and engraftment in NOD-SCID mice of umbilical cord blood CD34+ cells using the DIDECO ‘Pluricell System.’. Bone Marrow Transplant. 2005;35(11):1101–1106. doi: 10.1038/sj.bmt.1704964. [DOI] [PubMed] [Google Scholar]
- 82.Liu Y, Liu T, Fan X, Ma X, Cui Z. Ex vivo expansion of hematopoietic stem cells derived from umbilical cord blood in rotating wall vessel. J Biotechnol. 2006;124(3):592–601. doi: 10.1016/j.jbiotec.2006.01.020. [DOI] [PubMed] [Google Scholar]