Abstract
Objective
Children of mothers with mental illness are at risk for multiple untoward outcomes, including child maltreatment and foster care placement. The purpose of this analysis was to determine the association between maternal mental illness and children’s long term safety and stability.
Methods
A multi-sector administrative dataset from the Department of Social Services (DSS) and Department of Mental Health (DMH) was analyzed. The sample was 4,895 low income families (mother and child dyads) first reported to child welfare in 1993 or 1994. Families were followed until March of 2009. Dates of new report and foster care placement were obtained from DSS data. ICD-09 or ICD-10 diagnostic codes were obtained from Department of Mental Health data. Schizophrenic disorders, episodic mood disorders, anxiety disorders and personality disorders were examined.
Results
New reports were more likely for children of mothers with mental illness, regardless of diagnosis. While overall 67% of children had a new report over the course of their childhood, rates ranged from 80–90% for children of mothers with mental illness and occurred within a shorter time frame than for other children. In the multivariate models, mood (HR=1.41, p<.001) and anxiety disorders (HR=1.32, p<.05) placed children at greater risk for new reports. The proportion of children with foster placements was more than double for children of mothers with mental illness than for other children. In the multivariate model, anxiety disorders were strongly associated with the risk of placement (HR = 1.75, p < .001).
Conclusions and Practice Implications
Important differences in safety and stability were found between children of mothers with and without mental illnesses, as well as some variability across diagnoses. Since these mothers had already received services our findings suggest that access is not enough. The services they are receiving or have received may be an ineffective approach to helping them parent safely.
Introduction
Mental illness affects a substantial portion of the US population. Annual prevalence among adults is 18% for anxiety disorders, 7% for major depression, 3% for bipolar disorder, and 1% for schizophrenia (Kessler, Chiu, Demler, & Walters, 2005; Regier et al., 1993). Nearly 4% of adults have antisocial personality disorder (Compton, Conway, Stinson, Colliver, & Grant, 2005) and 2% have borderline personality disorder (Swartz, Blazer, George, & Winfield, 1990). Of further concern is that two-thirds of women with mental illness are mothers (Nicholson, Beibel, Hinden, Henry, & Stier, 2001) and maternal mental illness can have negative consequences for children. The purpose of this analysis was to examine the association between maternal mental illness and children’s long term safety and stability.
Mental illness influences parenting behaviors, which affect child safety. Depression elevates the risk of coercive or hostile parenting, and corporal punishment (Chung, McCollum, Elo, Lee, & Culhane, 2004; Lovejoy, Craczyk, O’Hare, & Neuman, 2000; Lyons-Ruth, Wolfe, Lyubchik, & Steingard, 2002; Shin & Stein, 2008). Mothers with schizophrenia are less responsive and emotionally involved with their children than depressed mothers and mothers without mental illness---although depressed mothers have lower quality interactions than undiagnosed mothers (Goodman & Brumley, 1990). Mothers with borderline personality disorder are less sensitive to their children’s needs, and experience more distress in their parenting role than mothers without this disorder (Newman, Stevenson, Bergman, & Boyce, 2007). Mothers with antisocial personality disorder also tend to engage in lower quality parenting (Simons, Beaman, Conger et al., 1993).
Furthermore, anxious mothers demonstrate less warmth, more criticism, and higher levels of control toward their children (Moore, Whaley, & Sigman, 2004); anxious mothers are also more disengaged from their children than non-anxious mothers (Woodruff-Borden, Morrow, Bourland, & Cambron, 2002).
Mental illness is associated with heightened risk of child maltreatment. Analysis of the National Institute for Mental Health’s Epidemiologic Catchment Area survey demonstrated that maternal depression places children at risk for abuse (Chaffin, Kelleher, & Hollenberg, 1996). Others have found a similar association between maternal depression and maltreatment (Kotch, Browne, Dufort, & Winsor1999; Sheppard, 1997; Windham et al., 2004). Children of parents with depression or schizophrenia are 2 times more likely to experience abuse than children of parents without mental illness; children of parents with antisocial behavior are 6 times more likely to experience abuse (Walsh, MacMillan, & Jamieson, 2002). Parents with undifferentiated mental illness are also 2 times more likely to abuse and neglect their children (Brown, Cohen, Johnson, & Salzinger, 1998). This maltreatment risk suggests that a high proportion of mothers entering the child welfare system have a mental disorder.
Moreover, children of mothers with mental illness have an increased likelihood of foster care placement. Among Medicaid-eligible mothers in one urban city, mothers with a serious mental illness (defined as schizophrenia or a major affective disorder) were 2.8 times more likely to have their child placed into out of home care than mothers without a serious mental illness (Park, Solomon, & Mandell, 2006). Nationally, children of caregivers with serious mental health problems identified by their child welfare caseworker were more likely to be placed into substitute care than other children (US DHHS ACF, 2005). Overall, estimates---albeit dated---indicate that between 70 and 80% of mothers with serious mental illness will experience the placement of a child into foster care (Burton, 1990).
The evidence of impaired parenting among mothers with mental illness is not without limitations. Much of what is known is based on research using small sample sizes (Nicholson et al., 2001) and relies on self-report of mental disorders. Furthermore, with few exceptions (Lewin & Abdrbo, 2009; Mowbray, Oyserman, Bybee, & MacFarlane, 2002), researchers have not differentiated between diagnoses, instead aggregating disorders into a single category---a practice that assumes “homogeneous effects on parenting” (Lewin & Abdrbo, 2009, p. 201). Depression and schizophrenia are the focus of most research in this area, while personality disorders and anxiety have had limited attention.
Finally, while substantial research has examined recurrent maltreatment (e.g., DePanfilis & Zuravin, 1998; English, Marshall, Brummel, & Orme, 1999; Fluke, Yuan, & Edwards, 1999), only limited attention has been given to mothers with a mental disorder in the child welfare system, despite the high rates of mental illness among this population. These families are also likely to be facing parenting barriers due to poverty (Drake & Zuravin, 1998). We know comparatively little about whether maternal mental illness has an impact on child safety and stability beyond the role of poverty. This hampers the ability to effectively and efficiently target intervention for this high risk group.
This study helps overcome these gaps. We conducted a longitudinal analyses of a large sample of children and their mothers (n = 4,895) using a multi-sector administrative database from the Department of Social Services (DSS) and the Department of Mental Health (DMH) in one Midwestern state. We focused on low income families with at least 1 maltreatment report and followed them for over a decade. This study advances knowledge by examining the risk of maltreatment recurrence associated with specific types of maternal mental disorders. Two hypotheses were tested: (1) Risk of new maltreatment reports is higher for children of mothers with mental illness than for children of mothers without mental illness; and (2) Risk of foster care placements is higher for children of mothers with mental illness than for children of mothers without mental illness. We also examined the following research question: Does the relationship between maternal mental illness and child outcomes vary by diagnosis (schizophrenic disorders, episodic mood disorders, anxiety disorders, and personality disorders)?
Methods
Data were extracted from state electronic information systems. While administrative data on services use and service system contact cannot be used to assess unmet need and lacks the ability to measure neurochemical or biological mechanisms discussed in theories of chronic exposure to stress, the data have several strengths. Administrative data allow for precise dating of maltreatment allegations and mental health treatment, avoiding the difficulties in retrospective recall of maltreatment and/or services encountered in the past (Hoagwood, Horwitz, Stiffman, et al., 2000; Widom, Raphael, & DuMont, 2004).
DMH data, obtained through mid-2006, included fee-for-service records submitted by public and private contracted agencies (16 psychiatric facilities and 400 community mental health centers). Although exact estimates of the proportion of mental health services funded by this agency were unavailable, it is likely that most low-income individuals that received services did so through these facilities and were captured in this analysis. DSS data included income maintenance, Medicaid reimbursed mental health care prior to 1995, maltreatment reporting, and child welfare services through March, 2009. Death records were available from vital statistics to allow for censoring out children who died during the study period. A common state-level identifier was available for most of the data; when this common identifier was unavailable matching procedures were used. Data were matched according to personal identifying information, including the first four letters of first and last name, as well as date of birth. Several procedures were followed to ensure accuracy of the match: (1) agency personnel were consulted, (2) results were compared against known and expected rates when available, and (3) data elements existing in multiple data bases were continually checked for inconsistencies. After matching was completed, the PI of the parent study removed all identifiers; hence no personal identifiers were retained in the data analyzed for this study. The study was approved by the Washington University Human Research Protection office.
Sampling
Data were drawn from a larger study of poor and maltreated compared to poverty only children. In the parent study families were limited to those whose children were all under the age of 12 and living at home (not in foster care) at the time of sampling. This age range was chosen to match the only similar study of its kind at the time of initial sampling (Widom, 2000) and to be able to track a child’s first entry into foster care. Moreover, families without older children in the home were selected to preclude contamination of outcomes like delinquency. This decision drew upon peer contagion theory. That is, children whose older siblings had problems may themselves be more likely to develop problems. One child was randomly selected within families; therefore, children were not nested within mothers and observations were independent.
Only the low income and maltreated (as measured by a first maltreatment report in 1993 or 1994) sample group was used. This is because of our focus on understanding families involved in child welfare and because the available mental health data did not include private payer options that would be available to higher income families. Further exclusion criteria were: (1) a limit to children born between 1987 and 1994 because Medicaid data were not available prior to 1987, (2) families with the father identified as the primary caregiver (n=124) because it is rare for father-only families to receive income maintenance and there were too few for multivariate analyses, and (3) families with racial or ethnic identities other than African American or Caucasian (n=40). This group was small due to the demographics of the study region and too heterogeneous to analyze as a single group. A total of 4,895 mother-child dyads were included in analyses.
Outcome measures
Safety was measured by new maltreatment reports made to the DSS Children’s Division (CD) more than 7 days after the first report and before March, 2009. Reports occurring within 7 days were considered to be related to the same incident and not a separate report. Stability was measured by foster care placements occurring after the first report and before March, 2009. Placement could have occurred as a result of the first report or later following a subsequent report. The dates on which the report or placement occurred were obtained from the DSS data. The entire study window was 1993 to 2009---approximately 15 years.
Mental illness measures
Mothers were identified as having a mental disorder if she had: (1) received services from a public or private contract agency reimbursed through Medicaid or other DMH funds, and (2) been assigned the ICD-09/ICD-10 diagnostic code for a diagnosis considered here: schizophrenic disorders, episodic mood disorders (major depressive and bipolar mood disorders), anxiety and dissociative disorders, and personality disorders (borderline and antisocial personality disorders). These diagnoses were selected due to evidence of their influence on parenting, as well as their prevalence rates. Others were available in the data; however, small numbers precluded meaningful subgroup analysis.
Other measures
Maltreatment types of the first report were obtained from the DSS data and classified into physical abuse, neglect or sexual abuse. For the multivariate models dummy coding was used to create two dichotomized categories: neglect (yes/no) or physical abuse (yes/no). Referral to services after the first report included services initiated within 45 days of the report but prior to a second report. Service categories were none, family centered (FC) services, family preservation (FP) services, FP services and foster care, and foster care. FC services included a range of treatment/support services. FP services were intensive, crisis-oriented in-home services provided over a short period of time. The combined FP services and foster care classification was created to account for families that received FP services followed by foster care placement after the first report but before a second report. Census track median income was used as a proxy for family income and was based on 1990 census data (as this was closest to the study start years of 1993 to 1994).
Analysis strategy
Data were analyzed using SAS 9.2. Independent variables in the statistical models were the mental disorders considered in this study. Demographics, census track median income, maltreatment type and services received after first report were included.
Frequencies and means were calculated to describe the sample at the time of the first report. Outcomes for children of mothers with and without mental illness were compared using Pearson chi-square tests. Primary analyses were conducted using event history analysis (Allison, 1995). The Kaplan-Meier method was used to test differences in survival rates according to mental disorders and check for possible violations of proportionality prior to multivariate analyses. Log-rank test of equality was used to test for differences between groups. Survival curves are presented to show the rate of new reports or foster care entry over time. The area under the curves represents those with no recurrence or entry into care. Cox regression modeling was used to examine predictors of new maltreatment reports and foster care placement controlling for a child’s time at risk. We also controlled for clustering by census track to appropriately adjust the standard errors to account for inter-cluster correlations. Hazard ratios (which are interpreted similarly to odds ratios) are reported.
Results
Case characteristics
Mean child age at time of first report was 4.7 years (SD = 3.3); mean age of the parent was 23.7 years (SD = 6.3). Most children were African American (75.8%) and had a mother without a high school degree at the onset of the study (62.8%; Table 1). Child gender was evenly distributed. Two-thirds (67.0%) of families were first reported to child protective services due to neglect compared to 26.1% who were reported for physical abuse and 6.8% who were reported for sexual abuse. Most families did not receive any child welfare services following their first report (79.3%).
Table 1.
Case Characteristics
| Characteristic (number missing) | Frequency | Percent |
|---|---|---|
| Child Gender (0) | … | … |
| Female | 2403 | 49.1 |
| Male | 2492 | 50.9 |
|
| ||
| Child Race (40) | … | … |
| Caucasian | 1174 | 24.2 |
| African American | 3681 | 75.8 |
|
| ||
| Parent High School Education (7) | … | … |
| Less than high school education | 3068 | 62.8 |
| High school education or more | 1820 | 37.2 |
|
| ||
| Maltreatment Type of First Report (3) | … | … |
| Neglect | 3279 | 67.0 |
| Physical abuse | 1279 | 26.1 |
| Sexual abuse | 334 | 6.8 |
|
| ||
| Child Welfare Services Following First Maltreatment Report (0) | … | … |
| None | 3881 | 79.3 |
| Family Centered Services | 608 | 12.4 |
| Family Preservation Services (FPS) | 127 | 2.6 |
| FPS and foster care | 45 | 0.9 |
| Foster Care Placement without FPS | 234 | 4.8 |
One percent of the women in our study (n= 50) were diagnosed with a schizophrenic disorder, 3.0% (n=148) with an episodic mood disorder, 1.6% (n=76) with an anxiety disorder, and 0.9% (n=46) with a personality disorder. Bivariate associations between disorder and outcomes are shown in Table 2. Overall, 67.0% of the children experienced a new maltreatment report and 23.6% had at a foster care placement over the study period. Children of mothers with mental illness were even more likely to have new reports, as well as foster care placements. For each of the diagnoses, between 80 and 90% of the children experienced a new report compared to approximately 66% for children of undiagnosed mothers. At least half of children of mothers with schizophrenic and anxiety disorders experienced foster care placements compared to a quarter of children of undiagnosed mothers.
Table 2.
Association between Maternal Mental Disorder and Safety and Stability Measures
| Diagnosis(ICD-9/ICD-10 Code) | New Maltreatment Report | Foster Care Placement |
|---|---|---|
| Yes | Yes | |
| Total | 67.0% | 23.6% |
|
| ||
| Schizophrenic Disorders (295) | … | … |
| Yes | 80.0%* | 50.0%*** |
| No | 66.9% | 23.3% |
|
| ||
| Episodic Mood Disorders (296) | … | … |
| Yes | 84.5%*** | 39.2%*** |
| No | 66.5% | 23.1% |
|
| ||
| Anxiety and Dissociative Disorders (300) | … | … |
| Yes | 89.5%*** | 52.6%*** |
| No | 66.7% | 23.1% |
|
| ||
| Personality Disorders (301) | … | … |
| Yes | 84.8%** | 47.8%*** |
| No | 66.8% | 23.4% |
p < .05
p < .01
p< .001
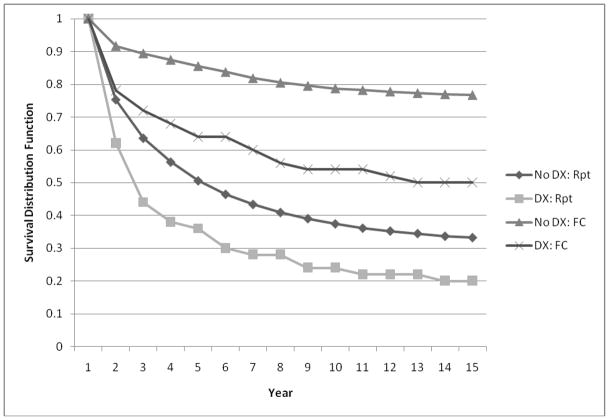
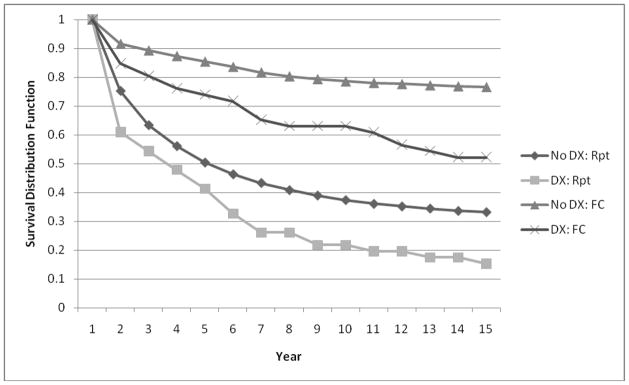
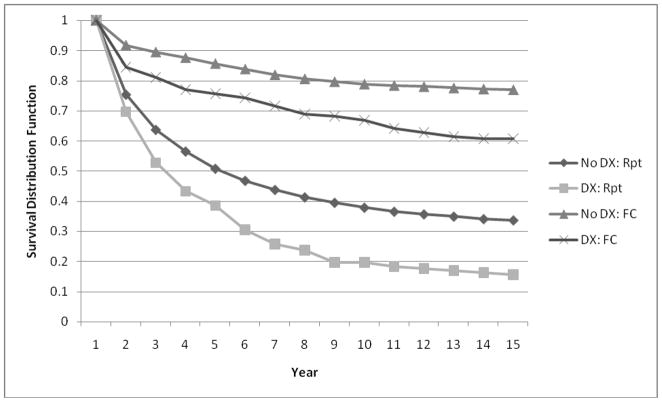
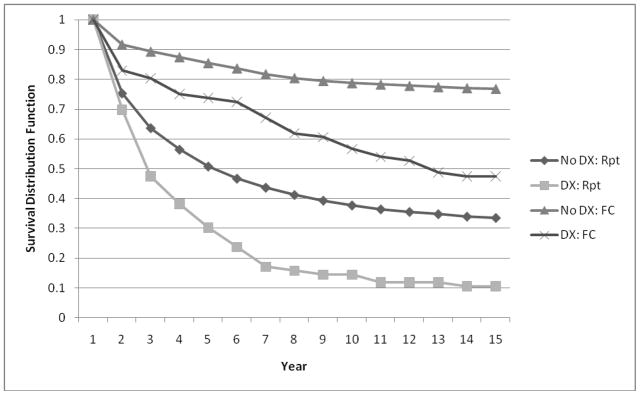
Survivor curves
Survivor curves for new maltreatment reports and foster care placements by mental disorder are shown in Figures 1–4. The x-axis is the time (in years) between study entry and event (i.e., new report or placement into care). The y-axis is the survivor distribution or percentage of cases without the event. New report and foster care placement are included in the same figure; comparisons should only be made between similar events. For example, when interpreting Figure 1, the reader should only compare the lines for no diagnosis: new report to diagnosis: new report. Likewise the reader should only compare the lines for no diagnosis: foster care placement to diagnoses: foster care placement. Times to new report were significantly different for mothers with and without schizophrenic disorders (Figure 1), mood disorders (Figure 2), anxiety disorders (Figure 3) and personality disorders (Figure 4). Children of mothers with diagnosed mental disorders all had higher rates of new reports over time; however, the recurrence rate for children whose mothers had schizophrenic or personality disorders had a much faster initial recurrence rate (as indicated by the steep downward trend in the curve indicating mental health disorder compared to those without). In contrast, the curves of mood disorders and anxiety disorders reveal initially similar patterns of new reports for children of mothers with and without diagnoses. Half of children of mothers with schizophrenic, mood and anxiety disorders experienced a new report prior to 2½ years following the first report. It took approximately 5 years for this proportion of children of undiagnosed mothers to experience a new report. Times to foster care placements were significantly different for mothers with and without schizophrenic disorders (Figure 1), mood disorders (Figure 2), anxiety disorders (Figure 3) and personality disorders (Figure 4). The initial risk was much greater for children of mothers with episodic mood disorders than for children of undiagnosed mothers. The curves then took on a similar shape but with constant differences in survival rates over time.
Figure 1. Survivor Function Estimated by Kaplan Meier Method: Stratified by Schizophrenic Disorders.
New Report: Log Rank chi-square = 7.20, p < .01; Log Rank chi-square = 24.85, p < .001
Note: DX = diagnosis, Rpt = new report, FC = foster care placement. The lines do not represent mutually exclusive groups; cases with a new report may also have a foster care placement.
Figure 4. Survivor Function Estimated by Kaplan Meier Method: Stratified by Personality Disorders.
New Report: Log Rank chi-square = 7.80, p < .01; Log Rank chi-square = 16.19, p < .001
Note: DX = diagnosis, Rpt = new report, FC = foster care placement. The lines do not represent mutually exclusive groups; cases with a new report may also have a foster care placement.
Figure 2. Survivor Function Estimated by Kaplan Meier Method: Stratified by Episodic Mood Disorders.
New Report: Log Rank chi-square = 24.68, p < .001; Log Rank chi-square = 22.68, p < .001
Note: DX = diagnosis, Rpt = new report, FC = foster care placement. The lines do not represent mutually exclusive groups; cases with a new report may also have a foster care placement.
Figure 3. Survivor Function Estimated by Kaplan Meier Method: Stratified by Anxiety Disorders.
New Report: Log Rank chi-square = 23.33, p < .001; Log Rank chi-square = 38.60, p < .001
Note: DX = diagnosis, Rpt = new report, FC = foster care placement. The lines do not represent mutually exclusive groups; cases with a new report may also have a foster care placement.
Cox regression models
When modeling a new maltreatment report as a proxy for safety, episodic mood disorders and anxiety disorders were associated with new reports (Table 3; Wald χ2 [sandwich] = 292.27, p < .001). The statistically significant hazard ratios (HR) of 1.41 and 1.32 indicated that the risk of new reports was higher for children of mothers with mood disorders and anxiety disorders, respectively, compared with children of non-diagnosed mothers. Although bivariate analyses revealed an increased risk for new reports among children of mothers with schizophrenic or personality disorders, the increased risk was mitigated when controlling for other case characteristics in the multivariate model. Other variables were significant in the model. For every $10,000 increase in the median family income within the census track in which the family lived, the risk of a new report was lowered (HR = 0.91). Additionally, for every one year increase in the child’s age, the risk of a new report was lowered slightly (HR = 0.98). Children of mothers without a high school education (HR = 1.23) and whose first report was for neglect (HR = 1.27) were more likely to have a new report. Receiving FC services immediately after a first report was also associated with a lower risk of re-report (HR = 0.52). Of note, when income and other case characteristics were taken into account within the multivariate models, African American children were less likely to have a new report than Caucasian children (HR = 0.89).
Table 3.
Cox Regression Models of Safety and Stability
| New Maltreatment Report | Foster Care Placements | |
|---|---|---|
| Hazard Ratio (95% CI) | Hazard Ratio (95% CI) | |
| Census track median income | 0.91 (0.87, 0.94)*** | 0.85 (0.80, 0.91)*** |
| Child age | 0.98 (0.96, 0.99)*** | 0.94 (0.92, 0.96)*** |
| Child race (African American: Caucasian) | 0.89 (0.81, 0.97)* | 1.26 (1.07, 1.48)** |
| Child gender (Male: female) | 1.00 (0.93, 1.07) | 1.06 (0.94, 1.19) |
| Mother age | 1.00 (0.99, 1.01) | 1.03 (1.02, 1.04)*** |
| Mothers education (less than high school education: high school or more) | 1.23 (1.14, 1.33)*** | 1.34 (1.18, 1.53)*** |
| Physical abuse (yes: no) | 1.11 (0.95, 1.29) | 1.25 (0.93, 1.67) |
| Neglect (yes: no) | 1.27 (1.10, 1.47)*** | 1.24 (0.94, 1.63) |
| Family centered services (yes: no)a | 0.52 (0.47, 0.59)*** | … |
| Schizophrenic Disorders (yes: no) | 1.02 (0.70, 1.48) | 1.37 (0.83, 2.25) |
| Episodic Mood Disorders (yes: no) | 1.41 (1.16, 1.73)*** | 1.16 (0.79, 1.70) |
| Anxiety Disorders (yes: no) | 1.32 (1.01, 1.73)* | 1.75 (1.18, 2.60)** |
| Personality Disorders (yes: no) | 0.97 (0.68, 1.40) | 1.26 (0.76, 2.10) |
Some children went into foster care after the first report resulting in a 0 probability of receiving Family Centered Services after the first report. This variable was therefore excluded from the foster care placement model.
p<.05
p<.01
p<.001
When modeling entry into foster care as a proxy for stability (Wald χ2 [sandwich] = 210.16, p < .001), children of mothers with anxiety disorders were more likely to have foster care placements than children of undiagnosed mothers (HR = 1.75); the other diagnoses were not significant in this model. African American children were 1.3 times more likely to be placed in foster care than Caucasian children (HR = 1.26); younger children had a higher risk of placement than older children (HR = 0.94). Children of mothers without a high school education were more likely to be placed into foster care than children of mothers with a high school education (HR = 1.34). The risk of a foster care placement was substantially lowered for families living in census tracts with higher median incomes (HR = 0.85).
Discussion
This study is strengthened by its ability to follow low income families for 15 years and provides insight into the risk to child safety and stability introduced by maternal mental illness. At first glance it appears that the rates of mental disorders found in this study of families who have entered the child welfare system are substantially lower than national estimates for all but schizophrenic disorders, which are 1% here and in the general population (Regier et al., 1993). However, the national estimates of episodic mood disorders and anxiety disorders are based on self-report measures (Kessler et al., 2005). DMH data were used in the current study to identify mothers with a diagnosis received through a mental health service system. It is likely that we capture the more serious cases. Comparisons with national estimates confirm this. Kessler and colleagues (2005) report prevalence rates of 4% for serious anxiety disorders, 2% for major depressive episode and 2% for bipolar disorder (4% for major depression and bipolar disorders combined). These estimates are much closer to our findings. Mothers with more severe disorders may be those who pose the greatest threat to their children’s safety and stability. Furthermore, the majority of mothers were diagnosed after the first maltreatment report---an indication that child welfare entry may serve as a gateway to mental health services for some mothers.
Although the sample was comprised entirely of low income families, variability in income (as measured by the census track median income) contributed to the safety and stability of children. Children living in census tracks with lower median income were at greater risk for both new maltreatment reports and placement into foster care.
Mental illness and reports
Analyses supported our first hypothesis. Overall, findings indicate that following low income families who have been reported for child maltreatment for many years yields high rates of recurrent maltreatment. In fact, two-thirds of the families in our study had at least 1 new report between 1993 and 2009. This risk was even higher for children of mothers with mental illness. Analyses also determined that recurrence rates varied by diagnosis.
The increased risk associated with schizophrenia and personality disorders was no longer significant when statistically controlling for demographics, case characteristics and other disorders; mood and anxiety disorders remained significant. This finding suggests that these two disorders are particularly potent as predictors of new reports. That depression is important is consistent with extant literature. Comparisons are not possible for anxiety due to lack of literature. Given its import, this relationship warrants further research to determine if this is consistent for other populations and regions.
Mental illness and foster care
African American children were more likely to be placed in foster care than Caucasian children. The over-representation of Black children in foster care has been clearly demonstrated elsewhere (Derezotes & Poertner, 2005) and further discussion of this relationship is outside the scope of the current study. Our second hypothesis was also confirmed. The risk of foster care placement was higher for children of mothers with mental illness than for children of mothers without mental illness. Consistent with the literature (Burton, 2009; Nicholson et al., 2001), we found high rates of foster care placement for children of mothers with mental illness. Again variation was found by diagnosis. Depending on the diagnosis, up to half of children experienced at least 1 foster care placement; the highest rates were for children of mothers with schizophrenia or anxiety. These high rates are more than twice the rate for other children. The risks associated with each disorder except anxiety, however, are diminished when statistically accounting for other characteristics and disorders. Foster care placement was nearly twice as likely for children of mothers with anxiety disorders. The role of anxiety as a strong indicator is consistent for both safety and stability. Schizophrenia’s lack of significance is surprising given other findings that placement is highly associated with this disorder (Burton, 2009). This may, in part, be associated with the fact that these mothers are receiving services. It is possible that greater attention is given to parents with such disorders or that they have assistance in the home from another caretaker.
The non-significance of some disorders in our statistical models suggests that it is not the disorder itself that impedes safety and stability, but it is the contribution of other factors---unmeasured in this study---that coexist in households with maternal mental illness. Further investigation is needed to better understand the complex associations between mental illness and maltreatment risk.
Limitations
It is possible that mothers in the study had received mental health services and been diagnosed with a mental disorder through a non-publicly funded agency and were not captured in the study. Although this may result in an underestimation of mental illness, we believe that we have largely mitigated this by limiting study inclusion to low income families. Further if this was occurring for significant numbers of mothers in the non-diagnosed group, one would expect a lack of significant differences. This was not the case. We also were unable to include information about severity and chronicity of mental disorders or treatment quality. Small sample sizes prevented our ability to separately analyze outcomes according to whether the initial diagnosis occurred prior to the first contact with child welfare or after. Future studies should attempt to examine whether the timing of mental health services has an effect on safety and stability. Small sample sizes may also have impeded our power to detect significant differences. That is, if we had higher numbers of mothers with schizophrenia and personality disorders in our data, it is possible that the hazard ratios for these two disorders for foster care placement would have been statistically significant.
Our 15-year follow-up period is a positive attribute of the study; however, it does also introduce the potential for sample attrition due to mobility. These concerns are diminished by analysis of the parent study’s complete dataset which demonstrated that families in the study are mobile, but typically only move short distances. Therefore, we believe the vast majority do not relocate outside of the area. Furthermore, the metropolitan region from which our sample was drawn has very low levels of outmigration (Tranel, 2000). While the multi-sector administrative database allowed us to include specific information not available elsewhere, it precluded the inclusion of some potentially informative contextual information. We were unable to assess the role of protective factors such as realistic expectations about children, ability to read children’s cues and social support, and additional risk factors such as parental stress (Azar, Robinson, Hekimian, & Twentyman, 1984; Crittenden, 1988; Belsky, 1993). These factors may have mediated the relationship between mental disorder and child outcomes. Additionally, data on families’ actual income were unavailable in the dataset. Although inclusion of census track median income strengthened our analyses, it is a proxy measure and lacks precision.
Practice implications
Maternal mental illness impedes the long term safety and stability of children in the child welfare system. Study implications extend beyond the need for improved access to mental health services. Analysis of this services data provided the opportunity to examine outcomes for children of mothers with mental illness who had already accessed mental health services. While it is possible that following an initial diagnosis, the mental illness may have spontaneously remitted or responded positively to treatment, the large differences in safety and stability found between children of mothers with and without mental disorders suggest that access to services is not enough. The services they are receiving are either ineffective or are insufficient. Coordination between child welfare and adult mental health services is necessary (Alakus, Conwell, Gilbert, Buist, & Castle, 2007; Nicholson et al., 2001). Mental health practitioners may be unaware that their client is a parent and mothers may be reluctant to disclose problems they are having with their children (Cowling, Luk, Mikeshkin, & Brileson, 2004). Better assessment of parenting competence is needed (Ackerson, 2003; Mowbray et al., 2002). Emerging efforts have begun that seek to develop interventions to meet maternal mental health needs and promote safe and stable environments for their children (Nicholson, Hinden, Biebel, Henry, & Katz-Leavy, 2007). Additional efforts are needed to further test these interventions and to disseminate them more broadly.
Acknowledgments
This work was funded by the National Institute of Mental Health, RO1 MH 061733-04 A1.
Footnotes
Points of view and opinions expressed here are the authors’ and do not necessarily express the views or opinions of the funding agency
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- Ackerson BJ. Parents with serious and persistent mental illness: Issues in assessment and services. Journal of Social Work. 2003;48(2):187–194. doi: 10.1093/sw/48.2.187. [DOI] [PubMed] [Google Scholar]
- Alakus C, Conwell R, Gilbert M, Buist A, Castle D. The needs of parents with a mental illness who have young children: An Australian perspective on service delivery options. International Journal of Social Psychiatry. 2007;53(4):333–339. doi: 10.1177/0020764006074543. [DOI] [PubMed] [Google Scholar]
- Allison P. Survival analysis using the SAS System: A practical guide. Cary, NC: SAS Institute; 1995. [Google Scholar]
- Azar ST, Robinson DR, Hekimian E, Twentyman CT. Unrealistic expectations and problem solving ability in maltreating and comparison mothers. Journal of Consulting and Clinical Psychology. 1984;52:687–691. doi: 10.1037//0022-006x.52.4.687. [DOI] [PubMed] [Google Scholar]
- Belsky J. Etiology of child maltreatment: a developmental-ecological analysis. Psychological Bulletin. 1993;114:413–434. doi: 10.1037/0033-2909.114.3.413. [DOI] [PubMed] [Google Scholar]
- Brown J, Cohen P, Johnson JG, Salzinger S. A longitudinal analysis of risk factors for child maltreatment: Findings of a 17-year prospective study of officially recorded and self-reported child abuse and neglect. Child Abuse & Neglect. 1998;22:1065–1078. doi: 10.1016/s0145-2134(98)00087-8. [DOI] [PubMed] [Google Scholar]
- Burton VS. The consequences of official labels: A research note on rights lost by the mentally ill, mentally incompetent, and convicted felons. Community Mental Health Journal. 1990;26(3):267–276. doi: 10.1007/BF00752777. [DOI] [PubMed] [Google Scholar]
- Chaffin M, Kelleher K, Hollenberg J. Onset of physical abuse and neglect: Psychiatric, substance abuse, and social risk factors from prospective community data. Child Abuse & Neglect. 1996;20(3):191–203. doi: 10.1016/s0145-2134(95)00144-1. [DOI] [PubMed] [Google Scholar]
- Chung EK, McCollum KF, Elo IT, Lee HJ, Culhane JF. Maternal depressive symptoms and infant health practices among low-income women. Pediatrics. 2004;113:e523–e529. doi: 10.1542/peds.113.6.e523. [DOI] [PubMed] [Google Scholar]
- Compton WM, Conway KP, Stinson FS, Colliver JD, Grant BF. Prevalence, correlates and comorbidity of DSM-IV antisocial personality syndromes and alcohol and specific drug use disorders in the United States: Results from the National Epidemiologic Survey on Alcohol and related conditions. Journal of Clinical Psychiatry. 2005;66:677–685. doi: 10.4088/jcp.v66n0602. [DOI] [PubMed] [Google Scholar]
- Cowling V, Luk ESL, Mikeshkin C, Brileson P. Children of adults with several mental illness: mental health, help seeking and service use. Psychiatric Bulletin. 2004;28:43–46. [Google Scholar]
- Crittenden PM. Relationship at risk. In: Belsky J, Nezworski TH, editors. Clinical implications of attachment. Hillsdale, NJ: Erlbaum; 1988. pp. 136–176. [Google Scholar]
- DePanfilis D, Zuravin SJ. Rates, patterns, and frequency of child maltreatment recurrences among families known to CPS. Child Maltreatment. 1998;3:27–42. [Google Scholar]
- Derezotes DM, Poertner J. Factors contributing to the overrepresentation of African American children in the child welfare system. In: Derezotes DM, Poertner J, Testa MF, editors. Race matters in child welfare: The overrepresentation of African American children in the system. Washington DC: Child Welfare League of America, Inc; 2005. pp. 1–23. [Google Scholar]
- Drake B, Zuravin S. Bias in child maltreatment reporting: Revisiting the myth of classlessness. American Journal of Orthopsychiatry. 1998;68(2):295–304. doi: 10.1037/h0080338. [DOI] [PubMed] [Google Scholar]
- English DJ, Marshall DB, Brummel S, Orme M. Characteristics of repeated referrals to child protective services in Washington state. Child Maltreatment. 1999;4:297–307. [Google Scholar]
- Fluke JD, Yuan YY, Edwards M. Recurrence of maltreatment: An application of the National Child Abuse and Neglect Data System (NCANDS) Child Abuse & Neglect. 1999;23:633–650. doi: 10.1016/s0145-2134(99)00039-3. [DOI] [PubMed] [Google Scholar]
- Goodman SH, Brumley HE. Schizophrenic and depressed mothers: Relational deficits in parenting. Developmental Psychology. 1990;26(1):31–39. [Google Scholar]
- Hoagwood K, Horwitz S, Stiffman A, Weisz J, Bean D, Rae D, Compton W, Cottler L, Bickman L, Leaf P. Concordance between parent reports of children’s mental health services and service records: The services assessment for children and adolescents (SACA) Journal of Child and Family Studies. 2000;9(3):1062–1024. [Google Scholar]
- Kessler RC, Chiu WT, Demler O, Walters EE. Prevalence, severity, and comorbidity of twelve-month DSM-IV disorders in the National Comorbidity Survey Replication (NCS-R) Archive of General Psychiatry. 2005;62(6):617–627. doi: 10.1001/archpsyc.62.6.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotch JB, Browne DC, Dufort V, Winsor J. Predicting child maltreatment in the first 4 years of life from characteristics assessed in the neonatal period. Child Abuse & Neglect. 1999;23(4):305–319. doi: 10.1016/s0145-2134(99)00003-4. [DOI] [PubMed] [Google Scholar]
- Lewin L, Abdrbo A. Mothers with self-reported axis I diagnoses and child protection. Archives of Psychiatric Nursing. 2009;23(3):200–209. doi: 10.1016/j.apnu.2008.05.011. [DOI] [PubMed] [Google Scholar]
- Mowbray C, Oyserman D, Bybee D, MacFarlane P. Parenting of mothers with a serious mental illness: Differential effects of diagnosis, clinical histories and other mental health variables. Social Work Research. 2002;26(4):225–240. [Google Scholar]
- Lovejoy MC, Craczyk PA, O’Hare E, Neuman G. Maternal depression and parenting behavior: A meta-analytical review. Clinical Psychology Review. 2000;20:561–592. doi: 10.1016/s0272-7358(98)00100-7. [DOI] [PubMed] [Google Scholar]
- Lyons-Ruth K, Wolfe R, Lyubchik A, Steingard R. Depressive symptoms in parents of children under age three: Sociodemographic predictors, current correlates, and associated parenting behaviors. In: Halfon N, McLearn KT, Schuster MA, editors. Child rearing in America: Challenges facing parents with young children. New York: Cambridge University Press; 2002. pp. 217–259. [Google Scholar]
- Moore PS, Whaley SE, Sigman M. Interactions between mothers and children: Impacts of maternal and child anxiety. Journal of Abnormal Psychology. 2004;113:471–476. doi: 10.1037/0021-843X.113.3.471. [DOI] [PubMed] [Google Scholar]
- Newman LK, Stevenson CS, Bergman LR, Boyce P. Borderline personality disorder, mother-infant interaction and parenting perceptions: Preliminary findings. Australian and New Zealand Journal of Psychiatry. 2007;41:598–605. doi: 10.1080/00048670701392833. [DOI] [PubMed] [Google Scholar]
- Nicholson J, Beibel K, Hinden B, Henry A, Stier L. Critical issues for parents with mental illness and their families. Report prepared for the Center for Mental Health Services, Substance Abuse and Mental Health Services Administration, Office of Policy, Planning and Administration; 2001. Retrieved online on July 14, 2009 from http://mentalhealth.samhsa.gov/publications/allpubs/KEN-01-0109.default. [Google Scholar]
- Nicholson J, Hinden BR, Biebel K, Henry AD, Katz-Leavy J. A qualitative study of programs for serious mental illness and their children: Building practice-based evidence. Journal of Behavioral Health Services and Research. 2007;10(3):51–65. doi: 10.1007/s11414-007-9063-5. [DOI] [PubMed] [Google Scholar]
- Park JM, Solomon P, Mandell DS. Involvement in the child welfare system among mothers with serious mental illness. Psychiatric Services. 2006;57:493–497. doi: 10.1176/ps.2006.57.4.493. [DOI] [PubMed] [Google Scholar]
- Regier DA, Narrow WE, Rae DS, Manderscheid RW, Locke BZ, Goodwin FK. The de facto US mental and addictive disorders service system. Epidemiologic catchment area prospective 1-year prevalence rates of disorders and services. Archives of General Psychiatry. 1993;50(2):85–94. doi: 10.1001/archpsyc.1993.01820140007001. [DOI] [PubMed] [Google Scholar]
- Sheppard M. Double jeopardy: The link between child abuse and maternal depression in child and family social work. Child and Family Social Work. 1997;2:91–107. [Google Scholar]
- Shin DW, Stein MA. Maternal depression predicts maternal use of corporal punishment in children with attention–deficit/hyperactivity disorder. Yonsei Medical Journal. 2008;49:573–580. doi: 10.3349/ymj.2008.49.4.573. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons RL, Beaman J, Conger RD, Chao W. Stress, support and antisocial behavior trait as determinants of emotional well-being and parenting. Journal of Marriage and Family. 1993;55(2):385–398. [Google Scholar]
- Swartz M, Blazer D, George L, Winfield I. Estimating the prevalence of borderline personality disorder in the community. Journal of Personality Disorders. 1990;4(3):257–72. [Google Scholar]
- Tranel M. PPRC In The News. Public Policy Research Center; St. Louis, MO: 2000. Sep, Concentration on city loss obscures regional problem. [Google Scholar]
- US Department of Health and Human Services, Administration on Children, Youth, and Families (US DHHS ACF) National survey of child and adolescent well-being (NSCAW): CPS sample component Wave 1 eata analysis report. Washington, DC: US Government Printing Office; 2005. [Google Scholar]
- Walsh C, MacMillan H, Jamieson E. The relationship between parental psychiatric disorder and child physical and sexual abuse: Findings from the Ontario Health Supplement. Child Abuse & Neglect. 2002;26(2):11–22. doi: 10.1016/s0145-2134(01)00308-8. [DOI] [PubMed] [Google Scholar]
- Widom C. Understanding the consequences of childhood victimization. In: Reece R, editor. Treatment of child abuse: Common ground for mental health, medical and legal practitioners. Baltimore: Johns-Hopkins University Press; 2000. pp. 339–361. [Google Scholar]
- Widom CS, Raphael K, DuMont K. The case for prospective longitudinal studies in child maltreatment research: Commentary on Dube, Williamson, Thompson, Felitti, & Anda. Child Abuse & Neglect. 2004;28:715–722. doi: 10.1016/j.chiabu.2004.03.009. [DOI] [PubMed] [Google Scholar]
- Windham AM, Rosenberg L, Fuddy L, McFarlane E, Sia C, Duggan AK. Risk of mother-reported child abuse in the first 3 years of life. Child Abuse & Neglect. 2004;28(6):645–667. doi: 10.1016/j.chiabu.2004.01.003. [DOI] [PubMed] [Google Scholar]
- Woodruff-Borden J, Morrow C, Bourland S, Cambron S. The behavior of anxious parents: Examining mechanisms of transmission of anxiety from parent to child. Journal of Clinical Child and Adolescent Psychiatry. 2002;31:364–374. doi: 10.1207/S15374424JCCP3103_08. [DOI] [PubMed] [Google Scholar]