Abstract
Objective
To examine whether benefit finding was associated with better adjustment among adolescents with diabetes by buffering negative affective reactions to diabetes stress and by promoting positive affective reactions.
Design
Early adolescents aged 10-14 with type 1 diabetes (n=252) described recent diabetes stressors, affective reactions, and perceived coping effectiveness. They also completed measures of benefit finding, depressive symptoms, and adherence. Metabolic control (i.e., HbA1c) was obtained from medical records.
Main Outcome Measures
The main outcome measures were perceived coping effectiveness, depressive symptoms, adherence, and HbA1c.
Results
Benefit finding was associated with lower depressive symptoms, higher perceived coping effectiveness and better adherence, and with higher positive as well as negative affective reactions to diabetes stress. Benefit finding interacted with negative affective reactions to predict depressive symptoms and HbA1c. Negative affective reactions to stress were associated with poorer adjustment among those with low benefit finding, but were unrelated or more weakly related to poor adjustment among those with high benefit finding. Positive affective reactions did not mediate associations between benefit finding and any outcome.
Conclusions
Consistent with a stress-buffering process, benefit finding may be a resource that buffers the disruptive aspects of negative affective reactions to stress for adolescents’ diabetes management.
Keywords: benefit finding, diabetes, adolescence, stress, coping, positive and negative affect
Adolescence is a difficult time for managing type 1 diabetes as evidenced by deteriorating metabolic control, poorer adherence, and heightened emotional distress (Helgeson, Snyder, Escobar, Siminerio, & Becker, 2007; Korbel, Wiebe, Berg, & Palmer, 2007). Such difficulties may occur, in part, because the increases in negative affect and emotional lability that occur normatively during adolescence (Larson, Moneta, Richards, & Wilson, 2002) may be exacerbated by the stress of diabetes, and may undermine diabetes self-management (de Groot, Anderson, Freedland, Clouse, & Lustman, 2001; Holmes et al., 2006). Understanding factors that predict these diabetes management patterns is important because self-management behaviors established during adolescence may carry into adulthood (Dovey-Pearce, Doherty, & May, 2007; Ickovics et al., 2006). We examined how one potential factor – benefit finding – is related to affective reactions to diabetes stress and to diabetes management among early adolescents with type 1 diabetes. Defined as the experience of identifying positive outcomes in the face of adversity, benefit finding has often been examined as a factor in positive emotional adjustment to illness (Helgeson, Reynolds, & Tomich, 2006; Linley & Joseph, 2004). Study of benefit finding among adolescents is limited (see Helgeson, Lopez, & Mennella, 2009 for review), but we theorized it may be an important resource for adolescents with diabetes particularly because it has been implicated in illness-related affective experiences.
Benefit finding has been associated with better psychosocial well-being and lower affective distress in numerous chronic illness populations such as cancer, HIV/AIDS, multiple sclerosis, and rheumatoid arthritis (see Algoe & Stanton, 2009 for review). In some instances, however, benefit finding is unrelated or even negatively related to emotional well-being, and the processes by which it may be adaptive remain unclear (Helgeson et al., 2006; Mohr et al., 1999; Tomich & Helgeson, 2004). These inconsistencies have raised questions about whether benefit finding is an effective resource for adapting to illness or whether it is primarily a cognitive defense to manage negative emotion (Affleck & Tennen, 1996; Park & Helgeson, 2006; Siegel & Schrimshaw, 2007). It is possible that benefit finding serves both functions by developing in a context of illness-related distress, but once developed, working to buffer the adverse consequences of negative affective experiences.
Benefit finding is based on the theory that the experience of adversity can alter one’s views of the self and the world, generating distress and anxiety; through re-evaluating these views, however, a new sense of meaning and self-worth can emerge (Janoff-Bulman & Frieze, 1983; Taylor, 1983). This meaning-making process may be accompanied by periods of stress and tumult, as individuals accommodate adverse circumstances into their understanding of themselves and the world, and set new life goals and priorities. If benefit finding develops in this context of distress, the result may be a positive relationship between benefit finding and negative affect. To the extent that these experiences of change and growth are adaptive, however, benefit finding should ultimately be associated with improved well-being and may buffer negative affect by allowing adolescents to positively reframe the meaning of their diabetes-related distress (Pakenham, 2005; Siegel & Schrimshaw, 2007). The primary objective of the present study was to examine whether benefit finding buffers the adverse associations between negative affective reactions to diabetes stress and adolescent well-being.
In addition to examining benefit finding as a moderator of negative affect, it is important to consider how benefit finding may interface with positive affect. A large literature suggests positive affect is distinct from negative affect, rather than opposite ends of a single continuum, and is related to well-being through different processes. Benefit finding is consistently associated with enhanced positive affect (Hart, Vella, & Mohr, 2008), and the ability to maintain positive affect in the face of diabetes stress may facilitate adolescents’ diabetes management. Limited research has focused on the role of positive emotions for promoting illness management, but positive affect has been argued to facilitate creative problem-solving and greater access to coping resources (Aspinwall, 1998; Folkman, 2008; Fredrickson, 2001). Fortenberry et al. (Fortenberry, Butler, Butner, Berg, Upchurch, & Wiebe, 2009) found support for this possibility among adolescents with diabetes. Specifically, daily experiences of positive affect were associated with enhanced perceptions of competence in managing diabetes-related problems which, in turn, predicted better daily blood glucose control among adolescents with diabetes. If benefit finding is related to greater positive affective reactions to diabetes stress, this may be reflected in higher coping effectiveness and better illness management. A second objective of this study was to examine whether positive affect mediates associations between benefit finding and better diabetes self-management.
Adolescence provides an important opportunity for studying benefit finding given the cognitive, social, and emotional changes that occur during this time of development. Future-oriented thoughts and concerns develop during early adolescence (Massey, Gebhardt, & Garnefski, 2008), which may provide a context for benefit finding to emerge as youth begin to grapple with the long-term implications of their illness. Early adolescents also have newly acquired secondary coping skills to manage the psychological implications of their illness (Band & Weisz, 1990; Seiffge-Krenke, Aunola, & Nurmi, 2009), which may involve efforts to make sense of the illness and frame one’s developing self-conceptions to accommodate illness-related stressors and challenges. Such developments in stress and coping, coupled with the heightened emotional lability of adolescents in general (Larsen et al., 2002), makes benefit finding a potentially important resource for adolescents. In the present study, we explored age-related differences in benefit finding among early adolescents with diabetes. Although the paucity of research on benefit finding among children and adolescents prevented us from making strong predictions, we thought it plausible that benefit finding would increase or have stronger associations as adolescents’ cognitive and abstract thinking skills matured.
In summary, the present study examined whether benefit finding buffers negative affective reactions and facilitates positive affective reactions to diabetes stress, and whether these associations are reflected in lower depressive symptoms, higher coping effectiveness, and better adherence and blood glucose control. Early adolescents provided detailed descriptions of recent diabetes-related stress, and reported their coping and affective responses to these stressful events. We predicted that: 1) benefit finding would buffer the adverse associations between stress-related negative affect and broader outcomes, suggesting that negative affect is less disruptive when adolescents endorse higher benefit finding; and 2) benefit finding would be associated with higher positive affect in the context of diabetes stress, which would mediate associations with higher perceived coping effectiveness and adherence.
Method
Participants
The study was approved by the appropriate Institutional Review Board. Parents gave written informed consent and adolescents gave written assent. Participants included 252 adolescents (M age = 12.49 years, SD = 1.53, 53.6% females) diagnosed with type 1 diabetes recruited from a university/private partnership clinic (76%) and a community-based private practice (24%). Eligibility criteria included adolescents who were between 10 and 14 years of age, able to read and write either English or Spanish at the 4th grade level, and had diabetes for at least one year (M = 4.13 years, SD = 3).
Of the qualifying individuals approached, 66% agreed to participate in the study, the first wave of a 3-year longitudinal study. Refusals included travel distance 18%, too busy 21%, not interested 30%, uncomfortable with being studied 14%, and the time commitment required 5%. Comparisons of eligible adolescents who did versus did not participate indicated participants were older (12.5 versus 11.6 years, t(367)=-6.2, p < .01), but did not differ on gender, insulin pump status, HbA1c, or time since diagnosis (ps > .20). Approximately half (50.8%) of adolescents were on an insulin pump, with the remainder prescribed multiple daily injections (MDI). Mothers of adolescents on MDI reported physicians recommended an average of 4.14 insulin injections (SD = 1.81) and 5.53 blood glucose checks per day (SD = 1.70). Families were largely Caucasian (94%) and middle class; 73% reported household incomes averaging $50,000 or more annually, and the sample had an average Hollingshead index (1975) of 42.04, indicating a medium business, minor professional, technical status.
Procedure
Participants were recruited during a routine diabetes clinic visit. Interested participants were scheduled for a separate lab appointment and received a packet of questionnaires to be completed individually and returned. At the lab appointment, participants completed an audiotaped Stress and Coping Interview, along with additional questionnaires.
Participants first recalled one thing they did each day of the past week to remind them of the week’s events. They then reported the two most stressful episodes of that week regarding their diabetes (Berg et al., 2009; Wiebe et al., 2005). They were asked to “describe the event in detail from beginning to end so that someone who has never experienced the event would understand what happened.” If adolescents could not think of a stressful event dealing with the diabetes, they were prompted with examples; if they still could not think of a diabetes event, they described the most stressful event of the week. Participants overwhelmingly described diabetes-stressors (96.2% of the first stressors were diabetes-related, 89.3% of the second). After describing each event, participants rated their emotional reactions as well as their perceived coping effectiveness as described below.
Measures
Affective reactions to diabetes stressors
After describing each stressor, adolescents rated how much they had experienced each of eight emotions using a 5-point scale ranging from 1 (not at all) to 5 (extremely). Two descriptors reflected the emotions of anxiety (anxious, nervous), anger (angry, mad), happiness (happy, excited), and sadness (sad, depressed). Means were computed across the two descriptors for each emotion per stressor, and subjected to a principal components analysis with varimax rotation. Three components with eigenvalues > 1 revealed a Depressive Affect factor consisting of the sadness and anger items across both stressors (eigenvalue = 2.58, 32% variance explained, α = .86), an Anxiety factor consisting of the anxiety items across both stressors (eigenvalue = 1.78, 22% variance explained, α = .69), and a Positive Affect (PA) factor consisting of the happy and excited items across both stressors (eigenvalue = 1.10, 14% variance explained, α = .78). Although we had expected the negative affect items to load on a single factor, and had no a priori hypotheses regarding different aspects of negative affect, the anxious and depressive affect scores were only modestly correlated, r = .26, p < .01. Thus, these scores were analyzed separately. Average scores across relevant items were computed to index PA, anxiety, and depressive affect reactions to stress.
Perceived Coping Effectiveness
After adolescents described each event, they rated how well they handled the event (1 = very bad to 5 = very good) (Berg et al., 2009). Ratings across the two stressors were averaged to create a single coping effectiveness score.
Benefit Finding
Participants reported on the benefits of diabetes using Antoni et al.’s (2001) 16-item benefit finding scale; one item was eliminated because it was not applicable to children or early adolescents (“Having diabetes has made me realize the importance of planning my family’s future”). Participants rated agreement with each benefit using a 1 (not at all) to 5 (extremely) scale. This scale required a 4th grade reading level, making it relevant to our sample. It should be noted that the recently developed Benefit Finding Scale for Children (Phipps, Long, & Ogden, 2007), which includes numerous items from the presently used scale, was unavailable at the time of data collection. A principal components analysis revealed one large factor (eigenvalue = 6.15, 38% variance explained) with good internal consistency (α = .89). Because limited research exists on benefit finding among children and adolescents, participants were allowed to list additional benefits to ensure the inclusion of personally-relevant benefits. Additional benefits were reported by 24% of adolescents. Content coding (Fortenberry et al., 2008) revealed adolescents most commonly reported perceiving increases in maturity and independence as an additional benefit of diabetes (e.g. “Makes me feel more independent”), but also elaborated on existing themes such as improved relationships (e.g., “It has really brought my family a lot closer,” “Friendships have grown”), and the development of personal characteristics (e.g., “Being able to accept change easily”) or world views (e.g., “It has taught me that not all things in life are good and go your way”). Scores across all items – including freely reported items - were averaged such that higher scores indicated higher benefit finding.
Symptoms of Depression
The Children’s Depression Inventory (Kovacs, 1985) was completed to indicate the extent to which adolescents experienced depressive symptoms (e.g., disturbances in mood, self-evaluation, interpersonal behaviors) in the past two weeks. This 27-item scale has high internal consistency and test-retest reliability, > .71, and is related to difficulties in managing diabetes (Korbel et al., 2007); present reliability was strong (α =.84)
Adherence
Participants individually completed the 14-item Self Care Inventory (La Greca, Follansbee, & Skyler, 1990) to assess adherence to various aspects of the diabetes regimen over the preceding month. The scale correlates well with more time-intensive interview methods for measuring adherence (La Greca et al., 1990). The scale was adapted to reflect current diabetes regimens (i.e., adding items for counting carbohydrates and calculating insulin doses based on carbohydrates) by a certified diabetes educator and a patient with type 1 diabetes. Reliability in the present study was excellent (α =.85).
Metabolic Control
As part of the routine clinic visit, participants’ glycosylated hemoglobin (HbA1c) levels were obtained. HbA1c provides information on average blood glucose levels over the preceding three or four months, and is the current standard to index whether diabetes treatment goals are being achieved (higher levels indicate poorer control). The average HbA1c level was 8.35 (1.58); 7% or lower is the target for good control (American Diabetes Association, 2009). At all clinics, HbA1c was obtained using the Bayer DCA2000 by clinic staff. Parent authorization provided access to children’s medical records to obtain HbA1c as well as other pertinent illness information (e.g., illness duration, insulin pump treatment).
Analysis plan
Correlations were initially conducted to identify potential covariates, and discern age-related differences in study variables. Multiple regression analyses were conducted to test the primary hypotheses; in all cases, the residuals were normally distributed and unrelated to the predicted values, supporting the assumptions underlying regression. Hierarchical regression analyses were conducted to examine whether benefit finding moderated associations between negative affective reactions and each outcome variable. In these analyses, covariates, benefit finding, and affective reactions to diabetes stress were mean centered (Cohen & Cohen, 1983) and entered on the first step of the equation, and the benefit finding X affect interaction term was entered on the second step. Significant interactions were interpreted by plotting the predicted means at M ± 1 sd for each variable, and then testing the significance of each simple slope (Aiken & West, 1991; Preacher, Curran, & Bauer, 2006). To examine whether the anxiety and depressive affective reactions variables were independently associated with outcomes, analyses for each negative affect variable were conducted while covarying the second variable. Mediation analyses were conducted to examine whether benefit finding associations with each outcome variable were mediated by PA reactions to diabetes stress. Following recommendations of Baron and Kenny (1986), a series of regression analyses determined whether benefit finding predicted the outcome variable (i.e., depressive symptoms, coping effectiveness, adherence, HbA1c), and the mediator (i.e., PA), and whether the association between benefit finding and the outcome was eliminated or reduced when the mediator was entered simultaneously. Finally, interactions between benefit finding and age were conducted to explore age-related differences.
Results
Descriptive statistics and correlations among study variables are reported in Table 1. Benefit finding was correlated with lower depressive symptoms, better adherence, and greater perceived coping effectiveness, but was not correlated with HbA1c. Benefit finding was also associated with higher levels of both positive and negative affective reactions to diabetes stress. PA reactions were correlated with higher perceived coping effectiveness, but were unrelated to other outcomes. Depressive affective reactions were associated with higher symptoms of depression, poorer HbA1c, and lower perceived coping effectiveness. Anxiety reactions to stress were similarly related to higher depression symptoms, but were unrelated to HbA1c and perceived coping effectiveness. Age, gender, illness duration, and pump status were each significantly correlated with at least one outcome, and were thus entered as covariates.
Table 1.
Sample Means, Standard Deviations, and Pearson Correlation Coefficients among Study Variables
| Mean (SD) | 1. | 2. | 3. | 4. | 5. | 6. | 7. | 8. | 9. | 10. | 11. | 12. | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Benefit Finding | 3.13 (0.79) | -- | |||||||||||
| 2. PA Reactions | 1.56 (0.79) | .129* | -- | ||||||||||
| 3. Depressive Reactions | 1.78 (0.75) | .135* | −.088 | -- | |||||||||
| 4. Anxiety Reactions | 2.03 (0.76) | .098 | .203** | .256** | -- | ||||||||
| 5. Coping Effectiveness | 3.67 (0.69) | .159* | .136* | −.331** | −.095 | -- | |||||||
| 6. Depression | 5.41 (5.13) | −.217** | .066 | .337** | .227** | −.355** | -- | ||||||
| 7. Adherence | 3.94 (0.57) | .259** | .023 | −.086 | −.040 | .223** | −.209** | -- | |||||
| 8. HbA1c | 8.35 (1.58) | −.114 | .094 | .138* | .072 | −.198** | .229** | −.311** | -- | ||||
| 9. Age | 12.50 (1.53) | −.053 | .004 | −.040 | .109 | .110 | −.019 | −.196** | .148* | -- | |||
| 10. Gendera (M = % female) | 54% | .099 | .044 | .082 | .098 | −.013 | .127* | .058 | −.059 | −.104 | -- | ||
| 11. Illness Duration (months) | 56.45 (35.72) | .026 | −.027 | −.054 | −.093 | .055 | −.048 | −.101 | .127* | .069 | −.036 | -- | |
| 12. Pump Statusb (M = % MDI) | 49% | −.174** | .031 | .014 | .028 | −.031 | .092 | −.094 | .268** | .005 | −.062 | −.152* | -- |
Note:
p < .01,
p < .05;
PA = Positive Affect;
Gender was coded as 1 = male and 2 = female;
Pump status was coded as 1 = pump therapy and 2 =multiple daily injections (MDI)
Does benefit finding buffer negative affective reactions to diabetes stress?
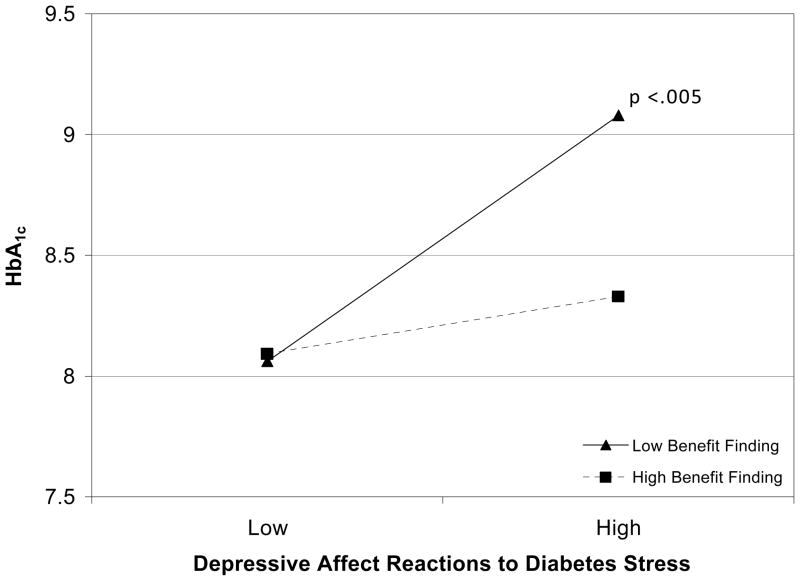
Regression analyses reported in Table 2 revealed that benefit finding interacted with depressive affective reactions to stress to predict both depression symptoms and HbA1c, and these associations were independent of reported levels of anxiety reactions to stress. As displayed in Figure 1, depressive affect reactions to stress were more strongly associated with symptoms of depression among those with low versus high benefit finding, although the simple slopes for both low, t (232) = 5.14, p < .001, and high benefit finding, t (232) = 3.35, p = .001, were significantly different from zero. Similarly, as displayed in Figure 2, depressive affect reactions were associated with poorer (higher) HbA1c among those with low benefit finding, t(232) = 3.06, p = .002, but this relationship was not significant among those reporting high benefit finding, t (232) = 1.02, p = .30. As displayed in the bottom portion of Table 2, analyses examining anxiety reactions to stress revealed the benefit finding X anxiety interaction also predicted HbA1c, but was unrelated to depression. As displayed in Figure 3, anxiety reactions to stress were associated with poorer HbA1c among those with low benefit finding, t(232) = 2.21, p = .03, but were unrelated to HbA1c among those with high benefit finding, t(232) = 1.26, p = .21. Benefit finding did not interact with either depressive affect or anxiety reactions to predict adherence, p > .18, or perceived coping effectiveness, p > .11. Taken together, findings suggest benefit finding buffers adverse emotional and physiological outcomes associated with negative affective reactions to diabetes stress.
Table 2.
Multiple Regression Analyses Testing the Benefit Finding X Depressive Affect and the Benefit Finding X Anxiety Interactions Predicting Depression and HbA1c
| Predictor Variables | Depression Symptoms | HbA1c | ||
|---|---|---|---|---|
| SE | β | SE | β | |
| Step 1 | ΔR2 = .233, F(7,233) = 10.084** | ΔR2 = .158, F (7, 233) = 6.263** | ||
| Age | (.196) | −.035 | (.062) | .131* |
| Gender | (.602) | .125* | (.191) | −.016 |
| Illness Duration | (.008) | .018 | (.003) | .183** |
| Pump Status | (.603) | .037 | (.192) | .275** |
| Anxiety Reactions | (.410) | .169** | (.130) | .045 |
| Depressive Affect | (.408) | .327** | (.129) | .156* |
| Benefit Finding | (.386) | −.289** | (.122) | −.102 |
| Step 2 | ΔR2 = .018, F(8, 232) = 9.702** | ΔR2 = .014, F(8, 232) = 6.035** | ||
| BF X Depressive | (.524) | −.148* | (.167) | −.130+ |
| Affect | ||||
| Step 2 | ΔR2 = .003, F(8, 232) = 8.952** | ΔR2 = .021, F(8, 232) = 6.351** | ||
| BF X Anxiety | (.518) | −.060 | (.162) | −.151* |
Note: Separate analyses were conducted to test interactions with depressive affect and with anxiety;
p < .01,
p < .05,
p = .05;
BF = Benefit Finding
Figure 1.
Predicted means for the benefit finding X depressive affect reactions interaction predicting symptoms of depression (CDI scores)
Figure 2.
Predicted means for the benefit finding X depressive affect reactions interaction predicting HbA1c
Figure 3.
Predicted means for the benefit finding X anxiety reactions interaction predicting HbA1c
Are benefit finding associations mediated by positive affective reactions?
Mediation analyses were conducted to examine whether benefit finding associations with outcomes were explained by heightened PA reactions to stress. To support mediation, the predictor (i.e., benefit finding) should be associated with the mediator (i.e., PA) and the outcome (e.g., perceived coping effectiveness), the mediator should be associated with the outcome, and the association between the predictor and the outcome should be eliminated or reduced when the mediator is statistically controlled. Correlations in Table 1 revealed support for this possibility only for perceived coping effectiveness, given that PA reactions were uncorrelated with all other outcome variables. Benefit finding predicted PA reactions, β = .129, p = .049, and coping effectiveness, β = .156, p = .02, after covariates were statistically controlled in the regression equation. However, when both benefit finding and PA reactions were entered into the equation simultaneously, the mediator (i.e., PA) was no longer associated with the outcome, β = .113, p = .08, while the predictor (i.e., benefit finding) remained significant, β = .141, p = .03. This pattern does not support PA reactions as a mediator of benefit finding effects.
Age differences and supplemental analyses
Correlations in Table 1 indicated age was unrelated to benefit finding, and the analyses reported above revealed benefit finding effects occurred independent of age. To explore whether benefit finding effects differed by age, we examined benefit finding X age interactions predicting each affect and benefit finding X affect X age interactions predicting each outcome. Only one of 15 tests was significant. We interpret this as a chance finding and do not discuss it further. The interested reader should note that similar analyses also revealed no gender differences.
Supplemental analyses were conducted to examine two additional issues. First, benefit finding X PA interactions were analyzed given recent suggestions that benefit finding may be associated with more adaptive physiological stress responses only among those who experience heightened PA (Moskowitz & Epel, 2006). These analyses revealed no significant interactions for any outcome, p > .07. Second, we considered the possibility that the heightened negative affective reactions may mediate benefit finding associations with better diabetes management, given the possibility that health-related threat perceptions may motivate better health behaviors (Schuettler & Kiviniemi, 2006). However, negative affective reactions were correlated with poorer rather than better adherence and effective management of diabetes problems (see Table 1), which is inconsistent with this alternative mediation model.
Discussion
Findings suggest benefit finding may be an important resource for adolescents who are facing heightened stress and emotional lability, while dealing with a complex and demanding illness such as diabetes. As hypothesized, benefit finding was associated with better adherence, lower symptoms of depression, as well as greater perceived coping effectiveness and positive affect in response to diabetes-related stress. Benefit finding was also associated with heightened anxiety and depressive affect in the face of diabetes stress, but appeared to buffer the adverse aspects of these negative emotional reactions for HbA1c and symptoms of depression. This buffering effect is particularly interesting because the correlations with heightened negative affective reactions were the only data that suggested benefit finding was associated with poorer well-being.
It is important to consider why benefit finding was associated with heightened negative affective reactions to diabetes stress. One explanation is that benefit finding is an emotional coping strategy that serves to manage distress (Helgeson et al., 2006). This reverse causation explanation could suggest that adolescents who are prone to depression and anger in the face of diabetes problems simply engage in more benefit finding. However, this explanation seems inconsistent with the fact that benefit finding was also associated with lower symptoms of depression. Our findings suggest that, even if benefit finding is activated by negative affect, it serves a more active function by minimizing the disruptive aspects of these emotional experiences. Wiebe and Korbel (2003) have argued that reality-based defensive processes can enhance the effectiveness of a dynamic system that manages health threats by regulating negative emotional arousal at adaptive levels. Benefit finding may reflect one such process, although we must acknowledge that negative affective reactions did not appear “adaptive” or to motivate better self-care, even among those with higher benefit finding. Negative affect appeared to be disruptive in general, but less so for those with higher benefit finding.
It is also possible that benefit finding reflects a process of growth and adaptation where adolescents who are establishing their identities and beginning to set life goals do so in the context of living with a serious illness. Future-oriented concerns develop during early adolescence (Massey et al., 2008; Seiffge-Krenke et al., 2009), and adolescents with diabetes routinely incorporate aspects of diabetes management into their life goals (Butler, Fortenberry, Berg, McCabe, Blakemore, & Wiebe, 2010). Such openness to new experiences and the future implications of diabetes may facilitate the identification of benefits while also exposing youth to different diabetes stressors that are inherently more distressing (Helgeson et al., 2006). We are currently beginning to code the described stressors to discern whether benefit finding was associated with qualitatively different types of diabetes stress.
A third explanation for the association between benefit finding and heightened negative affect is that benefit finding reflects broader individual differences in emotion regulation capabilities (Rabe, Zöllner, Maercker, & Karl, 2006; Siegel, Schrimshaw, & Pretter, 2005). In this scenario, adolescents who find more benefits may be more attuned to and therefore report higher levels of both negative and positive emotional experiences. By experiencing emotions as they occur, and using those emotions as information to make sense of and manage one’s illness experiences, adolescents may be able to regulate their diabetes more smoothly. This is consistent with findings that one’s affective associations with health or illness behaviors may be a shorthand cue to expected outcomes, allowing one to make efficient behavioral management decisions (Kiviniemi, Voss-Humke, & Seifert, 2007).
In the present study, anxiety factored separately from other negative affects, consistent with tripartite models of depression and anxiety (Clark & Watson, 1991; Joiner, Catanzaro, & Laurent, 1996). Furthermore, although benefit finding moderated the adverse outcomes associated with both depressive affect and anxiety, moderation of different affects predicted somewhat different outcomes. That is, the benefit finding X depressive affect interaction uniquely predicted symptoms of depression and HbA1c. In contrast, the benefit finding X anxiety interaction uniquely predicted HbA1c, but did not predict depression. These patterns may reflect different mechanisms through which benefit finding and emotions are associated with adolescent well-being (e.g., anxiety may reflect fairly direct influences of physiological arousal on blood glucose). Future research that replicates and explains these associations will be necessary to clarify the processes by which benefit finding buffers stress and negative affect.
Adolescents with higher benefit finding reported stronger PA reactions to diabetes stress, suggesting an ability to maintain or generate PA in the face of difficulties. Greater experiences of PA may in turn facilitate more adaptive coping in distressing situations. Although PA was associated with higher perceived coping effectiveness, however, there was no evidence that PA mediated or moderated benefit finding effects. This was surprising in light of growing evidence that PA is an important resource that facilitates adaptive responses to health threats by providing information that one has the resources to face these threats directly (Aspinwall, 1998), promoting efficient health care decisions (Kiviniemi et al., 2007), or bolstering self-efficacy beliefs (Schuettler & Kiviniemi, 2006). Our findings are also in contrast to Moskowitz and Epel’s (2006) report that benefit finding was associated with adaptive patterns of daily cortisol only among those with high PA. Contrasting findings may reflect the study of different populations and stress contexts, as well as the fact that we measured positive affect with two items that captured the more energized aspects of positive affect (e.g., excited), rather than calmness and serenity (Watson, Clark, & Tellegen, 1988). Additional research will be needed to clarify whether and how benefit finding effects are associated with positive affect.
Benefit finding was not correlated with age, and its associations with adolescent well-being did not differ by age. These findings may reflect our small age range, but are fairly consistent with the literature on benefit finding in children and adolescents. A better understanding of the development of benefit finding may occur by examining its relationships with specific aspects of cognitive development, rather than simply with age. As one example, future oriented thinking emerges during early adolescence and becomes increasingly complex as adolescents establish, plan, and pursue life goals (Massey et al., 2008; Seginer, 2008). Life experiences can alter these goal pursuits by constraining future expectations, or limiting beliefs that the investment in constructing one’s future will pay off. Seginer (2008) argues that, in the face of threat, adolescents use resources to arouse hope as they set and plan future goal pursuits. It is conceivable that benefit finding is a resource that frees adolescents to see a future unhindered by diabetes, and to select and pursue life goals that are compatible with or even enhanced by their illness. Research examining benefit finding in the context of this and other aspects of adolescent development (e.g., identity development) may be particularly fruitful for understanding how benefit finding develops and functions.
There are limitations of the study that should be considered in future research. First, the cross-sectional, retrospective and self-report nature of the data prevents causal interpretations. We note, however, that the temporal nature of the benefit finding and affective reaction variables appeared consistent with tested associations; that is, benefit finding is likely to reflect more trait-like characteristics that either buffer the more state-like negative affective reactions (Aim 1) or facilitate more state-like positive affective reactions to stressors (Aim 2). Second, the sample included adolescents who had been coping with diabetes for at least one year, presumably after experiencing the most active period of adaptation to illness and engaging in the process of finding benefits in those illness experiences. Helgeson et al. (2006) demonstrated that the positive effects of benefit finding are more evident as time since trauma increases, suggesting that beneficial outcomes require patients to take time to process and find genuine growth out of troubling events. Although duration of illness was covaried in all analyses, different findings may have emerged had newly diagnosed participants been included. Third, this is one of the first studies examining benefit finding among those with diabetes (Helgeson et al., 2009), and findings may differ in the context of other illnesses. Diabetes is a demanding and serious illness, but it is manageable and arguably less traumatic than the more well-studied illnesses such as cancer or HIV. Fourth, the sample was primarily middle-class and Caucasian, and findings may not generalize to a sample that has more ethnic and economic diversity. Finally, the benefit finding measure we utilized has not been validated on early adolescents. The benefit finding scale appeared reliable, was at a reading level appropriate for the sample, and predicted important indices of adolescent well-being independently of age. Nevertheless, measures of benefit finding developed specifically for adolescents, a larger age range, and measures of cognitive development may yield different interpretations.
In conclusion, evidence from this study suggests that benefit finding acts as a stress-buffer among adolescents with type 1 diabetes, protecting against disruptions related to negative affect reactions and maintaining or promoting positive affect in the face of illness-related difficulties. The stress-buffering role of benefit finding has been theorized in a limited set of studies (e.g., Pakenham, 2005; Siegel & Schrimshaw, 2007). The present findings provide insight into some inconsistencies in the benefit finding literature by demonstrating that benefit finding can be simultaneously associated with negative affect and better illness adjustment. To our knowledge, this is only the second study to investigate benefit finding in a diabetes population (Helgeson et al., 2009). Diabetes demands ongoing behavioral management and coping in comparison to other chronic illnesses that have been more commonly studied (e.g., cancer, HIV/AIDS). Future research is necessary to understand how benefit finding develops and matures across the adolescent years, why benefit finding was associated with heightened negative affective reactions to stress, and whether and how concurrent benefit finding associations may play out longitudinally across time. If supported by future research, interventions to promote benefit finding may prove useful for adolescents coping with this challenging illness.
Acknowledgments
This research was supported by grant R01 DK063044 from the National Institute of Diabetes and Digestive and Kidney Diseases. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Diabetes and Digestive and Kidney Diseases or the National Institutes of Health. We thank the families and staff at the Utah Diabetes Center and participating diabetes clinics, and all members of the ADAPT Research Team.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/hea
Contributor Information
Vincent Tran, Department of Psychiatry, University of Texas Southwestern Medical Center.
Deborah J. Wiebe, Department of Psychiatry, University of Texas Southwestern Medical Center
Katherine T. Fortenberry, Department of Psychology, University of Utah
Jorie M. Butler, Department of Psychology, University of Utah
Cynthia A. Berg, Department of Psychology, University of Utah
References
- Affleck G, Tennen H. Construing benefits from adversity: Adaptational significance and dispositional underpinnings. Journal of Personality. 1996;64:899–922. doi: 10.1111/j.1467-6494.1996.tb00948.x. [DOI] [PubMed] [Google Scholar]
- Aiken LS, West SG. Multiple regression: Testing and interpreting interactions. Thousand Oaks, CA: Sage Publications, Inc; 1991. [Google Scholar]
- Algoe SB, Stanton AL. Is benefit finding good for individuals with chronic disease? In: Park CL, Lechner SC, Antoni MH, Stanton AL, editors. Medical illness and positive life change: Can crisis lead to personal transformation? Washington, DC: American Psychological Association; 2009. pp. 173–193. [Google Scholar]
- American Diabetes Association. Standards of medical care in Diabetes – 2009. Diabetes Care. 2009;32:S13–S61. doi: 10.2337/dc09-S013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Antoni MH, Lehman JM, Klibourn KM, Boyers AE, Culver JL, Alferi SM, Carver CS. Cognitive-behavioral stress management intervention decreases the prevalence of depression and enhances benefit finding among women under treatment for early-stage breast cancer. Health Psychology. 2001;20:20–32. doi: 10.1037//0278-6133.20.1.20. [DOI] [PubMed] [Google Scholar]
- Aspinwall LG. Rethinking the role of positive affect in self-regulation. Motivation and Emotion. 1998;22:1–32. [Google Scholar]
- Band EB, Weisz JR. Developmental differences in primary and secondary control coping and adjustment to juvenile diabetes. Journal of Clinical Child Psychology. 1990;19:150–158. [Google Scholar]
- Baron RM, Kenny DA. The moderator-mediator variable distinction in social psychological research: Conceptual, strategic, and statistical considerations. Journal of Personality and Social Psychology. 1986;51:1173–1182. doi: 10.1037//0022-3514.51.6.1173. [DOI] [PubMed] [Google Scholar]
- Berg CA, Skinner M, Ko K, Butler JM, Palmer DL, Butner J, Wiebe DJ. The fit between stress appraisal and dyadic coping in predicting perceived coping effectiveness for adolescents with type 1 diabetes. Journal of Family Psychology. 2009;23:521–530. doi: 10.1037/a0015556. [DOI] [PubMed] [Google Scholar]
- Butler JM, Fortenberry KT, Berg CA, McCabe J, Blakemore T, Wiebe DJ. Adolescents’ goals and mothers’ accuracy in predicting adolescent goals in the context of type 1 diabetes. Children’s Health Care (in press) [Google Scholar]
- Cohen J, Cohen P. Applied multiple regression/correlation analysis for the behavioral sciences. 2. Hillsdale, N.J: L. Erlbaum Associates; 1983. [Google Scholar]
- de Groot M, Anderson R, Freedland KE, Clouse RE, Lustman PJ. Association of depression and diabetes complications: A meta-analysis. Psychosomatic Medicine. 2001;63:619–630. doi: 10.1097/00006842-200107000-00015. [DOI] [PubMed] [Google Scholar]
- Dovey-Pearce G, Doherty Y, May C. The influence of diabetes upon adolescent and young adult development: A qualitative study. British Journal of Health Psychology. 2007;12:75–91. doi: 10.1348/135910706X98317. [DOI] [PubMed] [Google Scholar]
- Folkman S. The case for positive emotions in the stress process. Anxiety, Stress & Coping: An International Journal. 2008;21:3–14. doi: 10.1080/10615800701740457. [DOI] [PubMed] [Google Scholar]
- Fortenberry KT, Blakemore T, Butler D, Gelfand D, Berg C, Wiebe DJ. Benefit finding in adolescents with diabetes: Additional themes. Poster presented at the meeting of the American Psychological Association; Boston, MA. 2008. Aug, [Google Scholar]
- Fortenberry KT, Butler JM, Butner J, Berg CA, Upchurch R, Wiebe DJ. Perceived diabetes task competence mediates the relationship of both negative and positive affect with blood glucose in adolescents with type 1 diabetes. Annals of Behavioral Medicine. 2009;37:1–9. doi: 10.1007/s12160-009-9086-7. [DOI] [PubMed] [Google Scholar]
- Fredrickson BL. The role of positive emotions in positive psychology: The broaden-and-build theory of positive emotions. American Psychologist. 2001;56:218–226. doi: 10.1037//0003-066x.56.3.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hart SL, Vella L, Mohr DC. Relationships among depressive symptoms, benefit-finding, optimism, and positive affect in multiple sclerosis patients after psychotherapy for depression. Health Psychology. 2008;27:230–238. doi: 10.1037/0278-6133.27.2.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Helgeson VS, Lopez L, Mennella C. Medical illness and positive life change: Can crisis lead to personal transformation? Washington, DC: American Psychological Association; 2009. Benefit finding among children and adolescents with diabetes; pp. 65–86. [Google Scholar]
- Helgeson VS, Reynolds KA, Tomich PL. A meta-analytic review of benefit finding and growth. Journal of Consulting and Clinical Psychology. 2006;74:797–816. doi: 10.1037/0022-006X.74.5.797. [DOI] [PubMed] [Google Scholar]
- Helgeson VS, Snyder PR, Escobar O, Siminerio L, Becker D. Comparison of adolescents with and without diabetes on indices of psychosocial functioning for three years. Journal of Pediatric Psychology. 2007;32:794–806. doi: 10.1093/jpepsy/jsm020. [DOI] [PubMed] [Google Scholar]
- Holmes CS, Chen R, Streis and R, Marschall DE, Souter S, Swift EE, Peterson CC. Predictors of youth diabetes care behaviors and metabolic control: A structural equation modeling approach. Journal of Pediatric Psychology. 2006;31:770–784. doi: 10.1093/jpepsy/jsj083. [DOI] [PubMed] [Google Scholar]
- Ickovics JR, Meade CS, Kershaw TS, Milan S, Lewis JB, Ethier KA. Urban teens: Trauma, posttraumatic growth, and emotional distress among female adolescents. Journal of Consulting and Clinical Psychology. 2006;74:841–850. doi: 10.1037/0022-006X.74.5.841. [DOI] [PubMed] [Google Scholar]
- Janoff-Bulman R, Frieze IH. A theoretical perspective for understanding reactions to victimization. Journal of Social Issues. 1983;39:1–17. [Google Scholar]
- Joiner TE, Jr, Catanzaro SJ, Laurent J. Tripartite structure of positive and negative affect, depression, and anxiety in child and adolescent psychiatric inpatients. Journal of Abnormal Psychology. 1996;105:401–409. doi: 10.1037//0021-843x.105.3.401. [DOI] [PubMed] [Google Scholar]
- Kiviniemi MT, Voss-Humke AM, Seifert AL. How do I feel about the behavior? The interplay of affective associations with behaviors and cognitive beliefs as influences on physical activity behavior. Health Psychology. 2007;26:152–158. doi: 10.1037/0278-6133.26.2.152. [DOI] [PubMed] [Google Scholar]
- Korbel CD, Wiebe DJ, Berg CA, Palmer DL. Gender differences in adherence to type 1 diabetes management across adolescence: The mediating role of depression. Children’s Health Care. 2007;36:83–98. [Google Scholar]
- Kovacs M. The Children’s Depression Inventory (CDI) Psychopharmacology Bulletin. 1985;21:995–998. [PubMed] [Google Scholar]
- La Greca AM, Follansbee D, Skyler JS. Developmental and behavioral aspects of diabetes management in youngsters. Children’s Health Care. 1990;19:132–139. [Google Scholar]
- Larson RW, Moneta G, Richards MH, Wilson S. Continuity, stability, and change in daily emotional experience across adolescence. Child Development. 2002;73:1151–1165. doi: 10.1111/1467-8624.00464. [DOI] [PubMed] [Google Scholar]
- Linley P, Joseph S. Positive change following trauma and adversity: A review. Journal of Traumatic Stress. 2004;17:11–21. doi: 10.1023/B:JOTS.0000014671.27856.7e. [DOI] [PubMed] [Google Scholar]
- Massey EK, Gebhardt WA, Garnefski N. Adolescent goal content and pursuit: A review of the literature from the past 16 years. Developmental Review. 2008;28:421–460. [Google Scholar]
- Mohr DC, Dick LP, Russo D, Pinn J, Boudewyn AC, Likosky W, Goodkin DE. The psychosocial impact of multiple sclerosis: Exploring the patient’s perspective. Health Psychology. 1999;18:376–382. doi: 10.1037//0278-6133.18.4.376. [DOI] [PubMed] [Google Scholar]
- Moskowitz JT, Epel ES. Benefit finding and diurnal cortisol slope in maternal caregivers: A moderating role for positive emotion. Journal of Positive Psychology. 2006;1:83–91. [Google Scholar]
- Pakenham KI. Benefit finding in multiple sclerosis and associations with positive and negative outcomes. Health Psychology. 2005;24:123–132. doi: 10.1037/0278-6133.24.2.123. [DOI] [PubMed] [Google Scholar]
- Park CL, Helgeson VS. Growth following highly stressful life events: Current status and future directions. Journal of Consulting and Clinical Psychology. 2006;74:791–796. doi: 10.1037/0022-006X.74.5.791. [DOI] [PubMed] [Google Scholar]
- Phipps S, Long AM, Ogden J. Benefit finding scale for children: Preliminary findings from a childhood cancer population. Journal of Pediatric Psychology. 2007;32:1264–1271. doi: 10.1093/jpepsy/jsl052. [DOI] [PubMed] [Google Scholar]
- Preacher KJ, Curran PJ, Bauer DJ. Computational tools for probing interactions in multiple linear regression, multilevel modeling, and latent curve analysis. Journal of Educational and Behavioral Statistics. 2006;31:437–448. [Google Scholar]
- Rabe S, Zöllner T, Maercker A, Karl A. Neural correlates of posttraumatic growth after severe motor vehicle accidents. Journal of Consulting and Clinical Psychology. 2006;74:880–886. doi: 10.1037/0022-006X.74.5.880. [DOI] [PubMed] [Google Scholar]
- Schuettler D, Kiviniemi MT. Does how I feel about it matter? The role of affect in cognitive and behavioral reactions to an illness diagnosis. Journal of Applied Social Psychology. 2006;36:2599–2618. [Google Scholar]
- Seginer R. Future orientation in times of threat and challenge: How resilient adolescents construct their future. International Journal of Behavioral Development. 2008;32:272–283. [Google Scholar]
- Seiffge-Krenke I, Aunola K, Nurmi J. Changes in stress perception and coping during adolescence: The role of situational and personal factors. Child Development. 2009;80:259–279. doi: 10.1111/j.1467-8624.2008.01258.x. [DOI] [PubMed] [Google Scholar]
- Siegel K, Schrimshaw EW. The stress moderating role of benefit finding on psychological distress and well-being among women living with HIV/AIDS. AIDS and Behavior. 2007;11:421–433. doi: 10.1007/s10461-006-9186-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siegel K, Schrimshaw EW, Pretter S. Stress-related growth among women living with HIV/AIDS: Examination of an explanatory model. Journal of Behavioral Medicine. 2005;28:403–414. doi: 10.1007/s10865-005-9015-6. [DOI] [PubMed] [Google Scholar]
- Taylor SE. Adjustment to threatening events: A theory of cognitive adaptation. American Psychologist. 1983;38:1161–1173. [Google Scholar]
- Watson D, Clark LA, Tellegen A. Development and validation of brief measures of positive and negative affect: The PANAS scales. Journal of Personality and Social Psychology. 1988;54:1063–1070. doi: 10.1037//0022-3514.54.6.1063. [DOI] [PubMed] [Google Scholar]
- Wiebe DJ, Berg CA, Palmer D, Korbel C, Beveridge R, Swinyard M, Donaldson DL. Children’s appraisals of maternal involvement in coping with diabetes: Enhancing our understanding of adherence, metabolic control, and quality of life across adolescence. Journal of Pediatric Psychology. 2005;30:167–178. doi: 10.1093/jpepsy/jsi004. [DOI] [PubMed] [Google Scholar]
- Wiebe DJ, Korbel C. Defensive denial, affect, and the self-regulation of health threats. In: Cameron LD, Leventhal H, editors. The self-regulation of health and illness behaviour. New York: Routledge; 2003. pp. 184–203. [Google Scholar]