Abstract
Background
Informal caregivers (IC) for medically fragile hematopoietic cell transplant (HCT) patients are a vital unrecognized population supporting the transplant patient along the illness continuum. The long transplant recovery period shifts a greater burden of care to the patient’s IC. Assessment of HCT caregiver quality of life and health status is critical to implementation of timely intervention and support.
Methods
A literature search using several search strategies covering 1980 to 2010 identified studies on ICs of hematopoietic cell transplant patients. These studies were summarized within the caregiver concepts of quality of life, role, and resources. Findings of this review were used to create recommended interventions and identify implications for further research.
Results
Although limited, research on ICs of hematopoietic call transplant patients provides beginning evidence for clinical interventions to support this caregiver population. Interventions created focus on Education, Psychosocial Support, and Self Care.
Conclusions
Although limited randomized trials of interventions have been reported, descriptive studies provide evidence for creating intervention content that addresses needs of ICs of hematopoietic cell transplant patients. Testing of these interventions and additional areas of research are identified.
Implications for Practice
Beginning descriptive evidence provides the basis for interventions for ICs of hematopoietic cell transplant patients. These interventions support caregiver quality of life and role implementation depending on individual caregivers’ resources and needs. Further evaluation and clinical research is needed.
Keywords: IC, hematopoietic cell transplant, hematologic cancers, quality of life
Introduction
Within the United States, approximately 65.7 million informal caregivers (IC) provide unpaid care for a care recipient 1. In 2007 ICs, a spouse, family member, friend or neighbor of a care recipient, provided approximately $375 billion of unpaid care to adults age 18 and older in need of either basic physical care or instrumental care such as transportation to the physician’s office for ongoing medical care 2. Approximately 7% of caregivers provide care to care recipients with a cancer diagnosis. The American Cancer Society (ACS) estimates the ICs will provide countless hours of care to the more than 1.4 million newly diagnosed patients with cancer 3.With five-year survival rates at 66%, up from 50% in 1975-1977, caregiving needs are increasing.
Background; Caregiving in Hematopoietic Cell Transplant Patients
A cancer population that requires an IC committed over a long period is the Hematopoietic Cell Transplantation (HCT) patient. Caregivers for medically fragile HCT patients are a vital unrecognized resource and essential to the patient throughout the illness continuum. Allogeneic transplantation from histocompatible related and unrelated donors is a treatment of choice for a variety of hematologic, oncologic, immunologic, and hereditary diseases. The number of patients undergoing allogeneic HCTs has steadily increased since the first successful human marrow allografts and today there are more survivors of allogeneic HCT than at any time over the last forty years with approximately 4300 transplants completed in 2008 4. The illness trajectory for patients undergoing HCT is long, can be highly variable and uncertain with varying demands of care based on the stage of disease at diagnosis, previous treatment intensity, and treatment-related complications. Many of these survivors are living longer but have continuing healthcare needs. Care needs are often complex and encompass a broad range of potential deficits across the physical, psychological, social, and spiritual domains of care. The potential strain on HCT ICs is tremendous as they attempt to support the transplant recipient throughout the illness trajectory.
During the first 100 days, post-transplant the HCT recipient and caregivers are focused on engraftment, preventing complications, symptom management, juggling multiple medications, and scheduling of clinic appointments 5-8. HCT recipients also need to be close to the transplant center. Thus, many temporarily relocate resulting in social isolation for both the recipient and the caregivers 5-6. Beyond the first 100 days, patients need to continue to be vigilant about prevention of infection; struggle with lingering fatigue, symptom management, cognitive disruption, depression, existential angst, and family role shifting; and worry about financial hardship 5. In the long-term, HCT recipients may experience ongoing complications related to treatment before transplant, the conditioning regimen prior to the transplant, and complications related to graft vs. host disease 5-8 The long transplant recovery period creates a long-term commitment of the caregiver to the care of the patient. Caregivers assume both physical and psychosocial aspects of care in addition to managing the frequent outpatient visits required 6. While the goal is always cure, 10%-25% of patients will relapse following HCT and need to face end-of-life issues 5 A beginning literature for this caregiver population provides valuable insight into the HCT-caregiver experience and can provide the basis for needed nursing interventions.
The purpose for this paper is to 1) summarize the literature on informal caregiving and the HCT population 2) recommend evidence-based interventions that target ICs of HCT patients and 3) identify areas of needed research.
Methodology of the Literature Search
Understanding the HCT caregiver role experience across the continuum of the HCT experience is essential both to increase caregiver sense of role preparedness and to improve caregiver quality of life and health. An extensive literature search of several databases was performed using the CINAHL, PubMed, and Scopus from 1980 to 2010. Keywords used for the search included caregiver, spouse, family member, HCT, bone marrow transplant, quality of life and burden. Research articles using qualitative, quantitative methods, or mixed methods were selected. Studies were included that addressed caregivers of adult HCT recipients of either autologous or allogeneic transplants. Pediatric HCT patient caregivers were excluded due to differences in treatment and symptom management. The search uncovered a body of literature identifying the multidimensional needs of HCT ICs, the importance of the assessment of HCT caregivers, and the need to implement evidence-based interventions throughout the continuum of the transplant experience6, 9-19 The literature available on HCT caregiver role is limited; however, it provides information valuable in planning nursing interventions directed to HCT caregiver QOL (QOL) and health.
Findings across studies were organized into three areas. The first area focused on the impact of the experience on the caregiver, namely the caregiver quality of life. The second area focused on caregiver responsibilities in caring for the patient; in other words, the caregiver role. The third area included the resources within or available to the caregiver. Each of these areas had subcomponents.
Concept 1: Caregiver Quality of Life
ICs of patients undergoing HCT experience high stress levels as a result of the intense physical and emotional care needs of the recipient post-transplant 20. QOL is a broad multidimensional construct comprised of the physical, psychological, social, and spiritual domains of life experience. It is an important outcome measure in cancer care research and has been used with family caregivers to describe QOL outcomes21. .
Physical Domain
HCT ICs report difficulty with physical symptoms when caring for care recipients before, during and after transplant. These include fatigue, cognitive dysfunction, sexual issues and sleep disturbance10, 12-14, 22-23. Managing fatigue or the energy drain associated with caregiving is very challenging for caregivers. Among HCT caregivers fatigue is generally thought to be caused by constant vigilance associated with attending to the recipient’s care needs that become more pronounced as time passes or as complexity of care increases 10, 13-14. In one descriptive study, investigators surveyed 102 HCT caregivers prior to transplant regarding subjective symptoms of fatigue. Results revealed caregivers reported high levels of fatigue and associated lower QOL scores pre-transplant 13. These findings highlight the importance of paying attention to caregivers who complain of feeling exhausted.
Bishop and colleagues (2007) discussed long-term effects on spouses after transplantation. Like the transplant survivors, the caregiver partners experienced physical symptoms of fatigue, cognitive dysfunction and sexual issues23. These issues were more significant in the caregivers than in matched peer-nominated controls even years after the transplant (sample mean in years 6.7; SD = 10)23. Interestingly they found that fatigue, cognitive dysfunction, sleep issues and depression were interrelated.
Even prior to transplant, in a study of thirty-nine HCT patients and caregivers, researchers collected quantitative data to identify differences in adaptation10. Of the thirty-nine caregivers who participated in the study, most were spousal caregivers with an average age of 44 years and 54% of the caregivers were working full-time. Caregivers reported having troubled dreams prior to the transplant experience. They also had recurring concerns about the upcoming HCT experience during daytime hours10.
Psychological Domain
Caregivers in general, often suffer high psychological morbidity related to the caregiving experience1. This is especially true for caregivers of patients undergoing HCT. Distress is associated with the care recipient’s physical and psychological well-being 20, 24-25. In one study, 28 HCT patient/caregiver dyads were assessed for psychological distress one week prior to transplant and at 3, 6, and 12 months post-transplant. Results showed that 88% had substantial distress pre-transplant that gradually decreased to 18% at 12 months25. This distress was measured by the 12-item self-completed General Health Questionnaire (GQH) which measured the present emotional condition when compared to their normal state. Most caregivers reported having to manage the patient’s emotional distress for up to 12 months post-transplant. Other psychological symptoms reported by caregivers include fear of cancer recurrence and general fear about the future13, 15, 26.. Such fears highlight the uncertainty felt by many caregivers as their loved ones recover from this life-threatening experience. Supporting the patient post-transplant can be especially difficult for caregivers if recipients themselves are struggling emotionally.
Social Domain
Socially, many HCT caregivers report tension with other family members, resentment and frustration, social isolation, financial concerns, and feeling as though their everyday lives have been turned upside down. Many caregivers struggle with adapting to their new roles and responsibilities. In a mixed method prospective longitudinal study of psychosocial adaptation of 28 HCT patients and their caregivers over a 12 month period findings reveal half of the caregivers reported taking over tasks and roles of the HCT recipient 25. In a few studies, caregivers describe the struggle to meet competing demands such as continuing to work outside the home while supporting the HCT recipient 16, 20, 27. Inability to meet conflicting work demands and caregiving might require the caregiver to stop working. In one study, 67% of caregivers did suspend working to care for the HCT recipient 20. In another study, investigators explored the time commitment and financial requirements of HCT caregivers during HCT recipient hospitalization. Forty caregivers participated and reported significant time and financial requirements in support of the HCT patient. Many of the caregivers commented that they used vacation time or altered their schedule to accommodate for the hospitalization 27. Worry about financial concerns resulting from suspension of employment has a significant social impact on the patient and family or caregiver. Lack of employment affects the patient’s and family’s ability to meet their daily living expenses and their ability to continue to carry health insurance benefits.
Frequently social networks and family relationships are affected by the caregiving experience. HCT recipients and their caregivers who need to relocate close to the transplant center leaving their social support network behind might find adjustment to the social isolation daunting 6 Successful management of this isolation requires the care recipient and caregiver to form new relationships with other patients, caregivers, and healthcare professionals. Inability to form these new social relationships can lead to greater isolation potentially increasing caregiver distress. For many caregivers social support is an important determinant of whether or not they would continue to provide support to the HCT recipient. Keogh et al interviewed 28 HCT caregivers’ pre transplant and 3 months post transplant. All of the caregivers stated they had some support with 68% of HCT caregivers reporting the support that came from friends, family, and neighbors kept them going 25. In another study, investigators examined the quality of life of 36 HCT patient and caregiver dyads following transplant. Interview themes revealed that negative family support affected caregivers’ social well-being 16. Caregivers had challenges with social reclimitization, stress reduction, relationship building and conflict resolution16 .
Spiritual Domain
Spirituality is defined as an inherent quality of all humans that drives the search for meaning and purpose in life and involves relationships with oneself, others, and the transcendent dimension 28-29. HCT caregivers often voice feelings of fear and uncertainty regarding their loved one’s future and the possibility of disease recurrence and death. The ability to find meaning and a sense of purpose as an HCT caregiver can enhance the ability to cope with the challenges they face. Cancer caregiver research indicates that spiritual beliefs of the caregiver can influence his or her ability to cope, views on the meaning of life, and the ability to support the patient who also may be experiencing spiritual distress.30. Boyle et al. explored HCT caregiver and survivor QOL perceptions post discharge. Using a mixed method design these investigators were able to survey and interview 36 dyads. Results revealed that those caregivers who were able to reorder their life according to their personal priorities gained new insights and found they appreciated life more 16. Their coping strategies included acceptance, staying positive, looking at life differently, setting goals, and praying. In a prospective study, examining emotional adaptation of 192 HCT caregivers’ pre-transplant and one-month post transplant quantitative data revealed that those caregivers with more spiritual connectedness experienced less emotional distress 24.
In summary, a number of studies have provided valuable evidence on the impact of HCT on ICs. Studies reviewed identified a broad array of challenges ICs experience in all four areas of quality of life. Physical problems included fatigue and sleep as well as cognitive changes. Psychological problems illustrated ICs struggling with depression themselves in addition to helping a depressed patient who is fearful of recurrence. Social problems were the most common and included social isolation, family tension, financial problems, and the need to develop new approaches to distributing responsibilities within the family. Spiritual distress was described as having to come to grips with the meaning of changed lives. Studies illustrated the broad impact of caregiving in transplant patients on ICs quality of life and provide direction for creating caregiver interventions that need testing and dissemination.
Concept 2: Informal HCT Caregiver Role
Relevant literature on informal caregiving of HCT patient also focuses on the role of the caregiver. This perspective was developed through studies of caregivers from a variety of chronically ill patient populations and includes three aspects of the caregiving role that affect the caregiver as well as the patient: the demands of care, preparedness for the role, and mutuality or the relationship between the patient and the caregiver.31
Demands of Care
The demands of care is defined as the time spent in the tasks and behaviors that comprise the caregiver role 32. This can vary widely across the cancer care trajectory and includes physical, social and psychological demands. As the perceived amount of care demand increases, the potential for negative caregiver emotions associated with the experience increases. For the HCT caregiver potential sources of stress include the life-threatening nature of the illness, uncertainty, and prolonged hospitalization/recovery causing disruption to family and work, infection risk, complex medication regimens, monitoring for symptoms, social isolation, and HCT recipient dependency. Twenty-four HCT caregivers interviewed prior to the patient’s hospitalization, and 5 and 20 days post-BMT in one study reported disruptions to daily routine, fear of the future, and changes in interpersonal relationships across all time periods 14. In another study, 36 HCT caregiver/recipient dyads over a period of 1-6 years described continuing need to adjust due to lingering care demands post transplant 16.
Role Preparedness
Role preparedness refers to how competent the caregiver feels carrying out this new role. HCT caregivers are often asked to take on this new role without fully appreciating the complexity of the new responsibilities and how this role will affect their life. The need to support and prepare HCT caregivers for the potential stressors associated with this new role has been documented 17. Role preparedness has been studied in terms of how acquisition of knowledge and skills might protect the caregiver from role distress when complexity of care or care demands is high In one study researchers examined patterns of HCT caregiving, relationship quality, preparedness and caregiver role strain and rewards 20. Fifty-two caregivers completed a quantitative survey at hospital discharge, 2, 6 and 12 weeks after discharge. Results revealed that the rewards of caregiving, defined as the extent to which the caregiver is emotionally or interpersonally satisfying, were associated with role preparedness.
Mutuality
Development of cancer caregiver distress is sometimes related to mutuality defined as the quality of the interpersonal relationship between the caregiver and care recipient.32 . Mutuality is an understudied area, and rich area for future research. Poor relationship quality between the HCT recipient and caregiver can potentially lead to a difficult caregiving situation increasing distress for both patient and caregiver. Poor relationship quality is also associated with caregiver tension, depression and anger.32. Tension within the transplant dyad relationship has been found to be a predictor of caregiver strain 20. In looking at how caregiving post-transplant can affect spousal relationships Langer et al. studied marital dyads over a 12-month period post-transplant12.. Findings revealed that matched perceptions of the relationship pre-transplant grew mismatched by 6 and 12 months post-transplant with female caregivers reporting lower levels of marital satisfaction compared to patients. In another study of 28 caregivers of HCT patients who did not return to “independence” by 6 months experienced irritability and dissatisfaction creating a source of tension and conflict within the caregiver dyad relationship 25.
In summary, the concept of the caregiver role includes what the role entails, how prepared the caregiver is for this role, and the nature of the relationship between the caregiver and the patient. This concept provides valuable information on how aspects of the caregiver role can influence the development of nursing interventions for caregivers of HCT patients.
Concept 3: HCT IC Resources
The third concept related to the literature on caregiving of HCT patient focuses attention on the resources available to the caregiver. Resource use by the IC can potentially influence how he or she perceives the caregiver experience. Resources may be internal such as: gender, age, co-morbidities, caregiver personality and caregiver self-care activities; or external such as social support, relationships, or financial security. Each of these resources can potentially influence how the caregiver perceives the experience.
Traditionally the caregiver role is thought of as a female role (wives, sisters, and daughters), however this prevailing trend is changing, currently approximately 34% of caregiver of patients with chronic illness are men 1. Among HCT caregivers men report having more energy in comparison to women whereas the women experience more symptoms of anxiety and depression related to caregiving 10, 12-13.
Age differences among cancer caregivers suggest that younger female caregivers are more likely to experience depression, fatigue, and mood disturbances as caregiving difficulty increases 32. Gaston-Johansson et al studied caregivers of patients with breast cancer undergoing an HCT. Correlation revealed that the lower the age the higher the subjection burden. Age was significantly negatively correlated with subjective burden, defined as subjective response to the caregiver experience13.Within this study, mean age was 47.59 years (SD = 10.76) and the range from 25-72 where 75% of the participants were men working full-time. Many older caregivers with their own healthcare issues often struggle to meet their own personal needs as well as the needs of those they care for. Currently no literature was found on how the older HCT caregivers manage their own healthcare concerns while providing care to the HCT recipient.
Caregiver personality, the way one thinks and acts, can also influence the caregiving situation. In a study of 192 HCT caregivers researchers examined caregiver adaptation during the acute phase of transplant. Self-report questionnaires reveal HCT caregivers with greater sense of personal control had a more positive adaptation and a lower level of distress24. Having a sense of personal control or a feeling of confidence in one’s ability to manage the caregiving role can serve as a buffer especially when taking on new tasks or dealing with very challenging situations. In another study of eleven HCT caregivers, researchers interviewed spouses regarding their caregiving experience 33. HCT caregivers who were spouses of the patients (3 husbands, 8 wives) were interviewed up to six times from hospital admission through outpatient visits. Results reveal that spouses dealt with “living the uncertainty of transplant” through three strategies: rituals such as routine and structure, forming a positive perspective such as trying to keep positive in the face of side effects, and envisioning a future such as preparing for the future. These strategies helped manage the caregiver’s internal perspective and allowed the caregiver to create a space for hope and meaning.
Caregivers often struggle with inner conflict related to attending to the needs of the care recipient while still attending to their own health needs. While no studies were found related to HCT caregiver attending to their own health needs, studies of other populations are relevant. In a recent survey by the National Alliance of Caregivers nearly 50% of caregivers who report a high burden associated with their caregiving role also rated their health as poor and reported getting less exercise than before caregiving 34. Acton examined the role of self-care behaviors on caregiver stress and well-being as compared to non-caregivers 35. Forty-six family caregivers of cognitively impaired Alzheimer patients reveal those caregivers who practiced self-care behaviors had less stress and improved well-being than demographically matched noncaregivers.
The ability to care for oneself is particularly important for caregivers of patients undergoing HCT because the illness trajectory is long and uncertain. In a multisite descriptive study, researchers collected data from 58 HCT caregivers regarding their psychological and social needs following hospital discharge. Caregivers reported having less leisure time to pursue social activities 15. Williams interviewed 40 HCT caregivers during HCT patient hospitalization to learn more about the concepts of commitment, expectations and role negotiation 9. Findings revealed caregivers who are able to take time for self-care activities and are able to find time to reflect on their experience gain new insights into the meaning of the experience9. In the area of IC resources, studies have illustrated characteristics of ICs that must be taken into account in designing and testing IC interventions. These include both characteristics of the individual IC, and also what family and community resources can be mobilized to help.
In summary, studies describing informal caregivers for hematopoietic cell transplant patients illustrate multiple QOL concerns, and caregiver challenges, including a lack of preparedness and the influence of the IC-patient relationship on the ability to give care. In addition, specific IC characteristics, such as age, gender and personality and personal health ratios may influence the ability to provide patient care without jeopardizing their own status. Availability of external resources such as family and financial resources are important influencing factors. All the areas – caregiver quality of life, caregiver role, and the resources available - provide evidence for potential differences across individual caregivers, individual patients, and unique environments. These differences point to the complexity of this caregiver experience and the resulting need for tailoring interventions to match the concerns and problems that are most important to the individual caregiver. One approach to organizing the content for such an intervention is presented in the next section.
Creating HCT Caregiver Interventions
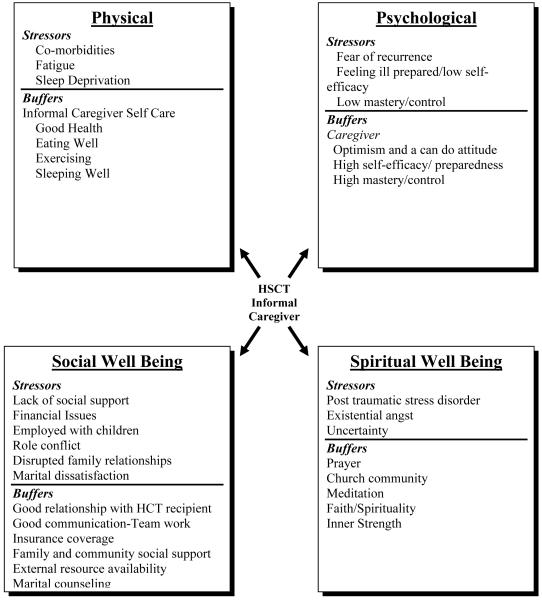
The first step in providing interventions for HCT caregivers is to identify a caregiver’s QOL, the view of the caregiver role, and the availability of resources. These aspects can be viewed as stressors or buffers. Stressors are a source of strain, for example co-morbidity, sleep disturbance and fatigue (Figure). Buffers are a source of support or aspects of an intervention that caregivers can use to mitigate the effects of the stressor and enhance health and well-being (Figure). Caregiver physical symptoms such as fatigue, a lack of confidence, poor challenging relationships with the patient, socio-demographic characteristics, role preparedness, financial concern, and uncertainty all have the potential to be stressors or buffers within the caregiving situation. Balancing the stressors and buffers involves timely tailored interventions that can lead to improved caregiver outcomes. For example, if an older adult has multiple co-morbidities, struggles with low perceived preparedness, and no social support network then these are stressors in need of tailored intervention and support. In contrast, if the IC is an older adult who is healthy with a positive attitude and social support then these attributes function as buffers to potential stressors.
Figure.
HCT IC Quality of Life Stressors and Buffers
Interventions described below are designed to assist the HCT caregiver to rebalance or shift from “what use to be” to “what is” by supporting their ability to access and use both internal and external resources. A cornerstone of the approaches suggested within this paper is an underlying assumption that success of a targeted intervention will be determined by the caregivers’ ability to participate in choosing what intervention might help and determining how it will be integrated into their life. This approach builds on work done by Cimprich (2003) et al. utilizing a self-management program called Taking CHARGE to equip breast cancer survivors with skills and information to deal with their ongoing concerns 36. Results reveal that when the participants have an opportunity to identify an issue of concern, assess current patterns of behavior, and develop a plan to address the area of concern, the study participant finds the intervention to be relevant and useful to them in dealing with psychosocial and physical concerns. Cimprich’s works highlights the importance of providing the participant choices in what the educational content will be and how it will be incorporated into their current situation.
Interventions to promote caregiver well-being can be grouped into three categories or modules: (1) an educational module to address caregiver mastery and preparedness; (2) a psychosocial module focusing on coping, relationship issues, and problem-solving strategies; and (3) a self-care module to promote caregiver health and well-being. Each of these modules can be used alone or in combination to support caregiver health status and QOL. A recent meta-analysis exploring the effectiveness of caregiver interventions recommends the use of multi-component interventions to increase caregiver well-being 37.
Implementing any or all of the modules involves creative education approaches. Increasingly researchers and policymakers are looking for innovative ways to provide assistance to patients and caregivers using technology. Numerous caregiver studies have explored how best to implement an intervention using telephone-based, online internet, individual, or group support. Each of these modalities offers a variety of advantages and disadvantages (Table). Each modality is designed to be caregiver focused allowing the caregiver to access services and support on their own schedule. Ploeg (2001) found most caregivers would use telephone support offered by a professional or a fellow caregiver if available 38. The value of telephone interventions was echoed by Mkanta et al (2007) who identified improvements among elderly patients undergoing chemotherapy in symptom management and health-related QOL following daily telehealth interactions between patients and nursing coordinators 39. Planning for caregivers includes not only the proposed content but the modality best suited to the caregiving situation and caregiver lifestyle.
Table.
Teaching Methods
| Intervention Modality | Advantages | Disadvantages |
|---|---|---|
Telehealth based strategies
|
Daily interaction and support with oncology professionals or lay persons |
Poor response time unless response time criteria built into the system Computerized support impersonal |
Web-based
|
Convenient Access online support any time of the day or night |
Need web-based skills to navigate the internet |
| Journaling | Expression of feelings for those who like to write |
Not for someone who does not write or like to write |
| Individual | One on one interaction to address specific needs |
Labor intensive |
| Group | Offers support of others to normalize the situation |
Not helpful for those who have difficulty sharing in a group setting. |
Educational Module
Tailored educational interventions are designed to provide the caregiver with training for skill development or increased knowledge to prepare and become competent in providing safe care for the HCT recipient. Group education or support may assist caregivers to see that others share the same challenges they face. Individual sessions, on the other hand, might be more helpful for caregivers who cannot leave the HCT recipient or when care needs are very complex encompassing both physical and psychosocial domains of care. Educational strategies include skill development, access to and use of resources, homecare/symptom management, and decision-making11, 17, 40. For many HCT caregivers the caregiving experience may be their first encounter with a healthcare system. Interventions designed to educate and train the caregiver about the ways to communicate with healthcare professionals to get answers to questions and to obtain needed resources and services can be very effective in minimizing stress 9, 18.
It is especially important that all educational materials and sessions be tailored to match the caregiver’s learning style and readiness to learn17. ICs prefer face-to-face communication with a healthcare professional when obtaining information about diagnosis or homecare instructions in preparation for discharge 15. Butcher et al explored the benefits of a 90 minute individualized problem solving education session with advanced cancer patients and caregivers. This teaching session occurred while patients and families were in the outpatient setting at a tertiary facility. Most participants felt more informed about community resources and had higher post session problem solving ability scores 41.
Psychosocial Module
Psychosocial interventions that are individualized and flexible and provide long-term support appear to be most effective 42. Psychosocial interventions include teaching caregivers problem-solving and coping skills18. Caregivers frequently cite the need for more education and support in coping. In one study a coping skill intervention using the family COPE model significantly improved caregiver QOL, burden of patient symptoms, and caregiving task burden compared to supportive visits alone 43. The COPE model focuses on Creativity viewing a problem from different perspectives to find solutions, Optimism or the ability to have a positive attitude, Planning or setting reasonable attainable goals, and Expert information needed to make a decision about when to access professional help 43. This approach to problem solving builds upon existing life experience. Session evaluations showed participants felt informed about community resources and had improved problem-solving skills.
The psychosocial module also addresses mutuality, or the interpersonal relationship between the caregiver and HCT patient which can influence the development of caregiver stress. In one study authors proposed interventions based on relationship strength or mutuality and preparedness targeted toward an identified deficit32.. When caregiver/HCT recipient dyad preparedness is low and mutuality is high offering opportunities for the caregiver to learn and build skills will increase their preparedness and support the existing high functioning relationship. On the other hand when preparedness is high and mutuality is low a referral for psychological counseling offers caregivers an opportunity to recognize their own feelings and engage in self-care activities and positive experiences to reduce caregiver strain.
Another strategy that might be helpful for those caregivers who are able to express their feelings is journal writing. For some caregivers the simple act of writing or journaling their experience offers great benefit 44. Dellasega and Zerbe (2002) offered caregivers the opportunity to participate in a pilot project using narrative writing within a support group format as a coping strategy. Participants demonstrated significant improvements in physical and mental health.
Self-Care Module
HCT caregivers in the Wilson et al study reveal it is important to balance the ’me and my world” with the “us and our world”33. Balancing the two worlds through integration of self-care strategies is a particular challenge for caregivers in light of all of the new caregiving responsibilities. Health-promotion techniques such as regular exercise, yoga, massage, eating well, and sleep hygiene offer caregivers an opportunity to focus on their own health and physical well-being.45-47. Simply teaching caregivers to plan healthy meals is a method of self-care and provides a measure of attainable control and assists with health promotion. Regular exercise provides caregivers with a physical outlet for the stresses associated with caregiving. It also improves the body’s cardiovascular, immune system, and mental well-being. Yoga, a combination of breathing exercise, physical postures, and meditation to reduce the health effects of daily stress, is the fifth most common complementary and alternative medicine technique used among Americans (http://nccam.nih.gov/news/report.pdf). Yoga with patients and caregivers in a palliative day care environment suggested that caregivers benefited from a restorative form of yoga 47. Massage therapy is another complementary therapy designed to reduce stress. Improvement of caregiver physical and psychological well-being through relaxing with a massage has been demonstrated 45.
Sleep deprivation or disturbance can significantly affect one’s physical and emotional well-being 22. Assessment and treatment of sleep problems associated with HCT caregiver role is critical to the caregiver’s physical and emotional well-being. Offering caregivers a plan for better sleep by teaching behavioral techniques (e.g., reducing external stimuli, promotion of relaxation, and adoption of healthy sleep routines) is a very effective strategy 46. A renewed and refreshed caregiver is better able to provide care and problem solve as needed.
Assisting caregivers in learning healthy behaviors is a very effective strategy for managing stress. Jacobsen et al. (2002) explored whether providing chemotherapy patients a self-administered stress management program utilizing relaxation and imagery techniques would improve QOL. Findings suggested that the program reduced stress, was cost-effective, and improved QOL scores especially mental well-being 48. An intervention such as this might also be applied to caregivers prior to undertaking the caregiver role.
Oncology nurses can encourage caregivers to take some time during the day to go for a walk or just be outdoors. Sometimes simply being in nature or truly present with full awareness of one’s surroundings can be restorative and counteract feelings of fatigue 49. All of these various interventions are designed to buffer the caregiver from the stresses of caregiving. They allow the caregiver to not only feel better physically and psychologically but also to appreciate and recognize the experience as meaningful.
In summary, as increasing HCT recipients survive their acute care experience, the long-term issues they and their caregivers need to face are coming to the forefront of research and healthcare initiatives. Fully understanding this experience from the caregiver perspective will enhance nurses’ abilities to identify caregivers with compromised QOL and health. In 177 dyads, partners described greater fatigue and cognitive dysfunction, and more depressive symptoms, sleep, and sexual problems than controls. Partners also reported 3.5 times more depression in comparison to controls and were less likely to seek mental health care. In addition, partners reported less social support and spiritual well-being with more dyad relationship dissatisfaction and loneliness as well as low levels of post-traumatic growth. Modification of caregiver distress throughout the caregiving experience through the implementation of tailored interventions that provide education on caregiving activities and psychosocial support and the promotion of healthy self-care behaviors is essential in support long-term caregiving.
Research Implications
HCT caregivers struggle with many issues, emotions, and an unpredictable and prolonged caregiving period. Concerns and needs vary as the caregiver and patient move along the HCT trajectory. Ongoing assessment of the IC provides information to support and offer referrals that are appropriate and timely. Current research has begun to demonstrate that interventions that effectively reduce caregiver strain include educational and or skills acquisition related to the disease, symptom management, available resources, psychosocial support discussing caregiver concerns/feelings with a referral to psychotherapy when indicated, and integration of health promotion self-care behaviors into caregiver lifestyle.
Additional research is indicated to test the effectiveness of interventions that appear to positively affect the caregiver/patient dyad relationship and, in doing so, better support the patient. The ability to focus limited resources is critical in developing effective strategies to support the caregiver/patient dyad throughout the continuum of care. Targeting those caregivers who exhibit distress or reduced well-being will allow for individualized timely interventions. Caregiver assessment, followed by nursing interventions tailored to match caregiver needs can be used to address their health status and QOL. Because of the long trajectory of HCT treatment and recovery, frequent and timely reassessment and intervention are needed. These clinical recommendations merit additional testing and research.
Acknowledgement
NCI R01-CA107446, Structured Nursing Intervention Protocol for HCT Patients
We would like to acknowledge Mary Mendelsohn, RN, MS for her contribution to data collection
Footnotes
This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.AARP NAfCa Executive Summary: Caregiving in the US. 2009 [Google Scholar]
- 2.AARP Valuing the Invaluable: The Economic Value of Family Caregiving. 2008 Update2008. [Google Scholar]
- 3.ACS . Cancer Facts and Figures. American Cancer Society; Atlanta, Georgia: 2006. [Google Scholar]
- 4.National Marrow Donor Program Outcomes Data. 2007 http://www.marrow.org/PHYSICIAN/Outcomes_Data/index.html#number.
- 5.Blume KF, Applebaum F. Hematopoetic Cell Transplantation. Blackwell Publishing; 2004. The Evaluation and Counseling of Candidates for Hematopoetic Cell Transplantation; pp. 449–462. S. [Google Scholar]
- 6.Grant M, Cooke L, Bhatia S, Forman S. Discharge and unscheduled readmissions of adult patients undergoing hematopoietic stem cell transplantation: implications for developing nursing interventions. Oncology nursing forum. 2005 Jan;32(1):E1–8. doi: 10.1188/05.onf.e1-e8. [DOI] [PubMed] [Google Scholar]
- 7.Saria MG, Gosselin-Acomb TK. Hematopoietic stem cell transplantation: implications for critical care nurses. Clinical journal of oncology nursing. 2007 Feb;11(1):53–63. doi: 10.1188/07.CJON.53-63. [DOI] [PubMed] [Google Scholar]
- 8.Ford RC, Madison J. Nursing Issues in Hematopoetic Cell Transplantation. In: Blume KF, Applebaum F, editors. Thomas’ Hematopoetic Cell Transplantation. Blackwell; 2004. pp. 469–482. J. S. [Google Scholar]
- 9.Williams LA. Whatever it takes: informal caregiving dynamics in blood and marrow transplantation. Oncology nursing forum. 2007 Mar;34(2):379–387. doi: 10.1188/07.ONF.379-387. [DOI] [PubMed] [Google Scholar]
- 10.Siston AK, List MA, Daugherty CK, et al. Psychosocial adjustment of patients and caregivers prior to allogeneic bone marrow transplantation. Bone Marrow Transplant. 2001 Jun;27(11):1181–1188. doi: 10.1038/sj.bmt.1703059. [DOI] [PubMed] [Google Scholar]
- 11.McDonald JC, Stetz KM, Compton K. Educational interventions for family caregivers during marrow transplantation. Oncology nursing forum. 1996 Oct;23(9):1432–1439. [PubMed] [Google Scholar]
- 12.Langer S, Abrams J, Syrjala K. Caregiver and patient marital satisfaction and affect following hematopoietic stem cell transplantation: a prospective, longitudinal investigation. Psychooncology. 2003 Apr-May;12(3):239–253. doi: 10.1002/pon.633. [DOI] [PubMed] [Google Scholar]
- 13.Gaston-Johansson F, Lachica EM, Fall-Dickson JM, Kennedy MJ. Psychological distress, fatigue, burden of care, and quality of life in primary caregivers of patients with breast cancer undergoing autologous bone marrow transplantation. Oncology nursing forum. 2004 Nov;31(6):1161–1169. doi: 10.1188/04.ONF.1161-1169. [DOI] [PubMed] [Google Scholar]
- 14.Foxall MJ, Gaston-Johansson F. Burden and health outcomes of family caregivers of hospitalized bone marrow transplant patients. J Adv Nurs. 1996 Nov;24(5):915–923. doi: 10.1111/j.1365-2648.1996.tb02926.x. [DOI] [PubMed] [Google Scholar]
- 15.Aslan O, Kav S, Meral C, et al. Needs of lay caregivers of bone marrow transplant patients in Turkey: a multicenter study. Cancer nursing. 2006 Nov-Dec;29(6):E1–7. doi: 10.1097/00002820-200611000-00014. [DOI] [PubMed] [Google Scholar]
- 16.Boyle D, Blodgett L, Gnesdiloff S, et al. Caregiver quality of life after autologous bone marrow transplantation. Cancer nursing. 2000 Jun;23(3):193–203. doi: 10.1097/00002820-200006000-00006. quiz 204-195. [DOI] [PubMed] [Google Scholar]
- 17.Compton K, McDonald JC, Stetz KM. Understanding the caring relationship during marrow transplantation: family caregivers and healthcare professionals. Oncology nursing forum. 1996 Oct;23(9):1428–1432. [PubMed] [Google Scholar]
- 18.Honea NJ, Brintnall R, Given B, et al. Putting Evidence into Practice: nursing assessment and interventions to reduce family caregiver strain and burden. Clinical journal of oncology nursing. 2008 Jun;12(3):507–516. doi: 10.1188/08.CJON.507-516. [DOI] [PubMed] [Google Scholar]
- 19.Stetz KM, McDonald JC, Compton K. Needs and experiences of family caregivers during marrow transplantation. Oncology nursing forum. 1996 Oct;23(9):1422–1427. [PubMed] [Google Scholar]
- 20.Eldredge DH, Nail LM, Maziarz RT, Hansen LK, Ewing D, Archbold PG. Explaining family caregiver role strain following autologous blood and marrow transplantation. Journal of psychosocial oncology. 2006;24(3):53–74. doi: 10.1300/J077v24n03_03. [DOI] [PubMed] [Google Scholar]
- 21.Ferrell BR. The quality of lives: 1,525 voices of cancer. Oncology nursing forum. 1996 Jul;23(6):909–916. [PubMed] [Google Scholar]
- 22.Carter PA. Family caregivers’ sleep loss and depression over time. Cancer nursing. 2003 Aug;26(4):253–259. doi: 10.1097/00002820-200308000-00001. [DOI] [PubMed] [Google Scholar]
- 23.Bishop MM, Beaumont JL, Hahn EA, et al. Late effects of cancer and hematopoietic stem-cell transplantation on spouses or partners compared with survivors and survivor-matched controls. J Clin Oncol. 2007 Apr 10;25(11):1403–1411. doi: 10.1200/JCO.2006.07.5705. [DOI] [PubMed] [Google Scholar]
- 24.Fife BL, Monahan PO, Abonour R, Wood LL, Stump TE. Adaptation of family caregivers during the acute phase of adult BMT. Bone Marrow Transplantation. 2009;43(12):959–966. doi: 10.1038/bmt.2008.405. [DOI] [PubMed] [Google Scholar]
- 25.Keogh F, O’Riordan J, McNamara C, Duggan C, McCann SR. Psychosocial adaptation of patients and families following bone marrow transplantation: a prospective, longitudinal study. Bone Marrow Transplant. 1998 Nov;22(9):905–911. doi: 10.1038/sj.bmt.1701443. [DOI] [PubMed] [Google Scholar]
- 26.Kim Y, Wellisch DK, Spillers RL, Crammer C. Psychological distress of female cancer caregivers: effects of type of cancer and caregivers’ spirituality. Support Care Cancer. 2007 Dec;15(12):1367–1374. doi: 10.1007/s00520-007-0265-4. [DOI] [PubMed] [Google Scholar]
- 27.Meehan KR, Fitzmaurice T, Root L, Kimtis E, Patchett L, Hill J. The financial requirements and time commitments of caregivers for autologous stem cell transplant recipients. The journal of supportive oncology. 2006 Apr;4(4):187–190. [PubMed] [Google Scholar]
- 28.Hermann C. A guide to the spiritual needs of elderly cancer patients. Geriatr Nurs. 2000 Nov-Dec;21(6):324–325. doi: 10.1067/mgn.2000.gn00324. [DOI] [PubMed] [Google Scholar]
- 29.Hampton DM, Hollis DE, Lloyd DA, Taylor J, McMillan SC. Spiritual needs of persons with advanced cancer. Am J Hosp Palliat Care. 2007 Feb-Mar;24(1):42–48. doi: 10.1177/1049909106295773. [DOI] [PubMed] [Google Scholar]
- 30.Weaver AJ, Flannelly KJ. The role of religion/spirituality for cancer patients and their caregivers. South Med J. 2004 Dec;97(12):1210–1214. doi: 10.1097/01.SMJ.0000146492.27650.1C. [DOI] [PubMed] [Google Scholar]
- 31.Archbold PG, Stewart BJ, Greenlick MR, Harvath T. Mutuality and preparedness as predictors of caregiver role strain. Res Nurs Health. 1990 Dec;13(6):375–384. doi: 10.1002/nur.4770130605. [DOI] [PubMed] [Google Scholar]
- 32.Schumacher KL, Stewart BJ, Archbold PG, Caparro M, Mutale F, Agrawal S. Effects of caregiving demand, mutuality, and preparedness on family caregiver outcomes during cancer treatment. Oncology nursing forum. 2008 Jan;35(1):49–56. doi: 10.1188/08.ONF.49-56. [DOI] [PubMed] [Google Scholar]
- 33.Wilson ME, Eilers J, Heermann JA, Million R. The experience of spouses as informal caregivers for recipients of hematopoietic stem cell transplants. Cancer nursing. 2009 May-Jun;32(3):E15–23. doi: 10.1097/NCC.0b013e31819962e0. [DOI] [PubMed] [Google Scholar]
- 34.NafCa A Caregiving in the United States. 2004 [Google Scholar]
- 35.Acton GJ. Health-promoting self-care in family caregivers. West J Nurs Res. 2002 Feb;24(1):73–86. doi: 10.1177/01939450222045716. [DOI] [PubMed] [Google Scholar]
- 36.Cimprich B, Janz NK, Northouse L, Wren PA, Given B, Given CW. Taking CHARGE: A self-management program for women following breast cancer treatment. Psychooncology. 2005 Sep;14(9):704–717. doi: 10.1002/pon.891. [DOI] [PubMed] [Google Scholar]
- 37.Sorensen S, Pinquart M, Duberstein P. How effective are interventions with caregivers? An updated meta-analysis. Gerontologist. 2002 Jun;42(3):356–372. doi: 10.1093/geront/42.3.356. [DOI] [PubMed] [Google Scholar]
- 38.Ploeg J, Biehler L, Willison K, Hutchison B, Blythe J. Perceived support needs of family caregivers and implications for a telephone support service. Can J Nurs Res. 2001 Sep;33(2):43–61. [PubMed] [Google Scholar]
- 39.Mkanta WN, Chumbler NR, Richardson LC, Kobb RF. Age-related differences in quality of life in cancer patients: a pilot study of a cancer care coordination/home-telehealth program. Cancer nursing. 2007 Nov-Dec;30(6):434–440. doi: 10.1097/01.NCC.0000300167.80466.91. [DOI] [PubMed] [Google Scholar]
- 40.Grimm PM, Zawacki KL, Mock V, Krumm S, Frink BB. Caregiver responses and needs. An ambulatory bone marrow transplant model. Cancer Pract. 2000 May-Jun;8(3):120–128. doi: 10.1046/j.1523-5394.2000.83005.x. [DOI] [PubMed] [Google Scholar]
- 41.Bucher JA, Loscalzo M, Zabora J, Houts PS, Hooker C, BrintzenhofeSzoc K. Problem-solving cancer care education for patients and caregivers. Cancer Pract. 2001 Mar-Apr;9(2):66–70. doi: 10.1046/j.1523-5394.2001.009002066.x. [DOI] [PubMed] [Google Scholar]
- 42.Mittelman M. Taking care of the caregivers. Curr Opin Psychiatry. 2005 Nov;18(6):633–639. doi: 10.1097/01.yco.0000184416.21458.40. [DOI] [PubMed] [Google Scholar]
- 43.McMillan SC, Small BJ, Weitzner M, et al. Impact of coping skills intervention with family caregivers of hospice patients with cancer: a randomized clinical trial. Cancer. 2006 Jan 1;106(1):214–222. doi: 10.1002/cncr.21567. [DOI] [PubMed] [Google Scholar]
- 44.Dellasega C, Zerbe TM. Caregivers of frail rural older adults. Effects of an advanced practice nursing intervention. J Gerontol Nurs. 2002 Oct;28(10):40–49. doi: 10.3928/0098-9134-20021001-11. [DOI] [PubMed] [Google Scholar]
- 45.Rexilius SJ, Mundt C, Erickson Megel M, Agrawal S. Therapeutic effects of massage therapy and handling touch on caregivers of patients undergoing autologous hematopoietic stem cell transplant. Oncology nursing forum. 2002 Apr;29(3):E35–44. doi: 10.1188/02.ONF.E35-E44. [DOI] [PubMed] [Google Scholar]
- 46.Carter PA. A brief behavioral sleep intervention for family caregivers of persons with cancer. Cancer nursing. 2006 Mar-Apr;29(2):95–103. doi: 10.1097/00002820-200603000-00003. [DOI] [PubMed] [Google Scholar]
- 47.McDonald A, Burjan E, Martin S. Yoga for patients and carers in a palliative day care setting. Int J Palliat Nurs. 2006 Nov;12(11):519–523. doi: 10.12968/ijpn.2006.12.11.22399. [DOI] [PubMed] [Google Scholar]
- 48.Jacobsen PB, Meade CD, Stein KD, Chirikos TN, Small BJ, Ruckdeschel JC. Efficacy and costs of two forms of stress management training for cancer patients undergoing chemotherapy. J Clin Oncol. 2002 Jun 15;20(12):2851–2862. doi: 10.1200/JCO.2002.08.301. [DOI] [PubMed] [Google Scholar]
- 49.Cimprich B, Ronis DL. An environmental intervention to restore attention in women with newly diagnosed breast cancer. Cancer nursing. 2003 Aug;26(4):284–292. doi: 10.1097/00002820-200308000-00005. quiz 293-284. [DOI] [PubMed] [Google Scholar]