Abstract
Background
The 2004 introduction of the pay-for-performance contract has increased the proportion of income that GPs are able to earn by targeting quality care to patients with chronic diseases such as hypertension.
Aim
To investigate the impact of pay for performance on the management of patients with hypertension in Scottish primary care.
Design and setting
A population-based repeated cross-sectional study in Scottish primary care practices (n = 315) contributing to the Primary Care Clinical Informatics Unit database.
Method
A dataset was extracted on 826 973 patients aged ≥40 years including, age, sex, socioeconomic deprivation status, hypertension diagnosis, recorded blood pressure measurement, attainment of target blood pressure levels, and provision of hypertension-related prescribing for each year from 2001 until 2006.
Results
Increasing treatment for hypertension (absolute difference [AD] 9.2%; 95% confidence interval [CI] = 9.0 to 9.5) occurred throughout the study period. The majority of increases found in blood pressure measurement (AD 46.8%; 95% CI = 46.5 to 47.1) and recorded hypertension (AD 5.9%; 95% CI = 5.7 to 6.0) occurred prior to 2004. Blood pressure control increased throughout the study period (absolute increase ≤140/90 mmHg; 18.9%; 95% CI = 18.5 to 19.4). After 2004, the oldest female, as well as the male and female patients with the greatest socioeconomic deprivation status, became less likely than their youngest (<40 years) and most affluent counterparts to have a blood pressure measurement recorded (P<0.05). Patients not prescribed therapy were younger and had higher blood pressure levels (P<0.001).
Conclusion
It is likely that the continued efforts of general practice to improve hypertension diagnosis, monitoring, and treatment will reduce future cardiovascular events and mortality in those with hypertension. However, there is a need to follow up patients who are older and more socioeconomically deprived once they are diagnosed, as well as prescribing antihypertensive therapy to younger patients, who are likely to benefit from early intervention.
Keywords: disease management, epidemiology, hypertension, pay for performance, prescriptions, primary care
INTRODUCTION
Cardiovascular diseases such as stroke, coronary heart disease, and heart failure account for almost a third of global deaths.1 Many episodes of these diseases are preventable, with hypertension — among other risk factors — being potentially modifiable.2 In two surveys of people in England, the proportion of people with hypertension but controlled blood pressure (<140/90 mmHg) rose from 22% in 2003 to 28% in 2006.3 This picture of marked improvement may, at least in part, have resulted from the introduction of the target-based new General Medical Services (nGMS) contract introduced to UK primary care in 2004.4
The nGMS contract increased the proportion of income GPs are able to earn from targeted quality care to, potentially, some 23% of total income. For instance, the contract provides payments to practices with an accurate register of patients who have hypertension — a prerequisite for the systematic monitoring of patients. Maximum payment can be achieved when 90% of patients with hypertension have their blood pressure regularly reviewed and if the blood pressure of 70% is below defined target levels.
A previous study found that improvements in the quality of care for patients with asthma, diabetes, or coronary heart disease accelerated in the short term after the introduction of pay for performance under the nGMS contract, but slowed once incentivised targets had been reached.5 Increases in the recording of stroke, coronary heart disease, and diabetes-related quality measures after the introduction of the new contract have also been reported, although not everyone in the population appeared to benefit equally from the improvements.6–8 However, other work has suggested that pay for performance has been accompanied by a diminution of the gap in achieving targets between areas of least and most deprivation.9
In a previous analysis conducted before the nGMS contract, important variations in the primary care management of different patients with hypertension were found: patients who were older and more socioeconomically deprived were 30% less likely to be under regular review (defined as being seen by a GP or nurse and/or prescribed regular antihypertensive therapy) than younger or more affluent individuals.10 Based on previous observations of patients with other conditions, it was hypothesised that the introduction of the target-based nGMS contract would improve the overall care of patients with hypertension registered with GPs, but that not everyone would benefit equally.
METHOD
In April 2000, the Primary Care Clinical Informatics Unit (PCCIU) was created to provide informatics support to primary care in Scotland.11 The aim of the PCCIU is to help primary care practices understand their clinical information needs through feedback reports, based on data extracted from their practice IT records. Data-entry templates have been developed for use by clinicians to systematically record information about a number of long-term conditions, including hypertension.
How this fits in
The pay-for-performance contract was introduced in 2004 but, in the period prior to this, there were large increases in patients recorded with a hypertension diagnosis and a blood pressure measurement. Attainment of blood pressure control and treatment of patients increased slowly and progressively throughout the study period (2001–2006). It is likely that the continued efforts of general practice to improve hypertension diagnosis, monitoring, and treatment will reduce future cardiovascular events and deaths in this population. However, during the study period, new inequalities emerged, particularly in the measurement of blood pressure in those patients who are older and socioeconomically deprived (who had the highest rates of hypertension and where the burden of future cardiovascular-related morbidity and mortality is likely to be highest) and in younger patients (who were less likely to be treated for hypertension). With the substantial increase in the number of patients recorded with a diagnosis of hypertension, there is an opportunity in general practice to ensure that all groups of patients are followed-up and managed appropriately.
A total of 315 (out of 1030; 30.6%) practices in Scotland contributed their computerised patient data to the PCCIU in April 2007. The 1.8 million patients registered with these practices have been found to be representative of the Scottish population (5.1 million).12 Almost all individuals resident in Scotland are registered with a primary care practice, which provides healthcare services free of charge. From the accumulated data all patients aged ≥40 years with a computer record of hypertension were identified (Read code G2, G20 and below, G24–G2z) and no subsequent recording of a Read code indicating that their hypertension had resolved (Read code 21261 and 212K) at six time points (1 April 2001, 1 April 2002, 1 April 2003, 1 April 2004, 1 April 2005, and 1 April 2006).
The following key characteristics of each identified person at each time point were determined:
sex;
age (grouped 40–59 years, 60–75 years, or ≥76 years);
evidence of previous cardiovascular related comorbidity: atrial fibrillation (G573 and below), coronary heart disease (G3%, G30z, G3z, G33), diabetes (C10 and below), heart failure (G58 and below), peripheral vascular disease (G73 and below), stroke or transient ischaemic attack (G56–G654; G656–G65zz; G61 and below, excluding G617; G66 and below; G63y0-1; G6760; G6w; G6x; and G64 and below); and
socioeconomic status, according to deprivation quintile (ranging from 1 [most affluent] to 5 [most deprived], based on Carstair's postcode categorisation [DEPCAT], which uses several indicators of poverty, such as household overcrowding, unemployment, social class, and proportion of all persons in private households with no car).13
The study then ascertained whether the identified individuals' computer records had, in the following year (for example, for 2006: 1 April 2006–31 March 2007), a measurement of blood pressure and, where appropriate, evidence of achieving target blood pressures according to British Hypertension Society and nGMS contract targets — that is, a recorded blood pressure measurement of systolic/diastolic ≤140/90 mmHg14 or ≤150/90 mmHg4 respectively. If more than one entry existed, the mean of any measurements in the year were used.
The study also determined whether the patient was prescribed one or more prescriptions of an alpha-blocker or centrally acting agent, angiotensin converting enzyme (ACE) inhibitor, angiotensin receptor blocker (ARB), a beta-blocker, a calcium channel antagonist, or a diuretic (including thiazides) in the 3 months preceding each time point (for example, for 2006: 1 January–31 March).
This study was approved under PCCIU research governance procedures.
Statistical analyses
Independent t-tests were used to determine changes in mean blood pressure. For the difference in proportions, 95% confidence intervals (CIs) were calculated.15 Logistic regression models were used to determine any differences between groups. Men and women were considered separately in the models because of interactions seen between age and sex for blood pressure measurement, therapy, and control. The covariates (independent variables) used in the logistic model were patient characteristics, namely age (in years), presence of cardiovascular disease-related comorbidities, and socioeconomic category. The coefficients of these independent variables are presented as adjusted odds ratios (AORs), together with their 95% CIs. To account for the effect of the clustering of patients within practices, adjustment was also made using robust standard errors.
In addition to controlling for potential confounding in these models, the study included interaction terms in the full logistic regression model to determine whether there was an association between a patient being present in the first year (2001) or the last year (2006) of the study, and whether the recording of quality indicators varied by age or deprivation status. All variables and terms for interaction in the first and last study years were entered simultaneously. All analyses were performed using SPSS for Windows (version 17.0) and Stata 9.2.
RESULTS
Blood pressure recording
In the three time points prior to the first nGMS contract census date in April 2004, an increasing number of patients registered with the PCCIU practices with hypertension had a blood pressure recorded in their primary care electronic health records (Figure 1). (Absolute difference [AD]: 46.8%; 95% confidence interval [CI] = 46.5 to 47.1).
Figure 1.
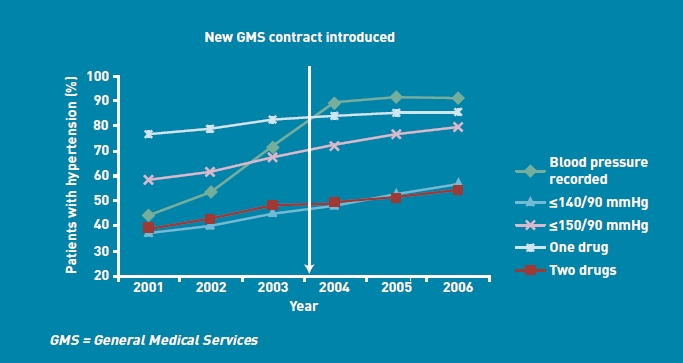
Blood pressure recording, control, and antihypertensive therapy in population with hypertension.
Recording of hypertension diagnosis
Over the study period, the number of registered patients aged ≥40 years with a primary care computer record of hypertension increased (Table 1; AD: 5.9%; 95% CI = 5.7 to 6.0). The largest increase in patients recorded as having hypertension occurred between 2003 and 2004, when the nGMS contract was introduced (3.5%; 95% CI = 3.4 to 3.6, Table 1).
Table 1.
Characteristics of patients with hypertension diagnosis (aged ≥40 years)
| 2001 (%) | 2002 (%) | 2003 (%) | 2004 (%) | 2005 (%) | 2006 (%) | Difference % (95% CI) 2001-2006 | |
|---|---|---|---|---|---|---|---|
| Patients with | 142 976/784 948 | 160 508/813 417 | 155 932/789 908 | 192 508/828 327 | 205 810/842 745 | 199 207/826 973 | 5.9 |
| hypertension/total: | (18.2) | (19.7) | (19.7) | (23.2) | (24.4) | (24.1) | (5.7 to 6.0) |
| Sex | |||||||
| Women | 84 011 (20.3) | 93 416 (21.9) | 90 818 (21.9) | 110 663 (25.5) | 117 381 (26.7) | 113 467 (26.3) | 6.0 (5.6 to 6.0) |
| Men | 58 965 (15.9) | 67 092 (17.4) | 65 114 (17.4) | 81 845 (20.7) | 88 429 (22.0) | 85 740 (21.7) | 5.8 (5.6 to 6.0) |
| Age band (years) | |||||||
| 40–59 | 43 105 (9.7) | 47 933 (10.4) | 47 736 (10.4) | 56 317 (11.9) | 59 335 (12.3) | 59 052 (11.1) | 2.5 (2.4 to 2.6) |
| 60–75 | 67 074 (28.2) | 74 340 (30.5) | 72 784 (30.7) | 70 968 (35.6) | 93 859 (37.4) | 91 770 (37.3) | 9.1 (8.8 to 9.4) |
| ≥76 | 32 797 (31.5) | 38 235 (35.6) | 35 412 (37.1) | 36 500 (45.0) | 52 616 (48.6) | 48 385 (49.2) | 17.7 (17.3 to 18.1) |
| Deprivation quintile | |||||||
| 1 | 25 581 (16.5) | 28 640 (17.9) | 27 987 (17.9) | 34 594 (21.1) | 36 891 (22.1) | 35 775 (21.8) | 5.3 (5.1 to 5.6) |
| 2 | 30 643 (18.2) | 35 094 (19.6) | 34 209 (19.6) | 41 828 (22.8) | 45 211 (24.1) | 43 923 (23.7) | 5.5 (5.3 to 5.8) |
| 3 | 33 696 (18.9) | 37 475 (20.5) | 36 617 (20.5) | 45 559 (24.3) | 48 581 (25.4) | 47 054 (25.1) | 6.2 (5.9 to 6.4) |
| 4 | 27 157 (18.4) | 30 357 (19.9) | 29 321 (19.9) | 36 930 (23.6) | 38 864 (24.9) | 37 540 (24.6) | 6.3 (6.0 to 6.5) |
| 5 | 25 899 (19.1) | 28 942 (20.8) | 27 798 (20.9) | 34 137 (24.6) | 36 264 (25.7) | 34 915 (25.3) | 6.2 (5.9 to 6.5) |
| Comorbidities | |||||||
| Diabetes | 16 450 (47.2) | 20 126 (50.5) | 21 559 (49.6) | 27 586 (57.3) | 31 002 (59.4) | 32 330 (58.3) | 11.1 (10.4 to 11.8) |
| Chronic kidney disease | 934 (59.1) | 1201 (62.5) | 1408 (62.0) | 1851 (68.9) | 2119 (71.1) | 2250 (70.7) | 11.6 (8.7 to 14.5) |
| Coronary heart disease | 23 645 (38.7) | 26 748 (41.4) | 27 233 (41.0) | 32 001 (47.3) | 33 545 (49.1) | 33 149 (48.6) | 9.8 (9.3 to 10.4) |
| Atrial fibrillation | 6325 (40.2) | 7611 (43.4) | 8165 (44.0) | 10 168 (50.6) | 11 167 (52.6) | 11 730 (52.1) | 12.0 (10.9 to 13.0) |
| Stroke | 12 963 (48.1) | 14 971 (51.1) | 15 457 (50.2) | 18 630 (57.6) | 19 980 (59.9) | 19 994 (58.7) | 10.6 (9.8 to 11.3) |
| Peripheral vascular disease | 6852 (39.0) | 7923 (41.8) | 8187 (41.3) | 9860 (47.4) | 10 439 (49.1) | 10 363 (48.3) | 9.3 (8.4 to 10.3) |
| Heart failure | 5974 (39.3) | 6294 (42.5) | 7224 (43.2) | 8397 (49.1) | 8824 (51.1) | 8655 (51.0) | 11.6 (10.5 to 12.7) |
Blood pressure control
Increases in blood pressure target attainment took place throughout the study period (Figure 1; absolute increase ≤140/90 mmHg: 18.9%; 95% CI = 18.5 to 19.4). Such that by 2006, more than half of patients with hypertension achieved the British Hypertension Society blood pressure target (≤140/90 mmHg), and four-fifths achieved the new contract target (≤150/90 mmHg). There was no evidence of a change in trend after the introduction of pay for performance. The mean systolic blood pressure (where measured) among patients with a recorded diagnosis of hypertension fell over the study period by 7.6 mmHg (95% CI = 7.4 to 7.7; P<0.001) (Table 2). Mean diastolic blood pressure also fell by 3.8 mmHg (95% CI = 3.8 to 3.9; P<0.001).
Table 2.
Mean diastolic and systolic blood pressures
| Year | Diastolic blood pressure mmHg (standard error) | Systolic blood pressure mmHg (standard error) |
|---|---|---|
| 2001 | 82.2 (0.04) | 146.9 (0.06) |
| 2002 | 81.5 (0.04) | 145.8 (0.06) |
| 2003 | 80.5 (0.03) | 143.7 (0.05) |
| 2004 | 80.4 (0.02) | 142.2 (0.04) |
| 2005 | 79.2 (0.02) | 140.6 (0.03) |
| 2006 | 78.4 (0.02) | 139.3 (0.04) |
Treatment
During the study period, there was a constant increase in the total number of patients recorded as having hypertension who were treated with at least one or two antihypertensive drugs (Figure 1; AD: 9.2%; 95% CI = 9.0 to 9.5). The largest increase over time in hypertension-related prescribing was for ACE inhibitors or ARBs. Only ACE inhibitors or ARBs were increasingly prescribed as a monotherapy over the study period (Figure 2). Diuretics remained the most commonly prescribed class of antihypertensive therapy (as monotherapy or in combination with other antihypertensive therapies). Patients not prescribed any therapy (in 2006) tended to be significantly younger (66.0 versus 68.3 years), have been diagnosed with hypertension for less time (7.2 versus 7.4 years) and have higher mean systolic (141.1 versus 139.0 mmHg) and diastolic blood pressure (81.2 versus 78.0; P<0.001) than patients prescribed at least one therapy.
Figure 2.
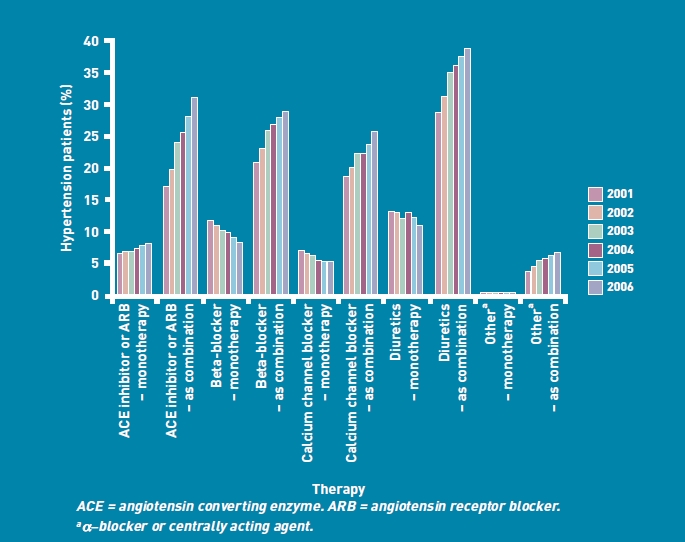
Mono or combined blood pressure treatments for patients with hypertension.
Sex, age, deprivation and comorbidity differences
At most time points, a greater proportion of women, older, and more deprived people than their counterparts, were recorded as having hypertension (Table 1). For most years, increases were found in the recording of hypertension across groups. The oldest group of women (aged ≥76 years) tended to be less likely than the youngest women (40–59 years) to have their blood pressure recorded (Table 3; P<0.05). At the most recent time point (2006), the patients with the greatest levels of deprivation in both sexes were less likely to have their blood pressure recorded than patients with the least level of deprivation (Table 4; P<0.05). Patients with chronic kidney disease had the highest proportion (of comorbidity groups) with a diagnosis of hypertension (Table 1). The largest increase in the recording of hypertension occurred for patients with atrial fibrillation.
Table 3.
Odds ratios for association of blood pressure recording, control, and treatment of patients by age
| Blood pressure recorded | Recorded with blood pressure (≤140/90 mmHg) | Recorded with blood pressure (≤150/90 mmHg) | Treated with at least one drug | Treated and blood pressure below target (≤150/90 mmHg) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Odds ratioa | Odds ratioa | Odds ratioa | Odds ratioa | Odds ratioa | |||||||
| Year | % | (95% CI) | % | (95% CI) | % | (95% CI) | % | (95% CI) | % | (95% CI) | |
| Female | |||||||||||
| Age band, years ≥76b | 2001 | 42.3 | 0.93 | 31.0 | 0.54 | 51.4 | 0.60 | 79.4 | 1.39 | 52.0 | 0.55 |
| (0.84 to 1.02) | (0.50 to 0.57) | (0.56 to 0.64) | (1.30 to 1.47) | (0.51 to 0.59) | |||||||
| 2002 | 50.2 | 0.93 | 33.7 | 0.54 | 54.8 | 0.60 | 81.4 | 1.34 | 55.1 | 0.55 | |
| (0.84 to 1.02) | (0.50 to 0.57) | (0.56 to 0.64) | (1.25 to 1.43) | (0.51 to 0.58) | |||||||
| 2003 | 66.9 | 0.80 | 38.8 | 0.53 | 60.4 | 0.59 | 82.9 | 1.25 | 60.9 | 0.53 | |
| (0.75 to 0.87) | (0.50 to 0.56) | (0.55 to 0.62) | (1.16 to 1.34) | (0.50 to 0.57) | |||||||
| 2004 | 86.1 | 0.80 | 41.2 | 0.50 | 65.9 | 0.59 | 85.5 | 1.41 | 66.4 | 0.54 | |
| (0.74 to 0.87) | (0.48 to 0.52) | (0.56 to 0.62) | (1.32 to 1.50) | (0.51 to 0.57) | |||||||
| 2005 | 87.9 | 0.74 | 45.6 | 0.51 | 71.3 | 0.63 | 86.3 | 1.42 | 71.9 | 0.57 | |
| (0.69 to 0.80) | (0.49 to 0.54) | (0.59 to 0.66) | (1.33 to 1.52) | (0.54 to 0.60) | |||||||
| 2006 | 87.8 | 0.78 | 49.9 | 0.53 | 74.3 | 0.63 | 86.4 | 1.34 | 74.7 | 0.57 | |
| (0.71 to 0.86)c | (0.51 to 0.56) | (0.60 to 0.66) | (1.23 to 1.45) | (0.54 to 0.61) | |||||||
| Male | |||||||||||
| Age band, years ≥76b | 2001 | 45.5 | 0.93 | 35.5 | 0.54 | 57.0 | 0.60 | 78.2 | 1.42 | 57.7 | 0.74 |
| (0.84 to 1.02) | (0.50 to 0.57) | (0.56 to 0.64) | (1.31 to 1.53) | (0.67 to 0.82) | |||||||
| 2002 | 53.8 | 1.11 | 39.4 | 0.66 | 61.7 | 0.85 | 80.0 | 1.37 | 62.2 | 0.76 | |
| (1.01 to 1.21) | (0.62 to 0.71) | (0.79 to 0.92) | (1.27 to 1.47) | (0.70 to 0.82) | |||||||
| 2003 | 69.6 | 1.01 | 44.2 | 0.68 | 67.7 | 0.89 | 82.1 | 1.38 | 68.4 | 0.83 | |
| (0.92 to 1.10) | (0.64 to 0.73) | (0.83 to 0.96) | (1.27 to 1.50) | (0.77 to 0.90) | |||||||
| 2004 | 87.8 | 1.12 | 48.3 | 0.72 | 73.3 | 1.00 | 85.1 | 1.52 | 74.1 | 0.91 | |
| (1.00 to 1.26) | (0.68 to 0.76) | (0.94 to 1.06) | (1.40 to 1.66) | (0.86 to 0.97) | |||||||
| 2005 | 89.9 | 1.10 | 52.6 | 0.74 | 77.8 | 1.06 | 86.3 | 1.53 | 78.6 | 0.96 | |
| (0.98 to 1.24) | (0.70 to 0.77) | (1.00 to 1.12) | (1.40 to 1.68) | (0.91 to 1.02) | |||||||
| 2006 | 88.8 | 0.97 | 57.5 | 0.81 | 81.4 | 1.20 | 86.1 | 1.35 | 81.9 | 1.11 | |
| (0.85 to 1.09)c | (0.77 to 0.84)c | (1.13 to 1.28)c | (1.23 to 1.50) | (1.04 to 1.19)c | |||||||
Odds ratio (95% CI) adjusted for deprivation and comorbidities where appropriate.
Reference group: aged 40–59 years.
Statistically significant associations between 2001 and 2006 (P<0.05).
Table 4.
Odds ratios for association of blood pressure recording, control, and treatment of patients by Carstairs deprivation quintile
| Blood pressure recorded | Recorded with blood pressure (≤140/90 mmHg) | Recorded with blood pressure (≤150/90 mmHg) | Treated with at least one drug | Treated and blood pressure below target (≤150/90 mmHg) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Odds ratioa | Odds ratioa | Odds ratioa | Odds ratioa | Odds ratioa | |||||||
| Year | % | (95% CI) | % | (95% CI) | % | (95% CI) | % | (95% CI) | % | (95% CI) | |
| Female | |||||||||||
| Deprivation | 2001 | 5.29 | 1.19 | 36.2 | 1.06 | 56.7 | 1.00 | 78.1 | 1.02 | 58.3 | 1.02 |
| quintile | (0.90 to 1.58) | (0.93 to 1.21) | (0.86 to 1.15) | (0.89 to 1.13) | (0.88 to 1.19) | ||||||
| 5b | 2002 | 5.91 | 1.19 | 39.7 | 1.06 | 60.1 | 1.00 | 81.1 | 1.04 | 62.1 | 1.03 |
| (0.90 to 1.58) | (0.93 to 1.21) | (0.86 to 1.15) | (0.93 to 1.17) | (0.89 to 1.19) | |||||||
| 2003 | 74.8 | 1.09 | 44.2 | 1.03 | 66.0 | 0.96 | 83.7 | 1.01 | 67.2 | 0.97 | |
| (0.85 to 1.40) | (0.91 to 1.15) | (0.85 to 1.09) | (0.90 to 1.14) | (0.85 to 1.11) | |||||||
| 2004 | 89.2 | 0.90 | 48.4 | 1.00 | 71.8 | 0.96 | 84.5 | 0.98 | 72.9 | 0.96 | |
| (0.74 to 0.97) | (0.90 to 1.12) | (0.84 to 1.09) | (0.87 to 1.10) | (0.84 to 1.09) | |||||||
| 2005 | 90.9 | 0.84 | 53.5 | 1.05 | 76.7 | 0.99 | 85.3 | 0.99 | 77.8 | 0.99 | |
| (0.72 to 0.97) | (0.93 to 1.18) | (0.87 to 1.13) | (0.88 to 1.11) | (0.87 to 1.12) | |||||||
| 2006 | 90.4 | 0.83 | 57.1 | 1.00 | 79.3 | 0.93 | 86.1 | 0.96 | 80.0 | 0.92 | |
| (0.72 to 0.96)c | (0.89 to 1.12) | (0.83 to 1.05) | (0.85 to 1.07) | (0.81 to 1.04) | |||||||
| Male | |||||||||||
| Deprivation | 2001 | 52.4 | 1.19 | 39.0 | 1.06 | 58.8 | 1.00 | 74.0 | 0.90 | 60.2 | 0.90 |
| quintile | (0.90 to 1.58) | (0.93 to 1.21) | (0.86 to 1.15) | (0.79 to 1.03) | (0.76 to 1.06) | ||||||
| 5b | 2002 | 60.0 | 1.18 | 41.8 | 1.00 | 61.9 | 0.89 | 76.9 | 0.95 | 63.7 | 0.88 |
| (0.90 to 1.54) | (0.87 to 1.14) | (0.78 to 1.02) | (0.84 to 1.07) | (0.76 to 1.02) | |||||||
| 2003 | 74.2 | 1.01 | 47.1 | 0.96 | 67.8 | 0.86 | 80.1 | 0.93 | 69.4 | 0.85 | |
| (0.79 to 1.28) | (0.86 to 1.07) | (0.76 to 0.97) | (0.81 to 1.05) | (0.75 to 0.96) | |||||||
| 2004 | 88.3 | 0.87 | 50.7 | 0.96 | 73.0 | 0.92 | 81.7 | 0.91 | 74.8 | 0.92 | |
| (0.73 to 1.04) | (0.86 to 1.07) | (0.81 to 1.04) | (0.81 to 1.03) | (0.80 to 1.05) | |||||||
| 2005 | 90.6 | 0.88 | 54.3 | 0.96 | 77.1 | 0.89 | 83.1 | 0.90 | 78.7 | 0.90 | |
| (0.77 to 1.01) | (0.85 to 1.08) | (0.79 to 1.01) | (0.79 to 1.02) | (0.79 to 1.02) | |||||||
| 2006 | 89.8 | 0.84 | 58.8 | 0.98 | 79.9 | 0.92 | 84.2 | 0.88 | 81.0 | 0.91 | |
| (0.71 to 0.98)c | (0.88 to 1.10) | (0.81 to 1.03) | (0.77 to 1.00) | (0.80 to 1.02) | |||||||
Odds ratio (95% CI) adjusted for age (in years) and comorbidities.
Reference group: deprivation quintile 1 (least deprived).
Statistically significant associations between 2001 and 2006
DISCUSSION
Summary
Over the study period — and, in particular, the years just prior to the introduction of the incentive-based nGMS contract, when GPs were improving patient disease registers in preparation for pay for performance — there was a large increase in the proportion of patients with hypertension recorded on their practice computer records. For these patients, there were increases, over time, in the proportions that were treated with hypertension-related therapy and that achieved blood pressure targets as well as reductions in mean blood pressure. These patients were also increasingly likely to have a blood pressure measurement noted electronically during the period just prior to the contract introduction.
Important differences between groups emerged during the study period: the women who were oldest and had the greatest socioeconomic deprivation status, together with the men with the greatest socioeconomic deprivation status, became less likely to have a recorded blood pressure measurement than younger and more affluent patients. Furthermore, the youngest patients in this study with hypertension were less likely to be prescribed a therapy.
Strengths and limitations
The main strengths of this study include the interrogation of a large nationally representative dataset16 and the observation of a range of processes and clinical endpoints. However, although the long-term nature of the database and its clinical focus helps to ensure that initially uncertain events are confirmed or refuted over time — especially those requiring continued care, such as hypertension — no direct validation of the hypertension diagnosis, drug prescribing, or blood pressure measurement was undertaken in this study.
The introduction of the nGMS contract has highlighted the importance (both clinically and financially) of high-quality disease registers with accurate data, including blood pressure measurements. In addition, while some inaccuracies undoubtedly exist, there is little reason to suppose that there are systematic errors between subgroups with each dataset.17 The study was unable to control directly for disease severity or duration, although it could allow for differences between groups in a number of other confounders such as age, sex, deprivation status, number of cardiovascular-related comorbidities, and the effect of clustering within practices. Residual confounding, however, may explain the current results.
The data presented in this study were derived from the electronic recording of data on primary care computer systems. An unknown amount of the increase in the recording of blood pressure and treatment will have occurred because of the transfer of data from paper to electronic patient records (rather than from the provision of additional care). However, it seems unlikely that practitioners would have systematically improved their computerised documentation of hypertension-related care for only certain groups of patients (for example, females).
The non-experimental design of the study means that the observed changes cannot be directly attributed to the nGMS contract. It is possible that other developments may have contributed, such as an increased awareness of patients and how best to manage their hypertension, as well as the impact of clinical guidelines. Nevertheless, the strong relationship between reaching targets and payment to practices suggests that the nGMS contract was a major driver, particularly in terms of increased electronic recording of hypertension diagnoses and blood pressure measurements.
Comparison with existing literature
The study findings differ from recent relevant national health survey data. For instance, the 2003 Scottish Health Survey found more patients in the community with hypertension (32%), of which a larger proportion (69%) had a blood pressure of <140/90 mmHg; however, a smaller proportion was receiving blood pressure lowering treatment (44%).18 Among those recorded as having hypertension and receiving treatment, fewer achieved blood pressure control (46%)18 than in the current study. These differences between studies are likely to reflect the contrasting methods used to find cases and collect data (interview and nurse visit for a community survey versus opportunistic screening and primary care electronic data recording), age differences of the populations studied (≥16 years versus ≥40 years), and differing definitions of hypertension (Scottish Health Survey: blood pressure ≥140/90 mmHg or antihypertensive medication versus PCCIU data: doctor diagnosis).
It is of note that in the Scottish Health Survey,18 slightly more men than women were classified as having hypertension (33.0% versus 31.7%); the opposite was true for patients recorded as having hypertension in the current primary care dataset. One explanation for this difference may be that more women than men present to primary care (for a range of conditions but, in particular, for genitourinary problems, reproductive health care, and reasons classified as minor or intermediate),19 and so have a greater opportunity for blood pressure to be measured and hypertension diagnosed. Women with hypertension may also be more aware of their diagnosis than men, and more likely to participate in follow up.20
The association between hypertension prevalence and low socioeconomic status in this study has been discussed previously.21 The association between increasing age and reduction in blood pressure control was also found in a North American study of men and women with hypertension.22 Using data from all general practices in England, higher rates of blood pressure monitoring were found in 2004–2005 among practices located in affluent areas, when compared with practices in areas of deprivation; by 2006–2007, only negligible differences were found.9 By using patient-level data from a longer period of time and adjusting for potential confounding of age and comorbidity, significant differences were found emerging over time in terms of blood pressure monitoring between patients who were affluent and those with a high deprivation status. These differences may, partially, be due to patients with a high deprivation status refusing or not responding to requests to attend primary care clinics for regular blood pressure monitoring.23
Implications for research and practice
Organised regular review, allied to the aggressive use of antihypertensive drug therapy, has been shown to reduce blood pressure and all-cause mortality in the longer term.24 During the preparation period for the nGMS contract for general practices in Scotland, increases were observed in the proportion of patients who were recorded as having hypertension, who had their blood pressure recorded, and who achieved blood pressure control. It is likely that the large increase in blood pressure monitoring resulted from the 90% threshold set under the terms of the contract for maximum payment, and the attempt by practices in Scotland to achieve this target by 2004 when pay for performance was introduced. However, new inequalities emerged, particularly in the inadequate measurement of blood pressure for patients who were older and had a high socioeconomic deprivation status. These patients also had the highest rates of hypertension. The burden of future cardiovascular-related morbidity and mortality is likely to be highest in these groups of patients;25 as such, further programmes should be developed, not only to ascertain hypertension in patients, but also to ensure follow up after diagnosis. A gap in the treatment of the youngest patients with hypertension has also been found; this group is likely to benefit from therapy as early intervention has been shown to be effective in halting vascular structural damage.26
It is of note that a similar large increase prior to pay for performance was not apparent for the achievement of blood pressure control, which required a more modest 70% threshold for maximum payment — a target near to being achieved in 2003. It is laudable, however, that the proportion of patients prescribed blood pressure therapy and achieving control increased, and that mean blood pressure fell after the 70% threshold set by the contract was reached without further incentives being introduced. It is likely that the continued efforts of general practice to improve hypertension diagnosis, monitoring, and treatment will reduce future cardiovascular events and deaths in this population.
Acknowledgments
We would like to record our thanks to the contributing general practices and patients, and to the PCCIU for providing technical expertise in creating, maintaining, and providing access to its database. We would also like to thank the Institute of Applied Health Science's data management and medical statistical teams.
Funding
This project was funded by a grant from NHS Grampian Endowments [08/45]. Colin R Simpson is supported by a health services and health of the public post-doctoral fellowship from the Chief Scientist Office of the Scottish Government [PDF/08/02].
Ethical approval
All data analyses were conducted using de-identified data and were subject to the Primary Care Clinical Informatics Unit (PCCIU) research governance processes.
Provenance
Freely submitted; externally peer reviewed.
Competing interests
The authors have declared no competing interests.
Ethical approval
All data analyses were conducted using de-identified data and were subject to the Primary Care Clinical Informatics Unit (PCCIU) research governance processes.
Discuss this article
Contribute and read comments about this article on the Discussion Forum: http://www.rcgp.org.uk/bjgp-discuss
REFERENCES
- 1.World Health Organization (2004) The world health report 2004 — changing history. http://www.who.int/entity/whr/2004/annex/topic/en/annex_2_en.pdf (accessed 10 Jun 2011) [Google Scholar]
- 2.Ezzati M, Lopez AD, Rodgers A, et al. Selected major risk factors and global and regional burden of disease. Lancet. 2002;360(9343):1347–1360. doi: 10.1016/S0140-6736(02)11403-6. [DOI] [PubMed] [Google Scholar]
- 3.Falaschetti E, Chaudhury M, Mindell J, Poulter N. Continued improvement in hypertension management in England. Results from the health survey for England 2006. Hypertension. 2009;53(3):480–486. doi: 10.1161/HYPERTENSIONAHA.108.125617. [DOI] [PubMed] [Google Scholar]
- 4.BMA Scotland. Investing in General Practice — the new general medical services contract. http://www.bma.org.uk/sc/employmentandcontracts/independent_contractors/general_medical_services_contract/investinggp.jsp (accessed 3 Jun 2011) [Google Scholar]
- 5.Campbell SM, Reeves D, Kontopantelis E, et al. Effects of pay for performance on the quality of primary care in England. N Engl J Med. 2009;361(4):368–378. doi: 10.1056/NEJMsa0807651. [DOI] [PubMed] [Google Scholar]
- 6.Simpson CR, Hannaford P, Lefevre K, Williams D. Effect of the UK incentive-based contract on the management of patients with stroke in primary care. Stroke. 2006;37(9):2354–2360. doi: 10.1161/01.STR.0000236067.37267.88. [DOI] [PubMed] [Google Scholar]
- 7.McGovern MP, Boroujerdi MA, Taylor MW, et al. The effect of the UK incentive-based contract on the management of patients with coronary heart disease in primary care. Fam Pract. 2008;25(1):33–39. doi: 10.1093/fampra/cmm073. [DOI] [PubMed] [Google Scholar]
- 8.McGovern MP, Williams DJ, Hannaford PC, et al. Introduction of a new incentive target based contract for family physicians in the United Kingdom: good for older patients with diabetes but less good for women? Diabetic Med. 2008;25(9):1083–1089. doi: 10.1111/j.1464-5491.2008.02544.x. [DOI] [PubMed] [Google Scholar]
- 9.Ashworth M, Medina J, Morgan M. Effect of social deprivation on blood pressure monitoring and control in England: a survey of data from the quality and outcomes framework. BMJ. 2008;337:a2030. doi: 10.1136/bmj.a2030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Pears E, Hannaford PC, Taylor MW. Gender, age and deprivation differences in the primary care management of hypertension in Scotland: a cross-sectional database study. Fam Pract. 2003;20(1):22–31. doi: 10.1093/fampra/20.1.22. [DOI] [PubMed] [Google Scholar]
- 11.Royal College of General Practitioners (RCGP) Scotland. Edinburgh: Royal College of General Practitioners; 2003. Making IT work for you. [Google Scholar]
- 12.Carstairs V, Morris R. Aberdeen: Aberdeen University Press; 1991. Deprivation and Health in Scotland. [Google Scholar]
- 13.Elder R, Kirkpatrick M, Ramsay W, et al. Edinburgh: Information and Statistics Division, NHS National Services Scotland; 2007. Measuring quality in primary medical services using data from SPICE. [Google Scholar]
- 14.Williams B, Poulter NR, Brown MJ, et al. British Hypertension Society guidelines for hypertension management 2004 (BHS-IV): summary. BMJ. 2004;328(7440):634–640. doi: 10.1136/bmj.328.7440.634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gardner MJ, Altman DG. Confidence intervals rather than P values: estimation rather than hypothesis testing. BMJ. 1986;292(6522):746–750. doi: 10.1136/bmj.292.6522.746. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.National Health Service (NHS) Scotland. Edinburgh: NHS National Services Scotland; 2007. Measuring quality in primary medical services using data from SPICE. [Google Scholar]
- 17.Department of Health. London: The Department of Health; 2004. The Quality and Outcomes Framework guidance. [Google Scholar]
- 18.The Scottish Government. The Scottish Health Survey. http://www.scotland.gov.uk/Publications/2005/12/02160336/summary-pdf (accessed 10 Jun 2011)
- 19.McCormick A, Fleming D, Charlton J. London: HMSO; 1995. Morbidity statistics from general practice: fourth national study 1991–1992. [Google Scholar]
- 20.Marques-Videl P, Tuolmilehto J. Hypertension awareness, treatment and control in the community: is the rule of halves still valid? J Hum Hypertens. 1997;11(4):213–220. doi: 10.1038/sj.jhh.1000426. [DOI] [PubMed] [Google Scholar]
- 21.Grotto I, Huerta M, Sharabi Y. Hypertension and socioeconomic status. Curr Opin Cardiol. 2008;23(4):335–339. doi: 10.1097/HCO.0b013e3283021c70. [DOI] [PubMed] [Google Scholar]
- 22.Ong KL, Tso AWK, Lam KSL, Cheung BMY. Gender difference in blood pressure control and cardiovascular risk factors in Americans with diagnosed hypertension. Hypertension. 2008;51(4):1142–1148. doi: 10.1161/HYPERTENSIONAHA.107.105205. [DOI] [PubMed] [Google Scholar]
- 23.Simpson CR, Hannaford PC, McGovern M, et al. Are different groups of patients with stroke more likely to be excluded from the new UK general medical services contract? A cross-sectional retrospective analysis of a large primary care population. BMC Fam Pract. 2007;8:56. doi: 10.1186/1471-2296-8-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.[No authors listed] Five-year findings of the hypertension detection and follow-up program. I. Reduction in mortality of persons with high blood pressure, including mild hypertension. JAMA. 1979;242(23):2562–2571. [PubMed] [Google Scholar]
- 25.Tudor-Hart J. The inverse care law. Lancet. 1971;297:405–412. doi: 10.1016/s0140-6736(71)92410-x. [DOI] [PubMed] [Google Scholar]
- 26.Williams B. Hypertension in the young: preventing the evolution of disease versus prevention of clinical events. J Am Coll Cardiol. 2007;50(9):840–842. doi: 10.1016/j.jacc.2007.05.020. [DOI] [PubMed] [Google Scholar]


