Abstract
Objective:
To evaluate the effect of tobacco smoking on the risk of nonfatal acute myocardial infarction in young adults (≤45 years).
Patient and Methods:
We conducted a population-based case-control study with 329 incident acute myocardial infarction cases (42 women; 287 men), consecutively admitted to the Cardiology department of hospitals in Aleppo, Syria, and 778 controls (486 women; 292 men), selected within the noninstitutionalized Aleppo population, during 2008-2010. Odds ratios (OR) and 95% confidence intervals (95%CI) were calculated using unconditional logistic regression.
Results:
The prevalence of current smoking was 80.8% in male cases and 53.8% in male controls (OR = 3.63, 95%CI: 2.50, 5.27) and 59.5% of female cases were smokers compared with 35.8% of controls (OR = 2.64, 95%CI: 1.39, 5.02). No interaction was found between current smoking and gender on myocardial infarction risk (P = 0.401). A dose-effect response was present, the odds favoring myocardial infarction reaching an eight-fold increase for those who smoked >25 cigarettes/day compared with never smokers. The risk estimate for former smokers was similar to never smokers.
Conclusions:
Tobacco smoking is an important independent risk factor for acute myocardial infarction in young adults, with similar strength of association for both genders.
Keywords: Ischemic heart disease, smoking, young patients
INTRODUCTION
The pathologic process leading to coronary artery disease begins early in life, though the clinical consequences of atherosclerosis are apparent mainly in older adults.[1–3] Short-term mortality studies showed that younger patients have more favorable prognosis, but long-term studies showed an overall poor prognosis for individuals with premature coronary artery disease.[4]
Myocardial infarction under the age of 45 years accounts for approximately 10% of all infarctions in the United States,[1] reflecting the perception of an uncommon event in this age group, and often has no evident association with atherosclerotic plaque rupture.[5] Smoking seems to be the most important risk factor for myocardial infarction events among young individuals.[6–8] In fact, active and passive smokers are exposed to a wide range of substances with a potential impact on atherogenesis.
Smoking can trigger myocardial infarction in individuals with minimal atherosclerosis or even with normal coronary arteries, especially among the young,[1–9] promoting temporary coronary vessel occlusion, as a result of thrombus formation, coronary artery spasm, or both.[9] Additionally, smokers tend to present other lifestyle choices, concerning diet and physical activity that have an independent effect on the risk of coronary disease.[10,11] Although smoking is a well established risk factor for early atherosclerosis[1,3,8,12–18] and plaque instability,[19] it has not been comprehensively evaluated using population-based data. Furthermore, gender differences are extremely important to take into account when considering the effect of smoking on myocardial infarction. Several studies describe an increase of myocardial infarction risk in young adults, with no gender differentiation.[8,12,13,16,17] Other studies emphasize differences by gender with a particularly damaging effect of smoking among women,[20–22] but additional information is needed, addressing the issue in the younger groups.
The sparse population-based data on nonfatal myocardial infarction events and the high impact of smoking on the occurrence of myocardial infarction in young adults led us to conduct a population-based case-control study in this age range.
This study aims to evaluate the effect of tobacco smoking on the risk of nonfatal acute myocardial infarction in young adults (≤45 years), and whether there is modification of this effect by gender.
PATIENTS AND METHODS
Case-control study participants
A population-based case-control study was conducted in Aleppo, the second largest city in Syria, with almost 300 000 inhabitants. Cases were Aleppo adults, aged 18 to 45 years, consecutively admitted with a first diagnosis of acute myocardial infarction to the department of Cardiology of the two hospitals providing acute coronary care in Aleppo, and who survived at least 4 days after the acute event. The diagnosis was established according to the criteria defined by the European Society of Cardiology and the American College of Cardiology,[23] considering acute myocardial infarction with and without ST-segment elevation. Patients were interviewed during the hospital stay, between the fourth and eighth days after admission, after clinical stabilization. During the study period, 353 patients were admitted but 22 were unable to participate, died before interview or did not complete the interview. Only two patients refused to participate.
Controls were identified as part of a health and nutrition survey of the adult population of Aleppo, representative of the catchment area of the hospitals where cases were recruited. We used random digit dialing to select households followed by simple random sampling to select one participant within each household.[24] Participants had no financial compensation and refusals were not replaced. The participation proportion was estimated in 63%. After a brief explanation of the purposes of the study, selected participants were invited to visit our department for an interview, which included a questionnaire on social, demographic, behavioral, and clinical data and anthropometrical evaluation. An overnight fasting venous blood sample was obtained, and a spirometry and an electrocardiogram were performed.
For the specific objective of this study, we considered participants aged less than 46 years and recruited during 2008-2010, with no evidence of ischemic heart disease, according to self-reported previous medical diagnosis and electrocardiography. Of 795 community participants, eleven were excluded due to evidence of a previous myocardial infarction and six because of incomplete information. The final sample included 329 cases (42 women and 287 men) and 778 controls (486 women and 292 men).
The Ethics committee of the two participating hospitals approved the study and all participants gave written informed consent.
Data collection
Data on cases and controls were collected by the same group of trained interviewers, with the use of a structured questionnaire. Smoking habits were self-reported and participants were classified based on World Health Organization categories,[25] into never-smokers, current smokers, including daily (at least one cigarette a day) or occasional smokers (less than one cigarette a day), and former smokers (quit smoking for at least 6 months). A subject who quit smoking less than six months was considered as a current smoker (regular or occasional smoker, according the number of cigarettes smoked per day). Current and former smokers were asked about the duration, age at smoking initiation, and the number of cigarettes smoked. The use of other types of tobacco was also questioned and recorded, but we only analyzed the number of cigarettes smoked due to the almost nil contribution of other types of tobacco (only three controls reported the use of tobacco pipe or rolled cigar, but also of cigarettes).
Family history of infarction was considered positive if at least one first-degree relative had an acute myocardial infarction, regardless of the age when the event occurred. Information on dyslipidemia, hypertension, diabetes, and angina was self-reported, based on the question: “Has a Doctor ever told you that you have...?”.
Leisure-time physical activity was quantified after a detailed recall of leisure activities, and expressed as metabolic equivalents.[26] Diet was assessed using a semiquantitative food frequency questionnaire, previously validated for the Portuguese population.[27]
Anthropometrics were obtained with the participants fasting, in light clothing and barefoot. For some independent variables considered as confounders, we have some missing information. The variable with more missing values was the body mass index (for 35 subjects, we could not access their weight and/or height due to methodological limitations at the time of the interview or even because participants refused to be measured).
Statistical analysis
Chi-squared test was used to evaluate the association between two categorical variables. Mann-Whitney test and Student's t-test were used to compare two or more independent samples, according to variables′ distribution. The distribution of variables was tested by Kolmogorov-Smirnov test. To estimate the magnitude of the association between smoking and myocardial infarction, adjusted odds ratios (OR) with 95% confidence intervals (95%CI) were calculated using unconditional logistic regression. The following four different models were considered: model (1) adjusting for gender; model (2) including gender, age, and education as covariates; model (3) including covariates of model 2 and additionally family history of infarction, body mass index, total energy intake, alcohol and caffeine consumption, and leisure-time physical activity; and model (4) including covariates of model 3 and additionally presence (yes or no) of angina, dyslipidemia, hypertension, and diabetes.
When assessing the association between acute myocardial infarction and different covariables, namely gender, effect modification by smoking was evaluated in the regression model testing interaction terms between smoking (dichotomous variable) and those other variables. Data were analyzed using SPSS® version 13.0.
RESULTS
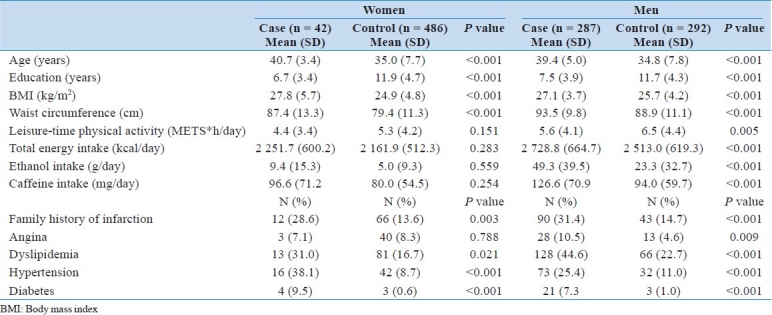
Characteristics of acute myocardial infarction cases and controls are presented in Table 1. Compared with controls, male and female cases were significantly older, less educated, showed higher means of body mass index and waist circumference, and more frequently reported dyslipidemia, hypertension, diabetes, and a family history of myocardial infarction. Additionally, male cases had significantly higher mean intake of total energy, alcohol, and caffeine, and lower mean leisure-time energy expenditure.
Table 1.
Sociodemographic, anthropometric, behavioral, and clinical characteristics of acute myocardial infarction cases and controls, by gender
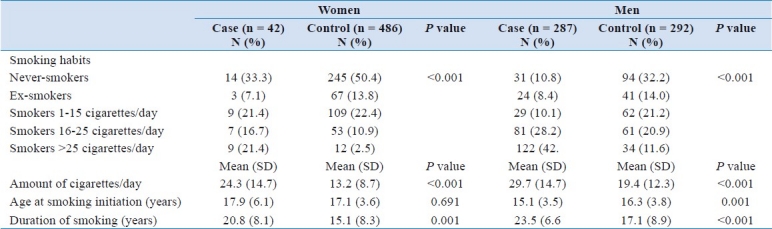
The prevalence of current smoking was 80.8% in male cases and 53.8% in male controls (OR = 3.63, 95%CI: 2.50, 5.27) and 59.5% of female cases were smokers compared with 35.8% of controls (OR = 2.64, 95%CI: 1.39, 5.02) [Table 2] (P value for interaction = 0.401). Heavier smokers (>25 cigarettes/day) were significantly more common among cases, both in women (21.4% vs 2.5%, P<0.001) and men (42.5% vs 11.6%, P<0.001), compared with controls. Mean number of cigarettes smoked per day was significantly higher among female (24.3 vs13.2 cigarettes/day) and male cases (29.7 vs 19.4 cigarettes/day) compared with controls. The mean age of smoking initiation was significantly lower in male cases (15.1 vs 16.3 years, P = 0.001) but not in females (17.9 vs 17.1 years, P = 0.691). Mean years of smoking duration were significantly higher both in female (20.8 vs 15.1 years, P = 0.001) and male cases (23.5 vs 17.1 years, P<0.001), compared with controls.
Table 2.
Smoking habits of acute myocardial infarction cases and controls, by gender
Since we found no significant interaction between current smoking and gender on acute myocardial infarction risk, the association analysis between smoking and acute myocardial infarction occurrence was made with the entire sample.
Myocardial infarction risk increased with increasing daily number of cigarettes smoked. The risk of an acute myocardial infarction doubled in smokers of 1 to 15 cigarettes a day (OR = 2.15, 95% CI: 1.22, 3.76), smokers of 16 to 25 cigarettes had a three times higher risk (OR = 3.11, 95%CI: 1.88, 5.14), and the odds for heavier smokers were eight times higher (OR = 8.35, 95%CI: 4.84, 14.4), compared with never smokers, adjusting for gender, age, and education [Table 3, model 2]. The risk of acute myocardial infarction for former smokers was similar to never smokers (OR = 1.01, 95%CI: 0.54, 1.89).
Table 3.
Adjusted odds ratios and 95% CI of smoking in AMI young patients
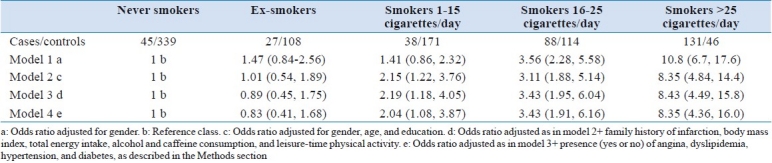
Additional adjustments for clinical, anthropometric, and behavioral covariates [Table 3, models 3 and 4] did not change the magnitude of the association between tobacco smoking and the occurrence of acute myocardial infarction.
DISCUSSION
In this population-based case-control study, a strong positive association was observed between smoking and acute myocardial infarction in young adults, and the effect was not modified by gender. Additionally, a clear dose-effect response was present, the odds favoring myocardial infarction reaching an eight-fold increase for those who smoked more than 25 cigarettes per day.
A recent Danish case-control study reported an OR around 6.0 for current smoking (OR = 6.4, 95%CI: 1.7, 24.1) among young adults,[16] and an Italian study presented an adjusted OR = 32.8 for young heavy smokers.[28] In the Framingham Study, the risk of myocardial infarction also increased with the daily number of cigarettes smoked. An increase of 10 cigarettes per day increased the risk of cardiovascular disease by 18% in men and 31% in women of all ages.[29]
Smoking is considered a major hazard for acute myocardial infarction in both genders, but studies pointed out the particularly harmful effect of the relative estrogen deficiency that female smokers appear to have[22] and suggested more metabolic effects among women,[20] predisposing them to acute myocardial infarction at a relatively younger age.[21] An interaction between oral contraceptives and smoking was also described.[30,31] In our study, we found no gender differences in the case-control evaluation of smoking effect.
Smokers tend to present a social and behavioral profile favoring coronary heart disease.[10,11] Smoking is negatively correlated with body weight, physical activity, and high-density lipoprotein cholesterol and positively with alcohol abuse, psychological stress, total serum cholesterol, and hematocrit levels.[32,33] Interactions between current smoking and such determinants of myocardial infarction were tested in our study, but no significant effect modification was found. Prescott et al. also did not find interaction between smoking and other myocardial infarction risk factors on myocardial infarction risk.[32]
Although young acute myocardial infarction patients contribute relatively little to the overall rate of infarction, significant risk factors identified are mainly those known to influence the development of early coronary atherosclerosis. The similar risk of acute myocardial infarction for former smokers and never smokers argues in favor of the beneficial effect of smoking cessation. The Albany and Framingham combined study showed that one year after quitting, the risk of coronary heart disease decreases by half and, in the long run, ex-smokers revealed similar risks to never-smokers.[34,35] Furthermore, the advantages of smoking cessation in an early age have been emphasized as it increases long-term survival.[36]
Study limitations and strengths
The observational and retrospective nature of this study is prone to specific bias. Trying to minimize recall bias as much as possible, the data collection on cases was done during the hospitalization period and only incident cases were included. These procedures also contributed to avoid potential bias due to behavioral modifications after the acute event. Furthermore, these hospital cases constitute a representative sample of nonfatal myocardial infarction patients, as all myocardial infarction cases that reach any medical care system are admitted to public hospitals.
In our study, educational level of cases and controls barely overlapped. A previous comparison considering the community sample used in this study showed that there were no significant differences between sociodemographic characteristics of participants and refusals,[37] which suggests a low likelihood of participation bias. On the other hand, recruitment of consecutively admitted cases should minimize selection bias at this level. Thus, the difference in educational level between cases and controls probably reflects the strong association between social class and coronary heart disease in our population.
Methodological problems inherent to community sample selection might introduce bias in our estimations. Although 95% of households had a telephone at the time of the recruitment, performed by random digit dialing, a high proportion of refusal was expected among younger participants. When comparing young adults of our community sample with the general population of Aleppo, we observed a similar proportion of adults in our sample at the age group of 30 to 44 years. However, a lower proportion was found for the youngsters (18-29 years) (8.5% vs16.4% for women and 9.0% vs 20.5% for men), which could represent a source of selection bias.
We used self-reported data on dyslipidemia, hypertension, diabetes, and angina. Blood pressure and serum cholesterol and glucose measurements were obtained for all cases and controls, but some measurements could not be obtained in the first 24 hours after infarction, which, together with changes in parameters following acute events, justified the use of self-reported data. Information on smoking was also self-reported and was not confirmed by biochemical tests, although an earlier meta-analysis described a high overall validity for self-reported data on tobacco consumption.[38] To minimize rounding bias, cut-off points at 15 and 25 cigarettes/day were established for the key variable and not 10 and 20 cigarettes (half a pack and a pack of cigarettes, respectively).
Risk estimates for light smokers were somewhat stronger after adjustment for age and education, whereas for the other smoking categories, the same adjustments notably attenuated the risk estimates. This finding can be explained by the differences in age and education distribution across the different smoking habits of participants. Those who smoked 1 to 15 cigarettes/day were younger and more educated than nonsmokers, whereas participants in all other classes of exposure were older and less educated than the reference class. Age is directly associated with acute myocardial infarction and education is inversely associated with the occurrence of the disease in this sample, as in previous reports in the literature. Therefore, when we adjust for age and education, the effect of smoking 1 to 15 cigarettes/day is increased, while the effect in other categories of exposure is attenuated.
The effect of passive smoking on acute myocardial infarction risk was not evaluated in our study. In fact, individuals described as nonsmokers could be at increased risk due to passive smoking, even if only occasionally exposed.[39,40] This might lead to underestimation of the true risk. Although there are missing information for some confounders, we do not think that it affected the results. Our conclusions are based in model 2, with no missing values (for smoking, gender, age, and education, we have information for all subjects, n = 1 107).
Only the models 3 and 4 were calculated with information on 1 068 subjects, because for these, we have to exclude the subjects who had missing information. The few number of missing data in each variable did not allow the inclusion of another category, but adjustments of models 3 and 4 did not change the magnitude of the associations, which put apart the possibility of an information bias.
CONCLUSIONS
This study supports that tobacco smoking is an important independent risk factor for acute myocardial infarction in young adults, with a similar effect for both genders. An increase in female cardiovascular disease morbidity can be expected if no effective interventions targeted particularly to adolescents and young adults take place.[41]
Footnotes
Source of Support: Nil
Conflict of Interest: None declared.
REFERENCES
- 1.Alpert JS, Thygesen K, Antman E, Bassand JP. Myocardial infarction redefined-a consensus document of The Joint European Society of Cardiology/American College of Cardiology Committee for the redefinition of myocardial infarction. J Am Coll Cardiol. 2000;36:959–69. doi: 10.1016/s0735-1097(00)00804-4. [DOI] [PubMed] [Google Scholar]
- 2.Baron JA, La Vecchia C, Levi F. The antiestrogenic effect of cigarette smoking in women. Am J Obstet Gynecol. 1990;162:502–14. doi: 10.1016/0002-9378(90)90420-c. [DOI] [PubMed] [Google Scholar]
- 3.Choudhury L, Marsh JD. Myocardial infarction in young patients. Am J Med. 1999;107:254–61. doi: 10.1016/s0002-9343(99)00218-1. [DOI] [PubMed] [Google Scholar]
- 4.Cole JH, Miller JI, Sperling LS, Weintraub WS. Long-term follow-up of coronary artery disease presenting in young adults. J Am Coll Cardiol. 2003;41:521–8. doi: 10.1016/s0735-1097(02)02862-0. [DOI] [PubMed] [Google Scholar]
- 5.Doll R, Peto R, Boreham J, Sutherland I. Mortality in relation to smoking: 50 years′ observations on male British doctors. BMJ. 2004;328:1519. doi: 10.1136/bmj.38142.554479.AE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Doughty M, Mehta R, Bruckman D, Das S, Karavite D, Tsai T, et al. Acute myocardial infarction in the young—The University of Michigan experience. Am Heart J. 2002;143:56–62. doi: 10.1067/mhj.2002.120300. [DOI] [PubMed] [Google Scholar]
- 7.Doyle JT, Dawber TR, Kannel WB, Heslin AS, Kahn HA. Cigarette smoking and coronary heart disease.Combined experience of the Albany and Framingham studies. N Engl J Med. 1988;266:796–801. doi: 10.1056/nejm196204192661602. [DOI] [PubMed] [Google Scholar]
- 8.Eliasson M, Lundblad D, Hagg E. Cardiovascular risk factors in young snuff-users and cigarette smokers. J Intern Med. 1991;230:17–22. doi: 10.1111/j.1365-2796.1991.tb00401.x. [DOI] [PubMed] [Google Scholar]
- 9.Farley TM, Meirik O, Chang CL, Poulter NR. Combined oral contraceptives, smoking, and cardiovascular risk. J Epidemiol Community Health. 1998;52:775–85. doi: 10.1136/jech.52.12.775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Fitzgerald GA, Oates JA, Nowak J. Cigarette smoking and hemostatic function. Am Heart J. 1988;115:267–71. doi: 10.1016/0002-8703(88)90648-5. [DOI] [PubMed] [Google Scholar]
- 11.Gal DL, Santos AC, Barros H. Leisure-time versus full-day energy expenditure: A cross-sectional study of sedentarism in a Portuguese urban population. BMC Public Health. 2005;5:16. doi: 10.1186/1471-2458-5-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Grundy SM, Balady GJ, Criqui ME. Primary prevention of coronary heart diseases: guidance from Framingham: A statement for health care professionals from the AHATask Force on Risk Reduction. Circulation. 1998;97:1876–87. doi: 10.1161/01.cir.97.18.1876. [DOI] [PubMed] [Google Scholar]
- 13.Hartge P, Brinton LA, Rosenthal JF, Cahill JI, Hoover RN, Waksberg J. Random digit dialing in selecting a population-based control group. Am J Epidemiol. 1984;120:825–33. doi: 10.1093/oxfordjournals.aje.a113955. [DOI] [PubMed] [Google Scholar]
- 14.Ismail J, Jafar TH, Jafary FH, White F, Faruqui AM, Chaturvedi N. Risk factors for non-fatal myocardial infarction in young South Asian adults. Heart. 2004;90:259–63. doi: 10.1136/hrt.2003.013631. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kanitz MG, Giovannucci SJ, Jones JS, Mott M. Myocardial infarction in young adults: Risk factors and clinical features. J Emerg Med. 1996;14:139–45. doi: 10.1016/0736-4679(95)02089-6. [DOI] [PubMed] [Google Scholar]
- 16.Kannel WB, Higgins M. Smoking and hypertension as predictors of cardiovascular risk in population studies. J Hypertens. 1990;8(Suppl 5):3–8. [PubMed] [Google Scholar]
- 17.Khader YS, Rice J, John L, Abueita O. Oral contraceptives use and the risk of myocardial infarction: A meta-analysis. Contraception. 2003;68:11–7. doi: 10.1016/s0010-7824(03)00073-8. [DOI] [PubMed] [Google Scholar]
- 18.Lopes C, Aro A, Azevedo A, Ramos E, Barros H. Intake and adipose tissue composition of fatty acids and risk of myocardial infarction in a male Portuguese community sample. J Am Diet Assoc. 2007;107:276–86. doi: 10.1016/j.jada.2006.11.008. [DOI] [PubMed] [Google Scholar]
- 19.Mähönen MS, McElduff P, Dobson AJ, Kuulasmaa KA, Evans AE. WHO MONICA Project. Current smoking and the risk of non-fatal myocardial infarction in the WHO MONICA Project populations. Tob Control. 2004;13:244–50. doi: 10.1136/tc.2003.003269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Matetzky S, Tani S, Kangavari S, Dimayuga P, Yano J, Xu H, et al. Smoking increases tissue factor expression in atherosclerotic plaques: Implications for plaque thrombogenicity. Circulation. 2000;102:602–4. doi: 10.1161/01.cir.102.6.602. [DOI] [PubMed] [Google Scholar]
- 21.Mcgill HC., Jr Potential mechanisms for the augmentation of atherosclerosis and atherosclerotic disease by cigarette smoking. Prev Med. 1979;8:390–403. doi: 10.1016/0091-7435(79)90016-1. [DOI] [PubMed] [Google Scholar]
- 22.Morillas PJ, Cabades A, Bertomeu V, Echanove I, Colomina F, Cebrian J, et al. Acute myocardial infarction in patients under 45 years. Rev Esp Cardiol. 2002;55:1124–31. doi: 10.1016/s0300-8932(02)76774-2. [DOI] [PubMed] [Google Scholar]
- 23.Negri E, La Vecchia C, Nobili A, D′Avanzo B, Bechi S. Cigarette smoking and acute myocardial infarction.A case-control study from the GISSI-2 trial. Eur J Epidemiol. 1994;10:361–6. doi: 10.1007/BF01719657. [DOI] [PubMed] [Google Scholar]
- 24.Nuttens MC, Romon M, Ruidavets JB, Arveiler D, Ducimetiere P, Lecerf JM, et al. Relationship between smoking and diet: The MONICA-France project. J Intern Med. 1992;231:349–56. doi: 10.1111/j.1365-2796.1992.tb00943.x. [DOI] [PubMed] [Google Scholar]
- 25.Nyboe J, Jensen G, Appleyard M, Schnohr P. Smoking and the risk of first acute myocardial infarction. Am Heart J. 1991;122:438–47. doi: 10.1016/0002-8703(91)90997-v. [DOI] [PubMed] [Google Scholar]
- 26.Pais P, Pogue J, Gerstein H, Zachariah E, Savitha D, Jayprakash S, et al. Risk factors for acute myocardial infarction in Indians: A case-control study. Lancet. 1996;348:358–63. doi: 10.1016/s0140-6736(96)02507-x. [DOI] [PubMed] [Google Scholar]
- 27.Panagiotakos DB, Chrysohoou C, Pitsavos C, Papaioannou I, Skoumas J, Stefanadis C, et al. The association between secondhand smoke and the risk of developing acute coronary syndromes, among non-smokers, under the presence of several cardiovascular risk factors: The CARDIO2000 case-control study. BMC Public Health. 2002;2:9–14. doi: 10.1186/1471-2458-2-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Panagiotakos DB, Rallidis LS, Pitsavos C, Stefanadis C, Kremastinos D. Cigarette smoking and myocardial infarction in young men and women: A case-control study. Int J Cardiol. 2006;116:371–5. doi: 10.1016/j.ijcard.2006.04.051. [DOI] [PubMed] [Google Scholar]
- 29.Parish S, Collins R, Peto R, Youngman L, Barton J, Jayne K, et al. Cigarette smoking, tar yields, and non-fatal myocardial infarction: 14,000 cases and 32,000 controls in the United Kingdom. The International Studies of Infarct Survival (ISIS) Collaborators. BMJ. 1995;311:471–7. doi: 10.1136/bmj.311.7003.471. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Patrick DL, Cheadle A, Thompson DC, Diehr P, Koepsell T, Kinne S. The validity of self-reported smoking: a review and meta-analysis. Am J Public Health. 1994;84:1086–93. doi: 10.2105/ajph.84.7.1086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pitsavos C, Panagiotakos DB, Chrysohoou C, Skoumas J, Tzioumis K, Stefanadis C. Association between exposure to environmental tobacco smoke and the development of acute coronary syndromes: The CARDIO2000 case-control study. Tob Control. 2002;11:220–5. doi: 10.1136/tc.11.3.220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Prescott E, Hippe M, Schnohr P, Hein HO, Vestbo J. Smoking and risk of myocardial infarction in women and men: Longitudinal population study. BMJ. 1998;316:1043–7. doi: 10.1136/bmj.316.7137.1043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ramos E, Lopes C, Barros H. Investigating the effect of nonparticipation using a population-based case-control study on myocardial infarction. Ann Epidemiol. 2004;14:437–41. doi: 10.1016/j.annepidem.2003.09.013. [DOI] [PubMed] [Google Scholar]
- 34.Ranjith N, Verho NK, Verho M, Winkelmann BR. Acute myocardial infarction in a young South African Indian-based population: Patient characteristics on admission and gender-specific risk factor prevalence. Curr Med Res Opin. 2002;18:242–8. doi: 10.1185/030079902125000624. [DOI] [PubMed] [Google Scholar]
- 35.Santos AC, Barros H. Smoking patterns in a community sample of Portuguese adults, 1999-2000. Prev Med. 2004;38:114–9. doi: 10.1016/j.ypmed.2003.09.040. [DOI] [PubMed] [Google Scholar]
- 36.Von Eyben FE, Von Eyben R. Smoking and other major coronary risk factors and acute myocardial infarction before 41 years of age. Scand Cardiovasc J. 2001;35:25–9. doi: 10.1080/140174301750101429. [DOI] [PubMed] [Google Scholar]
- 37.Von Eyben FE, Bech J, Madsen JK, Efsen F. High prevalence of smoking in young patients with acute myocardial infarction. J R Soc Health. 1996;116:153–6. doi: 10.1177/146642409611600305. [DOI] [PubMed] [Google Scholar]
- 38.Vriz O, Nesbitt S, Krause L, Majahalme S, Lu H, Julius S. Smoking is associated with higher cardiovascular risk in young women than in men: The Tecumseh Blood Pressure Study. J Hypertens. 1997;15:127–34. doi: 10.1097/00004872-199715020-00002. [DOI] [PubMed] [Google Scholar]
- 39.Williams MJ, Restieaux NJ, Low CJ. Myocardial infarction in young people with normal coronary arteries. Heart. 1998;79:191–4. doi: 10.1136/hrt.79.2.191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.WHO Tobacco or Health Programme. Geneva, Switzerland: WHO; 1997. World Health Organization. Guidelines for Controlling and Monitoring the Tobacco Epidemic. [Google Scholar]
- 41.Zimmerman FH, Cameron A, Fisher LD, Ng G. Myocardial infarction in young adults: Angiographic characterization, risk factors and prognosis (Coronary Artery Surgery Study Registry) J Am Coll Cardiol. 1995;26:654–61. doi: 10.1016/0735-1097(95)00254-2. [DOI] [PubMed] [Google Scholar]


