Abstract
Purpose
We aimed to verify the current status of transurethral resection of the prostate (TURP) in Korea.
Materials and Methods
The medical records of 1,341 men who underwent TURP in 9 Korean medical centers between 2004 and 2008 were reviewed. The patients were divided into two groups according to time periods: 2004-2005 (group 1) and 2006-2008 (group 2). To verify differences in the two patient groups, age, prostate volume, indications for TURP, preoperative International Prostate Symptom Score (IPSS), and resected tissue weight were evaluated.
Results
The mean age of the patients was 71.2 years and the mean IPSS was 22.7. The patients' characteristics were not significantly different between the two groups. The annual cases of TURP increased over the study period. The proportion of lower urinary tract symptoms (LUTS) as an indication for TURP increased up to 58.3% in group 2 compared with 51.6% in group 1 (p=0.019). However, the proportion of patients who presented with acute urinary retention decreased from 35.5% to 30.3% with marginal statistical significance (p=0.051). Other indications such as hematuria, bladder stone, recurrent urinary tract infection, and hydronephrosis were not significantly different between the groups. The mean resected weights of the prostate were similar (17.5 g in group 1 and 18.3 g in group 2, respectively; p>0.05).
Conclusions
TURP has been steadily performed in patients with benign prostatic hyperplasia and it is expected to remain constant. LUTS was the most common indication for TURP in recent years.
Keywords: Prostatic hyperplasia, Transurethral resection of prostate
INTRODUCTION
For many decades, transurethral resection of the prostate (TURP) has been considered the gold standard surgical treatment for lower urinary tract symptoms (LUTS), acute urinary retention (AUR), recurrent infection, hematuria, and azotemia resulting from benign prostatic hyperplasia (BPH) [1]. Despite the efficacy and safety of pharmacotherapy, the surgical management of BPH is still recommended in certain conditions, including the presence of refractory urinary retention, bladder stone, persistent gross hematuria, recurrent urinary tract infection, or renal insufficiency secondary to BPH [2].
Although TURP remains an effective treatment, 15% to 20% of patients develop significant complications, and 10% to 15% require a second intervention within 10 years [3]. To improve safety outcomes, a number of minimally invasive surgical techniques have been developed for the treatment of LUTS related to BPH, such as needle ablation, electrovaporization, vaporization resection, holmium laser, ultrasound, and microwave therapy [4]. Moreover, the introduction of medical therapy has brought about significant changes in the management of patients with moderate to severe LUTS [5]. In the era of medical therapy, TURP seems to be performed less frequently in patients with symptomatic BPH. The objective of this study was to assess the current status of TURP for BPH in Korea.
MATERIALS AND METHODS
The medical records of 1,341 men who underwent TURP in 9 medical centers between 2004 and 2008 were reviewed. Patients were eligible for inclusion only if their primary reason for TURP was BPH. Patients undergoing open prostatectomy were not included in this surgical analysis. Patients were excluded if they underwent TURP for carcinoma of the prostate or if their postoperative pathology was not compatible with a BPH diagnosis. The patients were divided into two groups according to the time periods in which they underwent TURP: 2004-2005 (group 1) and 2006-2008 (group 2). To verify the differences in the two patient groups, the parameters of age, prostate volume, indications for TURP, preoperative International Prostate Symptom Score (IPSS), and resected tissue weight were evaluated. The symptom severity of the patients was divided into two categories by IPSS as mild to moderate (IPSS <20) and severe (IPSS≥20). Preoperative prostatic volume was measured by transrectal ultrasound. The weight of the resected chips was documented from the pathology report.
Statistical analysis was performed by using the Student's t-test and chi-square test for categorical variables and a linear regression analysis for continuous variables. Results were considered significant at p<0.05.
RESULTS
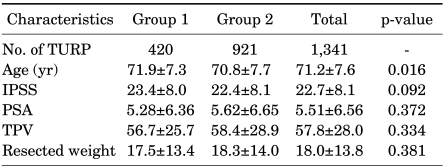
A total of 1,341 patients were identified with an average age of 71.2 years (range, 41-94 years). The average IPSS was 22.7. The baseline characteristics of the patients including IPSS, prostate volume, and serum prostate-specific antigen (PSA) were similar between the groups. The mean age of group 1 was 71.9 years, which was older than that of group 2 (Table 1).
TABLE 1.
Characteristics of the patients who underwent TURP
Data presented with standard deviation. IPSS: International Prostate Symptom Score, PSA: prostate-specific antigen, TPV: total prostate volume, TURP: transurethral resection of prostate
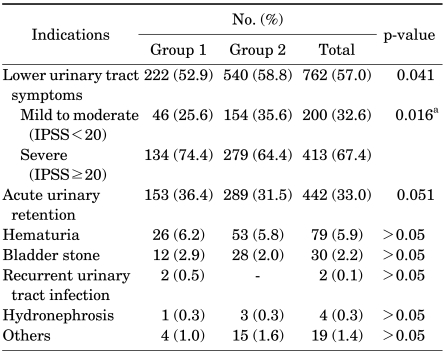
The annual cases of TURP increased over the study period (Fig. 1). The proportion of LUTS as an indication for TURP increased up to 58.3% in group 2 compared with 51.6% in group 1 (p=0.041). Also, the proportion of patients who underwent TURP for severe LUTS significantly decreased from 74.4% in group 1 to 64.4% in group 2, respectively (p=0.016). However, the proportion of patients who presented with AUR decreased from 35.5% to 30.3% with marginal statistical significance (p=0.051). The number of patients who suffered from hematuria, bladder stone, recurrent urinary tract infection, and hydronephrosis before their TURP was not significantly different between the time periods (Table 2).
FIG. 1.
Annual cases of transurethral resection of prostate in 9 medical centers Linear regression showed No.=40.8 x year-b. (p=0.026, R-square=0.85).
TABLE 2.
Indications for TURP in the time periods analyzed
TURP: transurethral resection of prostate, IPSS: International Prostate Symptom Score, a: chi-square statistical analysis between the mild to moderate symptom group and the severe symptom group
The average weight of the resected prostate was 18.0 g (range, 1.5-90 g). Over the study period, similar mean weights of the prostate were resected (17.5 g in group 1 and 18.3 g in group 2; p>0.05).
DISCUSSION
Two decades ago, we did not frequently offer medical therapy to patients with symptomatic LUTS associated with BPH, but rather recommended TURP as the primary mode of treatment. Over the course of the past two decades, medical therapy has become the standard first-line therapy for symptomatic LUTS associated with BPH. The increasing use of other minimally invasive treatment modalities, such as ablation, evaporation, and enucleation technique with laser, has led to a decline in TURP [6,7]. An American study reported a 43% decrease in cases of TURP between 1987 and 1994 [6], and this decline has also been observed in Europe [8]. Enthusiastic reports on the success of alternative treatment options represented by 'minimally invasive treatment' in the urological press seemed to herald the end of TURP as the gold standard, perhaps best reflected by Stamey's quote that 'TURP is now a therapy of history' [6]. In our study, however, contrary to other reports, the annul number of TURP procedures for BPH increased during the mid 2000s, despite other treatment modalities for BPH. One possible explanation for this increasing annual number of TURP procedures during the mid 2000s is the high prevalence of BPH in aged men and the continuously growing number of elderly men with BPH who needed surgical treatment. The other explanation is that the urologists participating in this study, to whom minimally invasive modalities were not available, performed TURP enthusiastically. Considering these facts, the overall proportion of TURP might be decreasing.
The proportion of TURP owing to BPH-related symptomatic LUTS in the current study increased over the time period. Several series of studies have demonstrated that medical treatment for patients with symptomatic BPH with an α-adrenergic antagonist and 5-α reductase inhibitors could lower the risk of AUR and recurrent gross hematuria [8-10]. It was our hypothesis that a trial of medical therapy that ended in failure may increase this proportion. In several previous studies, similar observations were reported. In 1990, 2% of patients undergoing TURP had previously been on prostatic medical therapy, and this proportion was increased up to 17% in 2000 [11]. In 57.0% of our patients, TURP was performed because of significant LUTS, which was the most common indication. Borboroglu et al reported that 80.9% of patients had significant LUTS preoperatively [12]. However, a controversial result was reported that TURP was performed in only 29.5% of patients with symptoms of prostatism [3]. These differences might be due to many factors, including public awareness about the disease, accessibility to medical care, widespread use of pharmacological agents as alternative therapy, and the health care system of each country. Although the exact number of patients taking pharmacological agents before TURP was not evaluated in our study, the majority might receive some form of medication for BPH before TURP.
There was a trend for the proportion of patients undergoing TURP because of AUR to decrease over the time period in the current study. We can attribute this observation to reduced needs for surgery by a voiding trial without catheter and medical treatment. However, in England, over a 10-year study between 1990 and 2000, the proportion of patients who underwent TURP for urinary retention increased from 33% to 58%, which has become the most common indication of TURP, whereas LUTS as an indication of TURP decreased from 65% to 42% [11]. Preoperatively, 33.0% of patients presented with AUR, which is still a somewhat higher rate than those reported in previous studies (15.2% to 27.1%) [3,12]. McConnell et al and Roehrborn et al demonstrated a lower rate of AUR in patients given medical therapy (α-adrenergic antagonist and/or 5-α reductase inhibitors) than in those given placebo [8,13,14]. This could be another explanation for the tendency for the proportion of patients who underwent TURP for AUR to decrease in our study.
The low incidence of recurrent gross hematuria as an indication for TURP (5.9%) compared to the study of Mebust et al (12.0%) in the era of no acceptable medical therapy for BPH could be due to the widespread use of medical therapy [3]. Finasteride has been shown to be effective for the treatment of BPH-related recurrent gross hematuria in more than 90% of treated patients [12,15].
The incidence of obstructive uropathy, as evidenced by the presence of hydronephrosis, was only 0.3% in our study. BPH-related renal insufficiency as an indication for TURP was under 1% in most studies [12,15]. This low incidence of obstructive uropathy could result from early access to medical care nowadays.
Because of the increasing use of pharmacological therapy in the management of BPH-related LUTS, TURP would be deferred. Also, delay in surgical therapy results in the progression of BPH.
Patients treated by TURP show an increase in not only prostate volume but also resected prostate volume, which may be because the surgery was delayed by treatment with α-1 blockers or 5-α reductase inhibitors [16].
As a result, it is supposed that larger glands would be resected in the era of medical therapy for BPH. The average weight of the resected prostate tissue in this study was 18.0 g, which was comparable to that in other reports (18.8-37 g) [3,12,17,18]. However, the resected prostate volume was not significantly different between the groups in the present study.
The mean age of the patients in group 1 was older than in group 2. This means that we consider TURP as a preemptive treatment in the era of medical therapy for BPH.
Meanwhile, among patients with LUTS (IPSS≥20) as an indication for TURP, severe LUTS decreased from 74.4% in group 1 to 64.4% in group 2. This might be explained by the operators' active trial or patients' increased request for TURP during this period.
This multicenter study of 5-years' experience with TURP is obviously limited by the retrospective nature and the short time period in which changes in the indication for TURP were evaluated. Moreover, because the 9 institutions involved in this study do not represent Korean urological society, the incidence of TURP may not be generalizable. Also, the effect of the minimally invasive procedures and medical therapy for BPH was not considered in this study. Because the prevalence of BPH is increasing in the Korean population, the proportion of TURP among the treatment options for BPH might have decreased relatively. However, we could see a temporal treatment status of TURP.
CONCLUSIONS
In the mid-2000s, TURP was steadily performed in patients with BPH and it is expected to remain constant. The proportion of TURP as a treatment for symptomatic BPH-related LUTS has increased. These changes seemed to coincide with the increasing use of medical therapy as a first-line treatment for LUTS associated with BPH. TURP is still considered as an effective surgical intervention for BPH and as such is expected to be constantly performed even in the era of medical therapy and minimally invasive therapy for BPH.
Footnotes
The authors have nothing to disclose.
References
- 1.Fitzpatrick JM. Minimally invasive and endoscopic management of benign prostatic hyperplasia. In: Wein AJ, Kavoussi LR, Novick AC, Partin AW, Peters CA, editors. Campbell-Walsh urology. 9th ed. Phliladelphia: Saunders; 2007. pp. 2803–2844. [Google Scholar]
- 2.AUA Practice Guideline Committee. AUA guideline on management of benign prostatic hyperplasia (2003). Chapter 1: Diagnosis and treatment recommendations. J Urol. 2003;170:530–547. doi: 10.1097/01.ju.0000078083.38675.79. [DOI] [PubMed] [Google Scholar]
- 3.Mebust WK, Holtgrewe HL, Cockett AT, Peters PC. Transurethral prostatectomy: immediate and postoperative complication. A cooperative study of 13 participating institutions evaluating 3,885 patients. J Urol. 1989;141:243–247. doi: 10.1016/s0022-5347(17)40731-2. [DOI] [PubMed] [Google Scholar]
- 4.Son H, Song SH, Paick JS. Current laser treatments for benign prostatic hyperplasia. Korean J Urol. 2010;51:737–744. doi: 10.4111/kju.2010.51.11.737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.O'Leary MP. Treatment and pharmacologic management of BPH in the context of common comorbidities. Am J Manag Care. 2006;12(5 Suppl):S129–S140. [PubMed] [Google Scholar]
- 6.Madersbacher S, Marberger M. Is transurethral resection of the prostate still justified? BJU Int. 1999;83:227–237. doi: 10.1046/j.1464-410x.1999.00908.x. [DOI] [PubMed] [Google Scholar]
- 7.Blomqvist P, Ekbom A, Carlsson P, Ahlstrand C, Johansson JE. Benign prostatic hyperplasia in Sweden 1987 to 1994: changing patterns of treatment, changing patterns of costs. Urology. 1997;50:214–219. doi: 10.1016/S0090-4295(97)00241-0. [DOI] [PubMed] [Google Scholar]
- 8.McConnell JD, Brukewitz R, Walsh P, Andriole G, Lieber M, Holtgrewe HL, et al. Finasteride Long-Term Efficacy and Safety Study Group. The effect of finasteride on the risk of acute urinary retention and the need for surgical treatment among men with benign prostatic hyperplasia. N Engl J Med. 1998;338:557–563. doi: 10.1056/NEJM199802263380901. [DOI] [PubMed] [Google Scholar]
- 9.Jardin A, Bensadoun H, Delauche-Cavallier MC, Attali P The BPH-ALF Group. Alfuzosin for treatment of benign prostatic hypertrophy. Lancet. 1991;337:1457–1461. doi: 10.1016/0140-6736(91)93140-5. [DOI] [PubMed] [Google Scholar]
- 10.Miller MI, Puchner PJ. Effects of finasteride on hematuria associated with benign prostatic hyperplasia: long-term follow-up. Urology. 1998;51:237–240. doi: 10.1016/s0090-4295(97)00614-6. [DOI] [PubMed] [Google Scholar]
- 11.Wilson JR, Urwin GH, Stower MJ. The changing practice of transurethral prostatectomy: a comparison of cases performed in 1990 and 2000. Ann R Coll Surg Engl. 2004;86:428–431. doi: 10.1308/147870804731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Borboroglu PG, Kane CJ, Ward JF, Roberts JL, Sands JP. Immediate and postoperative complications of transurethral prostatectomy in the 1990s. J Urol. 1999;162:1307–1310. [PubMed] [Google Scholar]
- 13.Roehrborn CG, Siami P, Barkin J, Damião R, Major-Walker K, Nandy I, et al. The effects of combination therapy with dutasteride and tamsulosin on clinical outcomes in men with symptomatic benign prostatic hyperplasia: 4-year results from the CombAT study. Eur Urol. 2010;57:123–131. doi: 10.1016/j.eururo.2009.09.035. [DOI] [PubMed] [Google Scholar]
- 14.McConnell JD, Roehrborn CG, Bautista OM, Andriole GL, Jr, Dixon CM, Kusek JW, et al. The long-term effect of doxazosin, finasteride, and combination therapy on the clinical progression of benign prostatic hyperplasia. N Engl J Med. 2003;349:2387–2398. doi: 10.1056/NEJMoa030656. [DOI] [PubMed] [Google Scholar]
- 15.Sieber PR, Rommel FM, Huffnagle HW, Breslin JA, Agusta VE, Harpster LE. The treatment of gross hematuria secondary to prostatic bleeding with finasteride. J Urol. 1998;159:1232–1233. [PubMed] [Google Scholar]
- 16.Shin YS, Park JK. Changes in surgical strategy for patients with benign prostatic hyperplasia: 12-year single-center experience. Korean J Urol. 2011;52:189–193. doi: 10.4111/kju.2011.52.3.189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Horninger W, Unterlechner H, Strasser H, Bartsch G. Transurethral prostatectomy: mortality and morbidity. Prostate. 1996;28:195–200. doi: 10.1002/(SICI)1097-0045(199603)28:3<195::AID-PROS6>3.0.CO;2-E. [DOI] [PubMed] [Google Scholar]
- 18.Estey EP, Mador DR, McPhee MS. A review of 1486 transurethral resections of the prostate in a teaching hospital. Can J Surg. 1993;36:37–40. [PubMed] [Google Scholar]