Abstract
Using behavioral self-regulation processes may facilitate exercise among older women with heart disease. Data from women in a heart disease-management program (n = 658, mean 73 years), was used to explore associations among exercise self-regulation components (i.e., choosing to improve exercise and observing, judging, and reacting to one’s behavior) and exercise capacity. General linear models showed that choosing exercise predicted higher exercise self-regulation scores postprogram and 8 months later. In turn, these scores predicted greater improvements in exercise capacity concurrently and 8 months later. Interaction analyses revealed that the effect of self-regulation on exercise capacity was stronger among women who chose to work on exercise.
Keywords: physical activity, heart disease, self-management, self-regulation, women
INTRODUCTION
Physical Activity, Heart Disease, and Older Women
Engaging in regular physical activity is essential for the optimal long-term management of most cardiovascular disease (CVD) (Smith et al., 2006; Thompson, 2003). Exercise training among CVD patients confers a number of benefits, from reducing the incidence of subsequent cardiac events and cardiac-related mortality, to enhancing quality of life via symptom reduction and improved physical functioning (Giannuzzi et al., 2008; Hung et al., 2004; Taylor et al., 2004; Thompson, 2005). Increasing physical activity levels is thus often the primary goal in cardiac rehabilitation programs and also forms a key component of “lifestyle” or self-management programs that target patients with cardiovascular disease (Haskell et al., 1994; Toobert, Glasgow, Nettekoven, & Brown, 1998).
Although women with heart disease may have even more to gain from exercise than men due to their initially lower exercise capacity (Moore, Ruland, Pashkow, & Blackburn, 1998), several factors place female heart patients at particular risk for inactivity. First, women tend to experience cardiac events at older ages than men, and also have a greater number of comorbid conditions (Loose & Fernhall, 1995; Mosca et al., 1997). They are more bothered by heart-related symptoms (Wiklund et al., 1993) and have worse physical functioning (Ades, Maloney, Savage, & Carhart, 1999; Clark, Janz, Dodge, & Garrity, 1994). All of these factors may present barriers to regular exercise (Yates, Price-Fowlkes, & Agrawal, 2003). Second, women are less likely to attend cardiac rehabilitation programs than men (Davidson et al., 2003; Mosca et al., 1997) and even when they do, exercise less than their male coparticipants (Schairer, Keteyian, Ehrman, Brawner, & Berkebile, 2003) and have difficulty maintaining increased activity levels once the program ends (Marcuccio, Loving, Bennett, & Hayes, 2003; Moore et al., 1998). Third, many older women have experienced traditional gender norms that discourage them from exercise, and are unaccustomed to engaging in physical activity in their leisure time (Schutzer & Graves, 2004; Singh, 2000). Moreover, some older women perceive serious medical risk even from common exercises recommended for older adults (O’Brien Cousins, 2000); this effect is likely to be heightened among women with preexisting cardiac conditions. Despite the fact that more than a quarter of women over age 65 have been diagnosed with heart disease (Federal Interagency Forum on Aging-Related Statistics, 2004), relatively few studies have been published on theory-based interventions to promote physical activity within this population.
Self-Regulation and Physical Activity
For many individuals, the challenges of initiating and maintaining a physically active lifestyle are such that mere knowledge of exercise’s benefits or even confidence that one can exercise on a regular basis (i.e., self-efficacy) are not sufficient; the ability to engage in behavioral self-regulation may be needed (Scholz, Knoll, Sniehotta, & Schwarzer, 2006; Schutzer & Graves, 2004). A model of self-regulation for chronic disease control, as developed by Clark, Gong, and Kaciroti (2001), may be a useful framework for informing interventions to help older women with heart disease or other chronic conditions learn a process for enhancing physical activity-related behavior.
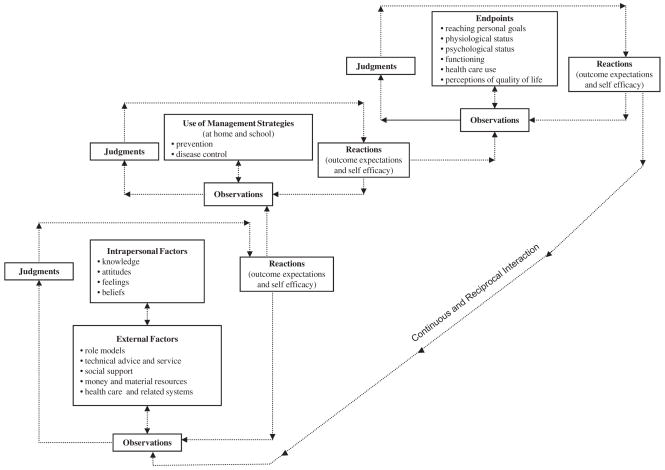
As shown in Figure 1, this model, which incorporates principles from social cognitive theory (Bandura, 1986), depicts the reciprocal cognitive and behavioral processes that individuals with a chronic illness use to achieve health-related goals. In brief, individuals select a personally important illness-management-related goal, such as increasing physical activity. To reach this goal, they observe their current behavior, make judgments based on these observations, and then experience cognitive reactions to their attempts at behavioral change, which in turn influence subsequent behavior. Two of these reactions are particularly important: self-efficacy, or an individual’s level of confidence that s/he can continue a behavior; and outcome expectations, or beliefs about likely effects of the behavior. Intrapersonal factors, such as knowledge and attitudes, both give rise to and are influenced by these self-regulatory processes. External factors, such as material resources and social support, also exert influence.
FIGURE 1.
The continuous and reciprocal nature of self-regulation processes in disease prevention and management (Clark et al., 2001).
The extent to which older women with heart disease are able to learn and apply self-regulation processes to increase exercise has not been fully explored. An earlier study by the authors explored how two framework elements—self-efficacy and outcomes expectations—predicted self-management behaviors related to diet, exercise, and stress among older women with heart disease (Clark & Dodge, 1999). In the case of exercise, it was found that baseline self-efficacy significantly predicted Six-Minute Walk Test (6MWT) distance 4 months later, whereas baseline outcome expectations predicted distance at both 4 and 12 months from baseline. Another small body of work reports on the use of a similar self-regulation model to design and assess exercise-focused interventions for patients with heart disease (predominantly men in late midlife: Scholz et al., 2006; Sniehotta et al., 2005). Other chronic disease-management programs that include older women have used social-cognitive elements like those described in the current framework—e.g., efficacy building, goal-setting—to improve self-management behaviors, including exercise (Allison & Keller, 2004; Brodie & Inoue, 2005; Marks, Allegrante, & Lorig, 2005; Schreurs, Colland, Kuijer, de Ridder, & van Elderen, 2003).
Although the above work suggests the value of behavioral self-regulation for increasing exercise among older women with chronic disease, no previous studies on this topic were identified that included both a large sample of women with cardiovascular disease and detailed measures of self-regulatory processes. In addition, no study was found that specifically examined how choosing a specific area on which to focus one’s self-regulatory efforts might affect the adoption and effect of these efforts. For example, the framework described above posits that use of the processes will be most effective when they are applied to a personally salient disease-management goal. Allowing patients to choose their health-behavior goals has been part of both disease-management programs and is also a central part of popular behavior-change techniques such as motivational interviewing (Emmons & Rollnick, 2001). However, the independent effect of making such a choice on related behavioral outcomes has not been assessed.
To help fill these gaps, the current study uses data from a longitudinal evaluation of an intervention for older women with heart disease. This intervention, entitled “Women Take PRIDE” (WTP), teaches the principles of self-regulation as described above. The goal of the current study is to assess the interrelationships among (a) consciously making a choice to improve one’s exercise behavior, (b) the use of exercise self-regulation processes, and (c) improvements in exercise capacity over time among the older women participating in this program. Specifically, it is hypothesized that:
Women who selected exercise as their self-management “problem area” to work on during the intervention will engage in exercise self-regulation behaviors more frequently and have more positive reactions (i.e., exercise self-efficacy and outcome expectations) over time than other women.
More frequent use of exercise self-regulation behaviors and more positive reactions immediately postprogram will be associated with greater improvements in exercise capacity over time.
The association between exercise self-regulation and improvements in exercise capacity will be strongest among those women who identified exercise as their problem area to work on during the program—that is, among those who made a conscious choice to improve their exercise behavior.
METHOD
Participant Recruitment and Study Sample
Participants were community-dwelling women 60 years of age or older who were being treated by daily heart medication for a cardiovascular condition (i.e., arrhythmia, angina, myocardial infarction, congestive heart failure, or valvular disease). Lists of potential participants were generated from patient rosters at cardiovascular clinics or physician offices in three urban areas in southeastern Michigan. Potential participants’ physicians excluded a small number of women who would not be able to fully benefit from the program due to other medical reasons (e.g., terminal illness or memory loss). Informed consent was provided by all participants. Prior publications provide details on the design (Janevic et al., 2003) and the health outcomes (Clark et al., 2008; Clark et al., 2009) of this study. Briefly, an innovative study design was used in which prospective participants were randomized, before any contact, into either (a) an randomized controlled trial (RCT) arm, where they were randomized into a Group program, Self-Directed program, or control condition; or (b) a “choice” arm, where they could choose their program format. Group participants attended six sessions at a hospital site. Self-Directed participants completed six units at home after an initial visit to a hospital site, and received weekly telephone calls from a health educator or peer leader.
The analyses presented here use data from all women who participated in the WTP program, regardless of program format (Group vs. Self-Directed) or study arm (Random vs. Choice), because all participants received similar instruction in use of self-regulation principles to achieve their disease-management goals. Control group women were excluded, as this study was not intended to assess the effect of the intervention; rather, study hypotheses concern intervention processes. In particular, we wished to explore the associations among framework variables within the context of a program guiding women in the use of self-regulation to meet their disease-management goals.
Intervention Content
Per the self-regulation framework, participants were encouraged to first select a disease-management problem area in which to set behavioral goals, and to use self-regulation to reach these goals. The acronym “PRIDE” in the program’s title refers to this process: Problem selecting; Researching one’s daily routine; Identifying a behavioral goal; Developing a plan to reach one’s goal; and Evaluating one’s progress. Although participants were free to set personal self-management goals of any nature, physical activity was used as a model behavior throughout the program. Women who chose other areas to work on (e.g., stress management) adapted the self-regulation examples to suit their own area of focus. Additionally, the benefits of exercise and ways to become more physically active were emphasized throughout the program curriculum. Thus, although WTP differs from cardiac rehabilitation interventions that focus primarily on exercise, it is similar to other programs that include exercise as one of various topics relevant to successful chronic disease self-management (e.g., Lorig, Ritter, & Plant, 2005).
Data Collection and Measures
Data were collected via telephone interviews at baseline; and at 4, 12, and 18 months from baseline. The authors developed the following measures to represent the variables in the self-regulation framework.
Selection of disease-management goal
At the Month 4 interview, which took place following the WTP program, participants were asked, “As a result of your participation in Women Take PRIDE, did you decide to work on a problem or to make any changes related to your heart condition?” Respondents who answered yes were asked an open-ended question about what problem or changes they worked on (up to two responses were recorded), which were subsequently coded. Participants who reported selecting exercise only or exercise along with another goal (e.g., diet) were coded “1”; all others were coded “0.”
Observation
Participants were asked to rate (1–5: “none of the time” to “all of the time”) how often they keep track of the amount of physical activity they do.
Judgment
Judgment is represented by the mean frequency (1 = “none of the time” and 5 = “all of the time”) of two related behaviors, goal-setting and evaluation of physical activity. To assess goal setting, participants were asked how often they set goals or make decisions to maintain or improve their levels of physical activity. Evaluation behavior was determined by asking “How often do you evaluate or think about whether you have followed through on your decision to maintain or improve your physical activity?” The bivariate correlation (Pearson’s r) between these two variables at baseline was .78.
Reaction
Reaction is made up of two constructs: (a) outcome expectations and (b) self-efficacy. To assess outcome expectations, participants were asked “Overall, if you try to maintain or improve your current level of physical activity, how much good do you think it will do you?” (1 = “not much good” and 5 = “a lot of good”). Self-efficacy was assessed by asking “On as scale of 1 to 10 where 1 = ‘not at all confident’ and 10 = ‘very confident,’ what number describes how confident you are that over the next month you can improve your physical activity?” (Scale transformed to 1–5 before analysis.)
Exercise self-regulation index
An index indicating overall level of exercise self-regulation was computed by summing the self-regulation variables described above (observation, judgment, and reaction). The index range is 5–25, with higher scores indicating better self-regulation for exercise. The baseline coefficient alpha for this scale was .78.
The exercise-related outcome was the Six-Minute Walk Test (6MWT) (Guyatt et al., 1985). This measure is an objective indicator of functional exercise capacity that is sensitive to increases in regular physical activity. It is frequently used with heart disease patients, including as an outcome in intervention studies (e.g., Brodie & Inoue, 2005; Verrill, Barton, Beasley, Lippard, & King, 2003) and is highly correlated with “gold standard” measures of functional status (Hamilton & Haennel, 2000). This measure indicates distance walked (at one’s own pace and with stops as needed) over 6 min. WTP participants visited a hospital site where this test was conducted by a research nurse.
Finally, the following variables were used as covariates in multivariate analysis: age (measured continuously), race (White = 1; otherwise = 0), education (coded 1 = 8th grade or less, 2 = some high school; 3 = high school, 4 = some college, 5 = college graduate, 6 = graduate school; treated as continuous variable), and number of comorbidities (a continuous variable derived from the following open-ended question at baseline, “Has a doctor told you that you have any other important health problems or conditions?”).
Analysis Plan
First, descriptive statistics were calculated in order to provide a profile of the study sample at baseline. Next, general linear models were used to test the first study hypothesis; i.e., a positive association between having selected exercise as one’s problem area during the program and levels of exercise self-regulation variables at Months 4, 12, and 18. Exercise self-regulation at a given timepoint was modeled on an indicator of whether or not participants selected exercise as their problem area, along with control variables indicating age, race, education, comorbidities, and baseline self-regulation index score. Models were fitted first with the overall self-regulation index as an outcome, followed by separate models predicting each of the four individual components of self-regulation that are included in the index (i.e., observation, judgment, self-efficacy, and outcome expectations).
General linear models were also used to address the second study hypothesis; i.e., to test whether change from baseline in 6MWT distance at Months 4, 12, and 18 was predicted by Month 4 exercise self-regulation level (that is, immediately postprogram), controlling for age, race, comorbidities, and baseline 6MWT distance. Again, models were constructed first using the self-regulation index as the predictor of interest, followed by separate models for each of the index components.
The third study hypothesis posited an interactive effect of selecting exercise as one’s problem area with level of self-regulation (as measured at Month 4) on 6MWT distance at Months 4, 12, and 18. Thus, an interaction term (selecting exercise as problem area X exercise self-regulation index) was added to the model predicting change from baseline in 6MWT distance at the various timepoints to determine its significance, controlling for age, race, comorbidities, and baseline 6MWT distance.
RESULTS
The analytic sample consisted of participants who had data at baseline and at least one follow-up point (N = 658). Descriptive statistics for selected study variables can be found in Table 1. The average age of the sample was 73 (SD = 6) years, and the majority of the participants were White (86%) with at least a high school education (84%). The most common cardiac diagnoses were hypertension (71%), arrythmias (56%), and MI (38%) (not shown in Table 1). Most women (58%) had one or two other chronic health conditions in addition to heart disease (not shown in Table 1).
TABLE 1.
Baseline Descriptive Statistics for the WTP Study Sample (N = 658)*
| N | Mean (SD) or % | Observed range | |
|---|---|---|---|
| Control Variables | |||
| Age | 657 | 73 (6) | [60 – 88] |
| Race (% White, N) | 654 | 86% (562) | |
| Education | |||
| Less than high school | 103 | 16% | |
| High school | 261 | 40% | |
| Some college or more | 294 | 45% | |
| Number of Comorbidities | 658 | 1.3 (1.2) | [0 – 6] |
| Exercise Self-Regulation Variables | |||
| Observation frequency* * | 657 | 2.0 (1.4) | [1 – 5] |
| Judgment frequency* * | 657 | 2.7 (1.2) | [1 – 5] |
| Reaction Level | |||
| Outcome expectations for exercise | 655 | 3.9 (1.2) | [1 – 5] |
| Self-efficacy for exercise | 651 | 6.6 (2.7) | [1 – 10] |
| Exercise Capacity | |||
| 6MWT(meters) | 560 | 232 (140) | [4 – 555] |
Participants in WTP intervention who had data from at least one follow-up point.
Scale: 1 = none of time to 5 = all of the time.
In terms of exercise self-regulation at baseline, Table 1 shows that the mean frequency of exercise observation behavior was 2.0 (SD = 1.4) on a 1–5 scale (equivalent to engaging in this behavior “a little of the time”); the mean frequency of judgment was 2.7 (SD = 1.2) (between “a little of the time” and “some of the time”). Mean exercise self-efficacy was 6.6 (SD = 2.7) on a 1–10 scale and outcome expectations 3.9 (SD = 1.2) on a 1–5 scale. Average 6MWT distance at baseline was 232 meters (SD = 140). Within the study sample, 42% of participants (N = 279) reported at the Month 4 interview that they selected “exercise” or “physical activity” as a problem area to work on during the program. This was the most popular area to work on, followed by diet at 30% (not shown in Table 1).
Hypothesis One
Table 2 shows that at Month 4, the adjusted mean exercise self-regulation index score among women who chose exercise as their focal problem area to work on during the program was significantly higher than among women who did not select this area (M = 17.2 vs. 15.5; p = .001). Selecting exercise also had a significant effect on each individual component of self-regulation; in other words, women who selected exercise as a problem area engaged more frequently in observation and judgment, and had more positive reactions (self-efficacy and outcome expectations) compared to other participants (all p < .01). By Month 12, a significant effect of selecting exercise remained on the mean exercise self-regulation index score (M = 15.8 among women who selected exercise versus 15.2 among others; p = .002) and on outcome expectations for exercise (4.06 vs. 3.77; p = .002). At Month 18, a significant effect remained on outcome expectations only (3.96 vs. 3.75; p = .026).
TABLE 2.
Effect of Selecting Exercise as Focal Problem Area During WTP Intervention* on Exercise Self-Regulation at Months 4, 12, and 18: Adjusted Means* *
| Outcome variables | Did not Select exercise | Selected exercise | p-Value |
|---|---|---|---|
| Exercise self-regulation index | |||
| Month 4 | 15.5 (.20) | 17.2 (.23) | .001 |
| Month 12 | 15.2 (.20) | 15.8 (.23) | .044 |
| Month 18 | 15.4 (.21) | 15.8 (.24) | .144 |
| Observation | |||
| Month 4 | 2.44 (.06) | 2.78 (.08) | .002 |
| Month 12 | 2.31 (.07) | 2.32 (.08) | .966 |
| Month 18 | 2.22 (.07) | 2.30 (.08) | .443 |
| Judgment | |||
| Month 4 | 2.88 (.05) | 3.23 (.06) | .001 |
| Month 12 | 2.81 (.06) | 2.90 (.06) | .242 |
| Month 18 | 2.94 (.06) | 3.03 (.07) | .392 |
| Reaction | |||
| a) Exercise outcome expectations | |||
| Month 4 | 3.80 (.05) | 4.15 (.06) | .001 |
| Month 12 | 3.77 (.06) | 4.06 (.07) | .002 |
| Month 18 | 3.75 (.06) | 3.96 (.07) | .026 |
| b) Exercise self efficacy | |||
| Month 4 | 6.65 (.12) | 7.20 (.14) | .004 |
| Month 12 | 6.63 (.13) | 6.79 (.15) | .400 |
| Month 18 | 6.57 (.13) | 6.59 (.15) | .941 |
As reported by participants in the postprogram interview, 4 months from baseline.
Adjusted for baseline value of self-regulation index, age, race, comorbidities, and education.
Boldface type indicates statistical significance at p < .05.
Hypothesis Two
Regarding the hypothesized association between the use of exercise self-regulation during the program period with increase in exercise capacity (i.e., 6MWT score), Table 3 shows that at Month 4, self-regulation index scores significantly predicted change from baseline in 6MWT distance in meters (β = 2.1; p = .015). Of the individual components of self-regulation, only the effect of judgment on 6MWT distance at this time point reached statistical significance at p < .05. significance (β = 8.7; p = .009). At Month 12, the Month 4 self-regulation index score continued to be a significant predictor of improvement from baseline in distance walked (β = 2.1; p = .051). By Month 18, exercise self-efficacy as measured at Month 4 was the sole significant predictor of an improved 6MWT score (β = 4.9; p = .013).
TABLE 3.
Effect of Postprogram (Month 4) Self-Regulation on Change From Baseline in Distance Walked (in Meters) in 6-Min Walk Test at Months 4, 12, and 18*
| Time | Self-Regulation index | Observation | Judgment | Outcome expectations | Self-Efficacy |
|---|---|---|---|---|---|
| Unstandardized regression coefficients (standard error) [p-value] | |||||
| Month 4 | 2.1 (0.9) [.015] | 5.0 (2.6) [.058] | 8.7 (3.3) [.009] | .23 (3.4) [.944] | 2.9 (1.6) [.063] |
| Month 12 | 2.1 (1.1) [.051] | 3.2 (3.1) [.230] | 7.1 (4.0) [.079] | 4.0 (4.0) [.324] | 3.2 (1.9) [.094] |
| Month 18 | 2.1 (1.1) [.059] | 3.7 (3.3) [.262] | 7.0 (4.4) [.109] | 1.2 (4.1) [.779] | 4.9 (2.0) [.013] |
Adjusted for age, race, comorbidities, education, and baseline value of outcome.
Boldface type indicates statistical
Hypothesis Three
Table 4 shows the results of the final analysis, which explored the interactive effect of selecting exercise as one’s focal problem area during the WTP intervention with overall exercise self-regulation score (as measured at Month 4) on change in 6MWT score. This interaction term was significant (p = .02; not shown) in the model that examined change in 6MWT score from baseline to 12 months as an outcome, and nonsignificant when outcomes were change in 6-min walk score from baseline to Months 4 and 18. Next, to further explore the nature of the interaction, possible exercise self-regulation index scores were categorized into tertiles (low, 5–12; medium, 13–18; and high, 19–25). The relationship of each tertile with 6MWT improvement was examined within two groups at each timepoint: women who selected exercise as a problem area and those who did not. Among women who fell into the highest tertile of exercise self-regulation, there was a statistically significant difference in 6MWT improvement at Month 12 between participants who chose exercise as a problem area and those who did not. Specifically, the mean change in 6MWT distance from baseline was an increase of 32 meters for women who selected exercise and had high levels of exercise self regulation; whereas women with high self-regulation who did not choose to work on exercise experienced a mean decrease of 1.6 meters. At Months 4 and 18, a similar pattern was evident; i.e., women who chose to work on exercise during the program and had high exercise self-regulation scores had a greater improvement in 6MWT score compared to women with equally high self-regulation who had not chosen to work on exercise during the program (24 vs. 19 meters at Month 4; 15.1 vs. 6.3 at Month 18). However, the between-group differences at these timepoints did not reach significance.
TABLE 4.
Effect of Selecting Exercise as Focus During Intervention on Change in 6-Min Walk Distance, by Level of Postprogram Self-Regulation
| Predictor: Selected exercise as focal problem area | Change from baseline in 6MWT distance in meters M (SE)
|
p-Value (Between- Group) | p-Value for linear trend in subgroup that selected exercise | ||
|---|---|---|---|---|---|
| Selected exercise | Did not select exercise | ||||
| Exercise self-regulation index tertile at Month 4 (M4SR) | |||||
| Month 4 | Low M4SR | −8.3m (11.8) | 7.2m (8.1) | .27 | |
| Medium M4SR | −5.4m (9.3) | −6.5m (9.4) | .93 | ||
| High M4SR | 23.8m (8.4) | 18.9m (9.1) | .69 | .013 | |
| Month 12 | Low M4SR | −27.3m (14.0) | 0.5m (9.7) | .1 | |
| Medium M4SR | 4.0m (11.0) | −15.8m (10.9 | .2 | ||
| High M4SR | 32.4m (10.3) | −1.6m (10.4) | .02 | .001 | |
| Month 18 | Low M4SR | −14.6m (14.4) | −3.1m (10.5) | .52 | |
| Medium M4SR | −0.1m (10.9) | −18.1m (11.5) | .26 | ||
| High M4SR | 15.1m (10.8) | 6.3m (11.5) | .57 | .11 | |
Subgroup sizes based on self-regulation index tertile at Month 4 are as follows: Low (N = 236; selected exercise = 74; did not select = 162); Medium (N = 196; selected exercise = 87; did not select = 109); High (N = 226; selected exercise = 116; did not select = 110).
Boldface type indicates statistical significance at p < .05.
Table 4 also shows that in the subgroup of women who chose to work on exercise, the relationship between exercise self-regulation tertile and improvement in 6MWT distance followed a positive, linear trend. The slope for this relationship was 59.8 (p = .013) at Month 4; 95.3 (p = .001) at Month 12, and 48.4 (p = .11) at Month 18. Among women who did not select exercise as a problem area, no linear relationship between self-regulation and change in 6MWT distance was observed.
DISCUSSION
Some support was found for the hypothesized associations among variables related to exercise self-regulation and improvements in exercise capacity in this sample of older women with heart disease. First, women who singled out exercise to work on during the WTP self-management intervention had higher overall levels of exercise self-regulation both immediately following the intervention and at Month 12, although not at Month 18. Second, higher exercise self-regulation index scores postprogram (Month 4) predicted greater improvements in exercise capacity at the same timepoint and also at Month 12, but not at Month 18. Finally, it was expected that higher Month 4 exercise self-regulation scores would have the strongest influence on exercise capacity among women who had made a choice to improve their exercise behavior; this interactive effect was strongest at Month 12 and nonsignificant at other points. However, at all three follow-up points, a positive, linear relationship between self-regulation level and improvement in exercise capacity was evident only among the subgroup of women who had chosen to work on exercise. Each of these findings is discussed in greater detail below.
The fact that participants who selected exercise as their focal problem area had higher scores across all exercise self-regulation variables immediately following the program demonstrated that older women can be successfully taught to apply the processes of self-regulation toward a desired disease-management goal. Moreover, women who focused on exercise during the program continued to be more likely to self-regulate this behavior even 8 months after its end compared to participants who did not focus on exercise. This result provides some validation for the utility of the “PRIDE” process as an intervention strategy, which asks participants to first select the problem area they most want to work on and then to focus self-regulatory efforts on specific goals within that domain. In a younger, predominantly male sample of heart disease patients, Sniehotta and colleagues (2005) also found that participants in an intervention promoting physical activity successfully practiced elements of self-regulation (e.g., planning and self-monitoring). The current study shows that even in the context of an intervention not solely focused on exercise, and despite the formidable exercise-related barriers faced by older, chronically ill women, those for whom increasing exercise is important will use self-regulatory cognitions and behaviors in an attempt to reach their goals.
When examining how choosing exercise affected individual components of exercise self-regulation, it was found that at Month 4, women who had identified exercise as their focus were not only more likely to engage in observation and judgment of exercise behavior, but also had more favorable reactions (exercise self-efficacy and outcome expectations). This may be due in part to the reciprocal nature of these processes, as posited by the framework, as well as to elements of the program that attempted to build efficacy and to highlight the value of exercise. As time went on, women who chose to work on exercise during the program did not continue to engage in observation and judgment of exercise behavior to a greater extent than other participants. It is possible that the lack of active program support caused participants to reduce the use of these strategies, or that women perceived them as less essential to reaching their behavioral goals. Similarly, the effect of choosing exercise during the program on exercise self-efficacy at Months 12 and 18 also became nonsignificant. Choosing exercise during the program period, was, however, associated with a sustained positive effect on outcome expectations for exercise. Prior research among older women suggests that outcome expectations may be especially important when it comes to maintaining exercise routines over time (Wilcox, Castro, & King, 2006).
In the test of the second hypothesis, it was found that higher scores on the self-regulation index immediately postprogram were associated with significantly greater (although clinically small) improvements from baseline in exercise capacity at this point and also at Month 12. This finding adds to prior intervention work in CVD populations, in which variables related to self-regulation or social cognitive theory were also significantly associated with exercise behavior (Allison & Keller, 2004; Brodie & Inoue, 2005; Sniehotta et al., 2005). Using the self-regulation processes during the WTP program may have helped to bring about an increase in physical activity during the intervention and beyond that was reflected in this outcome measure. Further analysis revealed that the frequency of “judgment” (i.e., goal-setting and evaluating) was most important in explaining improved exercise capacity immediately postprogram. Although the precise reason for this relationship is unknown, the concrete action represented by goal-setting may have been particularly powerful in bringing about behavioral change.
The biggest impact of self-regulation on exercise capacity was seen among women who had chosen exercise as their focal problem area during the program. For example, among participants in the highest tertile of the self-regulation index, the difference in 6MWT improvement at Month 12 between women who had chosen to work on exercise and those who did not was 34 m. This difference falls squarely between the “small” (20 m) and “substantial” (50 m) benchmarks for meaningful clinical change on this measure (Perera, Mody, Woodman, & Studenski, 2006). A linear trend in improvements in exercise capacity by self-regulation tertile was significant at Months 4 and 12 and near-significant at Month 18, but only among women who had chosen to work on exercise. In other words, women who not only selected to work on exercise during the program but also put into practice the self-regulation skills they were taught continued to improve on their baseline exercise capacity long after program’s end.
Thus, applying a specific set of behavior-change skills to a disease-management area of personal importance seemed to be effective in this sample in bringing about behavior change. This is in accordance with the principles in the self-regulation framework as described earlier, in which self-regulation is an intentional act, and consciously choosing a disease-management area to focus one’s energies on is part of the intention. It is not known why some participants and not others chose to work on exercise; but the fact that this choice turned out to work in tandem with self-regulation to bring about increases in exercise capacity suggests the value of future research on the factors associated with prioritizing exercise as a heart disease-management goal among older women.
It is also not known which aspect of choosing exercise was influential—whether it was participants’ formal designation of their chosen problem area, or simply the fact that exercise was important to them. In general, evidence for a positive effect of making formal commitments to health behavior change in the form of health contracts is not strong (Bosch-Capblanch, Abba, Prictor, & Garner, 2007). Nonetheless, there may be value in exploring the effects of varying levels of formality in behavioral change commitments as part of a disease-management intervention.
Results from the current study demonstrate that using self-regulation processes may be a way for older women with heart disease to increase their exercise capacity, once they have made an initial decision to improve their physical activity habits. These skills can be taught in the context of a relatively brief intervention. The WTP program, or comparable programs, can be provided at modest cost in terms of time, money, and expertise (Wheeler, Janz, & Dodge, 2003). This study also has some notable limitations. We did not have a reliable means of tracking actual physical activity behavior over time. Such a measure may have revealed a different relationship with exercise self-regulation; however, the 6MWT is a valid, reliable, and objective measure that is suitable for an older, chronically ill, sample. Also, our sample was self-selected and thus not representative of all older women with a cardiac diagnosis, but may well be typical of those who would participate in such an intervention in the future. Future replications of similar programs should attempt to broaden the racial/ethnic diversity of participants, as our sample was overwhelmingly White. Minority women are not only less likely to be active than White women, but also perceive unique barriers to engaging in physical activity (Heesch, Brown, & Blanton, 2000).
As the number of older women with heart disease increases, coming up with effective strategies to assist them in increasing their physical activity will be important to minimizing morbidity and mortality in this group. Because of the many barriers to increasing physical activity faced by this group of older women, developing cost-effective interventions that enable participants to not only initiate, but also to maintain exercise routines over the long term, remains an important priority.
Contributor Information
MARY R. JANEVIC, Center for Managing Chronic Disease, University of Michigan, Ann Arbor, MI
NANCY K. JANZ, Center for Managing Chronic Disease, University of Michigan, Ann Arbor, MI
NIKO KACIROTI, Center for Managing Chronic Disease, University of Michigan, Ann Arbor, MI.
JULIA A. DODGE, Center for Managing Chronic Disease, University of Michigan, Ann Arbor, MI
STEVEN J. KETEYIAN, William Clay Ford Center for Athletic Medicine, Henry Ford Health Systems–Division of Cardiology, Detroit, MI
LORI MOSCA, Preventive Cardiology, NewYork–Presbyterian Hospital/Columbia University Medical Center, New York, NY.
NOREEN M. CLARK, Center for Managing Chronic Disease, University of Michigan, Ann Arbor, MI
References
- Ades PA, Maloney A, Savage P, Carhart RLJ. Determinants of physical functioning in coronary patients: Response to cardiac rehabilitation. Archives of Internal Medicine. 1999;159:2357–2360. doi: 10.1001/archinte.159.19.2357. [DOI] [PubMed] [Google Scholar]
- Allison MJ, Keller C. Self-efficacy intervention effect on physical activity in older adults. Western Journal of Nursing Research. 2004;26:31–46. doi: 10.1177/0193945903259350. [DOI] [PubMed] [Google Scholar]
- Bandura A. Social learning theory. Englewood Cliffs, NJ: Prentice-Hall; 1986. [Google Scholar]
- Bosch-Capblanch X, Abba K, Prictor M, Garner P. Contracts between patients and healthcare practitioners for improving patients’ adherence to treatment, prevention, and health promotion activities. Cochrane Database of Systematic Reviews. 2007;2:CD004808. doi: 10.1002/14651858.CD004808.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brodie DA, Inoue A. Motivational interviewing to promote physical activity for people with chronic heart failure. Journal of Advanced Nursing. 2005;50:518–527. doi: 10.1111/j.1365-2648.2005.03422.x. [DOI] [PubMed] [Google Scholar]
- Clark NM, Dodge JA. Exploring self-efficacy as a predictor of disease management. Health Education & Behavior. 1999;26:72–89. doi: 10.1177/109019819902600107. [DOI] [PubMed] [Google Scholar]
- Clark NM, Gong M, Kaciroti N. A model of self-regulation for control of chronic disease. Health Education & Behavior. 2001;28:769–782. doi: 10.1177/109019810102800608. [DOI] [PubMed] [Google Scholar]
- Clark NM, Janz NK, Dodge JA, Garrity CR. Managing heart disease: A study of the experiences of older women. Journal of the American Medical Women’s Association. 1994;49:202–206. [PubMed] [Google Scholar]
- Clark NM, Janz NK, Dodge JA, Lin X, Trabert BL, Kaciroti N, et al. Heart disease management by women: Does intervention format matter? Health Education & Behavior. 2009;36:394–409. doi: 10.1177/1090198107309458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Clark NM, Janz NK, Dodge JA, Mosca L, Lin X, Long Q. The effect of patient choice of intervention on health outcomes. Contemporary Clinical Trials. 2008;29:679–686. doi: 10.1016/j.cct.2008.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Davidson PM, Daly J, Hancock K, Moser D, Chang E, Cockburn J. Perceptions and experiences of heart disease: A literature review and identifica-tion of a research agenda in older women. European Journal of Cardiovascular Nursing. 2003;2:255–264. doi: 10.1016/S1474-5151(03)00056-2. [DOI] [PubMed] [Google Scholar]
- Emmons KM, Rollnick S. Motivational interviewing in health care settings: Opportunities and limitations. American Journal of Preventative Medicine. 2001;20:255–264. doi: 10.1016/s0749-3797(00)00254-3. [DOI] [PubMed] [Google Scholar]
- Federal Interagency Forum on Aging-Related Statistics. Older Americans 2004: Key Indicators of Well-Being. Washington, D.C: Author; 2004. [Google Scholar]
- Giannuzzi P, Temporelli PL, Marchioli R, Maggioni AP, Balestroni G, Ceci V. Global secondary prevention strategies to limit event recurrence after myocardial infarction: Results of the GOSPEL study, a multicenter, randomized controlled trial from the Italian cardiac rehabilitation network. Archives of Internal Medicine. 2008;168:2194–2204. doi: 10.1001/archinte.168.20.2194. [DOI] [PubMed] [Google Scholar]
- Guyatt GH, Sullivan MJ, Thompson PJ, Fallen EL, Pugsley SO, Taylor DW. The 6-minute walk: A new measure of exercise capacity in patients with chronic heart failure. Canadian Medical Association Journal. 1985;132:919–923. [PMC free article] [PubMed] [Google Scholar]
- Hamilton DM, Haennel RG. Validity and reliability of the 6-minute walk test in a cardiac rehabilitation population. Journal of Cardiopulmonary Rehabilitation. 2000;20:156–164. doi: 10.1097/00008483-200005000-00003. [DOI] [PubMed] [Google Scholar]
- Haskell WL, Alderman EL, Fair JM, Maron DJ, Mackey SF, Superko HR. Effects of intensive multiple risk factor reduction on coronary atherosclerosis and clinical cardiac events in men and women with coronary artery disease: The Stanford coronary risk intervention project. Circulation. 1994;89:975–990. doi: 10.1161/01.cir.89.3.975. [DOI] [PubMed] [Google Scholar]
- Heesch KC, Brown DR, Blanton CJ. Perceived barriers to exercise and stage of exercise adoption in older women of different racial/ethnic groups. Women & Health. 2000;30(4):61–76. doi: 10.1300/J013v30n04_05. [DOI] [PubMed] [Google Scholar]
- Hung C, Daub B, Black B, Welsh R, Quinney A, Haykowsky M. Exercise training improves overall physical fitness and quality of life in older women with coronary artery disease. Chest. 2004;126:1026–1031. doi: 10.1378/chest.126.4.1026. [DOI] [PubMed] [Google Scholar]
- Janevic MR, Janz NK, Dodge JA, Lin X, Pan W, Sinco BR, et al. The role of choice in health education intervention trials: A review and case study. Social Science & Medicine. 2003;56:1581–1594. doi: 10.1016/s0277-9536(02)00158-2. [DOI] [PubMed] [Google Scholar]
- Loose MS, Fernhall B. Differences in quality of life among male and female cardiac rehabilitation participants. Journal of Cardiopulmonary Rehabilitation. 1995;15:225–231. doi: 10.1097/00008483-199505000-00009. [DOI] [PubMed] [Google Scholar]
- Lorig K, Ritter PL, Plant K. A disease-specific self-help program compared with a generalized chronic disease self-help program for arthritis patients. Arthritis & Rheumatism. 2005;53:950–957. doi: 10.1002/art.21604. [DOI] [PubMed] [Google Scholar]
- Marcuccio E, Loving N, Bennett SK, Hayes SN. A survey of attitudes and experiences of women with heart disease. Women’s Health Issues. 2003;13:23–31. doi: 10.1016/s1049-3867(02)00193-7. [DOI] [PubMed] [Google Scholar]
- Marks R, Allegrante JP, Lorig K. A review and synthesis of research evidence for self-efficacy-enhancing interventions for reducing chronic disability: Implications for health education practice (part II) Health Promotion Practice. 2005;6:148–156. doi: 10.1177/1524839904266792. [DOI] [PubMed] [Google Scholar]
- Moore SM, Ruland CM, Pashkow FJ, Blackburn CG. Women’s patterns of exercise following cardiac rehabilitation. Nursing Research. 1998;47:318–324. doi: 10.1097/00006199-199811000-00005. [DOI] [PubMed] [Google Scholar]
- Mosca SM, Manson JE, Sutherland SE, Langer RD, Manolio T, Barrett-Connor E. Cardiovascular disease in women: A statement for healthcare professionals from the American Heart Association. Circulation. 1997;96:2468–2482. doi: 10.1161/01.cir.96.7.2468. [DOI] [PubMed] [Google Scholar]
- O’Brien Cousins SJ. “My heart couldn’t take it”: Older women’s beliefs about exercise benefits and risks. Journal of Gerontology Series B: Psychological Sciences and Social Sciences. 2000;55:283–294. doi: 10.1093/geronb/55.5.p283. [DOI] [PubMed] [Google Scholar]
- Perera S, Mody SH, Woodman RC, Studenski SA. Meaningful change and responsiveness in common physical performance measures in older adults. Journal of the American Geriatrics Society. 2006;54:743–749. doi: 10.1111/j.1532-5415.2006.00701.x. [DOI] [PubMed] [Google Scholar]
- Schairer JR, Keteyian SJ, Ehrman JK, Brawner CA, Berkebile ND. Leisure time physical activity of patients in maintenance cardiac rehabilitation. Journal of Cardiopulmonary Rehabilitation. 2003;23:260–265. doi: 10.1097/00008483-200307000-00002. [DOI] [PubMed] [Google Scholar]
- Scholz U, Knoll N, Sniehotta FF, Schwarzer R. Physical activity and depressive symptoms in cardiac rehabilitation: Long-term effects of a self-management intervention. Social Science & Medicine. 2006;62:3109–3120. doi: 10.1016/j.socscimed.2005.11.035. [DOI] [PubMed] [Google Scholar]
- Schreurs KM, Colland VT, Kuijer RG, de Ridder DT, van Elderen T. Development, content, and process evaluation of a short self-management intervention in patients with chronic diseases requiring self-care behaviors. Patient Education and Counseling. 2003;51:133–141. doi: 10.1016/s0738-3991(02)00197-0. [DOI] [PubMed] [Google Scholar]
- Schutzer KA, Graves BS. Barriers and motivations to exercise in older adults. Preventative Medicine. 2004;39:1056–1061. doi: 10.1016/j.ypmed.2004.04.003. [DOI] [PubMed] [Google Scholar]
- Singh MAF. Exercise and aging. In: Fiatarone Singh MA, editor. Exercise, nutrition, and the older woman: Wellness for women over fifty. Boca Raton, FL: CRC Press; 2000. pp. 3–36. [Google Scholar]
- Smith SCJ, Allen J, Blair SN, Bonow RO, Brass LM, Fonarow GC. AHA/ACC guidelines for secondary prevention for patients with coronary and other atherosclerotic vascular disease: 2006 update. Circulation. 2006;113:2363–2372. doi: 10.1161/CIRCULATIONAHA.106.174516. [DOI] [PubMed] [Google Scholar]
- Sniehotta FF, Scholz U, Schwarzer R, Fuhrmann B, Kiwus U, Voller H. Long-term effects of two psychological interventions on physical exercise and self-regulation following coronary rehabilitation. International Journal of Behavioral Medicine. 2005;12:244–255. doi: 10.1207/s15327558ijbm1204_5. [DOI] [PubMed] [Google Scholar]
- Taylor RS, Brown A, Ebrahim S, Jolliffe J, Noorani H, Rees K. Exercise-based rehabilitation for patients with coronary heart disease: Systematic review and meta-analysis of randomized controlled trials. The American Journal of Medicine. 2004;116:682–692. doi: 10.1016/j.amjmed.2004.01.009. [DOI] [PubMed] [Google Scholar]
- Thompson PD. Exercise and physical activity in the prevention and treatment of atherosclerotic cardiovascular disease. Atherosclerosis, Thrombosis, and Vascular Biology. 2003;23:1319–1321. doi: 10.1161/01.ATV.0000087143.33998.F2. [DOI] [PubMed] [Google Scholar]
- Thompson PD. Exercise prescription and proscription for patients with coronary artery disease. Circulation. 2005;112:2354–2363. doi: 10.1161/CIRCULATIONAHA.104.502591. [DOI] [PubMed] [Google Scholar]
- Toobert DJ, Glasgow RE, Nettekoven LA, Brown JE. Behavioral and psychosocial effects of intensive lifestyle management for women with coronary heart disease. Patient Education and Counseling. 1998;35:177–188. doi: 10.1016/s0738-3991(98)00074-3. [DOI] [PubMed] [Google Scholar]
- Verrill DE, Barton C, Beasley W, Lippard M, King CN. Six-minute walk performance and quality of life comparisons in North Carolina cardiac rehabilitation programs. Heart & Lung. 2003;32:41–45. doi: 10.1067/mhl.2003.7. [DOI] [PubMed] [Google Scholar]
- Wheeler JR, Janz NK, Dodge JA. Can a disease self-management program reduce health care costs? The case of older women with heart disease. Medical Care. 2003;41:706–715. doi: 10.1097/01.MLR.0000065128.72148.D7. [DOI] [PubMed] [Google Scholar]
- Wiklund I, Herlitz J, Johansson S, Bengtson A, Karlson BW, Persson NG. Subjective symptoms and well-being differ in women and men after myocardial infarction. European Heart Journal. 1993;14:1315–1319. doi: 10.1093/eurheartj/14.10.1315. [DOI] [PubMed] [Google Scholar]
- Wilcox S, Castro CM, King AC. Outcome expectations and physical activity participation in two samples of older women. Journal of Health Psychology. 2006;11:65–77. doi: 10.1177/1359105306058850. [DOI] [PubMed] [Google Scholar]
- Yates BC, Price-Fowlkes T, Agrawal S. Barriers and facilitators of self-reported physical activity in cardiac patients. Research in Nursing & Health. 2003;26:459–469. doi: 10.1002/nur.10108. [DOI] [PubMed] [Google Scholar]