Abstract
Background
Mechanical ventilation is one of the most frequently used technological treatments in critical care units and induces great anxiety in patients.
Objectives
While mechanical ventilation and critical illness induce great anxiety and distress in hospitalized patients, little is known about anxiety ratings over the course of ventilatory support. Knowledge of anxiety ratings over time is needed in order to implement effective symptom management interventions. The purposes of this paper were to describe anxiety ratings for a subgroup of mechanically ventilated patients over the duration of enrollment in a multi-site clinical trial, to discern any pattern of change in anxiety ratings, to determine if anxiety decreases over time, and to explore the influence of sedative exposure on anxiety ratings.
Methods
Participants were 57 mechanically ventilated patients who were randomly assigned to the usual care group of a randomized controlled trial designed to assess the efficacy of music interventions on anxiety of mechanically ventilated patients in ICUs. Anxiety ratings were obtained at study entry and daily for up to 30 days. A 100-mm Visual Analog Scale-Anxiety (VAS-A) was used to measure anxiety. VAS-A scores were plotted as a function of study time in days for each participant to discern possible patterns of change. A mixed models analysis was performed to assess the nature and magnitude of change over time (slope) using 251 observations on 57 patients.
Results
Results of the unconditional means model indicated further modeling was appropriate. An autoregressive covariance structure with a random component for participant (AR + RE) was chosen as the most appropriate covariance structure for modeling. An unconditional growth model indicated that VAS-A declined slowly over time, −.53 points per day (p = .09).
Discussion
Anxiety is an individual patient experience which requires on-going management with appropriate assessment and intervention over the duration of mechanical ventilatory support.
Keywords: mechanical ventilation, anxiety, intensive care units
Mechanical ventilation (MV) is a common ICU modality used to treat respiratory failure from a variety of causes. Each year in the United States, more than one million persons admitted to intensive care units (ICU) receive MV, usually for less than 48 hours (Cox, Carson, Govert, Chelluri, & Sanders, 2007). However, approximately 34% of these patients require prolonged ventilatory support (PVS), and the rate of PVS is increasing (Cox et al., 2007).
While intubation and mechanical ventilation are necessary to support respiratory function and life, these technologies create many distressful physiological and psychological experiences for patients (Li & Puntillo, 2006; Rotondi et al., 2002). To be mechanically ventilated is to be grossly uncomfortable at best (McCartney & Boland, 1994). Patients have referred to mechanical ventilation as the most inhumane treatment ever experienced (Gries & Fernsler, 1988) and admit to being miserable most of the time while intubated (Logan & Jenny, 1997). Patients who were mechanically ventilated for more than 48 hours recall the endotracheal tube itself, being unable to talk, being thirsty, feeling tense, not being in control, difficulty swallowing (Rotondi et al., 2002), and moderately intense anxiety (Chlan, 2004; Li & Puntillo, 2006) as being most distressing. Anxiety is a state marked by apprehension, agitation, increased motor tension or activity, autonomic arousal, and fearful withdrawal (McCartney & Boland, 1994). It is one of the most common symptoms reported by patients receiving mechanical ventilatory support (Li & Puntillo, 2006; Rotondi, et al., 2002). Anxiety develops in response to these distressful experiences associated with mechanical ventilation (McCartney & Boland, 1994). Thus, anxiety compounded by fear causes increased sympathetic nervous system stimulation, increased work of breathing, increased oxygen demand, and myocardial stimulation (Johnston & Sexton, 1990).
Nurses caring for critically ill patients believe that treating anxiety is important. The most frequently used therapy is the administration of anti-anxiety, sedative medications (Frazier et al., 2003). Critically ill patients receive a wide variety of intravenous sedative medications from disparate drug classes over the course of ventilatory support that can influence anxiety ratings (Weinert & Calvin, 2007). These medications are administered to patients to promote breathing synchrony with the mechanical ventilator, to reduce anxiety, and promote comfort. Adjunctive, non-pharmacologic interventions used to treat anxiety include empathic touch, control of environmental stressors, providing choices with respect to care to enhance the patient’s sense of control, music, and relaxation techniques (Frazier et al., 2003). While symptom management for ventilated ICU patients can be a great challenge, it is imperative that nurses implement evidence-based strategies. However, for ICU nurses to effectively manage patient anxiety, an awareness of the dynamic nature of this distressful symptom over the course of ventilatory support must first be known in order to intervene appropriately.
Information about the course of anxiety across the duration of mechanical ventilation in the ICU is limited. Previous investigations of interventions to reduce anxiety in response to mechanical ventilatory support have used pre-post intervention measurement of anxiety, (Chlan, 1998; Wong, Lopez-Nahas, & Molassiotis, 2001) or have reported cross-sectional snap-shots of anxiety ratings at one point during ventilatory support (Chlan, 2003). Our impression from practice is that ICU clinicians believe that anxiety may decrease over the course of ventilatory support as the patient adjusts to this invasive treatment modality. However, little data about the reported experience or intensity of anxiety over the course of mechanical ventilatory support in the ICU is available.
The purposes of this paper were to describe anxiety ratings over the duration of study enrollment in a sample of critically ill patients receiving mechanical ventilatory support; to identify any pattern of change in anxiety ratings; to determine if anxiety decreases over the course of ventilatory support; and to explore the influence of sedative exposure on anxiety ratings.
Method
Design, Setting, and Sample
Persons included in this sample are a subgroup of participants enrolled in a multi-site, ICU-based randomized trial testing music interventions for anxiety self-management in patients receiving mechanical ventilatory support. Participants for the multi-site trial were recruited from five medical centers (12 separate ICUs) located throughout the Minneapolis-St. Paul urban area. Patients receiving mechanical ventilatory support for a primary pulmonary problem (e.g., pneumonia, respiratory distress, respiratory failure) making their own daily care decisions, and who were alert and interacting appropriately with nursing staff at time of enrollment were invited to participate in the study. Participants remained enrolled in the study until extubation or up to 30 days, they choose to withdraw, or they died. The multi-site clinical trial was approved by the University of Minnesota’s Institutional Review Board (IRB) and by IRBs of the participating sites.
A descriptive design was used for the purpose of this paper. Participants included in this secondary analysis are those randomized to the usual care control condition. Usual care consists of the standing medical orders and standardized nursing care protocols for each respective ICU whereby registered nurses provide care in a 1:1 or 1:2 nurse to patient ratio.
Procedure
Each participating ICU was screened daily by a research nurse for potential study participants. Once a new participant was enrolled, the study protocol commenced and data collection began. Study entry data collection consisted of severity of illness determination, length of ICU stay (days), length of ventilatory support (days), ventilator settings, and all medications abstracted from the medical record.
Anxiety was measured with the Visual Analog Scale-Anxiety (VAS-A) at study entry and then once daily as close to the same time each day as possible over the duration of study participation for all enrolled participants. The research nurse supported participants in completion of the VAS-A as needed by assisting participants with marking their current level of anxiety on the VAS-A. Not all participants provided anxiety ratings each day enrolled in the study, including day of enrollment, due to being unable to complete the VAS-A because of fatigue, need to leave the ICU for a diagnostic procedure, altered mental status or level of alertness, or refusal to complete the assessment due to other non-specified reasons.
Given the influence of sedative and analgesic medications on anxiety ratings, all medications were abstracted from the medical record. For this study, dosing and frequency of dose administration over each 24-hour period were obtained for midazolam, lorazepam, fentanyl, morphine, dexmedetomidine, hydromorphone, propofol, and haloperidol.
All participants were visited each day by a research nurse who conducted the anxiety assessment via the VAS-A and reviewed the medical record for additional study data on ventilator settings and recorded all medications. Participants remained on protocol as long as they were receiving mechanical ventilatory support, up to 30 days. Participants contained in this sample were extubated at different time-points, which marked study completion. Thus, a varying number of anxiety assessments were included for each study participant.
Variables and Measurement
Anxiety
Anxiety is a state marked by apprehension, agitation, increased motor tension or activity, autonomic arousal, and fearful withdrawal (McCartney & Boland, 1994). Participants rated their current level of anxiety on the VAS-A on a 100-millimeter vertical line that was anchored on each end by statements ‘not anxious at all’ to ‘the most anxious I have ever been’. The VAS-A had a vertical orientation, thought to be more sensitive and easier for participants to use, particularly for those with a narrowed visual field or when under stress (Cline, Herman, Shaw, & Morton, 1992; Gift, 1989). A VAS with a vertical orientation, analogous to a thermometer, to perform repeated measurement of anxiety in mechanically ventilated patients was reported to be less burdensome for participants to complete than other instruments with a Likert-based response format (Chlan, 2003; Chlan, Savik, & Weinert, 2003). Scores were derived by measuring the distance in millimeters from the bottom edge of the line anchor to the mark placed by the participant (Knebel, Janson-Bjerklie, Malley, Wilson, & Marini, 1994; Lee & Kieckhefer, 1989).
Visual analog scales are appropriate for tracking a participant’s clinical course because they are easily administered and easy for participants to see. Few words are used which minimizes the possibility of different interpretations (Gift, 1989; Wewers & Loew, 1990). The VAS-A has been used by investigators to measure anxiety in patients receiving mechanical ventilation (Cline et al., 1992) and to measure changes in anxiety in ventilated patients undergoing weaning trials (Knebel et al., 1994). The VAS-A and the Spielberger State Anxiety Inventory (SAI) were moderately correlated in ventilated ICU patients (r = .49; Chlan, 2004) and in patients undergoing ambulatory surgical procedures (r = .82; Vogelsang, 1988). These results demonstrate concurrent validity of the VAS-A. Stability (i.e., test-retest reliability) is not relevant due to the expected dynamic nature of state anxiety (Lush, Janson-Bjerklie, Carrieri, & Lovejoy, 1988; Wewers & Loew, 1990). Of crucial importance is the reproducibility of ratings obtained from these scales (Wewers & Loew, 1990). The VAS-A is an accurate and sensitive measure of state anxiety, capable of reproducing reliable measures of anxiety in ventilated patients undergoing weaning trials (Knebel et al., 1994) and ambulatory surgical procedures (Vogelsang 1988).
Sedative Exposure
Critically ill patients receive a wide variety of intravenous sedative and analgesic medications from disparate drug classes over the course of ventilatory support that can influence anxiety ratings, referred to as sedative exposure (Weinert & Calvin, 2007). These medications are administered to patients to promote breathing synchrony with the mechanical ventilator, to reduce anxiety, and promote comfort. In order to summarize medications mechanically ventilated patients may receive from disparate drug classes, which are not amenable to dose-equivalent calculations, we use the following approach. A dose frequency count of all sedative and analgesic medications documented in the medical record each day of study participation was used to calculate an aggregate dose, which yielded a sedation intensity score (Weinert & Calvin, 2007).
Dose frequency
Data were abstracted from the medical record on all sedative and analgesic medications received during a 24 hour period. Dose frequency was determined by dividing the calendar day into six, four-hour time blocks (00:00, 04:00, 08:00, 12:00, 16:00, and 20:00 hrs) and, for each medication (midazolam, lorazepam, fentanyl, morphine, dexmedetomidine, hydromorphone, propofol, and haloperidol) the occurrence(s) in which a drug was administered at least once during that interval was summed. Frequency of medication doses was then summed for each participant over each of the six, four-hour time blocks daily to yield a dose frequency count.
Sedation intensity
Likewise, the sedation intensity score (SIS) was based on aggregate doses of medication(s) received over the same 24-hour period as described above. The SIS is a validated measure that addresses the problem of aggregating sedative exposure across disparate drug classes (Weinert & Calvin, 2007). The weight-adjusted dose was first calculated based on an individual participant’s kg of body weight for each medication administered during a 4-hour time block. The dose was then categorized as 1 – 4 based on the quartile within the distribution of that drug for one time block. For instance, if 0.1 mg/kg of lorazepam and 0.2 mg/kg of morphine were given during a 4-hour interval and 0.1 mg/kg fell into the second quartile of the distribution of all 4-hour lorazepam doses in the entire group and 0.2 mg/kg of morphine was in the third quartile, then the SIS for that time block was 2 (second quartile) + 3 (third quartile) = 5. A participant’s mean SIS score (quotient of sum of participant’s SIS values and number of 4-hour intervals on mechanical ventilation) represents the average sedative exposure per hour relative to all other participants.
Severity of Illness
Severity of illness of each participant was ascertained at study entry via the Acute Physiology, Chronic Health Evaluation (APACHE) III to establish comparability of illness severity among groups at baseline; data for APACHE III scores were abstracted from the medical record from the first day of ICU admission. Scoring details are described elsewhere (Knaus, et al., 1991).
Time
Time was measured in days. Day 0 was set as the day of study enrollment. However, the date of initiation of mechanical ventilation was variable for each participant. In many cases, the initiation of mechanical ventilatory support occurred a number of days prior to study enrollment. Thus, the number of study days on which anxiety measurements were obtained varied for each participant. Length of time on protocol and number of daily measurements was limited to 30 days as 30 days was the established limit for study protocol participation.
Analysis
Descriptive statistics for interval and ordinal data were presented as medians with ranges given the skewed distributions of the data. Categorical data were presented as frequencies. In an initial analysis, anxiety trajectories were graphed for each participant to discern pattern of change.
Mixed effects models were used for analysis as they accommodate correlated and non-homogeneous residuals, which would be expected in repeated measures. Mixed models are an ideal analysis for dealing with disparate assessment time points and/or missing data points from subjects being unable or unwilling to complete daily anxiety assessments due to medical status, mental status, or level of fatigue. A series of models were estimated to determine the best model of change for the VAS-A in this study. Model parameters are defined in Table 1, and the estimated models are listed in Table 2. In each model, Yij is the VAS-A score for person i on Day j.
Table 1.
Description and Interpretation of Parameters and Variance Components in Estimated Models
| Level 1 | Parameter or Variance Component | Interpretation |
|---|---|---|
| π0i | Person i’s modeled initial value for VAS-A when DAY = 0; intercept term | |
| π1i | Person i’s modeled daily rate of linear change (slope) for VAS-A If a quadratic term is included in the model for change, π1i is the instantaneous rate of change (slope) when DAY = 0 |
|
| π2i | Person i’s curvature parameter (acceleration) that determines the changing rate of change in VAS-A instantaneously over time | |
| εij | Random error for person i on occasion j | |
| σ2ε | Variance of individual errors of prediction εij, used to summarize the deviation above and below the modeled trajectory for the observed measurements of VAS-A for person i in the population across occasions j | |
| 2 | γ00 | Population average for individual intercepts π0i In conditional models for sedation intensity (SIS) and frequency (SFS), γ00 is the intercept value when SIS and SFS are 0 |
| γ01 | In conditional models incorporating SIS and SFS as time-varying covariates, γ01 is the difference in individual intercepts π0i for each unit change in SIS and SFS | |
| γ10 | Population average for individual change parameters π1i as defined above In conditional models for SED1 and SED2, the population average for π1i when SIS and SFS have values of 0 |
|
| γ11 | In conditional models, the change in population average change in VAS-A due to unit change in SIS and SFS | |
| γ20 | Population average for individual curvature parameters π2i as defined above with sedation level = 0 | |
| γ21 | Population average for individual curvature parameters π2i as defined above with sedation level increase of 1 | |
| ζ0i | Person i’s deviation from population average intercept; level 2 error for intercept | |
| ζ1i | Person i’s deviation from population average slope; level 2 error for linear coefficient | |
| ζ2i | Person i’s deviation from population average quadratic curvature parameter; level 2 error for quadratic coefficient | |
| τ00 | Residual variance for π0i; the variance of ζ0i | |
| τ11 | Residual variance for π1i; the variance of ζ1i | |
| τ22 | Residual variance for π2i; the variance of ζ2i |
Table 2.
Models Used in the Analysis
| Description | Level 1 | Level 2 | Composite |
|---|---|---|---|
| Unconditional means | Yij = π0i + εij | π0i = γ00 + ζ0i | Yij = γ00 + (εij + ζ0i) |
| Unconditional change linear | Yij = π0i + π1i DAYij + εij | π0i = γ00 + ζ0i π1i = γ10 + ζ1i |
Yij = γ00 + γ10DAYij + (εij + ζ0i + ζ1i DAYij) |
| Unconditional change linear and quadratic | Yij = π0i + π1i DAYij + π2i DAY2ij + εij | π0i = γ00 + ζ0i π1i = γ10 + ζ1i π2i = γ20 + ζ2i |
Yij = γ00 + γ10 DAYij + γ20 DAY2ij + (εij + ζ0i + ζ1i DAYij + ζ2i DAY2ij) |
| Conditional change linear with SIS | Yij = π0i + π1i DAYij + εij | π0i = γ00 + γ01SISij + ζ0i π1i = γ10 + γ11SISij + ζ1i |
Yij = γ00 + γ01 SISij + γ10 DAYij + γ11 (SISij × DAYij) + (εij + ζ0i + ζ1i DAYij) |
| Conditional change linear with SFS | Yij = π0i + π1i DAYij + εij | π0i = γ00 + γ01SFSij + ζ0i π1i = γ10 + γ11SFSij + ζ1i |
Yij = γ00 + γ01 SFSij + γ10 DAYij + γ11 (SFSij × DAYij) + (εij + ζ0i + ζ1i DAYij) |
Note. Y = VAS-A. SIS = sedation intensity score. SFS = sedation frequency score. Model parameters are defined in Table 1.
The unconditional means model was estimated to determine if further modeling was appropriate. Each outcome Yij is a linear combination of the grand mean (γ00) plus the individual deviations from the grand mean (ζ0i) and a random error term (εij). The unconditional means model assesses two null hypotheses: (a) no change across occasions, and (b) no variation between subjects. Rejecting these null hypotheses warrants doing further analysis.
An unconditional growth model with DAY added as a predictor incorporated estimation of change coefficients. Models with several within-person error covariance structures that were compatible with the correlation pattern between VAS-A scores at different time points were explored. Correlations seemed to decrease as the lag time increased, which is indicative of an autoregressive structure. Three covariance structures were considered. The unstructured covariance model presupposes heterogeneous variance in VAS-A scores over time and thus no pattern in the covariance structure. This model is useful as it is usually the model that fits the data best and can serve as a baseline for evaluating other structures. The downside of this model is that it requires the estimation of the most parameters and thus reduces power. The autoregressive (AR) structure appeared to best fit the correlation pattern but does imply that correlation between measures on the same individual ultimately approach zero. The AR + random effects (RE) model specifies that covariance between observations comes from two sources, the AR structure and the fact that the measures come from the same subject. The AR + RE structure does not assume the correlations will approach zero.
An unconditional growth model with a quadratic term was also explored to assess if there were discernable non-linear changes in VAS-A scores over time. The (AR + RE) error covariance structure was used.
Two conditional models were estimated to explore the effect of sedation frequency and sedation intensity. SFS and SIS were incorporated as time varying covariates in linear growth models.
Analysis was performed using SPSS v.17 and Proc Mixed in SAS v.9.2 (Singer, 1998). Final parameter estimates were considered significant at p < .05. Aikake’s information criterion (AIC) and the Bayesian information criterion (BIC) were used to select the best model for this sample.
Results
Description of Study Sample
In this sample (N = 57), participants had been in the ICU for a median of 8 days (range 1–29) and had been receiving mechanical ventilatory support for a median of 6 days (range 1–27 days) prior to enrollment. Participants randomized to the usual care group remained enrolled in the study for a median of 4.1 days (range 1–30 days). Table 3 summarizes the demographic characteristics of the participants and other variables.
Table 3.
Description of Sample at Study Enrollment (N = 57)
| Variable | Median | Range |
|---|---|---|
| Days on Ventilator Prior to Study Enrollment | 6.0 | 1–27 |
| ICU Stay in Days Prior to Study Enrollment | 8.0 | 1–29 |
| Total ICU Stay in days (before and during study) | 15.9 | 2.3–52 |
| Total Days Enrolled in Study | 4.1 | 1–30 |
| Age (years) | 58.7 | 32–86 |
| ICU admission APACHE III score (Scale range 0–299) | 62.3 | 26–118 |
| Baseline Visual Analog Scale-Anxiety (Scale range 0–100) | 57.5 | 0–96 |
| Variable | n (%) | |
| Gender: Male | 23 (60) | |
| Status: Discharged alive | 50 (88) | |
| Race: Caucasian | 51 (90) |
Note. ICU = intensive care unit. APACHE = Acute Physiology and Chronic Health Evaluation.
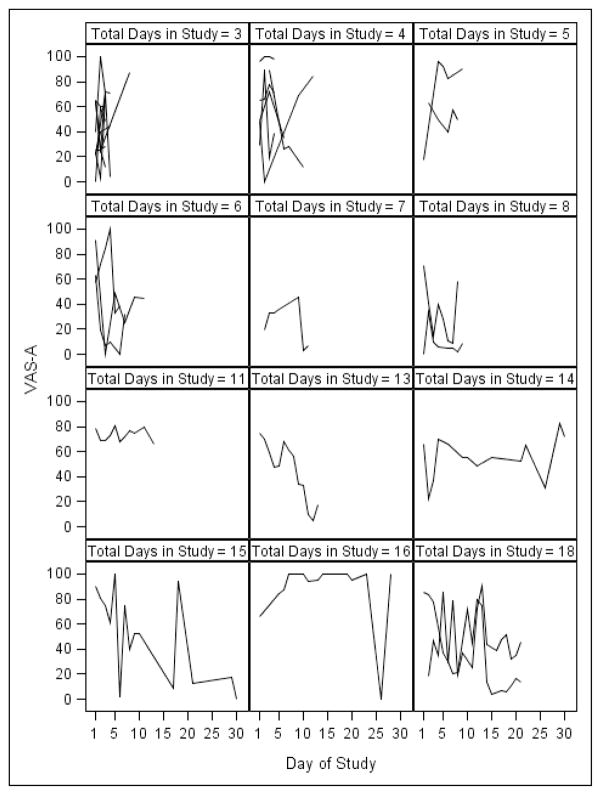
Description of Anxiety Ratings and Frequency of Missing Anxiety Data
Participants reported moderate anxiety at study entry (median VAS-A = 57.5) with a wide range in anxiety from 0 (not anxious at all) to 96 (near the maximum score of 100) (Table 3). Participants reported varying levels of anxiety over the course of study enrollment as illustrated in Figure 1. There is no discernable single pattern to the anxiety ratings for those participants who provided at least three anxiety ratings. For some participants, the pattern is highly variable with increases and decreases in anxiety ratings over the study enrollment period, whereas other participants’ anxiety ratings decrease, increase, or remain essentially at the same level over time.
Figure 1. Summary of Trajectories of Anxiety (VAS-A scores) over Day of Study (N = 31).
Note These graphs are for those subjects who had at least 3 days of VAS-A scores. Graphs are presented by the total number of days in the study with VAS-A scores. These graphs emphasize the great variability in VAS-A scores over time, with no definite pattern of change evident.
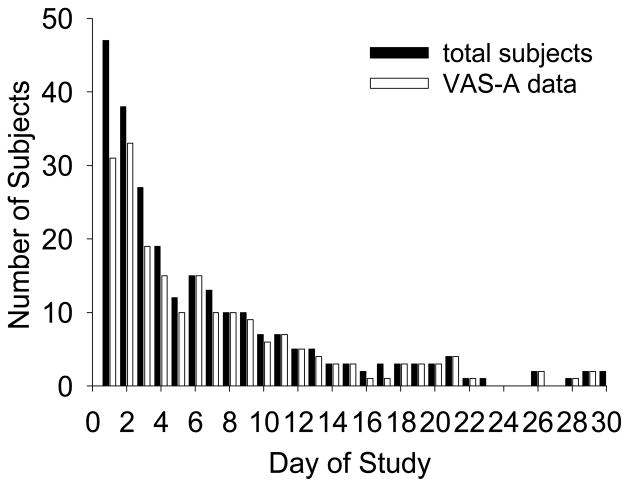
Not all enrolled participants were able to provide anxiety ratings each study day, even at study entry. The two reasons most often cited were that participants were too tired to complete the paper and pencil instrument or were sedated on subsequent study days. There was no relationship between first VAS-A score and the number of days receiving ventilatory support prior to study enrollment (ρ = −.04, p = .79). Overall, the mean number of missing daily VAS-A scores was 3.6 (SD 4.9) with a mode of 1 missing assessment. The numbers of participants able to provide anxiety ratings each study day are presented in Figure 2. All available anxiety scores (VAS-A) were used in the growth modeling analyses.
Figure 2. Number of Participants Providing Anxiety Ratings (VAS-A) by Day of Study.
NoteFirst day of VAS-A data was not always the first day enrolled in the study; 47 participants had their first anxiety data collection on Day 1, 8 participants on Day 2 and 2 participants on Day 3 (total N = 57 participants with VAS-A data).
Modeling Results
Modeling results are presented in Table 4. The first model explored for the analysis was the unconditional means model. This resulted in estimates of variance for both the average VAS-A score between participants and variance in the average within person over time mean. The intercept for this model was 49.5 (p < .001). Both variance parameter estimates were significant (p < .001) indicating that further modeling would be appropriate. The intraclass correlation coefficient (ICC) indicated that 33% of the total variance resulted from differences between participants and 67% was due to the variance over time within participant.
Table 4.
Results of Fitting Successive Models for Anxiety Over Time (N = 57)
| Parameter | (1) Unconditional Means model | (2) Unconditional linear growth model (unstructured variance) | (3) Unconditional linear growth model (Auto Regressive variance) | (4) Unconditional linear growth model (AR + random effects) | (5) Unconditional linear growth model with quadratic effects (AR + RE) | (6) Conditional linear growth model with Sedation intensity (AR + RE) | (7) Conditional linear growth model with Sedation frequency (AR + RE) | |
|---|---|---|---|---|---|---|---|---|
| Fixed Effects | ||||||||
| Intercept | γ00 | 49.5(3.1)** | 57.5(5.9)** | 57.0(5.5)** | 57.0(5.9)** | 37.1(9.5)** | 56.7(6.5)** | 55.7(6.8)** |
| Sedation frequency | γ01 | .19(.50) | ||||||
| Sedation intensity | γ01 | .01(.16) | ||||||
| Days | γ10 | -.54(.38) | -.53 (.32) | -.50(.38) | 2.8(1.3)* | -.49(.38) | -.48(.38) | |
| Days2 | γ20 | -.11(.04) | ||||||
| Variance Components | ||||||||
| Level 1 within person | σ2ε | 557.1(58.9)** | 500.2(55.7)** | 573.2(71.9)** | 521.3(67.4)** | 470.7(57.6)** | 522.4(327.7) | 522.6(67.6)** |
| Level 2-intercept | τ00 | 334.5(100.4)** | 566.8(310.7)* | 320.5(112.6)* | 509.4(317.1) | 557.4(304.4)* | 529.6(327.7) | 528.4(325.4) |
| Linear term variance | τ11 | 1.5(1.2) | .16(.10) | 1.3(1.2) | 2.0(1.5) | 1.3(1.2) | 1.3(1.2) | |
| Selection Criteria | ||||||||
| AIC | 2165.8 | 2161.2 | 2160.8 | 2162.6 | 2162.5 | 2164.4 | 2162.0 | |
| BIC | 2169.8 | 2169.3 | 2166.9 | 2162.8 | 2168.7 | 2174.6 | 2172.2 |
Note. AIC = Aikake’s information criterion. BIC = Bayesian information criterion.
p < .05,
p<.001
Unconditional linear growth models were estimated next. Among these, AIC selected the model with an unstructured within-person error variance-covariance matrix, whereas BIC identified the model with the AR + RE structure as best. In the unconditional growth model, with AR + RE within-person error covariance matrix, the estimated average starting VAS-A value was 57(SE = 5.5). Change was estimated at −.50(SE = .38) points per day; this was not statistically significant (p < .18). A model with a Day2 term was also generated. The coefficient for the quadratic DAY2 term was not significant and both AIC and BIC increased, so the quadratic change model received no further consideration.
A conditional linear growth model was then generated to account for the influence of sedative and analgesic medications on anxiety (sedative dose frequency and sedation intensity score). The daily sedation frequency count score and sedation intensity score was entered into separate unconditional growth models with DAY predicting VAS-A. The time varying effect of sedative exposure did not improve relative model fits and was not significant for either the dose frequency or the sedation intensity. Sedative exposure (dose frequency and sedation intensity) left the estimates of the intercept and slope virtually unchanged. These models all left a significant amount of unexplained variance both within person over time and between subjects. Figure 3 and Figure 4 depict median anxiety ratings with sedation dose frequency and sedation intensity over total days on study protocol.
Figure 3.
Median Anxiety Ratings and Sedation Dose Frequency over Day of Study
Figure 4.
Median Anxiety Ratings and Sedation Intensity Score over Day of Study
Discussion
The purposes of this paper were to describe anxiety ratings of critically ill patients receiving mechanical ventilatory support, to discern any pattern of change in daily anxiety ratings, to determine if anxiety decreases over the course of ventilatory support, and to explore the influence of sedative exposure on anxiety ratings. Participants in this sample were receiving prolonged periods of ventilatory support prior to study enrollment and reported moderate levels of anxiety when first measured at study entry, despite receiving sedative and analgesic medications known to influence anxiety.
The anxiety data reported in this paper reflects those participants randomized to the usual care condition only, and does not consider covariates such as illness severity, length of ventilatory support, or length of ICU stay. The individual anxiety ratings reported by participants demonstrated patterns of highly individual and variable anxiety. Reported anxiety ratings decreased for some participants over time; others reported anxiety ratings that fluctuated or increased.
The overall pattern of anxiety ratings for this group of participants over the duration of study enrollment suggested a possible slight decline over time with a highly variable pattern of this symptom experience. Participants demonstrated a general pattern of moderate anxiety over the course of study enrollment. These data are similar to findings from previous descriptive, cross-sectional work that showed patients receiving mechanical ventilatory support for 22 or more days had the highest anxiety ratings, followed by those in the 6–21 day group (Chlan 2003).
Results of the mixed models analysis were that VAS-A ratings slowly decreased over time. However, there was not a statistically significant decrease in these anxiety ratings over study enrollment in this group of participants.
Sedative exposure did not significantly influence the participants’ daily anxiety ratings. Neither dose frequency nor sedation intensity explained a statistically significant amount of variance within person or over time on anxiety ratings.
Limitations
Study limitations include the number of missing data points on the VAS-A when participants were too fatigued to complete the assessments, were sedated, or were too ill to provide daily anxiety assessments. Measurement of subjective symptoms remains a challenge in non-verbal, critically ill patients with profound physiological and psychological limitations. Anxiety arises from numerous physiological and psychological factors in ventilated patients. This study did not attempt to discern the sources of anxiety; anxiety ratings reported here provided only one assessment time point per day.
Another limitation is the various entry into study time points. Participants were enrolled at various times during their ICU stay and course of mechanical ventilatory support. Thus, it is not known how anxious a participant might have been the first day receiving mechanical ventilation in comparison to their first study enrolled day. However, there was no relationship between first anxiety rating obtained and days receiving ventilatory support prior to study enrollment.
Lastly, an influence of sedative and analgesic medications was not seen in the analysis possibly due to the relatively uniform pattern of dose frequency, but a varying pattern of sedation intensity. Further consideration of these issues is warranted.
Summary and Conclusions
While findings from this study do suggest that anxiety does decrease over time for some patients receiving mechanical ventilatory support, other patients do not readily adjust to the ventilator and/or the ICU environment and do not experience lessening anxiety over the course of treatment. Critical care clinicians should not expect that anxiety decreases over time for all ventilated patients. On-going nursing assessment and appropriate, individualized interventions with patients receiving mechanical ventilatory support are needed in order to appropriately address anxiety symptom management.
Acknowledgments
The project described was supported by Grant Number R01NR009295 from the National Institute of Nursing Research. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institute of Nursing Research or the National Institutes of Health.
Contributor Information
Linda Chlan, School of Nursing, University Of Minnesota, Minneapolis, Minnesota.
Kay Savik, School of Nursing, University Of Minnesota, Minneapolis, Minnesota.
References
- Chlan L. Effectiveness of a music therapy intervention on relaxation and anxiety for patients receiving ventilatory assistance. Heart and Lung. 1998;27:169–176. doi: 10.1016/s0147-9563(98)90004-8. [DOI] [PubMed] [Google Scholar]
- Chlan L. Description of anxiety levels by individual differences and clinical factors in patients receiving mechanical ventilatory support. Heart and Lung: The Journal of Acute and Critical Care. 2003;32:275–282. doi: 10.1016/s0147-9563(03)00096-7. [DOI] [PubMed] [Google Scholar]
- Chlan L. Relationship between two anxiety instruments in patients receiving mechanical ventilatory support. Journal of Advanced Nursing. 2004;48:493–499. doi: 10.1111/j.1365-2648.2004.03231.x. [DOI] [PubMed] [Google Scholar]
- Chlan L, Savik K, Weinert C. Development of a shortened state anxiety scale from the Spielberger State-Trait Anxiety Inventory (STAI) for patients receiving mechanical ventilatory support. Journal of Nursing Measurement. 2003;11:283–293. doi: 10.1891/jnum.11.3.283.61269. [DOI] [PubMed] [Google Scholar]
- Cline ME, Herman J, Shaw ER, Morton RD. Standardization of the visual analogue scale. Nursing Research. 1992;4:378–380. [PubMed] [Google Scholar]
- Cox C, Carson S, Govert J, Chelluri L, Sanders G. An economic evaluation of prolonged mechanical ventilation. Critical Care Medicine. 2007;35:1918–1927. doi: 10.1097/01.CCM.0000275391.35834.10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frazier S, Moser D, Daley L, McKinley S, Riegel B, Garvin B. Critical care nurses’ beliefs about and reported management of anxiety. American Journal of Critical Care. 2003;12:19–27. [PubMed] [Google Scholar]
- Gift AG. Visual analogue scales: measurement of subjective phenomena. Nursing Research. 1989;38:286–288. [PubMed] [Google Scholar]
- Gries ML, Fernsler J. Patient perceptions of the mechanical ventilation experience. Focus on Critical Care. 1988;15:52–59. [PubMed] [Google Scholar]
- Johnston M, Sexton D. Distress during mechanical ventilation: patients’ perceptions. Critical Care Nurse. 1990;10:48–52. [PubMed] [Google Scholar]
- Knaus WA, Wagner DP, Draper EA, Zimmerman JE, Bergner M, Bastos PG, et al. The APACHE III prognostic system. Risk prediction of hospital mortality for critically ill hospitalized adults. Chest. 1991;100:1619–1636. doi: 10.1378/chest.100.6.1619. [DOI] [PubMed] [Google Scholar]
- Knebel AR, Janson-Bjerklie SL, Malley JD, Wilson AG, Marini JJ. Comparison of breathing comfort during weaning with two ventilatory modes. American Journal of Respiratory and Critical Care Medicine. 1994;149:14–18. doi: 10.1164/ajrccm.149.1.8111572. [DOI] [PubMed] [Google Scholar]
- Lee KA, Kieckhefer GM. Measuring human responses using visual analogue scales. Western Journal of Nursing Research. 1989;11:128–132. doi: 10.1177/019394598901100111. [DOI] [PubMed] [Google Scholar]
- Li D, Puntillo K. A pilot study on coexisting symptoms in intensive care patients. Applied Nursing Research. 2006;19:216–219. doi: 10.1016/j.apnr.2006.01.003. [DOI] [PubMed] [Google Scholar]
- Logan J, Jenny J. Qualitative analysis of patients’ work during mechanical ventilation and weaning. Heart and Lung. 1997;26:140–147. doi: 10.1016/s0147-9563(97)90074-1. [DOI] [PubMed] [Google Scholar]
- Lush MT, Janson-Bjerklie S, Carrieri VK, Lovejoy N. Dyspnea in the ventilator-assisted patient. Heart and Lung. 1988;17:528–535. [PubMed] [Google Scholar]
- McCartney JR, Boland RJ. Anxiety and delirium in the intensive care unit. Critical Care Clinics. 1994;10:673–680. [PubMed] [Google Scholar]
- Rotondi A, Chelluri L, Sirio CA, Mendelsohn A, Schulz R, Belle S, et al. Patients’ recollections of stressful experiences while receiving prolonged mechanical ventilation in an intensive care unit. Critical Care Medicine. 2002;30:746–752. doi: 10.1097/00003246-200204000-00004. [DOI] [PubMed] [Google Scholar]
- Singer JD. Using SAS Proc Mixed to fit multilevel models, hierarchical models, and individual growth models. Journal of Educational and Behavioral Statistics. 1998;24:323–355. [Google Scholar]
- Vogelsang J. The Visual Analog Scale: an accurate and sensitive method for self-reporting preoperative anxiety. Journal of Post-Anesthesia Nursing. 1988;3:235–239. [PubMed] [Google Scholar]
- Weinert C, Calvin A. Epidemiology of sedation for mechanically ventilated patients. Critical Care Medicine. 2007;35:393–401. doi: 10.1097/01.CCM.0000254339.18639.1D. [DOI] [PubMed] [Google Scholar]
- Wewers M, Loew N. A critical review of visual analog scales in the measurement of clinical phenomena. Research in Nursing & Health. 1990;13:227–236. doi: 10.1002/nur.4770130405. [DOI] [PubMed] [Google Scholar]
- Wong H, Lopez-Nahas V, Molassiotis A. Effects of music therapy on anxiety in ventilator-dependent patients. Heart and Lung. 2001;30:376–387. doi: 10.1067/mhl.2001.118302. [DOI] [PubMed] [Google Scholar]