Abstract
The use of somatostatin analogs is a new conservative therapeutic approach for the treatment of chyle fistulas developing after thyroid cancer surgery. The combination therapy with a total parenteral nutrition should avoid the high morbidity of a re-intervention with an uncertain outcome. This promising trend is supported by the present case report of a chyle leak occurring after total thyroidectomy with central and lateral neck dissection for a papillary carcinoma, which was treated successfully without immediate or distant sequelae.
Key Words: Chyle fistula, Octreotide, Somatostatin, Thoracic duct, Thyroid cancer, Thyroid surgery
Introduction
Thoracic duct injury is a rare but troublesome complication of cervical surgeries. First described by Cushing in 1898, chyle fistula can induce severe nutritional, metabolic and immune disturbances, delay wound healing, prolong hospital stay and, in the past, even resulted in death [1, 2]. The incidence rate reported in the literature ranges from 0.5 to 2.5% [1, 2, 3, 4, 5, 6, 7, 8]. In thyroid surgery, the rate of chyle fistula increases significantly (p < 0.001) with the extent of the surgical procedure: 0.5% after less than total surgery with central compartment node dissection (CCND), 0.8% in patients with total thyroidectomy and CCND, 5.1% after total thyroidectomy associated with ipsilateral neck dissection, and 6.2% in patients treated by total thyroidectomy with bilateral neck dissection [5]. Due to anatomic reasons (left side termination of thoracic duct in 75–92%), these injuries occur predominantly on the left side in patients undergoing lateral neck dissection [3, 5, 9]. Conversely, Roh et al. [9] reported a higher but not significant incidence of chyle leakage on the right side (8.9 vs. 7.5%; p = 0.802). Most chyle fistulas (25–75%) develop postoperatively, with a 86% rate of occurrence between the first and the third postoperative day [6].
Case Report
A 27-year-old woman was referred to our department for the surgical treatment of a goiter with hyperthyroidism treated for 2 years with neomercazole 10 mg/day and levothyrox 50 µg/day. Physical examination revealed an enlarged thyroid associated with left mid-lower jugular nodes. Ultrasonography showed a suspicious 11-mm nodule in the left superior lobe and two ipsilateral 20-mm cervical nodes. Fine needle cytology aspiration of cervical lymphadenopathy confirmed the involvement of a papillary thyroid cancer. In May 2010, a total thyroidectomy with central and left lateral neck dissection was performed.
Pathologic specimen examination showed a 12 × 15 mm papillary cancer in the left superior lobe without extrathyroid extension. Three out of the 42 nodes removed were metastatic.
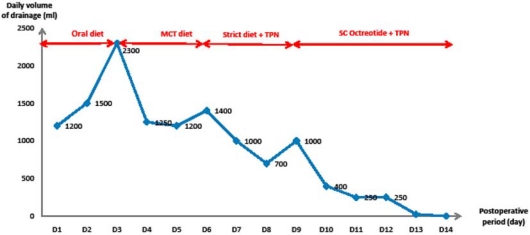
On the third postoperative day, a high-output lymph fistula with milky appearance was observed following a drainage collection of 2,300 ml. We decided to adopt a conservative medical management consisting of a diet of medium-chain triglycerides for 3 days. Persistence of the fistula (1,400 ml/day) on day 6 led to the introduction of a strict diet and parenteral nutrition, followed by a 50% reduction of the daily drainage (700 ml/day) of the chyle fistula. On day 8, after adjunction of a pharmacological treatment with subcutaneous octreotide (0.1 mg every 8 h), the fistulous debit decreased gradually until it disappeared completely after 6 days (fig. 1). No side effects were observed. Oral nutrition was initiated and the cervical closed suction drains removed. On postoperative day 16, the patient was discharged home in good condition with correct wound healing.
Fig. 1.
Evolution of the chyle fistula leak. MCT = Middle-chain triglyceride; SC Octreotide = subcutaneous octreotide administration; TPN = total parenteral nutrition.
One month later, the patient underwent a radioablation therapy (3.56 GBq) after a radioiodine scanning revealed no persistent disease or distant metastases. After a follow-up of 10 months, this young female had no signs of either local and/or distant recurrence or of postoperative functional and cosmetic sequelae.
Discussion
Priority must be given to the prevention of lymph fistulas related to an injury of the main thoracic duct or one of its multiple branches (40% of cases) [3, 6, 8, 10]. A meticulous surgical technique combined with magnifying glasses has recently been advocated by Lorenz et al. [6]. Intraoperative diagnosis of lymphatic leakage is better treated immediately by ligature (3-0 or 4-0 non-absorbable) than suture procedures [6, 9]. In most cases, postoperative diagnosis is clinically obvious and no complementary investigations such as lymphoscintigraphy and/or CT scan are required [3, 8]. Chyle fistula usually starts after an oral diet, with an increase of drainage volume with milky appearance, swelling of supraclavicular fossa, erythema or induration of the skin [3, 6, 8]. Measurement of triglyceride concentrations in postoperative fluid drainage may assist the early diagnosis of chyle fistula. A triglyceride level exceeding 100 mg/dl, a greater serum concentration or a lymphocyte count of 50% are thought to support the diagnosis [4, 6, 7, 8, 9, 11.
Although several therapeutic approaches, including nutritional, surgical and pharmacological procedures, have been proposed, there is currently no clear consensus on the optimal management of thoracic duct fistulas [5]. The decision between conservative and surgical treatment options still remains a subject of debate in literature reviews [5, 6, 7, 8, 11].
Conservative medical management includes several lines of treatment and is imperatively associated with adequate drainage, applying pressure dressing, serial aspirations, bed rest and nutritional modifications [11, 6, 7, 8, 8]. Except for initially large chyle leaks, conservative methods should be considered first since they allow a cure rate ranging from 58 to 100% [6].
The first step is an elemental diet supplemented with medium-chain triglycerides, directly absorbed into the portal circulation by passing the lymphatic system [4, 6, 7, 8, 9]. Conversely, long-chain triglycerides entering the blood stream via the chyle should be avoided [4, 7, 8]. According to Lorenz et al. [6], dietary restriction was less successful than total fasting.
In case of failure and despite the increased costs, a total parenteral nutrition is recommended as a second-line approach in most institutions [4, 6, 7, 8]. Conservative medical treatment should not exceed 30 days. Furthermore, the optimal timing and the decision between conservative and surgical options remain unclear. For Coşkun et al. [7] and others [1, 4, 8, 9], a persistent drainage output of >600 ml/day for 5–7 days despite medical conservative therapy or an extremely high output (>1.5–2 liters) may require surgical re-intervention. More recently, Lorenz et al. [6] have suggested a daily 300-ml output drainage threshold and an early decision on day 4 after initiating fasting protocol in favor of either continued medical treatment or surgery.
The aim of surgical therapy is to close the leak site with local application of fibrin glue, a pectoralis major muscle flap transfer or an absorbable mesh [6, 7, 8, 9]. En bloc ligature of the thoracic duct by videothoracoscopy has also been proposed in patients who not respond to cervical re-intervention [2, 3, 5, 9, 11]. However, sclerotherapy devices with topical application of tetracycline or doxycycline have been abandoned because of local neurotoxicities (phrenic or vagus nerve palsy) [2, 6, 9].
Somatostatin and its long-acting analog octreotide were first described in 1990 by Ulíbarri et al. [13] as an effective and successful adjunct to conservative therapy of iatrogenic thoracic duct injuries. These preliminary data were confirmed 10 years later by Markham et al. [14] in a prospective study on dogs demonstrating a threefold decrease in thoracic duct fistula output after administration of octreotide. The exact mechanism of action of this neurohormonal and panacrine agent remains unknown. It reduces gastrointestinal chyle production by decreasing splanchnic blood flow and decreasing gastric, biliary, pancreatic and intestinal secretions [1, 2, 4, 7, 11]. Administered at a recommended dose of 3.5–12 µg/kg/h for 3–14 days [11], octreotide therapy requires good monitoring of blood glucose levels every 6 h because of the inhibition induced by insulin, glucagon and motilin secretion [2]. The risk of cholecystitis secondary to cholestasis should also not be underestimated in patients eligible for prolonged treatment [1]. In addition to recent data [1, 4, 6, 7, 8, 11, 15], our observation demonstrated that octreotide is a promising alternative therapy useful for decreasing chyle fistula after thyroid cancer surgery and increasing the success of conservative management of this worrying complication.
Advances in surgeons’ knowledge of the anatomic landmarks and variability of the cervical portion of the thoracic duct should minimize the incidence of injuries which lead to an often unrecognized but significant morbidity rate [10].
References
- 1.Valentine CN, Barresi R, Prinz RA. Somatostatin analog treatment of a cervical thoracic duct fistula. Head Neck. 2002;24:810–813. doi: 10.1002/hed.10103. [DOI] [PubMed] [Google Scholar]
- 2.Collard JM, Laterre PF, Boemer F, Reynaert M, Ponlot R. Conservative treatment of postsurgical lymphatic leaks with somatostatin-14. Chest. 2000;117:902–905. doi: 10.1378/chest.117.3.902. [DOI] [PubMed] [Google Scholar]
- 3.Rodier JF, Issert B, Gadonneix P, Dauplat J, Gauthier JP, Giraud B, Condat P, Mercier R. Injury of the thoracic duct during neck surgery (in French) J Chir. 1986;123:729–732. [PubMed] [Google Scholar]
- 4.Smoke A, Delegge MH. Chyle leaks: consensus on management? Nutr Clin Pract. 2008;23:529–532. doi: 10.1177/0884533608323424. [DOI] [PubMed] [Google Scholar]
- 5.Lee YS, Nam KH, Chung WY, Chang HS, Park CS. Postoperative complications of thyroid cancer in a single center experience. J Korean Med Sci. 2010;25:541–545. doi: 10.3346/jkms.2010.25.4.541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lorenz K, Abuazab M, Sekulla C, Nguyen-Thanh P, Brauckhoff M, Dralle H. Management of lymph fistulas in thyroid surgery. Langenbecks Arch Surg. 2010;395:911–917. doi: 10.1007/s00423-010-0686-2. [DOI] [PubMed] [Google Scholar]
- 7.Coskun A, Yildirim M. Somatostatin in medical management of chyle fistula after neck dissection for papillary thyroid carcinoma. Am J Otolaryngol. 2010;31:395–396. doi: 10.1016/j.amjoto.2009.05.002. [DOI] [PubMed] [Google Scholar]
- 8.Priego Jiménez P, Collado Guirao MV, Rojo Blanco R, Grajal Marino R, Rodríguez Velasco G, García Villanueva A. Chyle fistula in right cervical area after thyroid surgery. Clin Transl Oncol. 2008;10:593–596. doi: 10.1007/s12094-008-0257-4. [DOI] [PubMed] [Google Scholar]
- 9.Roh JL, Kim DH, Park CI. Prospective identification of chyle leakage in patients undergoing lateral neck dissection for metastatic thyroid cancer. Ann Surg Oncol. 2008;15:424–429. doi: 10.1245/s10434-007-9692-1. [DOI] [PubMed] [Google Scholar]
- 10.Ammar K, Tubbs RS, Smyth MD, Wellons JC, 3rd, Blount JP, Salter G, Oakes WJ. Anatomic landmarks for the cervical portion of the thoracic duct. Neurosurgery. 2003;53:1385–1387. doi: 10.1227/01.neu.0000093826.31666.a5. [DOI] [PubMed] [Google Scholar]
- 11.Rosing DK, Smith BR, Konyalian V, Putnam B. Penetrating traumatic thoracic duct injury treated successfully with octreotide therapy. J Trauma. 2009;67:E20–E21. doi: 10.1097/01.ta.0000236052.38469.8e. [DOI] [PubMed] [Google Scholar]
- 12.Merante Boschin I, Meduri F, Toniato A, Pagetta C, Casalide E, Rubello D, Pelizzo MR. Cervical lymphorrea after nodal dissection: role of fasting based on clinical evidence (in Italian) Minerva Chir. 2006;61:57–62. [PubMed] [Google Scholar]
- 13.Ulíbarri JI, Sanz Y, Fuentes C, Mancha A, Aramendia M, Sánchez S. Reduction of lymphorrhagia from ruptured thoracic duct by somatostatin. Lancet. 1990;336:258. doi: 10.1016/0140-6736(90)91793-a. [DOI] [PubMed] [Google Scholar]
- 14.Markham KM, Glover JL, Welsh RJ, Lucas RJ, Bendick PJ. Octreotide in the treatment of thoracic duct injuries. Am Surg. 2000;66:1165–1167. [PubMed] [Google Scholar]
- 15.Mincher L, Evans J, Jenner MW, Varney VA. The successful treatment of chylous effusions in malignant disease with octreotide. Clin Oncol (R Coll Radiol) 2005;17:118–121. doi: 10.1016/j.clon.2004.06.016. [DOI] [PubMed] [Google Scholar]