Abstract
Objective
Given the fundamental role of thought disorder in schizophrenia, subtle communication disturbance may be a valuable predictor of subsequent development of psychosis. Here we examined the contribution of thought and communication disturbance to the prediction of outcome in adolescents identified as putatively prodromal for psychosis.
Method
Transcribed speech samples were elicited from 105 adolescents (54 identified as being at clinical high risk for a first episode of psychosis (CHR) and 51 demographically comparable comparison subjects) and coded for formal thought disorder (FTD) and linguistic cohesion. We then examined the association of baseline FTD/cohesion with conversion to psychosis and social and role outcome at follow-up, approximately one year later.
Results
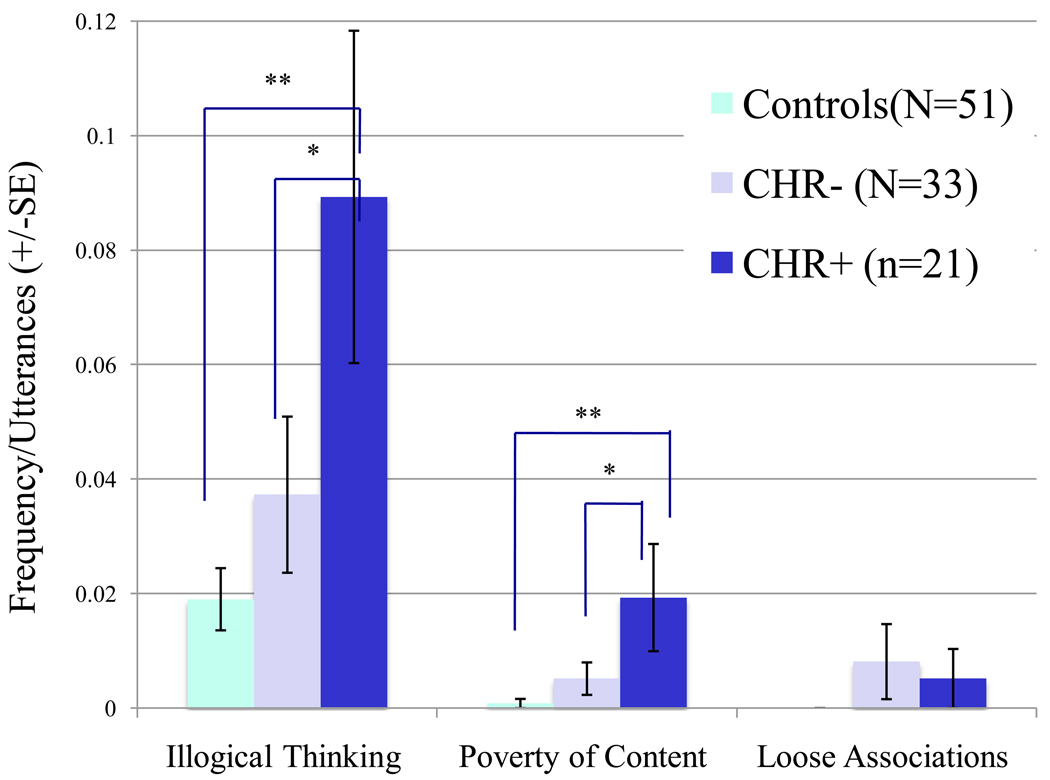
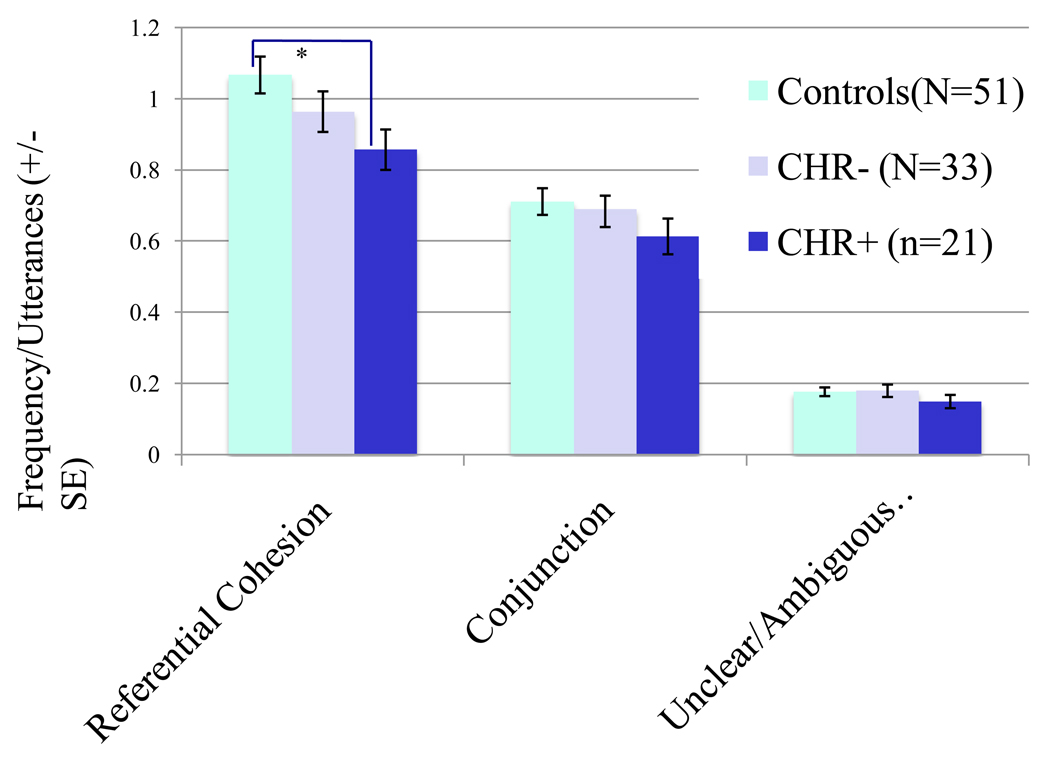
At baseline, CHR patients who subsequently converted to psychosis (CHR+) showed an elevated rate of illogical thinking and poverty of content (POC) in their speech, relative to both typically developing controls and non-converters (CHR−). CHR+ youth also used significantly less referential cohesion at baseline, indicating that they provide fewer references to people, objects, or events mentioned in preceding utterances. Multiple regression models indicated that, among measures of FTD/cohesion, illogical thinking was uniquely predictive of subsequent conversion to psychosis, whereas POC and referential cohesion were significant predictors of social and role functioning, respectively.
Conclusions
Despite the absence of fully psychotic symptoms, putatively prodromal individuals evidence signs of communication disturbance that are qualitatively similar to those seen in schizophrenia, and are predictive of both conversion to psychosis and psychosocial outcome. These findings suggest that FTD measures have prognostic significance for at-risk youth.
Keywords: thought disorder, psychosis prodrome, schizophrenia, language, psychosocial outcome
Introduction
Formal thought disorder (FTD) - a disruption in the flow of thought, inferred from disorganization of spoken language - is one of the most severe manifestations of disturbed language processing 1. Marked disturbances in thought and language are a hallmark of child- and adult-onset schizophrenia 2, 3. The persistence of thought disorder after the resolution of a psychotic episode is a robust predictor of poor outcome4, and thought disorder has been shown to be a sensitive and specific indicator of schizophrenia and schizophrenia spectrum disorder in a variety of studies2, 5, 6.
Notably, clinically unaffected relatives of patients with schizophrenia also have elevated scores on measures of communication deviance, indicating a pattern of confusing communications that may hinder the establishment and maintenance of a shared focus of attention between speaker and listener 7,8. Detailed analysis of speech samples of the first-degree relatives of patients with schizophrenia reveal increased instances of lack of structural clarity, vague, over-inclusive references and ambiguous word meanings 9–12. In addition, greater communication deviance in parents has been associated with more severe lifetime positive symptoms in patient offspring 13. In a twin study, Docherty and Gottesman 14 found that a particular type of communication failure, the ‘missing information’ reference (i.e. reference to information not previously presented to the listener), distinguished identical from fraternal non-ill co-twins. In addition, thought disorder, as characterized by deviant verbalizations, shows familial aggregation in clinically unaffected relatives of schizophrenic patients 15. Individuals with schizotypal personality disorder also display signs of thought disorder (illogical thinking and loose associations) that are qualitatively similar to those seen in childhood-onset schizophrenia patients 2. Additionally, from a developmental perspective, Caplan 2, 16 noted that the age -related increases in use of cohesive devices in typically developing children were not observed in children with schizophrenia, suggesting that illness onset may impact the ongoing development of communication skills 2, 17. Collectively, these findings support the notion that disordered communication and thought may be an important manifestation of genetic vulnerability to schizophrenia 18, 19, and indeed, may represent a more highly penetrant expression of schizophrenia susceptibility genes 15.
While such findings in those at familial high risk for psychosis support a neurodevelopmental model of vulnerability to the illness, the extent to which these deficits are predictive of the later onset of psychotic illness remains unclear. This difficulty- in combination with increasing evidence that longer duration of untreated psychosis results in poorer outcome 20–23 has stimulated an important new direction in the field, emphasizing the development and refinement of criteria for ascertaining adolescents and young adults deemed to be at high risk for imminent onset of psychotic illness. This ‘clinical high risk’ approach puts a premium on early treatment, with prevention as the ultimate goal 24–26. Such endeavors critically rely on accurate prediction of future diagnosis. As such, quantitative measures of thought disorder may provide a means of characterizing subtle deficits of communication and cognition in at-risk individuals. However, no study to date has attempted to use such measures in clinically at-risk youth as a means of predicting outcome.
The primary objective of this study is to determine whether manifestations of thought disorder and communication disturbance can be detected in clinical high-risk (CHR) youth prior to illness onset and predict conversion to psychosis. On the basis of the findings previously observed in children and adolescents with overt schizophrenia diagnoses, we made the following predictions. First, we anticipated that the speech of CHR youth would have significantly more formal thought disorder (i.e., illogical thinking, loose associations) and cohesive deficits (i.e., underuse of conjunction and referential cohesion) than that of healthy children. Second, thought disorder and cohesive deficits at baseline in CHR youth would predict subsequent conversion to psychosis and poorer psychosocial outcome at follow-up. Third, age-related changes would be observed for the cohesion and FTD scores of the typically developing, but not the CHR group.
Procedures
Participants
Fifty-nine CHR participants and 51 typically developing control subjects were enrolled in an ongoing longitudinal study at the University of California, Los Angeles. Fifty-four of the 59 CHR patients initially enrolled in the study completed at least one follow-up evaluation, resulting in a retention rate of 92%; these individuals were included in the current analysis (see Table 1). Control subjects were recruited from schools in the Los Angeles area and from the community via web-based and newspaper advertisements, and were age-matched to the CHR sample. Baseline measures included clinical and functional assessments, including the Story Game interview (described below), and a neuropsychological test battery. Subjects were followed for up to two years, and at intervening time points completed follow-up assessments of clinical and functional outcome. CHR participants met criteria for of one of three prodromal syndrome categories, as assessed by the Structured Interview for Prodromal Syndromes (SIPS 27): (1) attenuated (subthreshold) psychotic symptoms; (2) transient, recent-onset psychotic symptoms; or (3) a substantial drop in social/role functioning in conjunction with Schizotypal Personality Disorder diagnosis or a first-degree relative with a psychotic disorder. Controls did not meet DSM-IV criteria for a psychiatric disorder as determined by Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I/P 28) or Kiddie Schedule for Affective Disorders and Schizophrenia (K-SADS 29) interview, have a first-degree family history of a psychotic disorder, or meet criteria for any of the three prodromal states defined above. Additional exclusion criteria for all participants included the presence of a neurological disorder, drug or alcohol abuse or dependence within the past 6 months, insufficient English fluency, and/or IQ below 70. All clinical interviews were conducted by Master's-level or PhD. mental health specialists, who had been trained to rigorous standards of reliability (ICC ≥ 0.85 for symptom ratings; kappa >.90 for diagnostic agreement). Detailed information regarding SIPS prodromal criteria, reliability and consensus procedures are described elsewhere 30, 31. Study procedures were performed in accordance with policies of the human subject protection committees of the University of California at Los Angeles, and informed consent/assent was obtained from all subjects.
Table 1.
Baseline demographic and clinical characteristics of study participants
| Characteristic | CHR Not Converted (CHR− ; N=33) |
CHR Converted (CHR+; N=21) |
HC (N = 51) |
F/t/X2 statistic, p- value |
|---|---|---|---|---|
| Demographic Characteristics | ||||
| Age at examination, mean (± SD) |
16.97 (3.4) | 17.3 (4.4) | 16.2 (2.7) | F=1.13, p=.33 |
| % Female (N) | 36% (12) | 19% (4) | 39% (20) | η2=2.8, p =.25 |
| IQ a | 106.9(17.6) | 104.3 (14.4) | 111.5 (13.1) | F=1.59, p=.21 |
| Parental Education, mean (± SD) |
14.7 (3.7) | 15.0 (3.4) | 15.6 (3.3) | F=.28, p=.76 |
| Race/Ethnicity %Caucasian (N) |
61% (20) | 57% (12) | 49% (25) | η2=11.79, p =.30 |
| % Asian (N) | 3% (1) | 14% (3) | 8% (4) | |
| % African-American (N) |
3% (1) | 5% (1) | 14% (7) | |
| % Hispanic/ Latino (N) |
24% (8) | 19% (4) | 16% (8) | |
| % Mixed Race/ Other (N) |
9% (3) | 5% (1) | 14% (7) | |
| Clinical Characteristics | ||||
| GAF score, mean (± SD)b |
43.4 (11.0) | 37.4 (14.3) | 79.3 (14.1) | F=58.6, p<.001 |
| SOPS Mean Total Positive Symptom score (±SD) |
13.2 (3.9) | 14.3 (4.8) | N/A | t=0.77, p=.38 |
| Current Atypical Antipsychotic Use, n (%) |
6 (18%) | 4 (19%) | N/A | η2=.006, p=.94 |
| Current Mood Stabilizer Use, n (%) |
3 (9%) | 4 (19%) | N/A | η2=1.13, p=.29 |
| Current SSRI Use, n (%) |
9 (27%) | 3 (14%) | N/A | η2=1.25, p=.26 |
Note: SSRI = selective serotonin reuptake inhibitor.
IQ Estimate based on Wechsler Abbreviated Scale of Intelligence (WASI)
Global Assessment of Functioning (GAF) scores did not differ significantly between clinical high-risk converters (CHR+), and clinical high-risk non-converters (CHR−) (p=.11).
Procedures
During the follow up period, clinical interviews were re-administered at 6-month intervals, up to a maximum of 24 months. The mean duration of follow-up was 14.8 months (+/−9.5 months). If case managers observed clinical deterioration in the patients under their care, a reassessment was conducted between regularly scheduled assessments. Conversion to psychosis was defined according to SIPS criteria, as described in Cannon et al.32. Briefly, a SIPS diagnosis of a psychotic syndrome was assigned via consensus diagnosis when a patient experienced psychotic symptoms of certain intensity (e.g., delusional conviction) and frequency or duration (one hour per day for four days a week during the last month), or had a severe impact (seriously disorganizing or dangerous). These criteria are designed to operationalize the threshold for a DSM-IV Axis I psychotic disorder diagnosis. Additionally, DSM-IV diagnoses attained at the point of conversion were determined by direct SCID/K-SADS interview of the patient and their parent or guardian. Twenty-one of the CHR subjects in our sample (39%) converted to a psychotic disorder over the two-year follow-up period. Diagnostic outcomes were: schizophrenia (6), schizoaffective disorder (4; 3 depressive type, 1 bipolar type), delusional disorder (2), bipolar disorder with psychotic features (3), major depression with psychotic features (1), and Psychotic Disorder, Not Otherwise Specified (NOS; 5). At the time of the clinical assessment, social and role functioning were also assessed using the Global Functioning: Social scale (GFS 33) and the Global Functioning: Role scale (GFR34) measures designed to provide global assessments of psychosocial functioning in adolescent and young adult populations 35. These scales rate social and role function on two separate 10-point Likert scales, independent of symptom severity.
At baseline, 19.5% of the CHR subjects overall were taking antipsychotic medication, 13% were taking mood stabilizers, and 22% were taking SSRI antidepressants. Baseline medication status did not differ between those who did and did not subsequently convert to a psychotic disorder (see Table 1).
Thought Disorder Measures
FTD was assessed using the Story Game to elicit speech samples which were transcribed and scored with the Kiddie Formal Thought Disorder Rating Scale (K-FTDS 17) and Caplan and colleague’s 36 modification of Halliday and Hassan’s 37 analysis of cohesion, as described below.
The Story Game
A three-part audiotape is played for the study participant. In the first and the last part, the subject listens to a brief audiotaped story, and is asked to retell it, as well as to answer a set of open-ended questions about the narrative. Examples of such questions are: “What did (or didn’t) you like about that story?”, and “Do you think this is a true story? Why (or why not)?” In the middle part, the child is asked to select one of four topics (e.g., “an unhappy child”) and asked to construct their own story. The topics of the stories were selected because of their potential to elicit pathological thought content in children and adolescents. Three alternate forms of the Story Game were used, which were counterbalanced across subjects.
This task was designed to be an ecologically valid assessment of natural speech 17; it has been validated and used extensively in other clinical populations, including children and adolescents between the ages of 8–18 with autistic spectrum disorders 38, childhood-onset schizophrenia and spectrum disorders 2, 6, 39, attention deficit hyperactivity disorder 40, and epilepsy 41, 42. Task administration takes about 20–25 minutes, providing an extensive amount of speech for analysis.
Formal Thought Disorder
A single rater, who was trained to high standards of reliability (>90% agreement with gold standard ratings) in coding of the Kiddie Formal Thought Disorder Rating Scale (K-FTDS) and who was blind to risk status and diagnostic outcome, coded videotapes of the Story Game with the K-FTDS, according to the criteria described in Caplan et al. 17. The scores derived from the K-FTDS ratings are frequency counts of illogical thinking, loose associations, incoherence, and poverty of content of speech divided by the number of utterances made by the subject. Higher scores on these FTD measures are negative, indicating a higher level of thought disorder. Illogical thinking indicates a failure to present the listener with appropriate reasoning in causal and noncausal utterances, or contradicting oneself (see Table 2a for examples). The child with loose associations changes the topic of conversation unpredictably without preparing the listener for the topic change. The child with poverty of content of speech (POC) does not elaborate on the topic of conversation despite use of 2 or more utterances. Because of scrambled syntax, the contents of the utterance of the child with incoherence are not understood. Due to the low base rate of incoherence in our sample, this measure was dropped from further analysis.
Table 2.
Examples of formal thought disorder coded by Kiddie-Formal Thought Disorder Scale (K-FTDS)
| Code | Description | Example |
|---|---|---|
| Illogical thinking | Inappropriate or immature use of causal utterances |
“I went to school today because my name is Tom.” |
| Unfounded reasoning in non- causal utterances |
“Sometimes I go to school and when I am done singing, I start coughing and that is when I stop.” |
|
| Makes a statement and then refutes it |
“I liked the book but I don’t like books like that.” |
|
| Loose associations | Abrupt topic changes without alerting the listener |
“I have a lot of homework today and Patrick is my favorite character on that show about trains.” |
| Poverty of content | After two utterances, no content is expressed |
“I suppose … what? Maybe..Well yes, I see. I suppose that’s all.” |
| Incoherence | Contents of a statement cannot be understood due to scrambled syntax |
“The boys day no boys fast running.” |
Note: Adapted from Journal of the American Academy of Child and Adolescent Psychiatry, volume 31, Caplan R, Guthrie D, Foy JG. Communication deficits and formal thought disorder in schizophrenic children, 151–159., copyright 1992, with permission from Elsevier.36
Cohesion
The same blinded rater coded transcriptions of the videotaped Story Game 17, with the modified Halliday and Hassan 37 analysis of cohesion (see Table 3 for examples). She coded the rate (frequency/number of utterances) of the following cohesion devices: Conjunction ties together contiguous clauses (sentences) by using additive, contrastive, causal, temporal, and continuative relationships. Referential cohesion involves use of a pronoun, demonstrative, definite article, or comparative to refer back to people or objects in the preceding spoken text. In unclear reference, the speaker uses a pronoun, demonstrative, definite article, or comparative to refer to a person or object that has not been previously mentioned in the spoken text, which can confuse the listener. Similarly, the listener becomes confused if the speaker makes an ambiguous reference by using a referent that can apply to more than one person or object. Because of the low base rate of unclear and ambiguous references, we combined these 2 scores for each subject, as in prior publications 6. Higher unclear/ambiguous reference scores are negative (reflecting unclear communication), whereas higher scores on measures of referential cohesion and conjunction are positive, indicating more linguistically complex speech.
Table 3.
Examples of linguistic cohesion
| Category | Type | Example |
|---|---|---|
| Referential Cohesion | Pronomial | A boy called Peter saw a ghost. He was scared. |
| Demonstrative |
The boy was crying and then this boy called his mother. |
|
| Comparative | I don’t like this story. I like the first one more. |
|
| Conjunction | Additive | The witch gets burned and that’s the end of the story. |
| Adversative | I don’t know how, but he makes me be bad, bad, bad. |
|
| Causal | I have nightmares because I ate too much candy before bed. |
|
| Temporal | I’ll go play when I’m done eating. | |
| Reference Patterns | Unclear | Uh, I went and looked at the guy to see what they were doing. |
| Ambiguousp | And-and – and so when Halloween came her dad made a hat and then her mother made a witch costume and she was happy. |
Note: Adapted from Journal of the American Academy of Child and Adolescent Psychiatry, volume 31, Caplan R, Guthrie D, Foy JG. Communication deficits and formal thought disorder in schizophrenic children, 151–159., copyright 1992, with permission from Elsevier.36
Psychological Testing
A neuropsychological examination was also administered at baseline by supervised clinical psychology doctoral students or PhD staff. IQ estimates (presented in Table 1) were derived from the Wechsler Abbreviated Intelligence Scale (WASI 43), administered as part of the test battery.
Data Analysis
SPSS for Macintosh (SPSS version 18.0; SPSS, Chicago, Illinois) was used for statistical analyses. One-way analysis of variance (ANOVA) and chi-squared tests were conducted to compare groups [clinical high-risk converters (CHR+), clinical high-risk non-converters (CHR−), and healthy comparison subjects)] on demographic variables. The mean Full Scale IQ, age and parental education level of the CHR group were not statistically different from healthy controls (all p >.10), so no covariates were included in group comparisons. FTD and cohesion scores were logarithmically transformed because of their skewed distribution. Significance tests were based on the transformed scores, but actual values are presented in this article. Statistical significance was set at P ≤ .05 by means of 2-tailed tests for all analyses. Scheffé correction was used to control the type I error rate for univariate analyses. Effect sizes were calculated with the partial eta-squared statistic, which provides a measure of effect size for group differences 44.
Analysis 1
To test whether the speech of CHR youth differed from that of healthy controls, we conducted 2 MANOVAs, one for the three FTD variables (illogical thinking, POC, and loose associations) and a separate MANOVA for cohesive deficits (conjunction, referential cohesion, unclear/ambiguous references), based on prior principal components analysis demonstrating that FTD and cohesion measures represent two independent components 6. Subsequent planned post-hoc comparisons between groups (CHR+, CHR−, controls) were performed using Scheffé correction for multiple comparisons.
Analysis 2
Multiple logistic regression models were used to examine the joint predictive value of baseline thought disorder and cohesion measures within the CHR group for determining subsequent conversion to psychosis. To create the most parsimonious models, predictive variables were selected with the backward elimination algorithm (Wald statistics). Initially, the full model contained all six FTD/cohesion variables regardless of whether there was a significant difference between groups in the descriptive statistics. Cohesion and FTD measures were included in the model if the variable showed an association (P < .10) and contributed to the overall fit of the model (P < .05). Then, variables were excluded step by step if they did not sufficiently contribute to the prediction of psychosis. The final model focused only on those variables that were significantly related to conversion to psychosis in the previous steps. Secondly, multiple regression models were used to examine continuous psychosocial outcome measures (Global Social and Role Functioning Scales), also using the backward elimination procedure.
Analysis 3
Because age plays a role in children's communication skills 2, 16, 17, 36, 39, we examined age effects on FTD and cohesion measures, using separate Spearman correlations within the CHR and control groups.
Finally, we conducted three sets of secondary analyses to examine additional factors that may have affected our findings. 1) We conducted MANOVA analyses within the CHR group (antipsychotics vs. no antipsychotics) to determine whether FTD and cohesion measures differed as a function of antipsychotic medication usage. 2) we re-ran MANOVAs described in Analysis 1, including only the CHR− subjects with 12 months or more of follow-up; 3) to examine specificity of language measures to schizophrenia outcome, we conducted exploratory analyses compared baseline FTD and cohesion measures for subjects who converted to a schizophrenia spectrum disorder (N=12) as compared to those who did not (N=9).
RESULTS
Baseline demographic and clinical data for the three groups (CHR+, CHR−, and comparison subjects) are shown in Table 1. Groups did not differ with regard to age, gender, race/ethnicity, parental education, or estimated IQ. In addition, at baseline the CHR patients who subsequently developed a psychotic disorder (CHR+) did not significantly differ from non-converters (CHR−) with regard to Global Assessment of Functioning (GAF) score, mean positive symptom severity, or medication usage.
Between-Group Thought Disorder Differences
Figures 1 and 2 present the mean FTD and cohesion scores (frequency/number of utterances) of the CHR+, CHR− and typically developing groups. Thought disorder measures have low values in both CHR and control groups. This is typical of studies of children and adolescents with schizophrenia, ADHD, autism, and typical development using the K-FTDS 38, 39, 45.
Figure 1.
Baseline formal thought disorder (FTD) measures in clinical high risk (CHR) youth who subsequently converted to psychosis (CHR+), CHR youth who did not convert to psychosis (CHR−), and typically developing controls. SE = standard error. *p<.05; **p<.01
Figure 2.
Linguistic cohesion measures in clinical high risk youth who subsequently converted to psychosis (CHR+), CHR youth who did not convert to psychosis (CHR−), and typically developing controls. *p<.05. SE = standard error.
MANOVA examining effects of diagnostic group on FTD variables indicated a significant overall effect of group (F(6, 192)=4.63, Wilks’s lambda=0.74, p<0.001). Univariate analyses indicated a significant main effect of group on illogical thinking (F(2,102)=7.32, p=.001; partial η2 =.143) and POC (F(2,102)=6.73, p=.002; partial η2 =.133). The group effect on loose association was not significant (F(2,102)=1.71, p=.19; partial η2 =.037) Post-hoc contrasts (CHR+ vs. CHR− vs. CTL) for FTD variables showing significant main effects revealed that there were no significant differences between controls and CHR− for any FTD variables (all p>.10). However, CHR+ showed significantly greater illogical thinking at baseline than both controls (p=.001) and non-converters (p=.014). CHR+ also showed significantly more POC in their speech at baseline than both controls (p<.001) and non-converters (p=.015).
MANOVA of cohesion variables indicated a significant main effect of diagnostic group (F (6,192)=2.36, Wilk’s lambda= .91, p≤.05; partial η2 =.06). Univariate analyses indicated this was largely accounted for by the effect of group on referential cohesion (F(2,102)=3.06, p≤.05). Post-hoc contrasts revealed that referential cohesion significantly differed between controls and converters (p=.029), but not between controls and non-converters (p=.19). The pair-wise difference between converters and nonconverters was not significant (p=.31). In addition, the group effect was not significant for conjunction and unknown references (p=.37 and .49, respectively).
Prediction of Outcome
Conversion to Psychosis: In the multiple logistic regression analysis using baseline FTD and cohesion variables to predict conversion to psychotic disorder over the follow-up period, only illogical thinking was significantly and uniquely associated with prediction of subsequent conversion (Wald =5.19 (1), p=.023, OR=4.64, 95%CI=1.24–17.41). Illogical thinking score correctly classified 69% of the CHR patients who converted and 71% of those who did not convert, for an overall predictive accuracy of 70.5%. Social and Role Functioning: Multiple regression analyses were used to predict follow-up social and role functioning (Global Social and Role function scores) based on baseline thought disorder/cohesion variables, while controlling for baseline social and role functioning, respectively.
The overall regression model providing the best fit for social functioning at follow-up included Global Social Functioning at baseline (partial R2=.27; standardized β =.494, t=3.67, p=.001; 95% CI=.209−.725) and POC (partial R2=.11; standardized β = −.28, t=−2.06, p=.047; 95%CI= −31.7− −.26). Together, these variables explained 36% of the variance in social functioning at follow-up (F(2,51)=11.833, p<.001).
The best fitting stepwise regression model predicting role function at Time 2 included total referential cohesion (partial R2=.13; standardized β =.29, t=2.144, p=.037, 95%CI=.10–3.179), along with Global Role Functioning at baseline (partial R2=.34; standardized β =.69, t=5.46, p<.001, 95%CI=.377−.82). Together, these variables explained 42% of the variance in role functioning at follow-up (F(2,51)=16.96, p<.001).
Developmental effects
Spearman correlations for cohesion variables were not significant in either the CHR or TD control group (all p>.20). Of the FTD variables, only loose associations showed a significant inverse correlation with age (Spearmans’ rho= −.31, p=.04) within the CHR group, indicating a decline in loose associations with increasing age. No age correlations reached significance in the control group for FTD variables (all p>.40).
Medication Effects
Within the CHR sample, there was no relationship between antipsychotic medication use at baseline and any FTD or cohesion measures (p-values for all comparisons >.20).
Secondary Analyses of Non-converters with One Year or More of Follow-up
MANOVA analyses were re-done including only those CHR− subjects with 12 months or more of followup (N=19), as compared to CHR+ (N=21) and healthy controls (N=51). Main effects for illogical thinking and POC remained significant. ILL: (F(2,88)=7.34, p=.001; partial η2 =.155), POC: (F(2,83)=6.51, p=.002; partial η2 =.14). Post-hoc contrasts indicated that CHR+ showed significantly greater illogical thinking at baseline than controls (p=.001), with a trend toward more illogical thinking vs. non-converters (p=.085). CHR+ also showed significantly more POC in their speech at baseline than both controls (p<.001) and non-converters (p=.028). Main effects for referential cohesion were attenuated to a trend level in the reduced sample (F(2,88)=2.63, p=.08), but the effect size was similar to that obtained in the full sample (partial η2 = =.06).
Multiple logistic regression analysis conducted in this subset of the sample also revealed a similar pattern of results. Illogical thinking remained as a unique predictor of subsequent conversion, although the effect was attenuated (Wald =3.1(1), p=.078, OR=3.86).
Specificity of Diagnostic Outcome
Follow-up analyses compared baseline FTD and linguistic cohesion measures in CHR+ with schizophrenia-spectrum outcomes (N=12) as compared to those with other psychotic disorder outcomes (N=9). Those with schizophrenia spectrum outcomes had higher scores at baseline on measures of poverty of content of speech (t=2.495; p=.03; η2 =.12), and significantly lower referential cohesion scores (t= −2.49; p=.026; ; η2=.31), as well as a trend toward less use of conjunctive devices (t= −1.7; p= 0.11; ; η2 =.19) relative to those with non-schizophrenia spectrum outcomes (affective psychosis or Psychosis NOS). While group differences for other FTD measures (illogical thinking and loose association were not statistically significant, these scores were higher in the group who converted to schizophrenia-spectrum disorders (effect sizes: η2 = .042 for illogical thinking and η2 = .022 for LA, respectively).
Discussion
To our knowledge, this is the first investigation of thought disorder and communication deviance in youth at clinical high risk for psychosis using an ecologically valid measure of natural language. Several novel findings were revealed: 1) these measures, particularly illogical thinking, POC, and referential cohesion, were able to distinguish putatively prodromal individuals who would subsequently convert to overt psychotic illness; 2) baseline POC and referential cohesion were also significant predictors of social and role functioning respectively, at follow-up; and 3) in contrast to our expectations, age effects were significantly related to loose association but not with other FTD and cohesion scores within this age range.
Despite the absence of fully psychotic symptoms, CHR individuals evidence signs of FTD (illogical thinking and POC) and communication disturbance (referential cohesion) that are qualitatively similar to the kinds of speech abnormalities observed in children and adolescents with schizophrenia 6, 39. Moreover, illogical thinking distinguished those at-risk youth who would subsequently convert to a full-blown psychotic disorder. Reduced referential cohesion indicates that the speech of CHR patients provided the listener with less information on who and what they were talking about, whereas elevated rates of illogical thinking indicate that CHR youth are impaired in their ability to organize their thoughts and present the listener with adequate reasoning. Increased POC of speech indicates a failure to elaborate on the topic of conversation, despite adequate speech production.
Nevertheless, there were some important distinctions between our findings and those previously reported in adolescents meeting criteria for childhood-onset schizophrenia (COS) 6. In particular, COS patients were additionally found to have significantly more loose associations (i.e., unexpected topic changes) and fewer conjunctive devices used to tie together ideas across sentences, and more unclear/ambiguous references than typically developing controls. As such, there appears to be a more pervasive pattern of communication deficit in individuals with overt illness; it is tempting to speculate that onset of illness during this critical developmental period may be particularly damaging to processes involved in normal development of the higher-level linguistic skills involved in discourse.
In addition, while qualitatively similar, the deficits we observed in CHR youth are, on average, less severe in magnitude than the FTD and cohesion deficits previously observed in adolescents with COS. The childhood-onset form of the illness is typically associated with elevated rates of language delay and linguistic deficits 46, relative to the more typical, later-onset form. To our knowledge, no published studies have yet applied these specific measures to adolescents or adults with later-onset illness. Nevertheless, the marked severity of FTD observed in patients with chronic schizophrenia, as rated by other measures 47–49, suggests that there may be some progression of increasing thought disorder and language deterioration that occurs with the onset of overt illness. Longitudinal studies are needed in order to directly address this question.
Our findings suggest that impaired use of reasoning (illogical thinking) and development of the topic (POC) when formulating and organizing thoughts (i.e., coherence) as well as under-utilization of linguistic devices necessary for cohesive communication are present prior to the onset of overt psychosis. Increased illogical thinking, POC, and reduced referential cohesion were present at baseline in CHR patients who subsequently converted to psychosis, relative to both typically developing controls and non-converters (CHR−). CHR+ youth showed no baseline differences from the CHR− group in terms of positive psychotic symptom severity, suggesting that these measures may be able to improve the prediction of onset of psychosis. In addition, in a multiple logistic regression analysis, illogical thinking was uniquely associated with prediction of subsequent conversion. The overall accuracy of baseline illogical thinking for prediction of conversion over the follow-up period was 70.5%, a marked increase relative to SIPS criteria alone (35%) 32. The predictive accuracy of this model is thus very comparable to that of multivariate clinical prediction algorithms previously identified by Cannon and colleagues 32 in a multi-site study. In particular, this study found that a combination of three baseline predictor variables -genetic risk for schizophrenia with recent functional decline, higher levels of unusual beliefs or suspiciousness, and greater social impairment - resulted in positive predictive power of 74−81%.
In addition to predicting subsequent conversion to a full-blown psychotic disorder, FTD and cohesion measures (POC and referential cohesion) were also significant predictors of social and role functioning, respectively, at follow-up, approximately one year later, even when controlling for baseline social and role functioning. Although baseline social and role functioning accounted for relatively more of the variance in outcome, discourse measures (POC and referential cohesion) remained significant in the models, indicating that these variables uniquely contributed to the prediction of social and role outcome, respectively, over and above what could be predicted by past functioning alone. These findings have important clinical implications, as they suggest that underutilization of discourse devices necessary for cohesive communication has prognostic significance for at-risk individuals. These findings intuitively make sense, given the critical importance of coherent and cohesive communication in social relationships with others, and in performance in work and school. In other clinical populations, these measures have been shown to have implications for school performance; for example, in children with epilepsy, under-use of cohesive devices was associated with parent reports of school problems and social competence on the Child Behavior Checklist (CBCL), as well as reduced academic achievement, even when controlling for IQ 50, 51. Additionally, cohesion skills are related to reading ability in typically developing and language-disordered children 52, 53. Although it cannot be determined whether such deficits are causally related to psychosocial functioning in our CHR sample, these findings suggest that treatments targeting communication skills may be helpful in improving functional outcome.
In addition, secondary analyses revealed some degree of specificity of our findings to outcomes of schizophrenia spectrum disorders. In particular, those with schizophrenia spectrum outcomes had significantly more poverty of content at baseline, and significantly less referential cohesion, as well as a trend toward less use of conjunctive devices relative to those with non-schizophrenia spectrum outcomes. Baseline illogical thinking and loose association scores were also higher, although not significantly so, in the group who converted to schizophrenia-spectrum disorders. These findings are in line with prior studies finding that severity of thought disorder is a stable trait in patients with schizophrenia, whereas language performance of manic patients is not temporally stable 15, 54. Although preliminary, our findings also suggest that adding measures of thought disorder to predictive algorithms used to ascertain those at clinical high risk may improve our ability to predict to specific diagnostic outcomes.
FTD has been conceptualized as a marker of executive control impairment 55, involving an inability to use situational context to guide goal-directed action across multiple domains, including language 56. It was beyond the scope of the present study to comprehensively investigate the association of FTD and cohesion measures with specific neurocognitive functions; however, it is important to note that our CHR group did not differ in IQ from the typically developing control group, and thus the observed thought and communication disturbance are not reflective of a generalized cognitive deficit.
In a previous study, Caplan et al. 2, 16 found that the age–related increases in language cohesion skills observed in typically developing children over the 9 to 13 year-old age range were not observed in children with schizophrenia, suggesting a failure to develop age-appropriate communication skills. The primary explanation for our failure to find age-associated changes in these measures in our typically developing sample is due to the fact that our study participants were older (12–21 years of age). Consistent with prior studies of COS, in which significantly more FTD was observed in younger COS children 6, we observed an age-associated decrease in loose associations within the CHR group. Age-related changes in this and other FTD measures may not have been observable within the control group due to the low base rate of FTD overall. Nevertheless, because age effects were assessed cross-sectionally here, we cannot rule out the possibility that more subtle changes in language and communication skills may take place over this age range, which could be detected with a prospective longitudinal design.
We previously reported the results of a functional neuroimaging study of language processing in a partially overlapping sample of CHR youth, in which we find that relative to controls, CHR participants showed increased neural activity in a network of language-associated brain regions, including the medial prefrontal cortex bilaterally, left inferior frontal gyrus and middle temporal gyri, and the anterior cingulate 57. In that study, we also found that increased baseline activity in language-related brain regions (the superior temporal gyrus, caudate, and left inferior frontal gyrus) distinguished those who subsequently developed psychosis. Baseline activation differences within the CHR group were predictive of severity of positive FTD - and with social outcome- at follow-up. Consistent with these findings, children with established illness (COS) were found to exhibit aberrant patterns of neural activity during semantic as well as syntactic processing; further, the degree of functional abnormality in language-associated brain networks was associated with severity of thought disorder. Thus, collectively these findings suggest that there may be a neurobiological basis to thought and communication disturbance that precedes illness onset, and is additionally predictive of subsequent outcome.
Other functional magnetic resonance imaging (fMRI) studies of language tasks in adult patients with established schizophrenia have found that FTD is associated with altered neural recruitment in the inferior prefrontal and temporal cortices; brain regions implicated in language production and cognitive control 58. As such, FTD in those at-risk for schizophrenia could be viewed as evidence of abnormal connectivity between frontal brain areas involved in context maintenance and “top down control” and posterior brain areas involved in language production and processing 59, 60.
Certain limitations of the present study should be noted. As with the vast majority of studies involving psychiatric populations, medication is a potential confound. In our study, several of the CHR participants were taking psychoactive medication, although only a minority (19.5%) were taking atypical antipsychotics. However, baseline medications did not differ between those who later converted and those who did not, and therefore could not account for group differences in baseline FTD and cohesion measures. In addition, there was no relationship between antipsychotic medication use and FTD and cohesion measures. Additionally, Borofsky and colleagues recently found no significant relationship between antipsychotic medication usage and thought disorder in childhood-onset schizophrenia patients 61. Nevertheless, we fully acknowledge that our study was not designed to examine differential effects of medications, and this could be better addressed in the context of a randomized clinical trial in which treatment is standardized.
In addition, a longer follow-up period would have been desirable, to ensure that our ‘non-converters’ were not incorrectly classified. However, Cannon et al. 32 previously found that the majority of conversions in clinical high-risk individuals occurred in the year following ascertainment, with a decelerating trend after that (i.e., the rate of conversion was 13% in the first 6 months, decreasing to 9% from 7 to 12 months, slowing to 5% per each 6-month epoch at 13 to 24 months, and then slowing again to 2.7% from 25 to 30 months). Moreover, secondary analyses including only the non-converting study participants with twelve months or more of follow-up yielded highly comparable results to those obtained on the full sample.
Here we investigated the contribution of thought and communication disturbance at a single timepoint to prediction of subsequent outcome; thus, these results do not address the question of relative stability of these deficits, and whether there is further deterioration in these measures with the onset of illness. Longitudinal data are needed in order to examine the effects of progression of illness on these indices.
Acknowledgments
Funding for this study was provided by National Alliance for Research on Schizophrenia and Depression Young Investigator Award (Maxine and Jack Zarrow Investigator Award to CEB), and National Institute of Mental Health grants K23MH74644 (CEB), MH65079 and NIMH P50 MH066286 (TDC), as well as donations from the Rutherford Charitable Foundation and Staglin Music Festival for Mental Health to the University of California, Los Angeles Foundation.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Disclosures: Dr. Cannon has served as a consultant to Rules-Based Medicine on serum-based assays for psychiatric disorders. Drs. Bearden, and Caplan, and Ms. Wu report no biomedical financial interests or potential conflicts of interest.
References
- 1.Kuperberg GR, West WC, Lakshmanan BM, Goff D. Functional magnetic resonance imaging reveals neuroanatomical dissociations during semantic integration in schizophrenia. Biol Psychiatry. 2008 Sep 1;64(5):407–418. doi: 10.1016/j.biopsych.2008.03.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Caplan R. Thought disorder in childhood. J Am Acad Child Adolesc Psychiatry. 1994 Jun;33(5):605–615. doi: 10.1097/00004583-199406000-00001. [DOI] [PubMed] [Google Scholar]
- 3.Andreasen N. Thought, language and communication disorders, I: clinical assessment, definition of terms, and evaluation of their reliability. Arch Gen Psychiatry. 1979;36:1315–1321. doi: 10.1001/archpsyc.1979.01780120045006. [DOI] [PubMed] [Google Scholar]
- 4.Norman RM, Malla AK, Cortese L, et al. Symptoms and cognition as predictors of community functioning: a prospective analysis. Am J Psychiatry. 1999 Mar;156(3):400–405. doi: 10.1176/ajp.156.3.400. [DOI] [PubMed] [Google Scholar]
- 5.Taylor MA, Reed R, Berenbaum S. Patterns of speech disorders in schizophrenia and mania. J Nerv Ment Dis. 1994 Jun;182(6):319–326. doi: 10.1097/00005053-199406000-00002. [DOI] [PubMed] [Google Scholar]
- 6.Caplan R, Guthrie D, Tang B, Komo S, Asarnow RF. Thought disorder in childhood schizophrenia: replication and update of concept. J Am Acad Child Adolesc Psychiatry. 2000 Jun;39(6):771–778. doi: 10.1097/00004583-200006000-00016. [DOI] [PubMed] [Google Scholar]
- 7.Singer MT, Wynne LC. Thought Disorder and Family Relations of Schizophrenics. Iv. Results and Implications. Arch Gen Psychiatry. 1965 Feb;12:201–212. doi: 10.1001/archpsyc.1965.01720320089010. [DOI] [PubMed] [Google Scholar]
- 8.Goldstein MJ. Family factors that antedate the onset of schizophrenia and related disorders: the results of a fifteen year prospective longitudinal study. Acta Psychiatr Scand Suppl. 1985;319:7–18. doi: 10.1111/j.1600-0447.1985.tb08520.x. [DOI] [PubMed] [Google Scholar]
- 9.Docherty NM. Linguistic reference performance in parents of schizophrenic patients. Psychiatry. 1995 Feb;58(1):20–27. doi: 10.1080/00332747.1995.11024708. [DOI] [PubMed] [Google Scholar]
- 10.Docherty NM. Cognitive impairments and disordered speech in schizophrenia: thought disorder, disorganization, and communication failure perspectives. J Abnorm Psychol. 2005 May;114(2):269–278. doi: 10.1037/0021-843X.114.2.269. [DOI] [PubMed] [Google Scholar]
- 11.Docherty NM. Expressed emotion and language disturbances in parents of stable schizophrenia patients. Schizophr Bull. 1995;21(3):411–418. doi: 10.1093/schbul/21.3.411. [DOI] [PubMed] [Google Scholar]
- 12.Docherty NM, Gordinier SW, Hall MJ, Dombrowski ME. Referential communication disturbances in the speech of nonschizophrenic siblings of schizophrenia patients. J Abnorm Psychol. 2004 Aug;113(3):399–405. doi: 10.1037/0021-843X.113.3.399. [DOI] [PubMed] [Google Scholar]
- 13.Docherty NM, Miller TN, Lewis MA. Communication disturbances in the natural speech of schizophrenic patients and non-schizophrenic parents of patients. Acta Psychiatr Scand. 1997 Jun;95(6):500–507. doi: 10.1111/j.1600-0447.1997.tb10138.x. [DOI] [PubMed] [Google Scholar]
- 14.Docherty NM, Gottesman II. A twin study of communication disturbances in schizophrenia. J Nerv Ment Dis. 2000 Jul;188(7):395–401. doi: 10.1097/00005053-200007000-00001. [DOI] [PubMed] [Google Scholar]
- 15.Levy DL, Coleman MJ, Sung H, et al. The Genetic Basis of Thought Disorder and Language and Communication Disturbances in Schizophrenia. J Neurolinguistics. 2010 May 1;23(3):176. doi: 10.1016/j.jneuroling.2009.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Caplan R, Foy JG, Asarnow RF, Sherman T. Information processing deficits of schizophrenic children with formal thought disorder. Psychiatry Res. 1990 Feb;31(2):169–177. doi: 10.1016/0165-1781(90)90119-p. [DOI] [PubMed] [Google Scholar]
- 17.Caplan R, Guthrie D, Fish B, Tanguay PE, David-Lando G. The Kiddie Formal Thought Disorder Rating Scale: clinical assessment, reliability, and validity. J Am Acad Child Adolesc Psychiatry. 1989 May;28(3):408–416. doi: 10.1097/00004583-198905000-00018. [DOI] [PubMed] [Google Scholar]
- 18.Arboleda C, Holzman PS. Thought disorder in children at risk for psychosis. Arch Gen Psychiatry. 1985 Oct;42(10):1004–1013. doi: 10.1001/archpsyc.1985.01790330084010. [DOI] [PubMed] [Google Scholar]
- 19.Miklowitz DJ, Velligan DI, Goldstein MJ, et al. Communication deviance in families of schizophrenic and manic patients. J Abnorm Psychol. 1991 May;100(2):163–173. doi: 10.1037//0021-843x.100.2.163. [DOI] [PubMed] [Google Scholar]
- 20.Cannon TD, Cornblatt B, McGorry P. The empirical status of the ultra high-risk (prodromal) research paradigm. Schizophr Bull. 2007 May;33(3):661–664. doi: 10.1093/schbul/sbm031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.McGorry PD, Yung AR, Phillips LJ. The "close-in" or ultra high-risk model: a safe and effective strategy for research and clinical intervention in prepsychotic mental disorder. Schizophr Bull. 2003;29(4):771–790. doi: 10.1093/oxfordjournals.schbul.a007046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yung AR, McGorry PD. The prodromal phase of first-episode psychosis: Past and current conceptualizations. Schizophrenia Bulletin. 1996;22(2):353–370. doi: 10.1093/schbul/22.2.353. [DOI] [PubMed] [Google Scholar]
- 23.Marshall M, Lewis S, Lockwood A, Drake R, Jones P, Croudace T. Association between duration of untreated psychosis and outcome in cohorts of first-episode patients: a systematic review. Arch Gen Psychiatry. 2005 Sep;62(9):975–983. doi: 10.1001/archpsyc.62.9.975. [DOI] [PubMed] [Google Scholar]
- 24.Cannon TD. Neurodevelopment and the transition from schizophrenia prodrome to schizophrenia: research imperatives. Biol Psychiatry. 2008 Nov 1;64(9):737–738. doi: 10.1016/j.biopsych.2008.07.027. [DOI] [PubMed] [Google Scholar]
- 25.McGorry PD, Nelson B, Amminger GP, et al. Intervention in individuals at ultra-high risk for psychosis: a review and future directions. J Clin Psychiatry. 2009 Sep;70(9):1206–1212. doi: 10.4088/JCP.08r04472. [DOI] [PubMed] [Google Scholar]
- 26.McGorry PD, Yung AR, Pantelis C, Hickie IB. A clinical trials agenda for testing interventions in earlier stages of psychotic disorders. Med J Aust. 2009 Feb 16;190(4 Suppl):S33–S36. doi: 10.5694/j.1326-5377.2009.tb02372.x. [DOI] [PubMed] [Google Scholar]
- 27.McGlashan T. Structured Interview for Prodromal Syndromes (SIPS) New Haven, Conn: Yale University; 2001. [Google Scholar]
- 28.First MB, Spitzer RL, Gibbon M, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders, Research Version, Patient Edition. New York: Biometrics Research Department, New York State Psychiatric Institute; 1996. [Google Scholar]
- 29.Kaufman J, Birmaher B, Brent D, et al. Schedule for Affective Disorders and Schizophrenia for School-Age Children-Present and Lifetime Version (K-SADS-PL): initial reliability and validity data. Journal of the American Academy of Child & Adolescent Psychiatry. 1997;36(7):980–988. doi: 10.1097/00004583-199707000-00021. [DOI] [PubMed] [Google Scholar]
- 30.Meyer SE, Bearden CE, Lux SR, et al. The psychosis prodrome in adolescent patients viewed through the lens of DSM-IV. J Child Adolesc Psychopharmacol. 2005 Jun;15(3):434–451. doi: 10.1089/cap.2005.15.434. [DOI] [PubMed] [Google Scholar]
- 31.Niendam TA, Bearden CE, Johnson JK, et al. Neurocognitive performance and functional disability in the psychosis prodrome. Schizophr Res. 2006 May;84(1):100–111. doi: 10.1016/j.schres.2006.02.005. [DOI] [PubMed] [Google Scholar]
- 32.Cannon TD, Cadenhead K, Cornblatt B, et al. Prediction of psychosis in youth at high clinical risk: a multisite longitudinal study in North America. Arch Gen Psychiatry. 2008 Jan;65(1):28–37. doi: 10.1001/archgenpsychiatry.2007.3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Auther A, Smith C, Cornblatt B. Global Functioning: Social Scale (GF: Social) Glen Oaks, NY: Zucker-Hillside Hospital; 2006. [Google Scholar]
- 34.Niendam T, Bearden C, Johnson J, Cannon T. Global Functioning: Role Scale (GF: Role) Los Angeles, CA: University of California, Los Angeles; 2006. [Google Scholar]
- 35.Cornblatt BA, Auther AM, Niendam T, et al. Preliminary findings for two new measures of social and role functioning in the prodromal phase of schizophrenia. Schizophr Bull. 2007 May;33(3):688–702. doi: 10.1093/schbul/sbm029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Caplan R, Guthrie D, Foy JG. Communication deficits and formal thought disorder in schizophrenic children. J Am Acad Child Adolesc Psychiatry. 1992 Jan;31(1):151–159. doi: 10.1097/00004583-199201000-00023. [DOI] [PubMed] [Google Scholar]
- 37.Halliday MAK, Hassan R. Cohesion in Spoken and Written English. London: Longman’s; 1976. [Google Scholar]
- 38.Solomon M, Ozonoff S, Carter C, Caplan R. Formal thought disorder and the autism spectrum: relationship with symptoms, executive control, and anxiety. J Autism Dev Disord. 2008 Sep;38(8):1474–1484. doi: 10.1007/s10803-007-0526-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Caplan R. Communication deficits in childhood schizophrenia spectrum disorders. Schizophr Bull. 1994;20(4):671–683. doi: 10.1093/schbul/20.4.671. [DOI] [PubMed] [Google Scholar]
- 40.Caplan R, Guthrie D, Tang B, Nuechterlein KH, Asarnow RE. Thought disorder in attention-deficit hyperactivity disorder. J Am Acad Child Adolesc Psychiatry. 2001 Aug;40(8):965–972. doi: 10.1097/00004583-200108000-00019. [DOI] [PubMed] [Google Scholar]
- 41.Caplan R, Arbelle S, Guthrie D, et al. Formal thought disorder and psychopathology in pediatric primary generalized and complex partial epilepsy. J Am Acad Child Adolesc Psychiatry. 1997 Sep;36(9):1286–1294. doi: 10.1097/00004583-199709000-00022. [DOI] [PubMed] [Google Scholar]
- 42.Caplan R, Guthrie D, Komo S, et al. Social communication in children with epilepsy. J Child Psychol Psychiatry. 2002 Feb;43(2):245–253. doi: 10.1111/1469-7610.00017. [DOI] [PubMed] [Google Scholar]
- 43.Wechsler D. Manual for the Wechsler Abbreviated Intelligence Scale (WASI) San Antonio, TX: The Psychological Corporation; 1999. [Google Scholar]
- 44.Kirk RE. Experimental design: Procedures for the behavioral sciences. 2nd ed. Belmont, CA: Brooks/Cole; 1982. [Google Scholar]
- 45.van der Gaag RJ, Caplan R, van Engeland H, Loman F, Buitelaar JK. A controlled study of formal thought disorder in children with autism and multiple complex developmental disorders. J Child Adolesc Psychopharmacol. 2005 Jun;15(3):465–476. doi: 10.1089/cap.2005.15.465. [DOI] [PubMed] [Google Scholar]
- 46.Nicolson R, Lenane M, Singaracharlu S, et al. Premorbid speech and language impairments in childhood-onset schizophrenia: association with risk factors. Am J Psychiatry. 2000 May;157(5):794–800. doi: 10.1176/appi.ajp.157.5.794. [DOI] [PubMed] [Google Scholar]
- 47.Kuperberg GR. Language in schizophrenia Part 1: an Introduction. Lang Linguist Compass. Aug;4(8):576–589. doi: 10.1111/j.1749-818X.2010.00216.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Makowski D, Waternaux C, Lajonchere CM, et al. Thought disorder in adolescent-onset schizophrenia. Schizophr Res. 1997 Feb 7;23(2):147–165. doi: 10.1016/s0920-9964(96)00097-7. [DOI] [PubMed] [Google Scholar]
- 49.Gordinier SW, Docherty NM. Factor analysis of the Communication Disturbances Index. Psychiatry Res. 2001 Feb 14;101(1):55–62. doi: 10.1016/s0165-1781(00)00239-0. [DOI] [PubMed] [Google Scholar]
- 50.Caplan R, Sagun J, Siddarth P, et al. Social competence in pediatric epilepsy: insights into underlying mechanisms. Epilepsy Behav. 2005 Mar;6(2):218–228. doi: 10.1016/j.yebeh.2004.11.020. [DOI] [PubMed] [Google Scholar]
- 51.Caplan R, Siddarth P, Bailey CE, et al. Thought disorder: A developmental disability in pediatric epilepsy. Epilepsy Behav. 2006 Jun;8(4):726–735. doi: 10.1016/j.yebeh.2006.03.009. [DOI] [PubMed] [Google Scholar]
- 52.Liles BZ. Production and comprehension of narrative discourse in normal and language disordered children. J Commun Disord. 1985 Dec;18(6):409–427. doi: 10.1016/0021-9924(85)90030-9. [DOI] [PubMed] [Google Scholar]
- 53.Norris JA, Bruning RH. Cohesion in the narratives of good and poor readers. J Speech Hear Disord. 1988 Nov;53(4):416–424. doi: 10.1044/jshd.5304.416. [DOI] [PubMed] [Google Scholar]
- 54.Docherty N, Schnur M, Harvey PD. Reference performance and positive and negative thought disorder: a follow-up study of manics and schizophrenics. J Abnorm Psychol. 1988 Nov;97(4):437–442. doi: 10.1037//0021-843x.97.4.437. [DOI] [PubMed] [Google Scholar]
- 55.Kerns JG, Berenbaum H. Cognitive impairments associated with formal thought disorder in people with schizophrenia. J Abnorm Psychol. 2002 May;111(2):211–224. [PubMed] [Google Scholar]
- 56.Cohen JD, Servan-Schreiber D. Context, cortex, and dopamine: a connectionist approach to behavior and biology in schizophrenia. Psychol Rev. 1992 Jan;99(1):45–77. doi: 10.1037/0033-295x.99.1.45. [DOI] [PubMed] [Google Scholar]
- 57.Sabb FW, van Erp TG, Hardt ME, et al. Language network dysfunction as a predictor of outcome in youth at clinical high risk for psychosis. Schizophr Res. 2010 Feb;116(2–3):173–183. doi: 10.1016/j.schres.2009.09.042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Kuperberg GR. Neural mechanisms of language comprehension: challenges to syntax. Brain Res. 2007 May 18;1146:23–49. doi: 10.1016/j.brainres.2006.12.063. [DOI] [PubMed] [Google Scholar]
- 59.Symond MP, Harris AW, Gordon E, Williams LM. "Gamma synchrony" in first-episode schizophrenia: a disorder of temporal connectivity? Am J Psychiatry. 2005 Mar;162(3):459–465. doi: 10.1176/appi.ajp.162.3.459. [DOI] [PubMed] [Google Scholar]
- 60.Kuperberg GR, Deckersbach T, Holt DJ, Goff D, West WC. Increased temporal and prefrontal activity in response to semantic associations in schizophrenia. Arch Gen Psychiatry. 2007 Feb;64(2):138–151. doi: 10.1001/archpsyc.64.2.138. [DOI] [PubMed] [Google Scholar]
- 61.Borofsky LA, McNealy K, Siddarth P, Wu K, Dapretto M, Caplan R. Language and Thought Disorder in Childhood Schizophrenia. Schizophr Bull. doi: 10.1016/j.jneuroling.2009.07.004. submitted. [DOI] [PMC free article] [PubMed] [Google Scholar]