Abstract
Purpose
Little is known about the relationship between severe obesity and depressive symptoms, particularly in community as opposed to clinic-based samples. This study determined the relationship of severe obesity and depressive symptoms over three years in a community-based sample of non–Hispanic black and white adolescents in grades 7–12 at baseline.
Methods
Nested matched cohort study using data from a longitudinal school-based study of youth followed for three years. 51 severely obese participants (BMI-for-age ≥ 99% and a BMI ≥ 40 at one or more study visit) were identified and paired with an age-, sex-, and race-matched normal weight subject. Depressive symptoms (CESD scale) were assessed at baseline, 2 and 3 years later. CESD score above cut points predictive of major depressive disorder or use of antidepressant medication defined High Depressive Symptoms (HDS).
Results
Pairs were 73% non-Hispanic black, 67% female. There was no relationship between weight status and HDS at any assessment point. However, a positive association between weight status and CESD scores, while not present at baseline or 2 years, emerged at 3 years (p=0.02). This relationship was present only among non-Hispanic whites (p=0.006 whites, p=0.25 blacks) and did not differ by sex.
Conclusions
Severely obese youth in this community sample did not have increased likelihood of high levels of depressive symptoms. However, significantly increased depressive symptoms among non-Hispanic white youth at the end of the follow up period suggests that this racial/ethnic group may be particularly vulnerable to the psychological effects of obesity in late adolescence/early adulthood.
Keywords: obesity, depression, adolescence, race/ethnicity
Background
Obesity is a public health problem today. Rates of obesity in children and youth have risen among all age groups, racial/ethnic groups, and both sexes. The increasing prevalence of obesity has led to mounting concerns of parallel increases in its sequelae. Most studies of the sequelae of pediatric obesity have centered on physiological outcomes, such as cardiovascular risk factor levels and type 2 diabetes. Fewer have focused on psychological consequences, which may be more common among youth. For example, it is estimated that up to 20% of young people will experience major depressive disorder at some time during the adolescent years[1]. Concern for the psychological health of obese children and adolescents, particularly relative to depression and self esteem is cited as an important impetus for obesity treatment. The inherent assumption is that weight loss will improve affect by decreasing the shame, stigma, and negative self concept associated with obesity[2].
Despite these assumptions, the nature and direction of the relationship between obesity and depression in adolescence is unclear. Results of cross sectional and longitudinal studies are conflicting, some supporting an association between obesity and depressed mood while others suggest no association exists[3–9]. Those that support an association differ on the direction of the relationship[4, 6, 10–11]. Several studies suggest the relationship between obesity and depression is stronger among females and weaker or absent among males[3, 7, 9, 12] while others suggest that the relationship is present among males but not females[13]. There is also some indication that race/ethnicity influences the nature and direction of the relationship[5, 14]. Further, little is known about the relationship among youth with severe obesity. Severely obese adolescents are a vulnerable group who are highly likely to stay obese into adulthood. This persistent severe obesity increases risk for diabetes, cardiovascular disease, non-alcoholic fatty liver disease, and other related morbidities. Rates of severe obesity have tripled in the past 25 years; the derth of data about this population represents a critical gap in the literature[15]. Studies of health-related quality of life (HRQOL) among obese adolescents indicate that these young people have lower functioning in many HRQOL domains, particularly among severely obese adolescents[16–17]. From these data, many extrapolate that severely obese adolescents will have higher levels of depressive symptoms and poorer overall psychological health.
A major limitation of the studies of severe obesity and psychological health in children and adolescents is that these studies tend to use data from clinic-based, rather than community-based samples[18]. This distinction is critical, inasmuch as the active engagement in obesity treatment signals that weight status is dysphoric for clinic-based cohorts; this dysphoria may not be present among non-treatment seeking adolescents. Even among studies of clinic-based samples, there is lack of consistency amongst the findings vis-à-vis the association of obesity to depressive symptoms. A recent study by Zeller and colleagues of adolescents seeking treatment for bariatric surgery demonstrated that depressive symptoms are typically mild in this population[19]. However, depressive symptoms have also been shown to be higher amongst severely obese adolescents seeking bariatric surgery compared to a similarly obese comparison group, although this difference disappeared after approximately 5 months but still prior to surgery [20]
The objective of the current study was to assess the relationship of severe obesity to depressive symptoms using data from an ongoing school-based cohort of adolescents followed for three years. Using a nested matched study design, we explored whether depressive symptomatology differed between severely obese and normal weight adolescents and if these relationships were moderated by race/ethnicity and sex.
Methods
Data for this nested matched cohort study were drawn from a school-based longitudinal cohort study which began in the 2001–2002 academic year (Year 0) for students in grades 5–12 and included follow up for three years, through the 2004–2005 school year (Year 3)[21]. All study procedures were approved by the IRBs of participating institutions. Students 18 years of age or older gave written informed consent to participate. Those under 18 years of age gave assent and a parent provided written informed consent. The cohort was 94% Non-Hispanic black and white. Therefore, data for this study were restricted to these two racial/ethnic groups. At each wave of data collection, all participants had a physical exam and those in grades 7 and higher also received a survey which included assessment of depressive symptoms.
At baseline, there were 1646 eligible non-Hispanic black and white adolescents in grade 7 or higher, 72% of whom (N=1186) were seen again in Year 3. These 1186 adolescents provided the cohort from which the matched pairs were drawn. Severely obese adolescents were defined as those with a baseline BMI-for-age >= 99% and a BMI >= 40 at least once during the follow up period [15]. These adolescents were matched with a normal weight study participant, defined as those with a BMI-for-age < 85% and >5% [22]. Matching variables included baseline age (+/− 3 months), sex, and race/ethnicity.
Fifty-seven severely obese adolescents (5%) were identified, 93% (N=53) also provided information on depressive symptoms at Year 3. We found age-, sex-, and race/ethnicity-matched normal weight adolescents with information available on depressive symptoms for 51 of these severely obese adolescents. These 51 matched pairs were used as the analytic sample for the present study. The pairs were 66.7% female (N=34) and 72.5% (N=37) non-Hispanic black. Mean baseline age was 15.2 +/−1.5 years (range 12.8 – 18.7). Mean length of follow up was 2.7+/− 0.2yrs.
Measures
Weight status
Trained staff measured height and weight on students wearing indoor clothing with shoes removed and pockets empty. Each was measured twice, height using a portable stadiometer (RoadRod model, Quick Medical, North Bend, Washington) and weight using a digital scale (SECA 770, Hanover, MD). If measurements differed by a preset amount (0.3 kg and 0.5 cm, respectively) a third measurement was made. The mean of each set was used in analyses. BMI was calculated as kg/m2 and BMI percentiles and z scores determined using data from CDC growth charts[23].
Psychotropic Medication History
Participants were asked to list current medications at each annual study visit. From these, a variable indicating psychotropic medications used in the treatment of depressive or anxiety disorders was developed.
Depressive Symptoms
Depressive symptoms was assessed with the Centers for Epidemiological Study-Depression (CESD) Scale. The CESD is a 20-item scale with a possible range 0–60 [24]. It has been widely used among adults and adolescents to assess depressive symtomatology and as a marker for depression[5, 25]. To accomplish the latter, a dichotomous variable was created to represent High Depressive Symptoms (HDS) based on validated cut points for CESD score which maximizes the sensitivity and specificity for predicting major depressive disorder. For adolescents, these cut points are 22 for males and 24 for females[26]. Further, subjects were coded as having HDS regardless of CESD score if they indicated treatment with antidepressant medication. Because the cut points for HDS are lower in adults and half of the pairs were above age 18 years at Year 3, we also performed analyses with the adult cut point of 16 for this year. Results did not change, so only analyses with the adolescent-specific cut points are presented herein.
Analyses
Analyses were designed to assess whether depressive symptomatology differs between normal weight and severely obese adolescents at baseline and then two years (Year 2) and 3 years later (Year 3). We chose these three points in time rather than simply the changes between years 1 and 4 to take into account the natural history of changes in depressive symptoms during adolescence. Studies have shown that the natural history of depressive symptoms is to rise in mid-adolescence and then fall in late adolescence and early adulthood, the period of time this cohort describes [27]. Therefore, we hypothesized, that depressive symptoms in both groups would rise over the first two years and then decline in the following year, leading to an overall decrease in depressive symptoms between baseline and the Year 3 visit.
We used McNemar’s Test to test for differences in the presence of high depressive symptoms between severely obese and normal weight adolescents at each of the three time points. For McNemar’s test, only pairs with discordant status contribute to significance testing; pairs for whom both exposed and unexposed have the same outcome status (both depressed or both not depressed) do not contribute. We also analyzed depressive symptoms (CESD scores) as a continuous variable to assess if there were associations with psychological distress along the entire gradient of symptoms, rather than just at the pathological end of the spectrum. For the analyses of CESD scores, we excluded five pairs of subjects in which a member of the pair was taking antidepressant medication(s) at the time of one of the study visits. Because CES-D scores were not normally distributed and the data were matched, Wilcoxon Signed Rank tests were used to assess differences in depressive symptoms across the matched pairs. Within-person changes over time were also assessed using the Wilcoxon Signed Rank test. These analyses were stratified by weight status. An alpha level of p<0.05 was set a priori.
Results
Differences in BMI between severely obese and normal weight adolescents were clear. Mean BMI for the severely obese group was 42.3 at Year 0, 45.3 at Year 2 and 45.4 at Year 3. For the normal weight group, mean BMI was 19.9 at Year 0, 20.9 at Year 2 and 21.1 at Year 3. More than half (55%) of the severely obese adolescents had BMI>40 throughout the follow up period. Of note, one severely obese black female became overweight between years 2 and 3. Her CESD scores remained low throughout: 12 at baseline, 9 at Year 2, and 12 at Year 3. She did not report antidepressant medications at any wave. Five, all female, indicated treatment with psychotropic medication during the study period. Four took a single psychotropic medications; the remaining participant reported multiple psychotropic medications each year. Medications used included amitriptyline atomoxetine HCl, escitalopram oxalate, methylphenidate and sertraline. Three of these girls were severely obese (two white, one black). Two subjects were normal weight non-Hispanic black girls.
Association of Weight Status to High Depressive Symptoms
Table 1 provides information on the depressive symptomatology among the 51 age-, race-, and sex-matched pairs. At baseline, nearly one in ten severely obese and normal weight adolescents had HDS. The prevalence more than doubled in Year 2 in both severely obese and normal weight adolescents and then fell in Year 3 to less than 10%. Regardless of these changes in prevalence, there were no significant differences in the prevalence of HDS between severely obese and normal weight adolescents at any of the three time points. At baseline, there were equal numbers of discordant pairs in which the severely obese adolescents had HDS but normal weight adolescents did not and in which the normal weight adolescents had HDS but the severely obese adolescents did not. Although the prevalence of HDS increased at Year 2, it went up similarly within the pairs. At Year 3, there was the greatest degree of discordancer. However, this difference did not reach statistical significance. Post hoc testing did not suggest moderation by race/ethnicity or sex.
Table 1.
Depressive Symptom of 51 Age-, Race-, and Sex-matched Pairs of Severely Obese and Normal Weight Youth+
| Severely Obese | Normal weight | ||||||||
|---|---|---|---|---|---|---|---|---|---|
| High Depressive Symptoms | N | % | N Discordant | N | % | N Discordant | P value¶ | ||
| Year 0 | 5 | 9.8 | 5 | 5 | 9.8 | 5 | 1.00 | ||
| Year 2 | 14 | 27.5 | 9 | 13 | 25.5 | 8 | 1.00 | ||
| Year 3 | 4 | 7.8 | 4 | 1 | 2.0 | 1 | 0.38 | ||
| CESD* | Mean | SD | Min | Max | Mean | SD | Min | Max | P valueψ |
| Year 0 | 14.0 | 6.5 | 0 | 28 | 11.9 | 5.6 | 3 | 28 | 0.10 |
| Year 2 | 18.1 | 10.4 | 5 | 44 | 14.2 | 9.0 | 2 | 31 | 0.08 |
| Year 3 | 9.5 | 7.9 | 2 | 46 | 6.3 | 5.0 | 0 | 27 | 0.02 |
+ 67% of the pairs (N=34) were female and 72.5% (N=37) non-Hispanic black
p value derived from McNemar’s test which is based on discordant pairs.
Includes only data from the 46 pairs where neither subject was on antidepressant medication
p value derived from Wilcoxon Signed Rank test of severely obese and normal weight age, race and sex matched pairs
Association of Weight Status to Depressive Symptoms
As hypothesized, CESD scores had an inverted U-shaped trajectory over the 3 years. In the entire cohort of matched pairs, CESD scores rose significantly between Years 0 and 2 (p=0.047) and fell significantly between Years 2 and 3 (p<0.001). On average, CESD scores were higher in the severely obese group at each time point (Table 1). These differences were not significant at Year 0 or Year 2 but were statistically significant at Year 3 .
Analysis of the changes in CESD scores suggested that a greater rise in depressive symptom scores among severely obese adolescents between Years 0 and 2 drove the emergence of the difference in symptoms we observed at Year 3 (Table 2). CESD scores did not rise significantly from Years 0 to 2 for either normal weight or severely obese subjects. However, the differences were significant in the paired analysis; the change was significantly higher for the severely obese than normal weight adolescents. This was not the case for the within-person change in CESD scores between Years 2 and 3. CESD scores dropped significantly for both weight status strata in this interval, but the paired analysis showed that the change was not different for normal weight and severely obese adolescents .
Table 2.
Changes in CESD Scores Over Three Years
| Mean | SD | Median | Min | Max | P within person change in CESD* |
P change in CESD across pairsψ |
|
|---|---|---|---|---|---|---|---|
| Change from Year 0 to Year 2 | |||||||
| Severely Obese | 3.9 | 11.3 | 2.5 | −16 | 28 | 0.07 | 0.024 |
| Normal Weight | 2.2 | 8.0 | 2.4 | −12 | 21 | 0.10 | |
| Change from Year 2 to Year 3 | |||||||
| Severely Obese | −8.5 | 9.8 | −6.5 | −38 | 10 | <0.001 | 0.79 |
| Normal Weight | −7.8 | 8.2 | −6.0 | −23 | 5 | <0.001 | |
p value derived from Wilcoxon Signed Rank test comparing within person change across Years.
p value derived from Wilcoxon Signed Rank test of severely obese and normal weight age, race and sex matched pairs
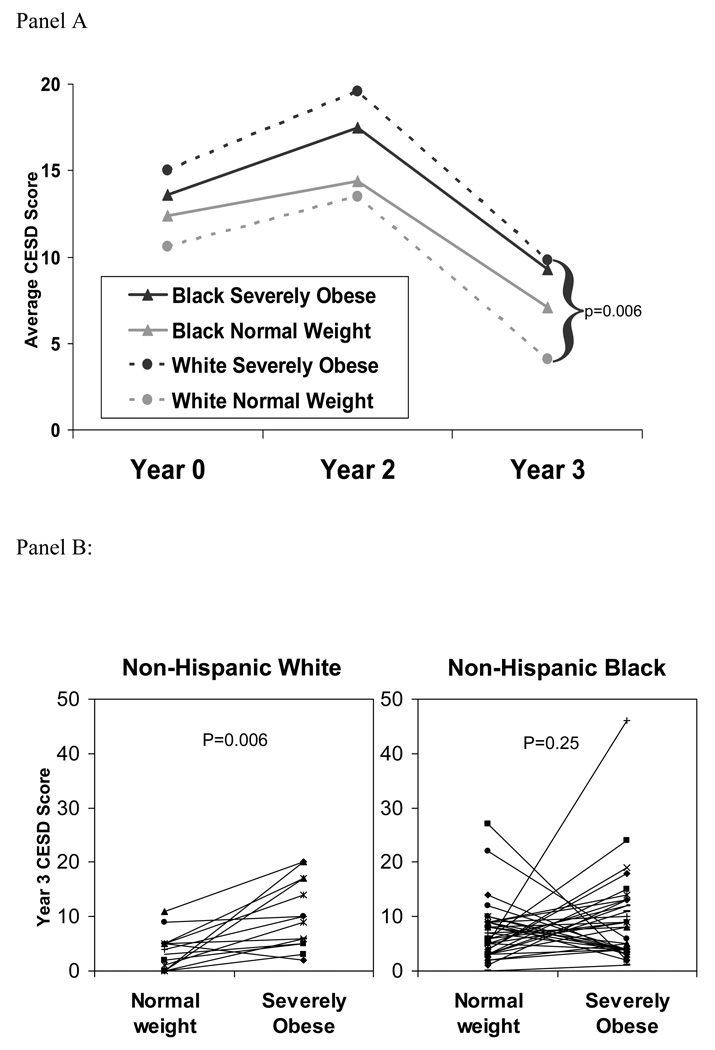
Stratified post-hoc analyses indicated that the relationship between weight status and depressive symptoms was moderated by race but not sex (Table 3, Figure 1). CESD scores were higher for severely obese white adolescents compared to their normal weight peers at Year 3 (Figure 1). There were no other statistically significant differences in post-hoc testing.
Table 3.
Post hoc Testing for Moderation of the Relationship between Severe Obesity and Depressive Symptoms by Race and Sex
| Severely Obese | Normal weight | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| CESD | Mean | SD | Median | Min | Max | Mean | SD | Median | Min | Max | P value* |
| Black (N=34 pairs) | |||||||||||
| Year 0 | 13.6 | 6.5 | 14.0 | 0 | 28 | 12.4 | 5.2 | 12.0 | 3 | 22 | 0.34 |
| Year 2 | 17.5 | 10.4 | 14.5 | 5 | 42 | 14.4 | 9.3 | 12.0 | 2 | 31 | 0.32 |
| Year 3 | 9.3 | 8.4 | 7 | 2 | 46 | 7.1 | 5.3 | 6.0 | 1 | 27 | 0.25 |
| White (N=12 pairs) | |||||||||||
| Year 0 | 15.0 | 6.9 | 12.5 | 8 | 28 | 10.6 | 6.4 | 8.7 | 5 | 28 | 0.13 |
| Year 2 | 19.6 | 10.7 | 17.5 | 7 | 44 | 13.5 | 8.2 | 12.5 | 4 | 30 | 0.08 |
| Year 3 | 9.8 | 6.4 | 8.0 | 2 | 20 | 4.1 | 3.4 | 4.5 | 0 | 11 | 0.006 |
| Girls (N=29 pairs) | |||||||||||
| Year 0 | 14.1 | 6.8 | 14.1 | 0 | 28 | 12.4 | 5.2 | 12.0 | 4 | 28 | 0.26 |
| Year 2 | 17.9 | 9.9 | 17.0 | 5 | 42 | 14.4 | 8.7 | 13.0 | 2 | 31 | 0.19 |
| Year 3 | 9.0 | 6.3 | 6.0 | 2 | 24 | 6.5 | 4.3 | 6.0 | 0 | 22 | 0.14 |
| Boys (N=17 pairs) | |||||||||||
| Year 0 | 13.8 | 6.2 | 14.0 | 4 | 28 | 11.2 | 6.2 | 9.0 | 3 | 22 | 0.22 |
| Year 2 | 18.4 | 11.6 | 15.0 | 6 | 44 | 13.8 | 9.7 | 11.0 | 4 | 31 | 0.31 |
| Year 3 | 10.2 | 10.2 | 9.0 | 2 | 46 | 6.0 | 6.2 | 5.0 | 0 | 27 | 0.07 |
p value derived from Wilcoxon Signed Rank test of pair-wise differences in severely obese and normal weight age-, race-, and sex- matched pairs
Figure 1.
Moderation of the Relationship between CESD Scores and Severe Obesity by Race/Ethnicity. Panel A: Average CESD Scores stratified by weight status and race/ethnicity. The only significant relationship between severe obesity and depressive symptoms is at Year 3 among non-Hispanic whites. Panel B: Paired Year 3 CESD Scores stratified by race/ethnicity.
Discussion
This nested matched cohort study of a biracial sample of adolescents reveals a complex relationship between severe obesity and depressive symptoms as adolescents age. No association was observed between severe obesity and a high level of depressive symptoms suggestive of major depressive disorder either cross-sectionally or prospectively after two or three years of follow-up. When viewed as a continuum, however, depressive symptoms were higher on average among severely obese adolescents than those of their matched controls at each time point. These differences reached statistical significance after 3 years of follow-up. Although the association of severe obesity and depressive symptoms did not differ by sex, this association was moderated by race; the relationship was apparent only among non-Hispanic white pairs despite the smaller number of non-Hispanic white as compared to non-Hispanic black pairs in the study.
These data suggest that the rise in depressive symptom scores among non–Hispanic white severely obese adolescents between Years 0 and 2 drove the emergence of the difference in symptoms we observed. Population-based data indicate that depressive symptoms tend to rise in both males and females over adolescence and then fall, with a peak between ages 15 and 18 years of age [27–28]. In our matched sample, we observed this general pattern for both the categorical high depressive symptom variable and for depressive symptoms score. The fact that statistically significant differences between severely obese and normal weight adolescents were only observed for symptoms scores, and not for a categorical variable reflective of risk for major depressive disorder suggest that, in adolescence, severe obesity may not be associated with increased risk for major depressive disorder despite increased psychological distress among severely obese adolescents, particularly non-Hispanic white adolescents. Whether increased distress in late adolescence increases risk for development of major depressive disorder amongst severely obese adolescents later in life remains to be established.
The high prevalence of both obesity and depression in adolescence has fueled a spate of studies designed to assess the strength and direction of the associations between these two conditions. Studying the link between obesity and depression in adolescence and young adulthood holds several challenges, however. First, because studies are often conducted among clinical samples of obese adolescents[18, 29], and therefore are likely to include individuals whose weight is interfering with their psychosocial functioning, associations with depression or depressive symptoms are likely to greater than would be found in the general population. Population-based studies, on the other hand, have not typically focused on adolescents who were severely obese, perhaps due to limited numbers. Additionally, evidence exists which suggests that psychological disorders, including depression, influence the trajectory of BMI[4, 6, 30]. A final challenge is the role of psychotropic medications, many of which influence both weight status and, by design, depressive symptomatology[31]. A strength of this study was the collection of information regarding psychotropic medication use. The pattern of BMI among the five subjects in the present study who were taking psychotropic medication, provided no evidence of medication effects on weight gain.
Few studies have evaluated differences by race in the association of obesity and depression in adolescence, and most of these are cross-sectional[5, 14, 32]. Latent trajectory analysis of the National Longitudinal Study of Adolescent Health indicated that blacks had higher levels of depressive symptoms compared whites at age 16, and that the trajectories moved in parallel over ~6 years of follow-up, remaining different as levels declined[32]. This large sample also identified sex differences; higher depression scores were observed among black and white females. Although sex disparities in social sequelae of obesity in adolescence have been prospectively demonstrated for self-esteem [33], and cross-sectionally for popularity [34] and depressive symptoms[5], these studies have not focused on the extreme definition of obesity used in the current study. At these higher levels of overweight the internalization of negative self concept associated with obesity may be similar for males and females. Similar to our findings here, there are also data to suggest that weight status may have less impact on self esteem among non-Hispanic black than among non-Hispanic white overweight children[2]. There is also evidence that health –related quality of life is better amongst non-Hispanic black compared to non-Hispanic white severely obese adolescents [35].
Our study had several noteworthy limitations. First, this study assessed depressive symptomatology rather than diagnostic interviews to establish the presence of Major Depressive Disorder. High depressive symptoms and depressive symptoms scores by CESD show strong correlations with diagnostic interviews across a range of populations[36]. Second, information was not available for covariates that could act as confounders of the observed relationships, including history of prior depression, and family history of any mood disorder. Additionally, a matched cohort design limits the number of variables one can match on; we elected to match on age, sex, and race, but not on other potential confounders such as socioeconomic status and smoking. We did not assess whether subjects sought treatment for their obesity over the three years of the study. Finally, our power was limited, despite the matched design, with a sample size comprising 51 matched pairs, or 102 subjects. This is particularly relevant for the HDS analyses, as categorical variables often require larger sample sizes to achieve the same level of power as for analysis of a continuous variable, such as depressive symptoms.
Several strengths of the current effort also bear highlighting. Our data derive from a large community-based biracial cohort with broad socioeconomic variation, excellent follow-up and measured heights and weights and information on psychotropic medication use. We used a validated, well established measure of depressive symptoms. Further, the age range over which we monitored depressive symptoms represents a critical developmental period in the natural history of mood disorders. Last, the size of the parent study enabled us to identify a relatively large number (N=51) of severely obese adolescents from a community based sample. This number was consistent with national data as there were 133 severely obese adolescents identified in NHANES 1999–2004 with a BMI> 40 from a sample of 6849 12–19 year olds[15].
Conclusions
This nested matched study from a community based cohort provides evidence that that the relationship between severity of obesity and depressive symptoms in adolescence is not a simple, direct association. We found that there was no difference in the prevalence of high depressive symptoms suggestive of major depressive disorder between normal weight and severely obese adolescents. These findings suggest that prior clinic-based studies which identify this association may have had problems with selection bias. These data also suggest that obesity-related programs should not assume severely obese adolescents are suffering from a high degree of psychological distress. However, higher depressive symptoms in non-Hispanic white severely obese adolescents after three years indicates that, for this group, late adolescence may be a period of increased vulnerability to psychological effects of obesity. These differential effects may be mediated by cultural norms and social environmental factors, and merit further study.
Acknowledgment
The authors would like to thank Minghua Chen, MD, MPH, for assistance with data analysis.
Funding Sources: Supported by NIH grants HD041527, DK59183, DL46200 and the Richard Saltonstall Fund.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Screening and treatment for major depressive disorder in children and adolescents: US Preventive Services Task Force Recommendation Statement. Pediatrics. 2009 Apr;123(4):1223–1228. doi: 10.1542/peds.2008-2381. [DOI] [PubMed] [Google Scholar]
- 2.Strauss RS, Pollack HA. Social marginalization of overweight children. Arch Pediatr Adolesc Med. 2003 Aug;157(8):746–752. doi: 10.1001/archpedi.157.8.746. [DOI] [PubMed] [Google Scholar]
- 3.Atlantis E, Baker M. Obesity effects on depression: systematic review of epidemiological studies. Int J Obes (Lond) 2008 Jun;32(6):881–891. doi: 10.1038/ijo.2008.54. [DOI] [PubMed] [Google Scholar]
- 4.Anderson SE, Cohen P, Naumova EN, et al. Association of depression and anxiety disorders with weight change in a prospective community-based study of children followed up into adulthood. Arch Pediatr Adolesc Med. 2006 Mar;160(3):285–291. doi: 10.1001/archpedi.160.3.285. [DOI] [PubMed] [Google Scholar]
- 5.Wardle J, Williamson S, Johnson F, et al. Depression in adolescent obesity: cultural moderators of the association between obesity and depressive symptoms. Int J Obes (Lond) 2006 Apr;30(4):634–643. doi: 10.1038/sj.ijo.0803142. [DOI] [PubMed] [Google Scholar]
- 6.Goodman E, Whitaker RC. A prospective study of the role of depression in the development and persistence of adolescent obesity. Pediatrics. 2002;110(3):497–504. doi: 10.1542/peds.110.3.497. [DOI] [PubMed] [Google Scholar]
- 7.Anderson SE, Cohen P, Naumova EN, et al. Adolescent obesity and risk for subsequent major depressive disorder and anxiety disorder: prospective evidence. Psychosom Med. 2007 Nov;69(8):740–747. doi: 10.1097/PSY.0b013e31815580b4. [DOI] [PubMed] [Google Scholar]
- 8.Sjoberg RL, Nilsson KW, Leppert J. Obesity, Shame, and Depression in School-Aged Children: A Population-Based Study. Pediatrics. 2005;116(3):e389–e392. doi: 10.1542/peds.2005-0170. [DOI] [PubMed] [Google Scholar]
- 9.Liem ET, Sauer PJJ, Oldehinkel AJ, et al. Association Between Depressive Symptoms in Childhood and Adolescence and Overweight in Later Life: Review of the Recent Literature. Archives of Pediatrics Adolescent Medicine. 2008;162(10):981–988. doi: 10.1001/archpedi.162.10.981. [DOI] [PubMed] [Google Scholar]
- 10.Ball K, Burton NW, Brown WJ. A prospective study of overweight, physical activity, and depressive symptoms in young women. Obesity (Silver Spring) 2009 Jan;17(1):66–71. doi: 10.1038/oby.2008.497. [DOI] [PubMed] [Google Scholar]
- 11.Merten MJ, Wickrama KAS, Williams AL. Adolescent obesity and young adult psychosocial outcomes: Gender and racial differences. Journal of Youth and Adolescence. 2008 Oct;37(9):1111–1122. [Google Scholar]
- 12.Wardle J, Williamson S, Johnson F, et al. Depression in adolescent obesity: cultural moderators of the association between obesity and depressive symptoms. International Journal of Obesity. 2006 Apr;30(4):634–643. doi: 10.1038/sj.ijo.0803142. [DOI] [PubMed] [Google Scholar]
- 13.Mustillo S, Worthman C, Erkanli A, et al. Obesity and psychiatric disorder: developmental trajectories. Pediatrics. 2003 Apr;111(4 Pt 1):851–859. doi: 10.1542/peds.111.4.851. [DOI] [PubMed] [Google Scholar]
- 14.BeLue R, Francis LA, Colaco B. Mental health problems and overweight in a nationally representative sample of adolescents: effects of race and ethnicity. Pediatrics. 2009 Feb;123(2):697–702. doi: 10.1542/peds.2008-0687. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Skelton JA, Cook SR, Auinger P, et al. Prevalence and trends of severe obesity among US children and adolescents. Acad Pediatr. 2009 Sep–Oct;9(5):322–329. doi: 10.1016/j.acap.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Zeller MH, Modi AC. Predictors of health-related quality of life in obese youth. Obesity (Silver Spring, Md. 2006 Jan;14(1):122–130. doi: 10.1038/oby.2006.15. [DOI] [PubMed] [Google Scholar]
- 17.Schwimmer JB, Burwinkle TM, Varni JW. Health-related quality of life of severely obese children and adolescents. JAMA. 2003 Apr 9;289(14):1813–1819. doi: 10.1001/jama.289.14.1813. [DOI] [PubMed] [Google Scholar]
- 18.Britz B, Siegfried W, Ziegler A, et al. Rates of psychiatric disorders in a clinical study group of adolescents with extreme obesity and in obese adolescents ascertained via a population based study. Int J Obes Relat Metab Disord. 2000 Dec;24(12):1707–1714. doi: 10.1038/sj.ijo.0801449. [DOI] [PubMed] [Google Scholar]
- 19.Zeller MH, Modi AC, Noll JG, et al. Psychosocial functioning improves following adolescent bariatric surgery. Obesity (Silver Spring) 2009 May;17(5):985–990. doi: 10.1038/oby.2008.644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ratcliff MB, Reiter-Purtill J, Inge TH, et al. Changes in depressive symptoms among adolescent bariatric candidates from preoperative psychological evaluation to immediately before surgery. Surg Obes Relat Dis. 2010 Jun 4; doi: 10.1016/j.soard.2010.05.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goodman E, Huang B, Schafer-Kalkhoff T, et al. Perceived socioeconomic status: a new type of identity that influences adolescents' self-rated health. J Adolesc Health. 2007 Nov;41(5):479–487. doi: 10.1016/j.jadohealth.2007.05.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Barlow SE. Expert committee recommendations regarding the prevention, assessment, and treatment of child and adolescent overweight and obesity: summary report. Pediatrics. 2007 Dec;120 Suppl 4:S164–S192. doi: 10.1542/peds.2007-2329C. [DOI] [PubMed] [Google Scholar]
- 23.National Center for Health Statistics. [cited 2001 July 2];CDC Growth Charts: United States. 2001 Available from: http://www.cdc.gov/nchs/about/major/nhanes/growthcharts/datafiles.htm.
- 24.Radloff L. The CES-D scale: a self report depression scale for research in the general population. Applied Psychological Measurement. 1977;1(3):385–401. [Google Scholar]
- 25.Swallen KC, Reither EN, Haas SA, et al. Overweight, obesity, and health-related quality of life among adolescents: the National Longitudinal Study of Adolescent Health. Pediatrics. 2005 Feb;115(2):340–347. doi: 10.1542/peds.2004-0678. [DOI] [PubMed] [Google Scholar]
- 26.Roberts RE, Lewinsohn PM, Seeley JR. Screening for adolescent depression: a comparison of depression scales. J Amer Acad Child Adol Psychiatry. 1991;30(1):58–66. doi: 10.1097/00004583-199101000-00009. [DOI] [PubMed] [Google Scholar]
- 27.Costello DM, Swendsen J, Rose JS, et al. Risk and protective factors associated with trajectories of depressed mood from adolescence to early adulthood. Journal of consulting and clinical psychology. 2008 Apr;76(2):173–183. doi: 10.1037/0022-006X.76.2.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hankin BL, Abramson LY, Moffitt TE, et al. Development of depression from preadolescence to young adulthood: emerging gender differences in a 10-year longitudinal study. Journal of Abnormal Psychology. 1998 Feb;107(1):128–140. doi: 10.1037//0021-843x.107.1.128. [DOI] [PubMed] [Google Scholar]
- 29.Fitzgibbon ML, Stolley MR, Kirschenbaum DS. Obese people who seek treatment have different characteristics than those who do not seek treatment. Health Psychology. 1993 Sep;12(5):342–345. doi: 10.1037//0278-6133.12.5.342. [DOI] [PubMed] [Google Scholar]
- 30.Needham BL, Epel ES, Adler NE, et al. Trajectories of Change in Obesity and Symptoms of Depression: The CARDIA Study. Am J Public Health. 2010 June 1;100(6):1040–1046. doi: 10.2105/AJPH.2009.172809. 2010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Herva A, Laitinen J, Miettunen J, et al. Obesity and depression: results from the longitudinal Northern Finland 1966 Birth Cohort Study. International Journal of Obesity. 2006 Mar;30(3):520–527. doi: 10.1038/sj.ijo.0803174. [DOI] [PubMed] [Google Scholar]
- 32.Brown JS, Meadows SO, Elder GH., Jr Race-ethnic inequality and psychological distress: depressive symptoms from adolescence to young adulthood. Dev Psychol. 2007 Nov;43(6):1295–1311. doi: 10.1037/0012-1649.43.6.1295. [DOI] [PubMed] [Google Scholar]
- 33.Strauss RS. Childhood obesity and self-esteem. Pediatrics. 2000;105(1):e15. doi: 10.1542/peds.105.1.e15. [DOI] [PubMed] [Google Scholar]
- 34.Strauss RS, Pollack HA. Social marginalization of overweight adolescents. Archives of Pediatrics & Adolescent Medicine. 2003;157:746–752. doi: 10.1001/archpedi.157.8.746. [DOI] [PubMed] [Google Scholar]
- 35.Modi AC, Loux TJ, Bell SK, et al. Weight-specific health-related quality of life in adolescents with extreme obesity. Obesity (Silver Spring) 2008 Oct;16(10):2266–2271. doi: 10.1038/oby.2008.347. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hales DP, Dishman RK, Motl RW, et al. Factorial validity and invariance of the center for epidemiologic studies depression (CES-D) scale in a sample of black and white adolescent girls. Ethnicity & Disease. 2006;16(1):1–8. [PubMed] [Google Scholar]