Abstract
We report the case of a 6-year-old female with ACTH-independent Cushing syndrome secondary to bilateral adrenal nodular hyperplasia, who presented with hypertension and seizures, and was found have MRI changes consistent with posterior reversible encephalopathy syndrome (PRES). The patient received anti-hypertensive medication and a bilateral adrenalectomy was performed. One month later, resolution of her brain MRI changes were seen. This is the first case described in the literature of a patient with Cushing syndrome and PRES. We review the link between hypertension and Cushing syndrome, along with the pathophysiology of PRES and emphasize the importance of early recognition and treatment of hypertension in pediatric patients with Cushing syndrome to avoid possible cerebrovascular complications that may be related to a hypertensive event.
Keywords: Cushing syndrome, hypertension, adrenal tumors, hyperplasia
Introduction
Hypertension is common among children with Cushing syndrome [1, 2]. Antihypertensive treatment is not often prescribed to these patients and available agents are only partially effective [3]. Serious hypertension-related cerebral events, although rare, may occur in pediatric patients with Cushing syndrome. We recently reported the case of a child with multiple cerebral infarctions and Cushing disease who was hypertensive surrounding the time of his transsphenoidal surgery [4]. Here we report the first case of a patient with Cushing syndrome associated with posterior reversible encephalopathy syndrome (PRES).
PRES is a clinicoradiographic syndrome characterized by headache, altered mental functioning, visual loss and seizures [5]. Neuroimaging findings show reversible vasogenic subcortical edema without infarction and corresponding white-matter abnormalities on computed tomography (CT) and magnetic resonance imaging (MRI) [6]. Although PRES has not been reported in children and adolescents with Cushing syndrome, it has been seen with other conditions associated with hypertension, such as eclampsia, hydrocephalus, renal dysfunction, systemic lupus erythematosus, as well as with chemotherapy and immuno-suppressive drugs [7–12].
Case report
A 6 year old African American female presented with 4 month history of rapid weight gain and decreased energy level. Review of her growth chart revealed deceleration of her linear growth from the 50% to the 10% between the ages of 4 and 6. Clinical examination revealed classic stigmata of Cushing syndrome such as obesity, short stature, plethoric face and posterior cervical fat pad. Body mass index was increased at 23 (>97%); she had Tanner III pubic hair, and significant for age hypertension with mean blood pressure of 131/76. Laboratory evaluation confirmed hypercortisolism, with an elevated urinary free cortisol of 689 mcg/24 hours and lack of diurnal variation of serum cortisol values (8 AM cortisol of 39.4 mcg/dL and midnight cortisol of 47.3 mcg/dL). CT showed bilateral hypertrophy of the adrenal glands, while brain and pituitary MRI at that time were normal. High dose dexamethasone suppression test showed a “paradoxical” increase in urinary cortisol in response to exogenous steroid administration, consistent with what is seen in the context of corticotrophin (ACTH)-independent micronodular adrenal disease (MAD) or primary pigmented nodular adrenocortical disease (PPNAD) [13].
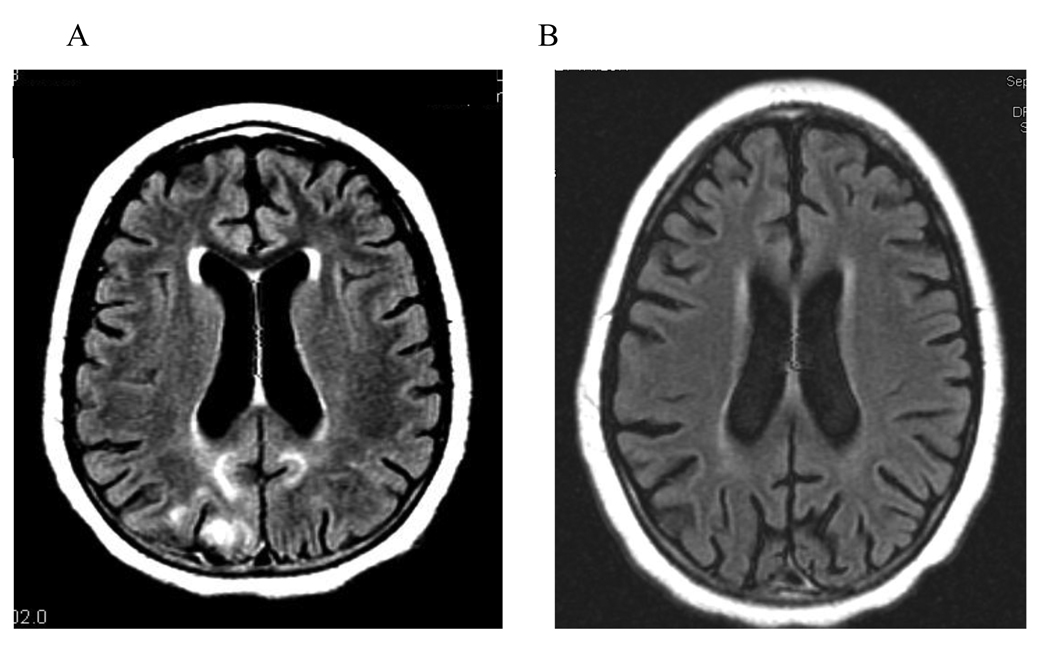
Almost two months after her initial evaluation, she presented to the emergency department with a new-onset seizure and hypertension. The patient was found to have MRI changes consistent with posterior encephalopathy (fig 1A). Her blood pressure was controlled with propranolol and hydrochlorathiazide. The patient underwent bilateral adrenalectomy; histology confirmed MAD.
Figure 1.
A. Brain MRI with multiple bilateral posterior white matter to white-gray matter lesions consistent with hypertensive encephalopathy. No corresponding abnormalities were present on diffusion weighted sequences to suggest infarcts (not shown). B. Follow up MRI one month later reveals resolution of lesions
Her hypertension largely resolved post-operatively. Resolution of her brain MRI changes followed a month later (fig 1B). Pathology was consistent with micronodular adrenocortical hyperplasia. The patient was not found to have mutations of the gene encoding the protein kinase A type I-alpha regulatory subunit (PRKAR1A) that is mutated in Carney complex (CNC) and can be associated with PPNAD; she also had no evidence of cardiac myxomas on echocardiogram, excluding therefore the possibility that her brain lesions were infarcts of the type that have been reported before in association with heart tumors and/or CNC [14].
Discussion
Hypertension has been reported in up to 50% of pediatric patients with Cushing syndrome [1, 2]. The pathogenesis of glucocorticoid-induced hypertension is not completely understood. It is thought to be related to both mineralocorticoid excess, as well as to effects of cortisol on the peripheral vasculature [15]. A hypertensive episode may serve as a trigger for PRES; in the largest clinical series of patients with PRES, hypertension was determined to be the etiology of PRES in 68% of patients [6]. In cases of PRES associated with hypertension, increased blood pressure is thought to cause hyperperfusion with resultant vasogenic edema and endothelial damage [16]. Prompt initiation of antihypertensive therapy may lead to reversal of the clinical and radiographic abnormalities of PRES [16]. Delay in diagnosis and therapy can result in permanent cerebral damage to affected patients with posterior encephalopathy [17, 18].
This is the first report linking PRES to Cushing syndrome. Hypertension induced by excessive hypercortisolism was likely a major contributor to the development of PRES in our patient. Early recognition of PRES as a potential complication of Cushing syndrome and appropriate treatment of hypertension in these patients may avoid long-term neurologic deficits.
Acknowledgement
This work was supported by the NICHD, NIH intramural program
References
- 1.Magiakou MA, Mastorakos G, Oldfield EH, Gomez MT, Doppman JL, Cutler GB, Jr, Nieman LK, Chrousos GP. Cushing's syndrome in children and adolescents, presentation, diagnosis, and therapy. N Engl J Med. 1994;331:629–636. doi: 10.1056/NEJM199409083311002. [DOI] [PubMed] [Google Scholar]
- 2.Magiakou MA, Mastorakos G, Zachman K, Chrousos GP. Blood pressure in children and adolescents with Cushing's syndrome before and after surgical care. J Clin Endocrinol Metab. 1997;82:1734–1738. doi: 10.1210/jcem.82.6.3985. [DOI] [PubMed] [Google Scholar]
- 3.Baid S, Nieman LK. Glucocorticoid excess and hypertension. Curr Hypertens Rep. 2004;6:493–499. doi: 10.1007/s11906-004-0046-0. [DOI] [PubMed] [Google Scholar]
- 4.Nguyen JH, Lodish MB, Patronas NJ, Ugrasbul F, Keil MF, Roberts M, Popovic J, Stratakis CA. Extensive ischemic infarctions in a prepubertal child with hypertension and Cushing disease. J Clin Endocrinol Metab. 2009;94:1–2. doi: 10.1210/jc.2008-1346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hinchey J, Chaves C, Appignani B, et al. A reversible posterior leukoencephalopathy syndrome. N Engl J Med. 1996;334:494–500. doi: 10.1056/NEJM199602223340803. [DOI] [PubMed] [Google Scholar]
- 6.Lee VH, Wijdicks EF, Manno EM, Rabinstein AA. Clinical spectrum of reversible posterior leukoencephalopathy syndrome. Arch Neurol. 2008;65:205–210. doi: 10.1001/archneurol.2007.46. [DOI] [PubMed] [Google Scholar]
- 7.Schaefer PW, Buonanno FS, Gonzalez RG, Schwamm LH. Diffusion-weighted imaging discriminates between cytotoxic and vasogenic edema in a patient with eclampsia. Stroke. 1997;28:1082–1085. doi: 10.1161/01.str.28.5.1082. [DOI] [PubMed] [Google Scholar]
- 8.Singhal AB. Postpartum angiopathy with reversible posterior leukoencephalopathy. Arch Neurol. 2004;61:411–416. doi: 10.1001/archneur.61.3.411. [DOI] [PubMed] [Google Scholar]
- 9.Lin KL, Hsu WC, Wang HS, Lui TN. Hypertension-induced cerebellar encephalopathy and hydrocephalus in a male. Pediatr Neurol. 2006;34:72–75. doi: 10.1016/j.pediatrneurol.2005.07.005. [DOI] [PubMed] [Google Scholar]
- 10.Yokobori S, Yokota H, Yamamoto Y. Pediatric posterior reversible leukoencephalopathy syndrome and NSAID-induced acute tubular interstitial nephritis. Pediatr Neurol. 2006;34:245–247. doi: 10.1016/j.pediatrneurol.2005.07.012. [DOI] [PubMed] [Google Scholar]
- 11.Zhang YX, Liu JR, Ding MP, Huang J, Zhang M, Jansen O, Deuschl G, Eschenfelder CC. Reversible posterior encephalopathy syndrome in systemic lupus erythematosus and lupus nephritis. Intern Med. 2008;47:867–875. doi: 10.2169/internalmedicine.47.0741. [DOI] [PubMed] [Google Scholar]
- 12.Govindarajan R, Adusumilli J, Baxter DL, et al. Reversible posterior leukoencephalopathy syndrome induced by RAF kinase inhibitor BAY 43-9006. J Clin Oncol. 2006;24:e48. doi: 10.1200/JCO.2006.08.4608. [DOI] [PubMed] [Google Scholar]
- 13.Bourdeau I, Lacroix A, Schürch W, Caron P, Antakly T, Stratakis CA. Primary pigmented nodular adrenocortical disease: paradoxical responses of cortisol secretion to dexamethasone occur in vitro and are associated with increased expression of the glucocorticoid receptor. J Clin Endocrinol Metab. 2003;88:3931–3937. doi: 10.1210/jc.2002-022001. [DOI] [PubMed] [Google Scholar]
- 14.Conroy S, Jenkins D, Stratakis C, Wassif WS, Cooper J. Atrial myxoma: a cardiocutaneous syndrome. Hosp Med. 2004;65:56–57. doi: 10.12968/hosp.2004.65.1.2423. [DOI] [PubMed] [Google Scholar]
- 15.Sacerdote A, Weiss K, Tran T, Rokeya Noor B, McFarlane SI. Hypertension in patients with Cushing's disease: pathophysiology, diagnosis, and management. Curr Hypertens Rep. 2005;7:212–218. doi: 10.1007/s11906-005-0013-4. [DOI] [PubMed] [Google Scholar]
- 16.Servillo G, Bifulco F, De Robertis E, Piazza O, Striano P, Tortora F, Striano S, Tufano R. Posterior reversible encephalopathy syndrome in intensive care medicine. Intensive Care Med. 2007;33:230–236. doi: 10.1007/s00134-006-0459-0. [DOI] [PubMed] [Google Scholar]
- 17.Kwon S, Koo J, Lee S. Clinical spectrum of reversible posterior leukoencephalopathy syndrome. Pediatr Neurol. 24:361–364. doi: 10.1016/s0887-8994(01)00265-x. [DOI] [PubMed] [Google Scholar]
- 18.Antunes NL, Small TN, George D, Boulad F, Lis E. Posterior leukoencephalopathy syndrome may not be reversible. Pediatr Neurol. 1999;20:241–243. doi: 10.1016/s0887-8994(98)00148-9. [DOI] [PubMed] [Google Scholar]