Abstract
Whether the metabolic syndrome (MetS) has prognostic value for coronary artery disease (CAD) beyond its individual components is controversial. We compared the relationship between the number of MetS components and CAD severity as assessed by angiography in non-diabetic and diabetic subjects. We consecutively enrolled 527 patients who underwent their first coronary angiography. Patients were divided into four groups according to the number of MetS components: 0/1, 2, 3, and 4/5. A coronary atherosclerosis score was used to quantify the extent of atherosclerotic involvement. The relationship between the MetS score and angiographic CAD severity or clinical presentation was compared between non-diabetic and diabetic subjects. Individuals with the MetS (n = 327) had a higher prevalence of CAD (60% vs 32%, P < 0.001), multi-vessel disease (34% vs 16%, P < 0.001), and acute coronary syndromes (49% vs 26%, P < 0.001) than those without the MetS. In the non-diabetic group, atherosclerosis score increased with the MetS score (1.0 ± 2.1, 2.0 ± 2.9, 2.8 ± 2.9, and 3.6 ± 3.9, P < 0.001) whereas there was no significant difference in the diabetic group (0.5 ± 1.0, 5.2 ± 4.7, 4.2 ± 2.9, and 4.4 ± 3.5, P = 0.102). The MetS score is related to CAD severity in non-diabetic patients but the association between the MetS score and angiographic CAD severity may be obscured in the presence of diabetes.
Keywords: Metabolic Syndrome, Coronary Atherosclerosis, Coronary Angiography
INTRODUCTION
The metabolic syndrome (MetS) is characterized by visceral adiposity, insulin resistance, dyslipidemia and increased blood pressure. It is not a single disease but a cluster of risk factors for atherosclerotic coronary artery disease (CAD) (1, 2). Consequently, the MetS has come to the fore as a major risk factor of CAD (3, 4). Isomaa et al. (5) reported that patients with the MetS had a higher incidence of CAD and increased all-cause mortality than those without it, but other researchers failed to verify these relationships (6, 7). Thus, unlike diabetes mellitus, which is a well-known established risk factor for CAD (8, 9), whether MetS has an additive impact on the development of CAD in addition to its individual components (e.g., hypertension, diabetes) is controversial (10). Conversely, it has been reported that the summation of the constituents of the MetS, the MetS score, is related to a higher incidence of CAD (11, 12).
The authors reported previously that epicardial fat measured by echocardiodraphy is related to the extent of coronary atherosclerosis in patients undergoing their first coronary angiography (13). From the data, we evaluated the relationship between the MetS score and CAD severity as assessed by angiography according to the presence of diabetes. Whether the MetS predicts angiographic CAD beyond well-established risk factors for CAD was also investigated.
MATERIALS AND METHODS
Study population
We collected clinical, biochemical, and angiographic information for 527 consecutive patients aged > 18 yr (267 males; mean age, 58.4 ± 10.8 yr) who underwent their first coronary angiography due to chest pain between January 2005 and October 2005 at Ajou University Medical Center. The medical records of all patients were reviewed. Patients were excluded if they had a history of percutaneous coronary intervention, coronary artery bypass graft, acute ST-segment elevation myocardial infarction, active inflammation, heart failure, chronic kidney disease, severe liver disease or cancer.
Anthropometric measurements such as the body mass index (BMI), waist circumference and hip circumference were collected. Plasma lipid profiles and levels of C-reactive protein (CRP), fibrinogen, uric acid and cardiac enzymes were measured. The homeostasis model assessment of insulin resistance (HOMA-IR) was calculated in non-diabetic patients using fasting plasma insulin concentrations and glucose concentrations as previously described (14). Patients with more than three of five criteria based on the updated guidelines issued by the Adult Treatment Panel (ATP III) of the National Cholesterol Education Program were considered to have the MetS. Central obesity was considered to be present if the waist circumference was > 90 cm in men and > 80 cm in women; these are the threshold values for Asian populations (15, 16). The MetS score was defined as the number of MetS components present.
Angiographic studies
On quantitative analyses of coronary angiograms (Quantcor QCA, version 4.0; Pie Medical Imaging, Maastricht, The Netherlands), the presence of stenosis ≥ 50% in diameter of major epicardial vessels was defined as CAD. The extent of CAD was quantified using the number of vessels with ≥ 50% stenosis and a coronary atherosclerosis score as follows (17). The coronary artery tree was divided into nine segments: left main coronary artery; proximal, mid-, and distal left anterior descending artery; proximal circumflex artery (including the first obtuse marginal branch); circumflex artery distal to the first marginal branch; proximal and mid-right coronary artery; posterior descending artery. Each of these segments was scored from 0 to 3 depending on the most severe stenosis according the following system: 0 = normal; 1 = stenosis of 1%-49%; 2 = stenosis of 50%-99%; and 3 = total occlusion. A coronary atherosclerosis score was generated as the sum of the scores in all segments.
Statistical analyses
SPSS version 17.0 (SPSS Incorporated, Chicago, IL, USA) was used for statistical analyses. Continuous variables were expressed as mean and standard deviation, and categorical variables as number and percentage. Comparisons of differences in anthropometric and biochemical values, and frequencies of CAD risk factors, CAD, and multi-vessel disease according to the presence of the MetS were undertaken using the Student's t-test and chi-squared test. Correlations of the MetS score with various clinical and biochemical parameters were examined by the Spearman's rank correlation analysis. Using one-way analysis of variance, the relationship between the MetS score and the extent of coronary atherosclerosis was explored in diabetic and non-diabetic subjects. A set of well-recognized risk factors for CAD (age; history of hyperlipidemia, hypertension, and diabetes; family history of early atherosclerotic CAD; current smoking; and elevated levels of CRP ≥ 1 mg/L) were included in a logistic regression model of angiographic CAD (1, 17). The presence of the MetS was then added to this model to determine if there was an additional predictive value. Statistical significance was considered at P < 0.05.
Ethics statement
The study protocol was approved by the institutional review board of Ajou University Medical Center (Suwon, Korea, IRB approval number: 4-2005-013-0). All patients provided written informed consent to be included in the study.
RESULTS
Baseline characteristics
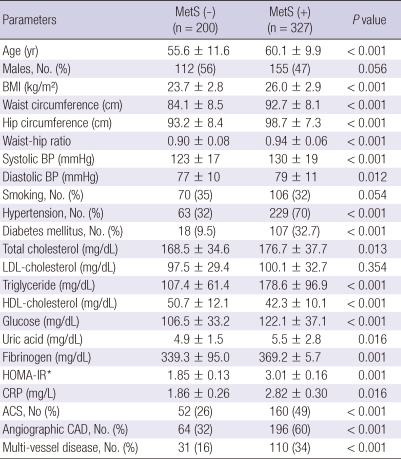
A summary of anthropometric, biochemical, and clinical characteristics according to the presence of the MetS is shown in Table 1. A total of 327 (62%) patients had the MetS, and 447 (85%) patients had more than two components of the MetS. The mean MetS score was 2.8 ± 1.3. Among patients with the MetS, an elevated fasting glucose level (85.6%) was the most frequent component followed by high blood pressure (85.3%), waist circumference (77.7%), high-density lipoprotein (HDL) cholesterol (61.2%) and triglyceride (TG; 56.3%). The HOMA-IR of non-diabetic patients (n = 402) was elevated in those with the MetS. The level of CRP was higher in those with the MetS. No difference was found in the level of low-density lipoprotein (LDL) cholesterol between the two groups.
Table 1.
Clinical characteristics and laboratory data according to the presence or absence of the metabolic syndrome (MetS)
Data are expressed as mean ± standard deviation (SD) or frequency (%). All variables were analyzed using Student's t-test and chi-squared test. *The homeostasis model assessment of insulin resistance (HOMA-IR) was calculated only for non-diabetic patients (n = 402). ACS, acute coronary syndrome; BMI, body mass index; BP, blood pressure; CAD, coronary artery disease; HDL; high-density lipoprotein; LDL, low-density lipoprotein.
Relationship between the MetS score and anthropometric, biochemical and angiographical variables
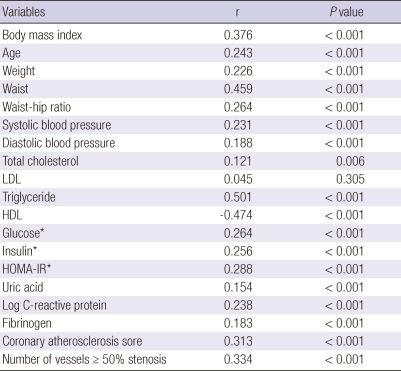
Spearman's rank correlation analysis showed that the MetS score was positively associated with age, weight, waist circumference, blood pressure, the HOMA-IR, as well as levels of total cholesterol (TC), TG, glucose, insulin, uric acid, CRP and fibrinogen, and negatively associated with the HDL-cholesterol level (Table 2). There was no association between the MetS score and LDL-cholesterol level. The degree of correlation between the MetS score and TG level was highest, followed by that with HDL cholesterol, waist circumference, BMI, and HOMA-IR.
Table 2.
Correlation of the metabolic syndrome (MetS) score with anthropometric, biochemical and angiographical variables
Correlations of the MetS score with various clinical and biochemical parameters were examined by the Spearman's rank correlation analysis. *Correlation of metabolic syndrome score with fasting insulin, glucose concentrations and homeostasis model assessment of insulin resistance (HOMA-IR) was analyzed only in non-diabetic patients (n = 402). HDL, high-density lipoprotein; LDL, low-density lipoprotein.
Relationship between the MetS score and severity of coronary atherosclerosis according to the presence of diabetes
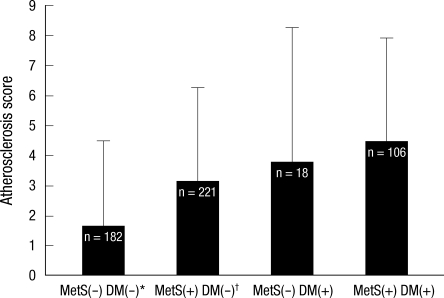
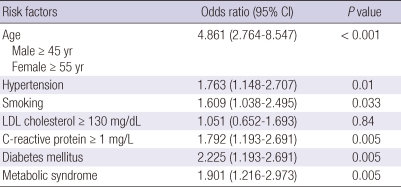
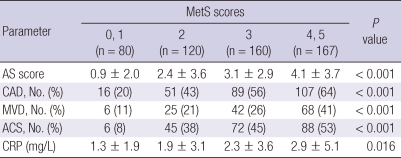
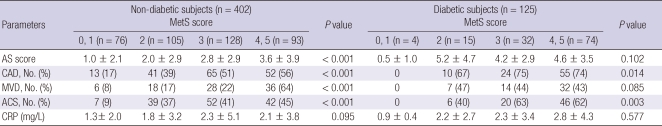
A total of 195 of 260 CAD patients (75%) had the MetS. The frequency of CAD and multi-vessel disease was higher in patients with the MetS compared with those without it (60% vs 32%, P < 0.001; 34% vs 16%, P < 0.001, respectively). Participants with at least two components of the MetS who did not meet the criteria for the definition of the MetS had a higher frequency of angiographic CAD (55% vs 16%, P < 0.001) and multi-vessel disease (30% vs 8%, P < 0.001) and a greater atherosclerosis score (3.3 ± 3.4 vs 1.0 ± 2.0, P < 0.001) in comparison with those with less than one MetS component. Patients with the MetS and diabetes had the highest coronary atherosclerosis score, followed by diabetic patients without the MetS, the MetS without diabetes, and patients with neither diabetes nor the MetS (4.5 ± 3.3, 3.8 ± 4.3, 3.1 ± 3.4, and 1.6 ± 2.8, respectively) (Fig. 1). On multiple logistic regression analysis, the MetS was independently associated with angiographic CAD (Table 3). In the overall population, the frequency of CAD, multi-vessel disease, coronary atherosclerosis score, and CRP level increased with MetS score (Table 4). These relationships persisted in non-diabetic individuals, whereas no relationship was found between the MetS score and coronary angiographic atherosclerosis in diabetic patients (Table 5).
Fig. 1.
Coronary atherosclerosis score according to the presence of the metabolic syndrome (MetS) or diabetes mellitus (DM). *vs MetS(+)DM(-), MetS(+)DM(+), P < 0.001, vs MetS(-)DM(+), P = 0.035; †vs MetS(+)DM(+), P = 0.002.
Table 3.
Multiple logistic analyses of risk factors for coronary artery disease including the metabolic syndrome for angiographic coronary artery disease
All variables were analyzed using multiple logistic analysis. LDL, low-density lipoprotein; CI, confidence interval.
Table 4.
Extent and clinical presentation of coronary artery disease (CAD) in relation to metabolic syndrome (MetS) scores
Data are expressed as mean ± standard deviation (SD) or frequency (%). All variables were analyzed using one-way analysis of variance and chi-squared test. ACS, acute coronary syndrome; AS, atherosclerosis; CRP, C-reactive protein; MVD, multi-vessel disease.
Table 5.
Relationship between the metabolic syndrome (MetS) score and the angiographic severity of coronary artery disease (CAD) and to disease activity dependent upon the presence of diabetes
Data are expressed as mean ± standard deviation (SD) or frequency (%). Using one-way analysis of variance and chi-squared test, the relationship between the MetS score and the extent of coronary atherosclerosis was explored in diabetic and non-diabetic subjects. ACS, acute coronary syndrome; AS, atherosclerosis; CRP, C-reactive protein, MVD, multi-vessel disease.
Relationship between the MetS and disease activity
As the MetS score increased, so did the frequency of acute coronary syndromes and CRP level (Table 4). Patients presenting with ACS (n = 212) had higher MetS scores compared with those with atypical chest pain or stable angina (3.3 ± 1.0 vs 2.6 ± 1.4, P < 0.001).
DISCUSSION
The aim of the present study was to investigate the relationship between the MetS score and CAD severity according to angiography and to determine if it differed based on the presence of diabetes. The MetS score influenced the severity of coronary atherosclerosis in non-diabetic patients, but there was no relationship between the MetS score and coronary atherosclerosis in diabetic subjects.
The MetS is determined by the presence of ≥ 3 quantitatively identified markers. It has been regarded to be an important risk factor for CAD and a predictor for cardiovascular events (1-5). Some authors have raised the question of whether it has additive prognostic value for CAD in tandem with its individual components. It was suggested that attempts to define a criteria of the MetS that simultaneously predicts for CAD and diabetes are unhelpful because the MetS had weak or no association with cardiovascular risk (6, 10, 18, 19). Those findings indicated that the MetS is a marker of CAD risk, but not above and beyond the risk associated with its individual components. In our cohort, elevated fasting glucose level and high blood pressure were the most frequently encountered factors in patients with the MetS. Our findings coincided with studies in which high blood pressure and a high fasting blood glucose level were strongly related to cardiovascular mortality among individual MetS components (10). The MetS remained an independently associated factor for angiographic CAD on multiple logistic regression analysis. Thus, glycemic level and high blood pressure are the most critical components of the MetS for the development of CAD, and the MetS might have an additive effect on the severity of coronary atherosclerosis beyond that of its individual components.
We also sought to investigate the usefulness of counting individual factors of the MetS for prediction of CAD. Increasing MetS score was significantly related to increasing coronary atherosclerosis score, consistent with the results of other studies (11, 12). Patients with more than two components of the MetS not fulfilling the criteria for the diagnosis of the MetS had a higher atherosclerosis score and more multi-vessel disease than subjects with one or fewer than one component of the MetS. Counting the components of the MetS appears to be more valuable for risk stratification for CAD than dichotomously diagnosing the MetS if there are more than three arbitrary components. To verify the relationship between the MetS score and coronary atherosclerosis in diabetes, we divided the study cohort into two groups based on the presence of diabetes. In non-diabetic subjects (n = 402), the relationship between the MetS score and the severity of coronary atherosclerosis persisted, whereas there was no such association in diabetic subjects (n = 125). These findings might be due to attenuation of the impact of the MetS on the development of CAD by the presence of diabetes (a well-recognized strong risk factor for CAD). Similarly, Zornitzki et al. (7) showed that only diabetes (and not the MetS) predicted the severity and extent of CAD in women. Therefore, the MetS score does not seem to be useful for prediction of the extent of CAD in the presence of diabetes.
It has been reported that the MetS imparts an increased risk of cardiovascular events after the first myocardial infarction (20). Lee et al. (21) showed that the MetS was an important predictor for in-hospital death in patients with ST-elevation myocardial infarction. CRP as a marker of vascular inflammation may have a role in increasing CAD activity as well as in promoting coronary atherosclerosis (17, 22, 23). Ridker et al. (24) demonstrated that the MetS score was well correlated with the CRP level, which is consistent with our results. Patients with acute coronary syndrome had a higher MetS score than those with atypical chest pain or stable angina. These findings suggest that accumulating individual components of the MetS may increase vascular inflammation, leading to heightened CAD activity. Thus, the MetS score and CRP level are closely related. The MetS score and CRP level could help us better predict future cardiovascular events in patients with established CAD as well as in those without CAD.
The present study had several limitations. First, the study group contained only Korean patients undergoing their first coronary angiography due to chest pain. Second, the design of our study was cross-sectional. Third, the coronary atherosclerosis score does not represent the actual atheroma volume or plaque burden; it is a crude method for estimating CAD severity. However, coronary angiography is the most widely used technique for assessing coronary anatomy, and this score was validated in a study that compared CRP level with the extent of CAD (17).
In conclusion, the MetS score can be readily obtained and calculated in most clinical situations. Although the association between the MetS score and angiographic CAD severity may be obscured by the presence of diabetes, the MetS score is related to the severity of coronary atherosclerosis in non-diabetic patients. Calculating the MetS score might provide additive information for predicting the extent of CAD in non-diabetic patient with angina.
AUTHOR SUMMARY
Differential Relationship between Metabolic Syndrome Score and Severity of Coronary Atherosclerosis as Assessed by Angiography in a Non-Diabetic and Diabetic Korean Population
Shin-Eui Yoon, Sung Gyun Ahn, Jang-Young Kim, Jin-Sun Park, Joon-Han Shin, Seung-Jae Tahk, Su-Kyeong Lee, Tae-Jin Kim and Na Han
The metabolic syndrome (MetS) and its individual components are regarded as an important factor for the development of atherosclerotic coronary artery disease (CAD). Here we investigated the influence of the presence of diabetes on the relationship between number of MetS components the CAD severity in 527 patients who underwent their first coronary angiography. Interestingly, in the non-diabetic group, atherosclerosis score increased with MetS score whereas there was no significant difference in the diabetic group. Although diabetes itself is a powerful risk factor for CAD, the association between MetS score and angiographic CAD severity may be obscured in the presence of diabetes.
References
- 1.Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults. Executive Summary of the Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 2.Eckel RH, Grundy SM, Zimmet PZ. The metabolic syndrome. Lancet. 2005;365:1415–1428. doi: 10.1016/S0140-6736(05)66378-7. [DOI] [PubMed] [Google Scholar]
- 3.Golden SH, Folsom AR, Coresh J, Sharrett AR, Szklo M, Brancati F. Risk factor groupings related to insulin resistance and their synergistic effects on subclinical atherosclerosis: the atherosclerosis risk in communities study. Diabetes. 2002;51:3069–3076. doi: 10.2337/diabetes.51.10.3069. [DOI] [PubMed] [Google Scholar]
- 4.Hong Y, Jin X, Mo J, Lin HM, Duan Y, Pu M, Wolbrette DL, Liao D. Metabolic syndrome, its preeminent clusters, incident coronary heart disease and all-cause mortality: results of prospective analysis for the Atherosclerosis Risk in Communities study. J Intern Med. 2007;262:113–122. doi: 10.1111/j.1365-2796.2007.01781.x. [DOI] [PubMed] [Google Scholar]
- 5.Isomaa B, Almgren P, Tuomi T, Forsén B, Lahti K, Nissén M, Taskinen MR, Groop L. Cardiovascular morbidity and mortality associated with the metabolic syndrome. Diabetes Care. 2001;24:683–689. doi: 10.2337/diacare.24.4.683. [DOI] [PubMed] [Google Scholar]
- 6.Petersen JL, Yow E, AlJaroudi W, Shaw LK, Goyal A, McGuire DK, Peterson ED, Harrington RA. Metabolic syndrome is not associated with increased mortality or cardiovascular risk in nondiabetic patients with a new diagnosis of coronary artery disease. Circ Cardiovasc Qual Outcomes. 2010;3:165–172. doi: 10.1161/CIRCOUTCOMES.109.864447. [DOI] [PubMed] [Google Scholar]
- 7.Zornitzki T, Ayzenberg O, Gandelman G, Vered S, Yaskil E, Faraggi D, Caspi A, Goland S, Shvez O, Schattner A, Knobler H. Diabetes, but not the metabolic syndrome, predicts the severity and extent of coronary artery disease in women. QJM. 2007;100:575–581. doi: 10.1093/qjmed/hcm066. [DOI] [PubMed] [Google Scholar]
- 8.Resnick HE, Howard BV. Diabetes and cardiovascular disease. Annu Rev Med. 2002;53:245–267. doi: 10.1146/annurev.med.53.082901.103904. [DOI] [PubMed] [Google Scholar]
- 9.Turner R, Cull C, Holman R. United Kingdom Prospective Diabetes Study 17: a nine-year update of a randomized, controlled trial on the effect of improved metabolic control on complications in non-insulin-dependent diabetes mellitus. Ann Intern Med. 1996;124:136–145. doi: 10.7326/0003-4819-124-1_part_2-199601011-00011. [DOI] [PubMed] [Google Scholar]
- 10.Mente A, Yusuf S, Islam S, McQueen MJ, Tanomsup S, Onen CL, Rangarajan S, Gerstein HC, Anand SS. Metabolic syndrome and risk of acute myocardial infarction a case-control study of 26,903 subjects from 52 countries. J Am Coll Cardiol. 2010;55:2390–2398. doi: 10.1016/j.jacc.2009.12.053. [DOI] [PubMed] [Google Scholar]
- 11.Solymoss BC, Bourassa MG, Campeau L, Sniderman A, Marcil M, Lespérance J, Lévesque S, Varga S. Effect of increasing metabolic syndrome score on atherosclerotic risk profile and coronary artery disease angiographic severity. Am J Cardiol. 2004;93:159–164. doi: 10.1016/j.amjcard.2003.09.032. [DOI] [PubMed] [Google Scholar]
- 12.Kim JY, Mun HS, Lee BK, Yoon SB, Choi EY, Min PK, Yoon YW, Hong BK, Rim SJ, Kwon HM. Impact of metabolic syndrome and its individual components on the presence and severity of angiographic coronary artery disease. Yonsei Med J. 2010;51:676–682. doi: 10.3349/ymj.2010.51.5.676. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Ahn SG, Lim HS, Joe DY, Kang SJ, Choi BJ, Choi SY, Yoon MH, Hwang GS, Tahk SJ, Shin JH. Relationship of epicardial adipose tissue by echocardiography to coronary artery disease. Heart. 2008;94:e7. doi: 10.1136/hrt.2007.118471. [DOI] [PubMed] [Google Scholar]
- 14.Haffner SM, Miettinen H, Stern MP. The homeostasis model in San Antonio Heart Study. Diabetes Care. 1997;20:1087–1092. doi: 10.2337/diacare.20.7.1087. [DOI] [PubMed] [Google Scholar]
- 15.Grundy SM, Cleeman JI, Daniels SR, Donato KA, Eckel RH, Franklin BA, Gordon DJ, Krauss RM, Savage PJ, Smith SC, Jr, Spertus JA, Costa F American Heart Association; National Heart, Lung, and Blood Institute. Diagnosis and management of the metabolic syndrome: an American Heart Association/National Heart, Lung, and Blood Institute scientific statement. Circulation. 2005;112:2735–2752. doi: 10.1161/CIRCULATIONAHA.105.169404. [DOI] [PubMed] [Google Scholar]
- 16.Kwon HS, Park YM, Lee HJ, Lee JH, Choi YH, Ko SH, Lee JM, Kim SR, Kang SY, Lee WC, Ahn MS, Noh JH, Kang JM, Kim DS, Yoon KH, Cha BY, Lee KW, Kang SK, Son HY. Prevalence and clinical characteristics of the metabolic syndrome in middle-aged Korean adults. Korean J Intern Med. 2005;20:310–316. doi: 10.3904/kjim.2005.20.4.310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Azar RR, Aoun G, Fram DB, Waters DD, Wu AH, Kiernan FJ. Relation of C-reactive protein to extent and severity of coronary narrowing in patients with stable angina pectoris or abnormal exercise tests. Am J Cardiol. 2000;86:205–207. doi: 10.1016/s0002-9149(00)00856-0. [DOI] [PubMed] [Google Scholar]
- 18.Sattar N, McConnachie A, Shaper AG, Blauw GJ, Buckley BM, de Craen AJ, Ford I, Forouhi NG, Freeman DJ, Jukema JW, Lennon L, Macfarlane PW, Murphy MB, Packard CJ, Stott DJ, Westendorp RG, Whincup PH, Shepherd J, Wannamethee SG. Can metabolic syndrome usefully predict cardiovascular disease and diabetes? Outcome data from two prospective studies. Lancet. 2008;371:1927–1935. doi: 10.1016/S0140-6736(08)60602-9. [DOI] [PubMed] [Google Scholar]
- 19.Greenland P. Critical questions about the metabolic syndrome. Circulation. 2005;112:3675–3676. doi: 10.1161/CIRCULATIONAHA.105.583310. [DOI] [PubMed] [Google Scholar]
- 20.Levantesi G, Macchia A, Marfisi R, Franzosi MG, Maggioni AP, Nicolosi GL, Schweiger C, Tavazzi L, Tognoni G, Valagussa F, Marchioli R GISSI-Prevenzione Investigators. Metabolic syndrome and risk of cardiovascular events after myocardial infarction. J Am Coll Cardiol. 2005;46:277–283. doi: 10.1016/j.jacc.2005.03.062. [DOI] [PubMed] [Google Scholar]
- 21.Lee MG, Jeong MH, Ahn YK, Chae SC, Hur SH, Hong TJ, Kim YJ, Seong IW, Chae JK, Rhew JY, Chae IH, Cho MC, Bae JH, Rha SW, Kim CJ, Choi DH, Jang YS, Yoon JH, Chung WS, Cho JG, Seung KB, Park SJ. Impact of the metabolic syndome on the clinical outcome of patients with acute ST-elevation myocardial infarction. J Korean Med Sci. 2010;25:1456–1461. doi: 10.3346/jkms.2010.25.10.1456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zebrack JS, Muhlestein JB, Horne BD, Anderson JL Intermountain Heart Collaboration Study Group. C-reactive protein and angiographic coronary artery disease: independent and additive predictors of risk in subjects with angina. J Am Coll Cardiol. 2002;39:632–637. doi: 10.1016/s0735-1097(01)01804-6. [DOI] [PubMed] [Google Scholar]
- 23.Rifai N. High-sensitivity C-reactive protein: a useful marker for cardiovascular disease risk prediction and the metabolic syndrome. Clin Chem. 2005;51:504–505. doi: 10.1373/clinchem.2004.044990. [DOI] [PubMed] [Google Scholar]
- 24.Ridker PM, Buring JE, Cook NR, Rifai N. C-reactive protein, the metabolic syndrome, and risk of incident cardiovascular events: an 8-year follow-up of 14719 initially healthy American women. Circulation. 2003;107:391–397. doi: 10.1161/01.cir.0000055014.62083.05. [DOI] [PubMed] [Google Scholar]