Abstract
Alcoholic liver disease (ALD) is a major cause of alcohol-related morbidity and mortality. Its presentation ranges from fatty liver to alcoholic hepatitis (AH), cirrhosis, and hepatocellular carcinoma. Although the amount and pattern of alcohol consumption is a well recognized predisposing factor for the development of serious liver pathology, environmental factors and the host’s genetic make-up may also play significant roles that have not yet been entirely explored. Continuing alcohol consumption is a major factor that influences the survival of patients with AH. The presence of cirrhosis at presentation or its development on follow up is a major factor determining the outcome in the long run. This chapter deals with the epidemiology and magnitude of ALD in general and AH in particular.
Keywords: Alcoholic hepatitis, Acute alcoholic hepatitis, Alcoholic liver disease, Epidemiology, Magnitude, Disease burden
DEFINITION
Alcoholic liver disease (ALD) describes a spectrum of conditions ranging from reversible fatty liver to alcoholic hepatitis (AH), cirrhosis, and hepatocellular carcinoma (HCC). AH is a distinct clinical syndrome caused by chronic alcohol abuse and carries a particularly poor prognosis with a 28-day mortality ranging from 30% to 50%[1]. Although AH is an acute condition, nearly 50% of patients with AH have established cirrhosis at the time of clinical presentation[2].
AH typically occurs in an individual with long-standing history of alcohol intake although abstinence for several weeks prior to admission is not uncommon. However, clinical presentation after abstinence of more than 3 mo should raise suspicion of advanced underlying alcoholic cirrhosis or chronic liver disease.
Several pro-inflammatory cytokines have been detected in AH patients. In uncomplicated cases, histology of AH is characterized by neutrophilic infiltration (a marker of alcohol-induced hepatitis), ballooning degeneration of hepatocytes, spotty necrosis and fibrosis in the perivenular and perisinusoidal space of Disse (‘‘chicken wire’’ fibrosis), and Mallory hyaline inclusions[3].
EPIDEMIOLOGY
Amount of alcohol intake
The amount of alcohol consumption that places an individual at risk of developing AH is not known. However, in practice, most patients with AH drink more than 100 g/d[4] (which corresponds to 6-7 drinks per day where one drink contains 13-15 g of alcohol), with 150-200 g per day being common[5]. The typical patient has consumed alcohol heavily for two or more decades[5], although in an occasional patient alcohol abuse may be for less than 10 years. However, clinicians should consider anyone drinking more than 30-50 g/d for more than 5-10 years at risk of developing ALD[6].
Estimates of the amount of alcohol consumed may not be accurate since it is based on interviewing the patient and/or family members[7]. The patient’s history reveals the type of alcohol intake and the amount consumed in volume or number of drinks. One drink is typically defined as 12 ounces (355 mL, 4%-5% weight by volume or w/v) of beer, 5 ounces (125 mL, 10%-12% w/v) of wine or 1.5 ounces (45 mL, 40%-50% w/v) of spirits.
Patterns of alcohol intake around the world are constantly evolving and have a strong bearing on the prevalence and incidence of ALD. In one study reporting data for adult per capita consumption of alcohol in the year 2000, spirits dominated the type of alcohol consumed in most regions of the world. The highest amount of alcohol per adult was reported in Europe, especially in Russia and surrounding countries, and the least was in the mostly Islamic regions of the Eastern Mediterranean and in the less developed region of Southeast Asia, predominantly India[8]. The annual per capita change in alcohol consumption in various countries has a direct correlation to cirrhosis mortality rates. A Canadian study confirmed that per capita alcohol consumption is closely related to mortality rates from alcoholic cirrhosis in both men and women[9]. In another analysis of 22 European countries, the relationship between an increase in liver disease and increase in per capita alcohol intake was shown for both men and women[10].
Population-based surveys indicate that 68% of adult Americans drink at least one alcoholic beverage per month. Traditionally, drinking is considered harmful if alcohol use impacts the daily functioning and/or social life of the individual such as loss of job, accident, loss of family member, or death[11]. About 10% of the population consumes more than two drinks per day, which is a commonly used definition of “heavy drinking”[12]. However, substantial differences exist in the prevalence of heavy drinking among population subgroups. For example, 18% of men but only 3% of women are classified as heavy drinkers. Further, heavy drinking is reported to be more common in Whites than in African Americans or Hispanics. Heavy alcohol consumption is generally more common in people with low educational level and income, the unemployed, and in those with occupations that are characterized by job alienation, job stress, and low job satisfaction[13].
Environmental and host factors
A dose-dependent relationship has been observed between self-reported alcohol intake and the risk of developing ALD[6]. Although physicians should consider anyone drinking ≥ 30-50 g/d for more than 5-10 years at risk for developing ALD, the disease does not develop in everyone with this amount of alcohol consumption. About 90% to 100% of heavy drinkers have steatosis, 10% to 35% have AH, and 8% to 20% have alcoholic cirrhosis[14]. The point prevalence of cirrhosis is 1% in persons drinking 30 to 60 g of alcohol a day and up to 5.7% in those consuming 120 g daily[15]. Clearly, other factors related to environment or the host predispose an individual to the development of liver disease[16]. These factors are:
Age: The typical age at presentation of AH is between 40 and 50 years, with the majority occurring before the age of 60 years[17,18].
Gender: The risk of developing alcohol-induced liver disease increases significantly from 7 to 13 beverages per week for women and from 14 to 27 beverages per week for men; the relative risk increases more steeply for women than for men with increasing alcohol intake[6]. This gender difference is due to several factors such as differences in gastric alcohol, dehydrogenase (ADH) levels, and a higher proportion of body fat in women[19]. Although women are at an increased risk of developing liver disease with alcohol intake[16], the majority of patients with AH are males because men are twice as likely to abuse alcohol compared to women[11].
Race and ethnicity: The rates of development of cirrhosis and mortality are higher in African Americans and Hispanics compared to Caucasians[20]. This was reflected in an analysis of changes in national drinking patterns between 1984 and 1992, which showed longer and heavier drinking patterns in blacks and Hispanics compared to whites[21].
Obesity: The presence of long-standing obesity is an independent risk factor for liver disease and cirrhosis in alcoholics[22]. Given the burgeoning problem of obesity in the developed world, it is likely that alcohol-related injury will increase[23]. Obesity potentiates the severity of ALD in all its stages, including fatty liver, AH, and cirrhosis[24].
Protein Calorie Malnutrition: Most patients with AH are malnourished[25], and the risk of death is closely correlated with the degree of malnutrition[26]. Mortality increases in direct proportion to the extent of malnutrition, approaching 80% in patients with severe malnutrition (i.e., less than 50% of normal nutritional intake)[27]. Micronutrient abnormalities, such as hepatic vitamin A depletion or depressed vitamin E levels, may also potentially aggravate liver disease[28]. Parenteral and enteral feeding improves nutritional status but does not improve short-term survival[29].
Drinking patterns and type: The type of alcoholic beverage and the pattern of drinking also affect the development of liver disease. In one study from Denmark, the chances of getting liver disease were higher from drinking beer and spirits as compared to drinking wine[30]. Drinking outside of meal times increases the risk of developing liver disease. Binge drinking defined as intake of ≥ 5 drinks at a time, another risk factor for AH, is reported in about 28% of adults with a history of alcohol abuse[31-33].
Hepatitis C virus: Concomitant alcohol abuse and hepatitis C virus (HCV) for various reasons, occur in about 14% of individuals with chronic liver disease[34]. Alcohol and HCV act synergistically to increase the incidence of cirrhosis and HCC, more rapid progression to fibrosis and cirrhosis, and reduced survival compared to when either of these factors is present alone[34]. Drinking more than 50 g/day of alcohol increases the relative risk of liver fibrosis in HCV patients 1.3-fold compared to HCV-infected non-drinkers and is associated with higher viremia[35]. Worse clinical course with a higher mortality is also observed with AH in the presence of hepatitis C[36]. A similar interaction has been postulated between chronic hepatitis B infection and alcohol[37], but the evidence is unclear.
Genetic factors: There is higher occurrence of alcoholism in adopted children of alcoholic parents and in monozygotic twins compared to dizygotic twins[38,39]. Polymorphisms of genes encoding for ADH and cytochrome P-450enzymes have been associated with higher occurrence of liver disease[40,41].
MAGNITUDE
Incidence and prevalence
The precise incidence of AH is unknown, although a prevalence of approximately 20% was noted in a cohort of 1604 patients with alcoholism who underwent liver biopsy[4]. The true prevalence of AH is difficult to assess because AH may be completely asymptomatic and often remains undiagnosed[32]. The prevalence of AH may be estimated from the prevalence of alcoholism, which affects 8% of general population in the United States or about 16 million people. In Italy the estimated number of alcoholics is 1 500 000, with 3 500 000 at-risk drinkers[42]. About 10 to 35% of all alcoholics have changes consistent with AH[43]. Since up to 35% of alcoholics are estimated to have AH, the number of AH patients in the United States may be nearly 5 million and in Italy about 500 000.
Global and economic burden
Heavy drinking and its consequences have a significant impact on public health. Five percent of the deaths occurring annually in the United States (approximately 100 000 per year) are either directly or indirectly attributable to alcohol abuse[12]. In 1994, approximately 7.4% of adult Americans met the DSM-IV criteria for the diagnosis of alcohol abuse and/or alcohol dependence[44]. More recent data suggest that 4.6% meet criteria for alcohol abuse and 3.8% for alcohol dependence[45].
In 1990, alcohol accounted for 3.5% of the global burden of disease, whereas tobacco accounted for 2.6%[8]. In industrialized countries, between 5% and 66% of all chronic liver disease is related to alcohol use. The costs to society from alcohol abuse cannot be overemphasized. The estimated overall cost in the United States in 1998 was $184.6 billion, with healthcare costs accounting for $26.5 billion of that total. Approximately $600 million to $1.8 billion was spent on hospital-related costs. As per the Centers for Disease Control (CDC), the incidence of chronic liver disease between December 1998 and November 1999 was 72.3 per 100 000. Of these cases, 24% were due to alcohol and 57% were due to HCV[46].
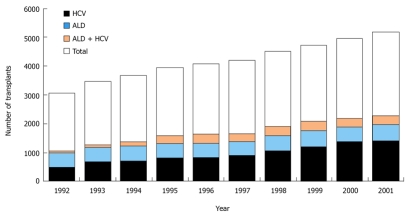
ALD is the second most common indication for orthotopic liver transplantation (OLT) for chronic liver disease in the Western world[47]. According to the United Network for Organ Sharing (UNOS) database, 41 734 liver transplants using organs from dead donors (cadaveric transplants) were performed in the United States between 1992 and 2001[48]. Of those, 12.5% were performed on patients with ALD, and 5.8% on patients with ALD and concurrent HCV infection (Figure 1). This makes ALD the second most frequent indication (after hepatitis C) for OLT. Whereas alcoholic cirrhosis is a widely accepted indication for OLT, there is only limited experience of transplantation in patients with AH. Since the current consensus is that at least 6 mo of abstinence is required prior to OLT, most patients with AH do not qualify for OLT[47].
Figure 1.
Liver transplantation for alcoholic liver disease and hepatitis C, 1992-2001. Source: United network for organ sharing (UNOS) registry, 1988-2001. Public data from UNOS/OPTN scientific registry (http://www.unos.org). Accessed on December 2002.ALD: Alcoholic liver disease; HCV: Hepatitis C virus infection.
Mortality data
Excessive alcohol consumption is the third leading preventable cause of death in the United States[49,50]. Globally alcohol consumption accounts for an estimated 3.8% mortality[8]. Although there are varoius causes of death among alcoholics, liver disease stands out as a significant cause of mortality. In 2003, 44% of all deaths from liver disease were attributed to alcohol[51], while approximately 10%-15% of U.S. alcoholics eventually developed ALD[52]. Since alcoholism is high among young people, approximately 30 years of life are lost per alcohol-associated death with about 2.3 million years of potential life lost in 2001 in the U.S.[49].
Trends in mortality from ALD: Age- and sex adjusted incidence rates of ALD-related deaths decreased from 6.9/100 000 persons in 1980 to 4.4/100 000 persons in 2003. The age- and sex-adjusted ALD-related mortality (per 100 000 persons) decreased from 6.3 to 4.5 in Caucasians, 11.6 to 4.1 in African Americans, and 8.0 to 3.7 in the “other” race groups[53]. Hence, as of 2003, ALD-related mortality affected the three race categories similarly. The rates of deaths related to AH did not increase over the 24-year period[54]. However, this may provide an incomplete picture as AH is often misdiagnosed by physicians and by coding specialists and the true burden of AH related deaths may be underestimated[32].
Short-term mortality of AH: In the short term, the mortality of AH is closely related to the severity of illness on presentation. Overall, there is 15% mortality at 30 d and 39% at 1 year[55]. Mortality varies with the disease severity with about 20% in mild forms, and between 30% and 60% in severe AH[56]. In a British study, 30-day mortality rates of less than 20% were observed in patients with mild to moderate disease but exceeded 40% in individuals with severe liver injury[57]. Survival in this study was poorer among women[57].
Long-term follow up and progression to cirrhosis of AH: In a study on a cohort of patients with AH followed for over 4 years, survival was about 58% in uncomplicated AH, but 35% in AH with cirrhosis[58]. The probability of developing cirrhosis in patients with AH is approximately 10% to 20% per year, and approximately 70% of patients with AH will ultimately develop cirrhosis[59]. In one study, approximately 40% of patients with AH were found to have cirrhosis on repeat biopsy 5 years later[60]. Outcome depends largely on abstinence from alcohol. In individuals with complete cessation of alcohol intake, complete recovery of liver function and reversion to normal liver histology has been described in about 10% of the cases[61]. In this same study, progression of AH to cirrhosis despite abstinence occurred in a higher proportion of women compared to men indicating that women are at a greater risk of progression of ALD[62].
In summary, AH, a frequent cause of alcohol related morbidity and mortality in patients with chronic alcohol abuse is a common and distinct clinical syndrome. Alcohol abstinence is the dominant factor determining outcome in the short-term as well as on long-term follow-up.
Footnotes
Peer reviewers: Valentina Medici, MD, PhD, Department of Internal Medicine, University of California Davis, 4150 V Street, Suite 3500, Sacramento, CA 95817, United States; Neeraj Saxena, PhD, Assistant Professor of Medicine, Department of Medicine, Division of Digestive Diseases, Room 255, Whitehead Biomedical Research Bldg.615 Michael Street, Atlanta, GA 30322, United States
S- Editor Zhang HN L- Editor Hughes D E- Editor Zhang L
References
- 1.Maddrey WC, Boitnott JK, Bedine MS, Weber FL, Mezey E, White RI. Corticosteroid therapy of alcoholic hepatitis. Gastroenterology. 1978;75:193–199. [PubMed] [Google Scholar]
- 2.O’Shea RS, Dasarathy S, McCullough AJ. Alcoholic liver disease. Hepatology. 2010;51:307–328. doi: 10.1002/hep.23258. [DOI] [PubMed] [Google Scholar]
- 3.Purohit V, Russo D. Cellular and molecular mechanisms of alcoholic hepatitis: introduction and summary of the symposium. Alcohol. 2002;27:3–6. doi: 10.1016/s0741-8329(02)00211-2. [DOI] [PubMed] [Google Scholar]
- 4.Naveau S, Giraud V, Borotto E, Aubert A, Capron F, Chaput JC. Excess weight risk factor for alcoholic liver disease. Hepatology. 1997;25:108–111. doi: 10.1002/hep.510250120. [DOI] [PubMed] [Google Scholar]
- 5.Mendenhall CL, Moritz TE, Roselle GA, Morgan TR, Nemchausky BA, Tamburro CH, Schiff ER, McClain CJ, Marsano LS, Allen JI. A study of oral nutritional support with oxandrolone in malnourished patients with alcoholic hepatitis: results of a Department of Veterans Affairs cooperative study. Hepatology. 1993;17:564–576. doi: 10.1002/hep.1840170407. [DOI] [PubMed] [Google Scholar]
- 6.Becker U, Deis A, Sørensen TI, Grønbaek M, Borch-Johnsen K, Müller CF, Schnohr P, Jensen G. Prediction of risk of liver disease by alcohol intake, sex, and age: a prospective population study. Hepatology. 1996;23:1025–1029. doi: 10.1002/hep.510230513. [DOI] [PubMed] [Google Scholar]
- 7.Midanik L. The validity of self-reported alcohol consumption and alcohol problems: a literature review. Br J Addict. 1982;77:357–382. doi: 10.1111/j.1360-0443.1982.tb02469.x. [DOI] [PubMed] [Google Scholar]
- 8.Rehm J, Mathers C, Popova S, Thavorncharoensap M, Teerawattananon Y, Patra J. Global burden of disease and injury and economic cost attributable to alcohol use and alcohol-use disorders. Lancet. 2009;373:2223–2233. doi: 10.1016/S0140-6736(09)60746-7. [DOI] [PubMed] [Google Scholar]
- 9.Ramstedt M. Alcohol consumption and liver cirrhosis mortality with and without mention of alcohol--the case of Canada. Addiction. 2003;98:1267–1276. doi: 10.1046/j.1360-0443.2003.00464.x. [DOI] [PubMed] [Google Scholar]
- 10.Corrao G, Ferrari P, Zambon A, Torchio P. Are the recent trends in liver cirrhosis mortality affected by the changes in alcohol consumption? Analysis of latency period in European countries. J Stud Alcohol. 1997;58:486–494. doi: 10.15288/jsa.1997.58.486. [DOI] [PubMed] [Google Scholar]
- 11.Mandayam S, Jamal MM, Morgan TR. Epidemiology of alcoholic liver disease. Semin Liver Dis. 2004;24:217–232. doi: 10.1055/s-2004-832936. [DOI] [PubMed] [Google Scholar]
- 12.Hoofnagle JH, Kresina T, Fuller RK, Lake JR, Lucey MR, Sorrell MF, Beresford TP. Liver transplantation for alcoholic liver disease: executive statement and recommendations. Summary of a National Institutes of Health workshop held December 6-7, 1996, Bethesda, Maryland. Liver Transpl Surg. 1997;3:347–350. doi: 10.1002/lt.500030324. [DOI] [PubMed] [Google Scholar]
- 13.Singh GK, Hoyert DL. Social epidemiology of chronic liver disease and cirrhosis mortality in the United States, 1935-1997: trends and differentials by ethnicity, socioeconomic status, and alcohol consumption. Hum Biol. 2000;72:801–820. [PubMed] [Google Scholar]
- 14.Sorrell MF, Mukherjee S. Non-Alcoholic Steatohepatitis (NASH) Curr Treat Options Gastroenterol. 1999;2:447–450. doi: 10.1007/s11938-999-0047-9. [DOI] [PubMed] [Google Scholar]
- 15.Lucey MR, Mathurin P, Morgan TR. Alcoholic hepatitis. N Engl J Med. 2009;360:2758–2769. doi: 10.1056/NEJMra0805786. [DOI] [PubMed] [Google Scholar]
- 16.Bellentani S, Saccoccio G, Costa G, Tiribelli C, Manenti F, Sodde M, Saveria Crocè L, Sasso F, Pozzato G, Cristianini G, et al. Drinking habits as cofactors of risk for alcohol induced liver damage. The Dionysos Study Group. Gut. 1997;41:845–850. doi: 10.1136/gut.41.6.845. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mendenhall CL. Alcoholic hepatitis. Clin Gastroenterol. 1981;10:417–441. [PubMed] [Google Scholar]
- 18.Lischner MW, Alexander JF, Galambos JT. Natural history of alcoholic hepatitis. I. The acute disease. Am J Dig Dis. 1971;16:481–494. doi: 10.1007/BF02235538. [DOI] [PubMed] [Google Scholar]
- 19.Frezza M, Terpin MM. [Acute alcoholic hepatitis: clinical and therapeutic considerations] G Clin Med. 1990;71:707–716. [PubMed] [Google Scholar]
- 20.Stinson FS, Grant BF, Dufour MC. The critical dimension of ethnicity in liver cirrhosis mortality statistics. Alcohol Clin Exp Res. 2001;25:1181–1187. [PubMed] [Google Scholar]
- 21.Caetano R, Kaskutas LA. Changes in drinking patterns among whites, blacks and Hispanics, 1984-1992. J Stud Alcohol. 1995;56:558–565. doi: 10.15288/jsa.1995.56.558. [DOI] [PubMed] [Google Scholar]
- 22.Goldin RD, Wickramasinghe SN. Hepatotoxicity of ethanol in mice. Br J Exp Pathol. 1987;68:815–824. [PMC free article] [PubMed] [Google Scholar]
- 23.Raynard B, Balian A, Fallik D, Capron F, Bedossa P, Chaput JC, Naveau S. Risk factors of fibrosis in alcohol-induced liver disease. Hepatology. 2002;35:635–638. doi: 10.1053/jhep.2002.31782. [DOI] [PubMed] [Google Scholar]
- 24.Mathurin P, Beuzin F, Louvet A, Carrie-Ganne N, Balian A, Trinchet JC, Dalsoglio D, Prevot S, Naveau S. Fibrosis progression occurs in a subgroup of heavy drinkers with typical histological features. Aliment Pharmacol Ther. 2007;25:1047–1054. doi: 10.1111/j.1365-2036.2007.03302.x. [DOI] [PubMed] [Google Scholar]
- 25.Mendenhall CL, Anderson S, Weesner RE, Goldberg SJ, Crolic KA. Protein-calorie malnutrition associated with alcoholic hepatitis. Veterans Administration Cooperative Study Group on Alcoholic Hepatitis. Am J Med. 1984;76:211–222. doi: 10.1016/0002-9343(84)90776-9. [DOI] [PubMed] [Google Scholar]
- 26.Mendenhall CL, Tosch T, Weesner RE, Garcia-Pont P, Goldberg SJ, Kiernan T, Seeff LB, Sorell M, Tamburro C, Zetterman R. VA cooperative study on alcoholic hepatitis. II: Prognostic significance of protein-calorie malnutrition. Am J Clin Nutr. 1986;43:213–218. doi: 10.1093/ajcn/43.2.213. [DOI] [PubMed] [Google Scholar]
- 27.Mendenhall C, Roselle GA, Gartside P, Moritz T. Relationship of protein calorie malnutrition to alcoholic liver disease: a reexamination of data from two Veterans Administration Cooperative Studies. Alcohol Clin Exp Res. 1995;19:635–641. doi: 10.1111/j.1530-0277.1995.tb01560.x. [DOI] [PubMed] [Google Scholar]
- 28.Leevy CM, Moroianu SA. Nutritional aspects of alcoholic liver disease. Clin Liver Dis. 2005;9:67–81. doi: 10.1016/j.cld.2004.11.003. [DOI] [PubMed] [Google Scholar]
- 29.Stickel F, Hoehn B, Schuppan D, Seitz HK. Review article: Nutritional therapy in alcoholic liver disease. Aliment Pharmacol Ther. 2003;18:357–373. doi: 10.1046/j.1365-2036.2003.01660.x. [DOI] [PubMed] [Google Scholar]
- 30.Becker U, Grønbaek M, Johansen D, Sørensen TI. Lower risk for alcohol-induced cirrhosis in wine drinkers. Hepatology. 2002;35:868–875. doi: 10.1053/jhep.2002.32101. [DOI] [PubMed] [Google Scholar]
- 31.Wechsler H, Austin SB. Binge drinking: the five/four measure. J Stud Alcohol. 1998;59:122–124. doi: 10.15288/jsa.1998.59.122. [DOI] [PubMed] [Google Scholar]
- 32.Ceccanti M, Attili A, Balducci G, Attilia F, Giacomelli S, Rotondo C, Sasso GF, Xirouchakis E, Attilia ML. Acute alcoholic hepatitis. J Clin Gastroenterol. 2006;40:833–841. doi: 10.1097/01.mcg.0000225570.04773.5d. [DOI] [PubMed] [Google Scholar]
- 33.Zakhari S, Li TK. Determinants of alcohol use and abuse: Impact of quantity and frequency patterns on liver disease. Hepatology. 2007;46:2032–2039. doi: 10.1002/hep.22010. [DOI] [PubMed] [Google Scholar]
- 34.Singal AK, Anand BS. Mechanisms of synergy between alcohol and hepatitis C virus. J Clin Gastroenterol. 2007;41:761–772. doi: 10.1097/MCG.0b013e3180381584. [DOI] [PubMed] [Google Scholar]
- 35.Poynard T, Bedossa P, Opolon P. Natural history of liver fibrosis progression in patients with chronic hepatitis C. The OBSVIRC, METAVIR, CLINIVIR, and DOSVIRC groups. Lancet. 1997;349:825–832. doi: 10.1016/s0140-6736(96)07642-8. [DOI] [PubMed] [Google Scholar]
- 36.Singal AK, Sagi SV, Weinman SA, Snyder N. Impact of hepatitis C on the outcome and severity of acute alcoholic hepatitis. Eur J Gastroenterol and Hepatol. 2011;23:204–209. doi: 10.1097/MEG.0b013e328343b085. [DOI] [PubMed] [Google Scholar]
- 37.Brechot C, Nalpas B, Feitelson MA. Interactions between alcohol and hepatitis viruses in the liver. Clin Lab Med. 1996;16:273–287. [PubMed] [Google Scholar]
- 38.Goodwin BL, Xi H, Tejiram R, Eason DD, Ghosh N, Wright KL, Nagarajan U, Boss JM, Blanck G. Varying functions of specific major histocompatibility class II transactivator promoter III and IV elements in melanoma cell lines. Cell Growth Differ. 2001;12:327–335. [PubMed] [Google Scholar]
- 39.Kaprio J, Koskenvuo M, Langinvainio H, Romanov K, Sarna S, Rose RJ. Genetic influences on use and abuse of alcohol: a study of 5638 adult Finnish twin brothers. Alcohol Clin Exp Res. 1987;11:349–356. doi: 10.1111/j.1530-0277.1987.tb01324.x. [DOI] [PubMed] [Google Scholar]
- 40.McClain CJ, Song Z, Barve SS, Hill DB, Deaciuc I. Recent advances in alcoholic liver disease. IV. Dysregulated cytokine metabolism in alcoholic liver disease. Am J Physiol Gastrointest Liver Physiol. 2004;287:G497–G502. doi: 10.1152/ajpgi.00171.2004. [DOI] [PubMed] [Google Scholar]
- 41.Monzoni A, Masutti F, Saccoccio G, Bellentani S, Tiribelli C, Giacca M. Genetic determinants of ethanol-induced liver damage. Mol Med. 2001;7:255–262. [PMC free article] [PubMed] [Google Scholar]
- 42.Hornyak SC, Gehlsen KR, Haaparanta T. Histamine dihydrochloride protects against early alcohol-induced liver injury in a rat model. Inflammation. 2003;27:317–327. doi: 10.1023/a:1026032611643. [DOI] [PubMed] [Google Scholar]
- 43.McCullough AJ, O’Connor JF. Alcoholic liver disease: proposed recommendations for the American College of Gastroenterology. Am J Gastroenterol. 1998;93:2022–2036. doi: 10.1111/j.1572-0241.1998.00587.x. [DOI] [PubMed] [Google Scholar]
- 44.Grant BF, Harford TC, Dawson DA, Chou P, Dufour M, Pickering R. Prevalence of DSM-IV alcohol abuse and dependence: UNITED STATES, 1992. Alcohol Health & Research World. 1994;18:243–248. [PMC free article] [PubMed] [Google Scholar]
- 45.Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991-1992 and 2001-2002 (Reprinted from. Drug and Alcohol Dependence 2004; 74: 223-234). Alcohol Research & Health. 2006;29:79–91. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- 46.Kim WR, Brown RS, Terrault NA, El-Serag H. Burden of liver disease in the United States: summary of a workshop. Hepatology. 2002;36:227–242. doi: 10.1053/jhep.2002.34734. [DOI] [PubMed] [Google Scholar]
- 47.Burra P, Lucey MR. Liver transplantation in alcoholic patients. Transpl Int. 2005;18:491–498. doi: 10.1111/j.1432-2277.2005.00079.x. [DOI] [PubMed] [Google Scholar]
- 48.Public data from UNOS/OPTN scientific registry, 2002 [Google Scholar]
- 49.Alcohol-attributable deaths and years of potential life lost--United States, 2001. MMWR Morb Mortal Wkly Rep. 2004;53:866–870. [PubMed] [Google Scholar]
- 50.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Correction: actual causes of death in the United States, 2000. JAMA. 2005;293:293–294. doi: 10.1001/jama.293.3.293. [DOI] [PubMed] [Google Scholar]
- 51.Yoon YH, Yi HY. Surveillance report #75: liver cirrhosis mortality in the United States, 1970–2003. National Institute on Alcohol Abuse and Alcoholism Web site. Available at: http: //pubs.niaaa.nih.gov/publications/surveillance75/Cirr03.htm. Accessed September; 2007. [Google Scholar]
- 52.Anantharaju A, Van Thiel DH. Liver transplantation for alcoholic liver disease. Alcohol Res Health. 2003;27:257–268. [PMC free article] [PubMed] [Google Scholar]
- 53.Paula H, Asrani SK, Boetticher NC, Pedersen R, Shah VH, Kim WR. Alcoholic liver disease-related mortality in the United States: 1980-2003. Am J Gastroenterol. 2010;105:1782–1787. doi: 10.1038/ajg.2010.46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Yang AL, Vadhavkar S, Singh G, Omary MB. Epidemiology of alcohol-related liver and pancreatic disease in the United States. Arch Intern Med. 2008;168:649–656. doi: 10.1001/archinte.168.6.649. [DOI] [PubMed] [Google Scholar]
- 55.Mathurin P, Duchatelle V, Ramond MJ, Degott C, Bedossa P, Erlinger S, Benhamou JP, Chaput JC, Rueff B, Poynard T. Survival and prognostic factors in patients with severe alcoholic hepatitis treated with prednisolone. Gastroenterology. 1996;110:1847–1853. doi: 10.1053/gast.1996.v110.pm8964410. [DOI] [PubMed] [Google Scholar]
- 56.Fujimoto M, Uemura M, Kojima H, Ishii Y, Ann T, Sakurai S, Okuda K, Noguchi R, Adachi S, Kitano H, et al. Prognostic factors in severe alcoholic liver injury. Nara Liver Study Group. Alcohol Clin Exp Res. 1999;23:33S–38S. doi: 10.1111/j.1530-0277.1999.tb04531.x. [DOI] [PubMed] [Google Scholar]
- 57.Morgan MY. The prognosis and outcome of alcoholic liver disease. Alcohol Alcohol Suppl. 1994;2:335–343. [PubMed] [Google Scholar]
- 58.Maher JJ. Treatment of alcoholic hepatitis. J Gastroenterol Hepatol. 2002;17:448–455. doi: 10.1046/j.1440-1746.2002.02722.x. [DOI] [PubMed] [Google Scholar]
- 59.Bird GL, Williams R. Factors determining cirrhosis in alcoholic liver disease. Mol Aspects Med. 1988;10:97–105. doi: 10.1016/0098-2997(88)90017-9. [DOI] [PubMed] [Google Scholar]
- 60.Alexander JF, Lischner MW, Galambos JT. Natural history of alcoholic hepatitis. II. The long-term prognosis. Am J Gastroenterol. 1971;56:515–525. [PubMed] [Google Scholar]
- 61.Pares A, Caballeria J, Bruguera M, Torres M, Rodes J. Histological course of alcoholic hepatitis. Influence of abstinence, sex and extent of hepatic damage. J Hepatol. 1986;2:33–42. doi: 10.1016/s0168-8278(86)80006-x. [DOI] [PubMed] [Google Scholar]
- 62.Chen JJ, Schenker S, Henderson GI. 4-hydroxynonenal levels are enhanced in fetal liver mitochondria by in utero ethanol exposure. Hepatology. 1997;25:142–147. doi: 10.1002/hep.510250126. [DOI] [PubMed] [Google Scholar]