Abstract
Background:
Medical curriculum does not provide required space for oral health; hence, many medical interns are unfamiliar with the oral cavity and oral health research.
Aims:
To study the level of awareness regarding systemic effects of periodontal disease among medical interns.
Settings and design:
A cross-sectional qualitative study recruiting medical interns from two medical institutions affiliated to two different universities in Southern India.
Materials and Methods:
Study was carried out in two medical institutions affiliated to two different universities in Southern India. A total of 143 interns participated in the study. Each participant was given a self-administered, pre-tested, multiple choice question–type questionnaire to solve on the spot. In order to summarise the awareness level, respondents were graded on a five-level scale as poor, fair, good, very good, and excellent.
Statistical analysis used:
Percentages, proportions.
Results:
A total of 67 respondents (47%) had fair; 60(42%), poor; and 18(11%), good level of awareness regarding the systemic effects of periodontal disease. Only 23(16%), 17(12%), 12(8%), 6(4%) and 4(3%) respondents were aware that the periodontal disease may be the possible risk factor for coronary heart disease, cerebral infarction, diabetes mellitus, hospital-acquired pneumonia, and preterm labour (low birth-weight infants), respectively. Only 12 respondents (8%) would seek dentist's opinion for all patients with systemic diseases related to dental disease.
Conclusions:
Medical interns had inadequate awareness regarding the systemic effects of periodontal disease. Therefore, an integrated teaching of medical and dental sciences is recommended.
Keywords: Awareness, India, Medical interns, Periodontal disease, Systemic effects
INTRODUCTION
Periodontal disease is predominantly a Gram-negative infection resulting in severe inflammation, with potential in vascular dissemination (via the sulcular epithelium) of microorganisms and their products such as Lipopolysaccharides (LPS) throughout the body.[1] By far it is the most common oral infection in India, with a prevalence rate of 66.2% among individuals of age 15 years and about 89.2% among adults in the age group of 35-44 years.[2] The potential impact of many systemic disorders on the periodontium is documented, though recent evidence suggests that periodontal infection may significantly enhance the risk for certain systemic diseases or alter the natural course of systemic conditions.[3,4] Conditions in which the influences of periodontal infections are documented include coronary heart disease; coronary heart disease-related events such as angina, infarction and atherosclerosis; stroke; diabetes mellitus; preterm labour (low birth-weight infants); and respiratory conditions such as Chronic Obstructive Pulmonary Disease (COPD).[3–5] Since many medical professionals are unfamiliar with the oral cavity and oral health research, they do not recognise the potential infection that may exist within the oral cavity.[1] Given the high prevalence of periodontal disease in India and its deleterious association with systemic disease, patients visiting medical practitioners may not be receiving the required education and guidance. In India where the dentist to population ratio is 1:30000 in urban areas and 1:150000 in rural areas, medical practitioners have to take care of the oral health needs of people.[6]
Therefore, the present study was carried out to understand the level of awareness regarding the systemic effects of periodontal disease among medical interns–the future medical practitioners–so that their training needs with respect to the subject under study may be realised.
MATERIALS AND METHODS
In order to know the level of awareness among medical interns regarding the systemic effects of periodontal disease, the present study was carried out in one of the Southern States in India. Medical interns from two conveniently located medical institutions affiliated to two different universities were included in the study order to rule out institutional bias. Consent for conducting the study was obtained from the concerned authorities of the institutions selected for study after appraising them regarding the purpose and significance of the study, as well as ensuring anonymity of the institutions and the respondents. The interns were posted in different departments, including outreach postings, with different time schedules. Therefore, the study included all interns who were posted in the hospital and could be contacted between 9 a.m. and 4 p.m. A verbal consent was obtained from all participants. The purpose of the study and all the terms used in the study were explained to the respondents and were ensured maintaining total confidentiality. Each participant was given a self-administered, pre-tested, Multiple Choice Questions type questionnaire to solve on the spot. The questionnaire was developed to assess the knowledge of medical interns regarding etio-pathogenesis of periodontitis, its relationship with systemic diseases, its prevention and referral choices and training of medical interns in regards to oral health. The questionnaire had a total of 10 questions and 15 right choices, as some of the questions had more than one right choice (respondents were informed about this aspect of the questionnaire).The data thus collected were compiled, analysed using SPSS version 11.5 and interpreted. In order to summarise the awareness level, responses were graded from 0-15 based on the correct responses. The respondents securing 0-3, 4-6, 7-9, 10-12, and 13-15 marks were graded as having awareness level as poor, fair, good, very good, and excellent, respectively. Results were expressed in terms of percentage and proportions.
RESULTS
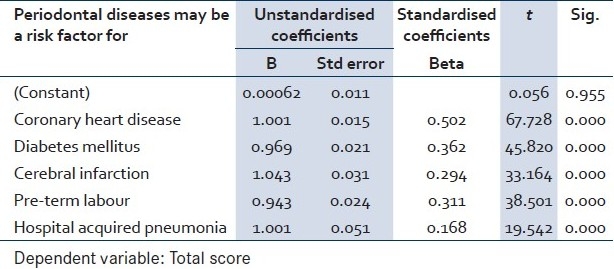
A total of 196 interns from the institutions were included in the study. The interns were posted in different departments, including outreach postings, with different time schedules. Therefore, 143 interns (73 from institution A and 70 from institution B) who were posted in the hospital and could be contacted between 9 a.m. and 4 p.m. were included in the study. The interns who were contacted for the purpose of study participated in the study. All participants answered all questions except the question on referral preferences, which was not answered by 20 participants (14%). No statistically significant difference was observed in the level of awareness regarding the systemic effects of periodontal disease among medical interns of the participating institutions. Table 1 shows the distribution of the responses regarding the relationship between systemic and dental diseases. Only 16(11%) of the respondents were aware that it is a two-way process, while a majority [120(84%)] of the respondents knew only half the fact. Surprisingly, 7 respondents (5%) believed that the oral cavity is a remote cavity so no relationship exists between the two. A majority of respondents 94(66%) considered periodontal disease as an inflammatory disease with superimposed infection, whereas only 46(32%) were aware that it is an infectious disease resulting in inflammation. Fifty-four respondents (38%) were aware that it is predominantly a Gram–negative infection. A total of 84 respondents (59%) considered cigarette smoking or any mechanical force as its cause, 78(74%) and 74(71%) considered it as a risk factor for bad breath and dental caries, respectively. Table 2 shows that only 23(16%), 17(12%), 12(8%), 6(4%) and 4(3%) of the respondents were aware that the periodontal disease may be the possible risk factor for coronary heart disease, cerebral infarction, diabetes mellitus, hospital-acquired pneumonia and preterm labour (low birth-weight infants), respectively [Figure 1]. Multivariate analysis for Table 2 for questions whether periodontal disease may be a risk factor for systemic diseases like coronary heart disease, diabetes mellitus, cerebral infarction, pre-term labour and hospital-acquired pneumonia showed that only 11 respondents have given correct answers for two or more questions at the same time. Responses to these questions have affected the total scores, which is statistically significant [Table 3].
Table 1.
Distribution of responses regarding relationship between systemic and periodontal disease
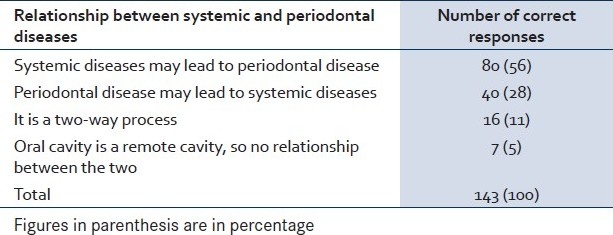
Table 2.
Distribution of responses on periodontal disease as a risk factor for various systemic diseases
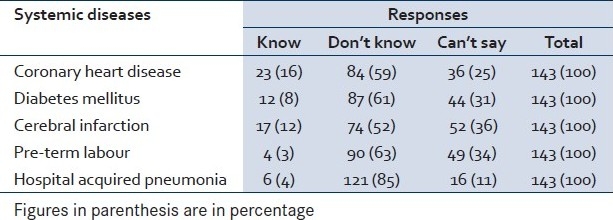
Figure 1.
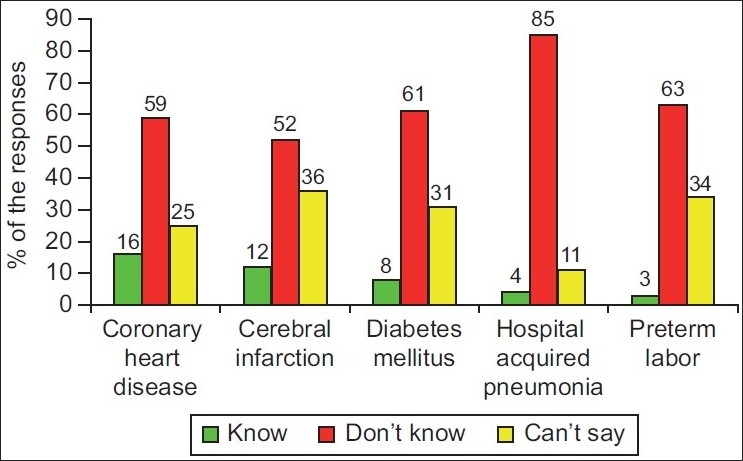
Distribution of responses regarding periodontal disease as a risk factor for various systemic diseases
Table 3.
Multivariate analysis for questions whether periodontal disease may be a risk factor systemic diseases
A majority of respondents 137(96%) reported that they never asked patients if they were diagnosed with periodontal disease and 134(94%) reported not receiving any training about periodontal disease during their medical course. Fifty-nine respondents (41%) were of the opinion that periodontal disease is a non-modifiable condition. More than three-fourth (78%) of the medical interns would prefer referring only those patients to dentists who have some dental disease. Only 12 respondents (8%) would seek dentist's opinion for all patients with systemic diseases related to dental disease. Twenty respondents (14%) did not respond to this question.
Table 4 shows the level of awareness regarding the systemic effects of periodontal disease among medical interns. Sixty respondents (42%) were having poor; 67(47%), fair; 16(11%), good level of awareness. None of the respondents showed very good or excellent level of awareness regarding the inter-relationship between the systemic and dental diseases [Figure 2].
Table 4.
Level of awareness regarding the systemic effects of periodontal disease among medical interns
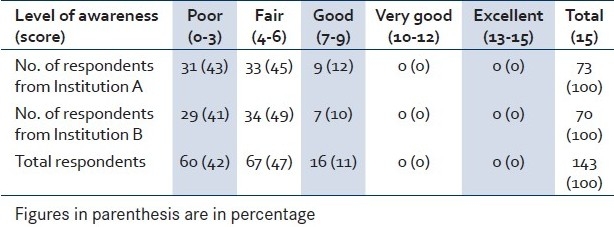
Figure 2.
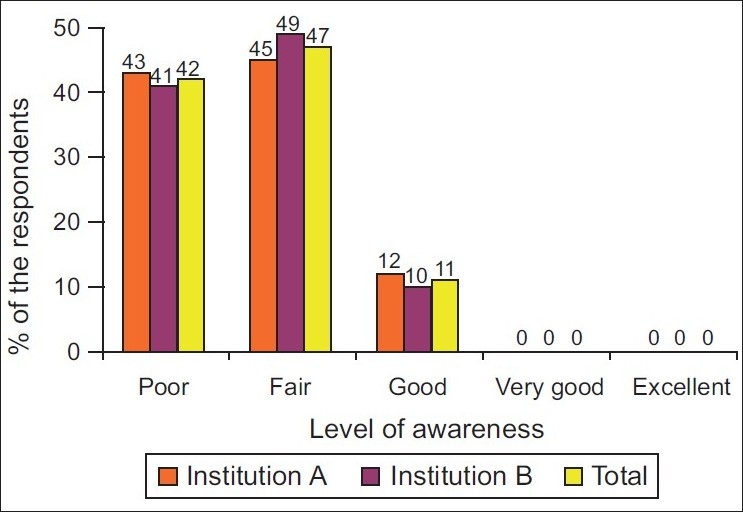
Level of awareness regarding the systemic effects of periodontal disease among the medical interns
DISCUSSION
Periodontal disease is a complex infectious disease resulting from interplay of bacterial infections and host-response to bacterial challenges. It is estimated that more than 500 different bacterial species are capable of colonising the mouth of an adult.[7] Systemic challenges with the potential vascular dissemination of microorganisms and their products (via the sulcular epithelium) such as Lipopolysaccharides (LPS) throughout the body induce a major vascular response.[1,5] This host-response may offer explanatory mechanism for the interaction between periodontal infection and a variety of systemic disorders like coronary heart disease;[8–11] coronary heart disease–related events such as angina, infarction and atherosclerosis;[11,12] stroke;[3,13] diabetes mellitus;[14,15] preterm labour (low birth-weight infants);[16–18] chronic obstructive pulmonary disease;[19,20] and hospital-acquired pneumonia.[3,21,22] The total surface area of pocket epithelium in contact with sub-gingival bacteria and their products in a patient with generalised moderate periodontitis is estimated to be the size of an adult hand and with even larger areas of exposure in case of more a dvanced periodontal destruction.[23] An infection of the size of the palm of a hand on the leg of a pregnant women or an individual with diabetes mellitus would be a major concern for a patient and his or her doctor. Periodontal infection must be viewed in a similar manner. In susceptible individuals, it may act as an independent risk factor for systemic diseases.[1] Fortunately, it is a readily modifiable risk factor. The present study reveals that medical interns had limited awareness regarding the systemic effects of periodontal disease. Similar finding have been observed elsewhere also.[24,25] Specialisation has indeed isolated the practitioners.[26]
These findings raise important concerns. Given the high prevalence of periodontal disease, its deleterious impact on oral health and its association with systemic disease, patients seeing internal medicine physicians may not be receiving the education and guidance needed. An increased awareness of certain aspects of periodontal disease and its link to systemic conditions are important, and patients should be counselled about this at each healthcare contact they have, whether it is with a dentist, a physician, or any other healthcare provider.
This issue is of extreme importance for India that is being labelled as diabetes capital of the world. Also, coronary heart disease is expected to become the single most important cause of death by the year 2015,[27] and prematurely accounts for 51% of infant deaths in India.[28] The situation is further compounded by the fact that medical doctors have to take care of the oral health needs of the people due to an acute shortage of qualified dentists in India, particularly in rural India where about 72% (Census of India 2001) of the Indian population lives.
Limitations
This study was carried out in one area only; hence, the finding may not be applicable on the national scale. Furthermore, all medical interns could not be included in the study because of their different duty schedules. This may have led to some bias; therefore, a similar study on a larger scale is required to give more representative findings.
CONCLUSION AND RECOMMENDATIONS
The level of awareness regarding the systemic effects of periodontal disease among medical interns is limited. Therefore, it recommended that more space be allocated to the subject of dental sciences in the medical curriculum to improve physicians’ ability to contribute to oral health and stress be given to integrated teaching of medical and dental sciences in order to produce thorough professionals who can serve the humanity in a better way.
Acknowledgments
Authors are thankful to the authorities and the medical interns from both the institutions for their kind permission, cooperation and the enthusiasm they have shown for the study.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Mealy BL, Klokkevold Perry R. Periodontal Medicine: Carranza's Clinical Periodontology. 9th ed. New Delhi: Elsevier; 2004. pp. 229–44. [Google Scholar]
- 2.National Oral Health Survey and Flouride Mapping: Dental Council of India. New Delhi: Dental Council of India; 2004. [Last accessed on 2010 Mar 10]. p. 13. Available from: http://iaphd.org/NationalSurvey/summary.pdf . [Google Scholar]
- 3.Mealy BL. Influence of periodontal infections on systemic health. Periodontology 2000. 1999;21:197–209. doi: 10.1111/j.1600-0757.1999.tb00176.x. [DOI] [PubMed] [Google Scholar]
- 4.Rai B. Systemic Effect of Oral Disease. Internet J Family Pract. 2007;5:1. [Google Scholar]
- 5.Page RC, Beck JD. Risk assessment for periodontal diseases. Int Dent J. 1997;47:61–5. doi: 10.1111/j.1875-595x.1997.tb00680.x. [DOI] [PubMed] [Google Scholar]
- 6.National Oral Health Care Program. Ministry of Health and Family Welfare. New Delhi: Government of India; 2003. [Last accessed on 2010 Aug 21]. Available from: http://www.nohcpaiims.org/imp_strategies.htm . [Google Scholar]
- 7.Moore WE, Moore LV. The bacteria of periodontal disease. Periodontology 2000. 1996;5:66–77. doi: 10.1111/j.1600-0757.1994.tb00019.x. [DOI] [PubMed] [Google Scholar]
- 8.Beck J, Garcia R, Heiss G, Vokonas PS, Offenbacher S. Periodontal disease and cardiovascular disease. J Periodontol. 1996;67:1123–37. doi: 10.1902/jop.1996.67.10s.1123. [DOI] [PubMed] [Google Scholar]
- 9.Beck JD, Offenbacher S, Williams R, Gibbs P, Garcia R. Periodontitis: A risk factor for coronary heart disease? Ann Periodontol. 1998;3:127–41. doi: 10.1902/annals.1998.3.1.127. [DOI] [PubMed] [Google Scholar]
- 10.Mattila KJ, Valtonen VV, Nieminen M, Huttunen JK. Dental infection and the risk of new coronary events: Prospective study of patients with documented coronary artery disease. Clin Infect Dis. 1995;20:588–92. doi: 10.1093/clinids/20.3.588. [DOI] [PubMed] [Google Scholar]
- 11.Rai B, Kharb S. Effect of scaling and root planning in periodontitis on peripheral blood. Internet J Dent Sci. 2008;6:1. [Google Scholar]
- 12.Mattila KJ, Valle MS, Nieminen MS, Valtonen VV, Hietaniemi KL. Dental infections and coronary atherosclerosis. Atherosclerosis. 1993;103:205–11. doi: 10.1016/0021-9150(93)90263-t. [DOI] [PubMed] [Google Scholar]
- 13.Syrjänen J, Peltola J, Valtonen V, Iivanainen M, Kaste M, Huttunen JK. Dental infections in association with cerebral infarction in young and middle aged men. J Intern Med. 1989;225:179–84. doi: 10.1111/j.1365-2796.1989.tb00060.x. [DOI] [PubMed] [Google Scholar]
- 14.Sammalkorpi K. Glucose intolerance in acute infections. J Intern Med. 1989;225:15–9. doi: 10.1111/j.1365-2796.1989.tb00030.x. [DOI] [PubMed] [Google Scholar]
- 15.Grossi SG, Genco RJ. Periodontal diseases and diabetes mellitus: A two-way relationship. Ann Periodontol. 1998;3:51–61. doi: 10.1902/annals.1998.3.1.51. [DOI] [PubMed] [Google Scholar]
- 16.Hill GB. Preterm birth: Association with genital and possible oral microflora. Ann Periodontol. 1998;3:222–32. doi: 10.1902/annals.1998.3.1.222. [DOI] [PubMed] [Google Scholar]
- 17.Offenbacher S, Jared HL, O’Reilly PG, Wells SR, Salvi GE, Lawrence HP, et al. Potential pathogenic mechanisms of periodontitis-associated pregnancy complications. Ann Periodontol. 1998;3:233–50. doi: 10.1902/annals.1998.3.1.233. [DOI] [PubMed] [Google Scholar]
- 18.Dasanayake AP. Poor periodontal health of the pregnant women as a risk factor for low birth weight. Ann Periodontol. 1998;3:202–7. doi: 10.1902/annals.1998.3.1.206. [DOI] [PubMed] [Google Scholar]
- 19.Hayes C, Sparrow D, Cohen M, Vokonas PS, Garcia RI. The association between alveolar bone loss and pulmonary function: The VA dental longitudinal study. Ann Periodontol. 1998;3:257–61. doi: 10.1902/annals.1998.3.1.257. [DOI] [PubMed] [Google Scholar]
- 20.Beck JD. Periodontal implications: Older adults. Ann Periodontol. 1996;1:322–7. doi: 10.1902/annals.1996.1.1.322. [DOI] [PubMed] [Google Scholar]
- 21.Pugin J, Auckenthaler R, Lew DP, Suter PM. Oropharyngeal decontamination decreases incidence of ventilator-associated pneumonia.A randomized, placebo-controlled, double blind clinical trial. JAMA. 1991;265:2704–10. [PubMed] [Google Scholar]
- 22.Stoutenbeek CP, van Saene HK, Miranda DR, Zandstra DF, Langrehr D. The effect of oropharyngeal decontamination on the incidence of nosocomial respiratory tract infections. J Trauma. 1987;27:357–63. doi: 10.1097/00005373-198704000-00003. [DOI] [PubMed] [Google Scholar]
- 23.Page RC. The pathobiology of Periodontal diseases may affect the systemic diseases: Inversion of a paradigm. Ann Periodontol. 1998;3:108–20. doi: 10.1902/annals.1998.3.1.108. [DOI] [PubMed] [Google Scholar]
- 24.Gur A, Majra JP. Knowledge, Attitude and Practices Regarding the Systemic Effects of Oral Diseases among the Medical Practitioners. [Last accessed on 2010 Mar10];Int J Dent Sci. 2009 6:25–9. Available from: http://www.ispub.com/journal/the_internet_journal_of_dental_science/volume_6_number_2_25/article/knowledge_attitude_and_practices_regarding_the_systemic_effects_of_oral_diseases_among_the_medical_practitioners.html . [Google Scholar]
- 25.Quijano A, Shah AJ, Schwarcz AI, Lalla E, Ostfeld RJ. Knowledge and orientations of internal medicine trainees towards periodontal disease. J Periodontol. 2010;81:359–69. doi: 10.1902/jop.2009.090475. [DOI] [PubMed] [Google Scholar]
- 26.Gur A, Majra JP. Has specialization isolated practitioners? Indian J Dent Res. 2010;21:144–5. doi: 10.4103/0970-9290.62790. [DOI] [PubMed] [Google Scholar]
- 27.Park K. Epidemiology of chronic non-communicable diseases and conditions. Park's text book of preventive and social medicine. 20th ed. Jabalpur: Bhanot Publications; 2009. p. 318. [Google Scholar]
- 28.WHO. Improving Maternal, Newborn and Child Health in South East Asian Region. New Delhi: WHO; 2005. [Google Scholar]


