Abstract
For decades, onchocerciasis (or river blindness) was one of the most common infectious causes of blindness in the world. Primarily an infection of Africa, with limited distribution in the new world, disease due to the nematode Onchocerca volvulus is rapidly diminishing as a result of large public health campaigns targeting at risk populations in Africa and the Americas. Existing and newly-developed treatment strategies offer the chance to eliminate onchocercal ocular morbidity in some parts of the world. This article reviews these treatment strategies, current clinical and epidemiologic aspects of onchocerciasis, and the next steps toward elimination.
Keywords: Doxycycline, Ivermectin, Onchocerciasis, Onchocerca volvulus, River blindness, Wolbachia
ONCHOCERCIASIS EPIDEMIOLOGY AND TRANSMISSION
Onchocerciasis is the second leading infectious cause of blindness in the world, after trachoma.[1] For centuries, Onchocerca volvulus has infected humans causing severe skin and eye disease. Transmitted by the bite of the Simulian sp. black fly, the disease is prevalent in 19 African countries, and endemic in now just six American foci. In total, 37 million people are thought to have active disease, with nearly all such cases in Africa where over 100 million people live at risk of new infection.[2,3] This old world disease originated in Africa and spread to New World via the slave trade, where it formerly existed in 13 discrete geographic foci within Latin America.[4,5] Over 500,000 individuals live with a significant visual impairment from the disease, with an additional 270,000 individuals who have suffered from complete vision loss.[6]
Onchocerca volvulus lives only in humans, making it a good candidate for elimination. The Simulian vector is infected when biting infected humans, and after maturation of larva within the fly, can then re-infect others during subsequent blood-meals. These flies breed within and live around fast-flowing rivers (hence the name “river-blindness”), and generally only persons living in and around these areas are at risk for infection after repeated biting. Transmission efficiency of most Simulian species is quite low relative to other diseases (e.g., Anopheles mosquito with malaria), although variable between regions, such that travelers are generally not at risk for this infection unless living long-term in endemic areas.[7]
Once deposited within the skin, infective stage larvas maturate and trigger the development of fibrous subcutaneous nodule in which they will mate and reproduce. Annually, female adult worms can release hundreds of thousands of microfilariae (MF) that migrate freely through skin with the potential for reaching and invading the eye. In the skin, MF cause pruritis and dermatitis, and eventually can lead to skin atrophy and discoloration (“leopard skin”). In the eye, repeated MF insults can lead to significant intraocular inflammation and subsequent eye damage.
THE OCULAR PATHOLOGY OF ONCHOCERCIASIS
The ocular pathology of this disease occurs in both anterior and posterior segments of the eye. Anteriorly, MF travel through scleral and subconjunctival tissues to reach the cornea whereby they attempt to penetrate and migrate through the cornea. Within the corneal stroma, MF can die and release Wolbachia sp. bacteria, an intracellular, rickettsia-like bacteria that lives symbiotically with MF and adult Onchocerca worms.[8,9] Interestingly, these organisms are extremely important to the lifecycle and reproduction of Onchocerca, and without them, female adult worms cannot reproduce.[10] Within the cornea, as with other tissues, release of Wolbachia elicits an immune response and inflammation.[11,12] This process clinically appears in the cornea as a punctate keratitis (PK), lesions that gradually resolve over 2–3 months as the MF are degraded by immune cells. The prevalence of PK has served as the cornerstone for evaluating the progress of mass ivermectin therapy during recent elimination campaigns in the Americas.[13] Repeated MF-associated corneal insults eventually lead to sclerosing keratitis (opacification and scarring of the cornea), a major cause of onchocercal-related visual loss. A large proportion of visual morbidity and blindness caused by this disease, however, is due to posterior pole lesions that persist even after ivermectin therapy.[14–16] In the posterior segment of the eye, MF invade retinal tissues causing chronic chorioretinitis, inflammation, scarring, and in some cases optic atrophy and glaucoma. It is likely that dying MF in these tissues trigger an inflammatory response there, one that is potentially promoted by cross reactivity between O. volvulus antigen (Ov39) and human retinal pathogen (hr44) found in the optic nerve and neural epithelial layers of the retina.[17–19] Interestingly, Onchocercal chorioretinitis continues despite ivermectin therapy and extermination of the parasite from the eye, potentially as a result of an autoimmune response provoked by the parasite.[14,20]
DIAGNOSIS AND CLINICAL MANAGEMENT OF ONCHOCERCIASIS
Diagnosing onchocerciasis relies on demonstration of characteristic eye pathology (visible MF in the cornea or anterior chamber) or demonstration of MF within the skin. On the individual level, visible MF in the anterior segment are specific to onchocerciasis; however, it is often difficult to observe MF in the anterior chamber, and punctuate keratitis lesions are fleeting and can be nonspecific for onchocerciasis if the degraded MF is not visible within the lesion.[21] At lower levels of microfiladermia, ocular lesions are rare and are less likely to be present. Skin-snips, a superficial (dermal) biopsy of 1–3mg, examined microscopically for MF are invasive and suffer from poor sensitivity in patients with low levels of microfiladermia. PCR examination of skin snips improves this situation, although sensitivity is still low in such persons, making this tool less useful in endemic areas where ivermectin has been used to treat this disease for years.[22,23] Skin patch testing with diethylcarbamazine (DEC) has been shown as a good alternative to skin snip evaluations in Africa. This test relies upon DEC killing of MF within the dermis and subsequent provocation of a hypersensitivity reaction (i.e., localized Mazzoti reaction). Advantages over skin snip evaluation (noninvasive, better patient acceptance), although can be operationally difficult (patches can fall off, patients must return in 24 h for test reading). The sensitivity and specificity of the DEC patch test is not yet clear, although recent studies using newer formulations suggest its utility in monitoring for infection within mass onchocerciasis treatment programs in Africa.[1,24,25] Serologic antibody tests using recombinant antigens, such as the OV-16, can be useful, but cannot distinguish between past and active infection.[26–29] In addition, the sensitivity of this assay is questionable, with at least one study showing that a large percentage of those with active eye disease living in endemic areas have negative OV-16 results.[21] A highly specific antigen detection test capable of diagnosing active infection has been reported in the literature, but to date, has received little evaluation.[30] The development of a highly specific and sensitive test capable of determining active onchocercal infection remains an imperative for public health campaigns seeking to control and eliminate this parasite.
Antifilarial therapy
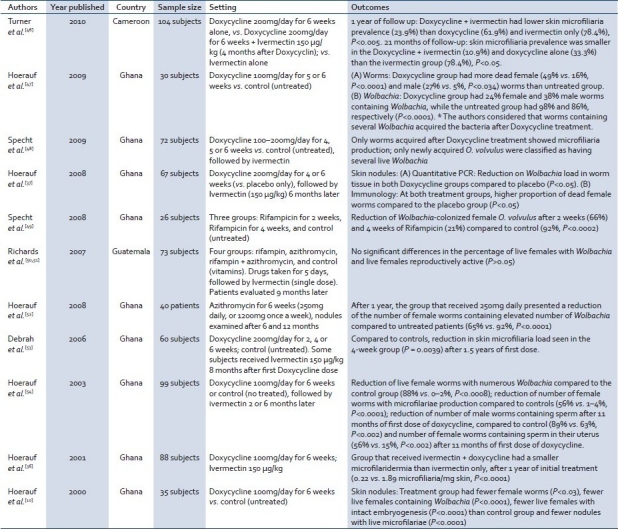
The development of a safe and effective macrofilaricidal drug has been long sought for this disease. For years, ivermectin, a macrocyclic lactone, has been the mainstay of therapy; however, ivermectin kills only the MF.[31,32] In effect, ivermectin serves as a birth control device for adult worms, in that female worms are temporarily sterilized for an average of 6 months, preventing the release of MF during that time. Consequently, periodic single dose oral treatment prevents the onset of new ocular and dermal lesions and reduces transmission as the vector is less exposed to MF during its feeding on human skin.[33] Ivermectin is excluded from the eye by the blood–ocular barrier, thus avoiding intraocular killing of MF and subsequent intraocular damage due to inflammation. Newer lactones in development include moxidectin that has shown some potential as a macrofilaricide.[34,35] However, new therapies targeting the endosymbiotic Wolbachia within the adult worms have now been proven to be effective in causing long-term (and potentially permanent) sterilization of adult worms and early worm death. Doxycycline treatment (100mg/day) for 6 weeks with a single dose of ivermectin has become the treatment of choice for individuals based on recent clinical trial data, although 4 week courses of doxycycline or rifampin are also effective [Table 1].[36,37] From a public health perspective, however, the mass treatment of affected populations with doxycycline is difficult given the length of necessary therapy and the potential for re-infection in endemic areas. However, these therapies may be of particular use in areas of co-endemicity with loiasis where mass distribution of ivermectin is complicated by potential adverse events in patients co-infected with loiasis.[38]
Table 1.
Studies evaluating the efficacy of antibiotic therapy directed at onchocercal endosymbiotic Wolbachia bacteria
CONTROL AND ELIMINATION OF ONCHOCERCIASIS
Two large public health campaigns currently operate worldwide with goals of either elimination or control of this parasite. The cornerstone of these campaigns is the mass distribution of ivermectin, delivered semi-annually or annually, and donated in perpetuity for this cause by Merck.[39] When ivermectin is delivered as such in the long-term, sustained fashion to large percentages of at risk populations (e.g., >85% is the goal in Latin America), dermal MF levels fall such that new eye lesions and transmission are prevented.[7,40,41] The African Programme for Onchocerciasis Control (APOC) currently strives to eliminate onchocerciasis as a “public health concern” by delivering ivermectin to populations where dermal MF prevalence of ≥40%.[39,42] Recent studies in Mali and Senegal indicate a tremendous reduction in microfilaridermia and a profound reduction in the prevalence of black fly infection indicating that elimination is feasible in at least some African foci.[24]
In the Americas, the Onchocerciasis Elimination Program for the Americas (OEPA) strives to completely eliminate the disease by treating ≥85% of at risk persons with ivermectin every 6 months.[4] As of 2010, 7 of the 13 endemic foci have been declared free of onchocerciasis, treatment with ivermectin therapy has stopped, and surveillance for disease recrudescence will continue for 3 years prior to a declaration of disease elimination in these foci. Currently, active eye disease only exists within several foci within Venezuela and Brazil, where treatment coverage has been more recently increased and it is anticipated that elimination of eye disease in these areas will follow in subsequent years.[2]
As anti-Wolbachia therapy has been shown to be effective in clinical trials, its optimal use within these public health campaigns is not yet clear. Within Latin America, conceivably, anti-Wolbachia therapy could be used in limited circumstances either to “mop-up” or “catch-up” in regions that continue to have active disease or where ivermectin coverage has been less than complete. As elimination with ivermectin looms near in Latin America, however, it is not clear that such alternative therapies will ever be needed.[43] Within Africa, at least one large scale community directed treatment program using doxycycline has been reported.[38] As with Latin America, a role for mass doxycycline therapy there has not yet been clearly defined, and might differ by region based on vector competence, parasite pathogenicity, public health capacity, and the ability to deliver 4–6 weeks of such therapy in mass fashion. Lastly, anti-Wolbachia would theoretically become very important in either region should the parasite develop resistance to ivermectin. Although ivermectin resistance has not definitively been reported, it remains a concern and anti-Wolbachia therapy offers an alternative should such an event occur.[16,44,45]
FUTURE EFFORTS
In Latin America, OEPA has declared the year 2015 as a goal for the final year of mass treatment with ivermectin for onchocerciasis,[55] and in Africa great reductions in disease have been documented with mass ivermectin therapy. Although current progress with these mass ivermectin drug campaigns is encouraging, improved diagnostics and further development and evaluation of anti-Wolbachia and other drug therapies will improve the chances that these large regional public health initiatives will achieve long-term success.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Boatin BA, Richards FO., Jr Control of onchocerciasis. Adv Parasitol. 2006;61:349–94. doi: 10.1016/S0065-308X(05)61009-3. [DOI] [PubMed] [Google Scholar]
- 2.Report from the 2009 Inter-American conference on onchocerciasis: Progress towards eliminating river blindness in the Region of the Americas. Wkly Epidemiol Rec. 2010;85:321–6. [PubMed] [Google Scholar]
- 3.African programme for onchocerciasis control - Report of the sixth meeting of national task forces, October 2009. Wkly Epidemiol Rec. 2010;85:23–8. [PubMed] [Google Scholar]
- 4.Onchocerciasis (river blindness). Report from the sixteenth InterAmerican conference on onchocerciasis, Antigua Guatemala, Guatemala. Wkly Epidemiol Rec. 2007;82:314–6. [PubMed] [Google Scholar]
- 5.Zimmerman PA, Katholi CR, Wooten MC, Lang-Unnasch N, Unnasch TR. Recent evolutionary history of American Onchocerca volvulus, based on analysis of a tandemly repeated DNA sequence family. Mol Biol Evol. 1994;11:384–92. doi: 10.1093/oxfordjournals.molbev.a040114. [DOI] [PubMed] [Google Scholar]
- 6.Basáñez MG, Pion SD, Churcher TS, Breitling LP, Little MP, Boussinesq M. River blindness: A success story under threat? PLoS Med. 2006;3:e371. doi: 10.1371/journal.pmed.0030371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cupp EW, Ochoa JO, Collins RC, Cupp MS, Gonzales-Peralta C, Castro J, et al. The effects of repetitive community-wide ivermectin treatment on transmission of Onchocerca volvulus in Guatemala. Am J Trop Med Hyg. 1992;47:170–80. doi: 10.4269/ajtmh.1992.47.170. [DOI] [PubMed] [Google Scholar]
- 8.Pearlman E. Immunopathogenesis of Onchocerca volvulus keratitis (river blindness): A novel role for endosymbiotic Wolbachia bacteria. Med Microbiol Immunol. 2003;192:57–60. doi: 10.1007/s00430-002-0160-z. [DOI] [PubMed] [Google Scholar]
- 9.Saint André A, Blackwell NM, Hall LR, Hoerauf A, Brattig NW, Volkmann L, et al. The role of endosymbiotic Wolbachia bacteria in the pathogenesis of river blindness. Science. 2002;295:1892–5. doi: 10.1126/science.1068732. [DOI] [PubMed] [Google Scholar]
- 10.Hoerauf A, Volkmann L, Hamelmann C, Adjei O, Autenrieth IB, Fleischer B, et al. Endosymbiotic bacteria in worms as targets for a novel chemotherapy in filariasis. Lancet. 2000;355:1242–3. doi: 10.1016/S0140-6736(00)02095-X. [DOI] [PubMed] [Google Scholar]
- 11.Hise AG, Daehnel K, Gillette-Ferguson I, Cho E, McGarry HF, Taylor MJ, et al. Innate immune responses to endosymbiotic Wolbachia bacteria in Brugia malayi and Onchocerca volvulus are dependent on TLR2, TLR6, MyD88, and Mal, but not TLR4, TRIF, or TRAM. J Immunol. 2007;178:1068–76. doi: 10.4049/jimmunol.178.2.1068. [DOI] [PubMed] [Google Scholar]
- 12.Brattig NW, Bazzocchi C, Kirschning CJ, Reiling N, Büttner DW, Ceciliani F, et al. The major surface protein of Wolbachia endosymbionts in filarial nematodes elicits immune responses through TLR2 and TLR4. J Immunol. 2004;173:437–45. doi: 10.4049/jimmunol.173.1.437. [DOI] [PubMed] [Google Scholar]
- 13.Silva JC, Beltran F, Semba R. Evaluacion oftalmológica de la onchocercosis en las Americas. Guatemala: Organizacion panamericana de la Salud and river blindness foundation; pp. 1–14. (published in 1992) [Google Scholar]
- 14.Semba RD, Murphy RP, Newland HS, Awadzi K, Greene BM, Taylor HR. Longitudinal study of lesions of the posterior segment in onchocerciasis. Ophthalmology. 1990;97:1334–41. doi: 10.1016/s0161-6420(90)32413-2. [DOI] [PubMed] [Google Scholar]
- 15.Amazigo U. The African Programme for Onchocerciasis Control (APOC) Ann Trop Med Parasitol. 2008;102:19–22. doi: 10.1179/136485908X337436. [DOI] [PubMed] [Google Scholar]
- 16.Winthrop KL, Pilkington EF, Dance D, Sauerbrey M, Richards FO. River blindness: Old disease, new challenges. Ophthalmol Int. 2008:53–6. [Google Scholar]
- 17.Braun G, McKechnie NM, Connor V, Gilbert CE, Engelbrecht F, Whitworth JA, et al. Immunological crossreactivity between a cloned antigen of Onchocerca volvulus and a component of the retinal pigment epithelium. J Exp Med. 1991;174:169–77. doi: 10.1084/jem.174.1.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.McKechnie NM, Braun G, Connor V, Kläger S, Taylor DW, Alexander RA, et al. Immunologic cross-reactivity in the pathogenesis of ocular onchocerciasis. Invest Ophthalmol Vis Sci. 1993;34:2888–902. [PubMed] [Google Scholar]
- 19.Braun G, McKechnie NM, Gürr W. Molecular and immunological characterization of hr44, a human ocular component immunologically cross-reactive with antigen Ov39 of Onchocerca volvulus. J Exp Med. 1995;182:1121–31. doi: 10.1084/jem.182.4.1121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chippaux JP, Boussinesq M, Fobi G, Lafleur C, Audugé A, Banos MT, et al. Effect of repeated ivermectin treatments on ocular onchocerciasis: Evaluation after six to eight doses. Ophthalmic Epidemiol. 1999;6:229–46. doi: 10.1076/opep.6.4.229.4185. [DOI] [PubMed] [Google Scholar]
- 21.Winthrop KL, Proaño R, Oliva O, Arana B, Mendoza C, Dominguez A, et al. The reliability of anterior segment lesions as indicators of onchocercal eye disease in Guatemala. Am J Trop Med Hyg. 2006;75:1058–62. [PubMed] [Google Scholar]
- 22.Taylor HR, Munoz B, Keyvan-Larijani E, Greene BM. Reliability of detection of microfilariae in skin snips in the diagnosis of onchocerciasis. Am J Trop Med Hyg. 1989;41:467–71. doi: 10.4269/ajtmh.1989.41.467. [DOI] [PubMed] [Google Scholar]
- 23.Newell ED. Comparison of the use of skin scarification and skin biopsies to determine the prevalence and intensity of Onchocerca volvulus infection. Ann Trop Med Parasitol. 1997;91:633–42. doi: 10.1080/00034989760734. [DOI] [PubMed] [Google Scholar]
- 24.Diawara L, Traoré MO, Badji A, Bissan Y, Doumbia K, Goita SF, et al. Feasibility of onchocerciasis elimination with ivermectin treatment in endemic foci in Africa: First evidence from studies in Mali and Senegal. PLoS Negl Trop Dis. 2009;3:e497. doi: 10.1371/journal.pntd.0000497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ozoh G, Boussinesq M, Bissek AC, Kobangue L, Kombila M, Mbina JR, et al. Evaluation of the diethylcarbamazine patch to evaluate onchocerciasis endemicity in Central Africa. Trop Med Int Health. 2007;12:123–9. doi: 10.1111/j.1365-3156.2006.01750.x. [DOI] [PubMed] [Google Scholar]
- 26.Lavebratt C, Dalhammar G, Adamafio NA, Nykänen-Dejerud U, Mingarini K, Ingemarsson K, et al. A simple dot blot assay adaptable for field use in the diagnosis of onchocerciasis: Preparation of an adult worm antigen fraction which enhances sensitivity and specificity. Trans R Soc Trop Med Hyg. 1994;88:303–6. doi: 10.1016/0035-9203(94)90090-6. [DOI] [PubMed] [Google Scholar]
- 27.Chandrashekar R, Ogunrinade AF, Weil GJ. Use of recombinant Onchocerca volvulus antigens for diagnosis and surveillance of human onchocerciasis. Trop Med Int Health. 1996;1:575–80. doi: 10.1111/j.1365-3156.1996.tb00082.x. [DOI] [PubMed] [Google Scholar]
- 28.Lipner EM, Dembele N, Souleymane S, Alley WS, Prevots DR, Toe L, et al. Field applicability of a rapid-format anti-Ov-16 antibody test for the assessment of onchocerciasis control measures in regions of endemicity. J Infect Dis. 2006;194:216–21. doi: 10.1086/505081. [DOI] [PubMed] [Google Scholar]
- 29.Weil GJ, Steel C, Liftis F, Li BW, Mearns G, Lobos E, et al. A rapid-format antibody card test for diagnosis of onchocerciasis. J Infect Dis. 2000;182:1796–9. doi: 10.1086/317629. [DOI] [PubMed] [Google Scholar]
- 30.Ayong LS, Tume CB, Wembe FE, Simo G, Asonganyi T, Lando G, et al. Development and evaluation of an antigen detection dipstick assay for the diagnosis of human onchocerciasis. Trop Med Int Health. 2005;10:228–33. doi: 10.1111/j.1365-3156.2004.01384.x. [DOI] [PubMed] [Google Scholar]
- 31.Kita K, Shiomi K, Omura S. Advances in drug discovery and biochemical studies. Trends Parasitol. 2007;23:223–9. doi: 10.1016/j.pt.2007.03.005. [DOI] [PubMed] [Google Scholar]
- 32.Richard-Lenoble D, Chandenier J, Gaxotte P. Ivermectin and filariasis. Fundam Clin Pharmacol. 2003;17:199–203. doi: 10.1046/j.1472-8206.2003.00170.x. [DOI] [PubMed] [Google Scholar]
- 33.Cupp EW, Bernardo MJ, Kiszewski AE, Collins RC, Taylor HR, Aziz MA, et al. The effects of ivermectin on transmission of Onchocerca volvulus. Science. 1986;231:740–2. doi: 10.1126/science.3753801. [DOI] [PubMed] [Google Scholar]
- 34.Tagboto SK, Townson S. Onchocerca volvulus and O. lienalis: The microfilaricidal activity of moxidectin compared with that of ivermectin in vitro and in vivo. Ann Trop Med Parasitol. 1996;90:497–505. doi: 10.1080/00034983.1996.11813075. [DOI] [PubMed] [Google Scholar]
- 35.Cotreau MM, Warren S, Ryan JL, Fleckenstein L, Vanapalli SR, Brown KR, et al. The antiparasitic moxidectin: Safety, tolerability, and pharmacokinetics in humans. J Clin Pharmacol. 2003;43:1108–15. doi: 10.1177/0091270003257456. [DOI] [PubMed] [Google Scholar]
- 36.Hoerauf A, Mand S, Adjei O, Fleischer B, Büttner DW. Depletion of Wolbachia endobacteria in Onchocerca volvulus by doxycycline and microfilaridermia after ivermectin treatment. Lancet. 2001;357:1415–6. doi: 10.1016/S0140-6736(00)04581-5. [DOI] [PubMed] [Google Scholar]
- 37.Hoerauf A, Specht S, Büttner M, Pfarr K, Mand S, Fimmers R, et al. Wolbachia endobacteria depletion by doxycycline as antifilarial therapy has macrofilaricidal activity in onchocerciasis: A randomized placebo-controlled study. Med Microbiol Immunol. 2008;197:295–311. doi: 10.1007/s00430-007-0062-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Wanji S, Tendongfor N, Nji T, Esum M, Che JN, Nkwescheu A, et al. Community-directed delivery of doxycycline for the treatment of onchocerciasis in areas of co-endemicity with loiasis in Cameroon. Parasit Vectors. 2009;2:39. doi: 10.1186/1756-3305-2-39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Alleman MM, Twun-Danso NA, Thylefors BI. The Mectizan Donation Program-highlights from 2005. Filaria Journal. 2006;5:11. doi: 10.1186/1475-2883-5-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Collins RC, Gonzales-Peralta C, Castro J, Zea-Flores G, Cupp MS, Richards FO, Jr, et al. Ivermectin: Reduction in prevalence and infection intensity of Onchocerca volvulus following biannual treatments in five Guatemalan communities. Am J Trop Med Hyg. 1992;47:156–69. doi: 10.4269/ajtmh.1992.47.156. [DOI] [PubMed] [Google Scholar]
- 41.Dadzie Y, Neira M, Hopkins D. Final report of the Conference on the eradicability of Onchocerciasis. Filaria J. 2003;2:2. doi: 10.1186/1475-2883-2-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Sékétéli A. APOC at mid-point: So far so good. Ann Trop Med Parasitol. 2002;96:S3–4. [PubMed] [Google Scholar]
- 43.Furtado JM, Winthrop KL, Richards FO., Jr River Blindness: Reducing the risk in at-risk populations. Expert Rev Ophthalmol. 2011;6:33–41. [Google Scholar]
- 44.Osei-Atweneboana MY, Eng JK, Boakye DA, Gyapong JO, Prichard RK. Prevalence and intensity of Onchocerca volvulus infection and efficacy of ivermectin in endemic communities in Ghana: A two-phase epidemiological study. Lancet. 2007;369:2021–9. doi: 10.1016/S0140-6736(07)60942-8. [DOI] [PubMed] [Google Scholar]
- 45.Cupp E, Richards F, Lammie P, Eberhard M. Efficacy of ivermectin against Onchocerca volvulus in Ghana. Lancet. 2007;370:1123–5. doi: 10.1016/S0140-6736(07)61501-3. [DOI] [PubMed] [Google Scholar]
- 46.Turner JD, Tendongfor N, Esum M, Johnston KL, Langley RS, Ford L, et al. Macrofilaricidal activity after doxycycline only treatment of Onchocerca volvulus in an area of Loa loa co-endemicity: A randomized controlled trial. PLoS Negl Trop Dis. 2010;4:e660. doi: 10.1371/journal.pntd.0000660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hoerauf A, Specht S, Marfo-Debrekyei Y, Büttner M, Debrah AY, Mand S, et al. Efficacy of 5-week doxycycline treatment on adult Onchocerca volvulus. Parasitol Res. 2009;104:437–47. doi: 10.1007/s00436-008-1217-8. [DOI] [PubMed] [Google Scholar]
- 48.Specht S, Hoerauf A, Adjei O, Debrah A, Büttner DW. Newly acquired Onchocerca volvulus filariae after doxycycline treatment. Parasitol Res. 2009;106:23–31. doi: 10.1007/s00436-009-1624-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Specht S, Mand S, Marfo-Debrekyei Y, Debrah AY, Konadu P, Adjei O, et al. Efficacy of 2- and 4-week rifampicin treatment on the Wolbachia of Onchocerca volvulus. Parasitol Res. 2008;103:1303–9. doi: 10.1007/s00436-008-1133-y. [DOI] [PubMed] [Google Scholar]
- 50.Richards FO, Jr, Miri ES, Katabarwa M, Eyamba A, Sauerbrey M, Zea-Flores G, et al. The Carter Center's assistance to river blindness control programs: Establishing treatment objectives and goals for monitoring ivermectin delivery systems on two continents. Am J Trop Med Hyg. 2001;65:108–14. doi: 10.4269/ajtmh.2001.65.108. [DOI] [PubMed] [Google Scholar]
- 51.Richards FO, Jr, Amann J, Arana B, Punkosdy G, Klein R, Blanco C, et al. No depletion of Wolbachia from Onchocerca volvulus after a short course of rifampin and/or azithromycin. Am J Trop Med Hyg. 2007;77:878–82. [PubMed] [Google Scholar]
- 52.Hoerauf A, Marfo-Debrekyei Y, Büttner M, Debrah AY, Konadu P, Mand S, et al. Effects of 6-week azithromycin treatment on the Wolbachia endobacteria of Onchocerca volvulus. Parasitol Res. 2008;103:279–86. doi: 10.1007/s00436-008-0964-x. [DOI] [PubMed] [Google Scholar]
- 53.Debrah AY, Mand S, Marfo-Debrekyei Y, Larbi J, Adjei O, Hoerauf A. Assessment of microfilarial loads in the skin of onchocerciasis patients after treatment with different regimens of doxycycline plus ivermectin. Filaria J. 2006;5:1. doi: 10.1186/1475-2883-5-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Hoerauf A, Mand S, Volkmann L, Büttner M, Marfo-Debrekyei Y, Taylor M, et al. Doxycycline in the treatment of human onchocerciasis: Kinetics of Wolbachia endobacteria reduction and of inhibition of embryogenesis in female Onchocerca worms. Microbes Infect. 2003;5:261–73. doi: 10.1016/s1286-4579(03)00026-1. [DOI] [PubMed] [Google Scholar]
- 55. [Last cited on 2010 Dec 28]. Available from: http://www.paho.org/english/gov/cd/cd48-10-e.pdf .


