Abstract
Zoonotic filariasis due to Dirofilaria repens (D. repens) is prevalent in several regions of the world. In view of recent rise of human D. repens infections in Europe, Africa and Asia, it is considered an emerging zoonosis in these continents. Most of the documented cases of human dirofilariasis recorded in India had ocular infections, but very few subcutaneous dirofilariasis have been reported. We hereby report two cases of subcutaneous human dirofilariasis due to D.repens with varied clinical presentations.
Keywords: Dirofilariasis, Subcutaneous, Zoonosis
INTRODUCTION
The genus Dirofilaria includes various species that are natural parasites of dogs, cats, foxes, and wild mammals.[1] Dirofilariasis is a zoonotic infection which can be found world-wide. It is caused by D. repens, D. immitis, D. tenuis and D. ursi.[2] D. repens is commonly encountered in the subcutaneous tissue of dogs, foxes, and cats, while D. immitis in the right ventricle and pulmonary artery of the dogs and cats.[1] Human dirofilariasis due to D. repens has not been widely recognized in India, but there is probably a focus of infection in Kerala.[1] The disease is relatively common in Sri Lanka which is geographically close to southern India.[3] Culex, Aedes, and Anopheles mosquitoes are vectors for this parasite, which take up the microfilaria while feeding the blood of an infected host. Microfilaria develops in the malpighian tubules into the third stage larva and then migrates to the proboscis through the body cavity. The transmission takes place when a potential vector bites the dogs or other hosts including humans during a subsequent blood meal.[1] Most of the documented cases of human dirofilariasis recorded in India presented with ocular infections.[4–6] D. repens is the main causative agent of subcutaneous human dirofilariasis in Asia, including India.[7,8] We report two cases of subcutaneous human dirofilariasis affecting the face and neck region with varied clinical presentations.
CASE REPORTS
Case 1
A 40-year-old male, farmer hailing from northern Kerala, presented with a nodule over the cheek since 3 months. On examination the nodule measured less than 1 cm and was soft to firm in consistency. The complete hemogram was normal. As differential diagnosis, basal cell carcinoma was considered; hence the lesion was excised. Grossly, the tissue was gray white and granular. Microscopy revealed a smooth thick multilayered cuticle [Figure 1]. The outer most layers had prominent wavy longitudinal ridges, each separated from the next by a distance greater than the width of the ridge [Figure 2] and also transverse striations. The muscle layer below the cuticle was well developed and the body cavity showed uteri and intestinal tube. The surrounding soft tissue showed infiltration by eosinophils, lymphocytes, and occasional foreign body giant cells. Based on these features, the worm was morphologically identified as an adult female D. repens.
Figure 1.
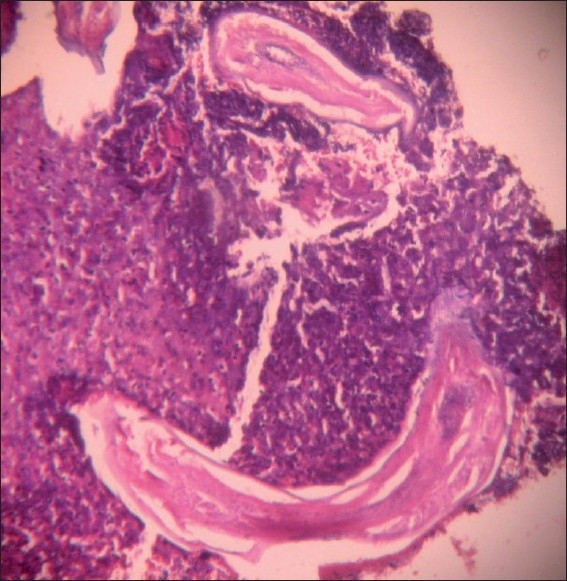
Histopathology of cheek mass showing the longitudinal section of Dirofilaria (H and E, ×100)
Figure 2.
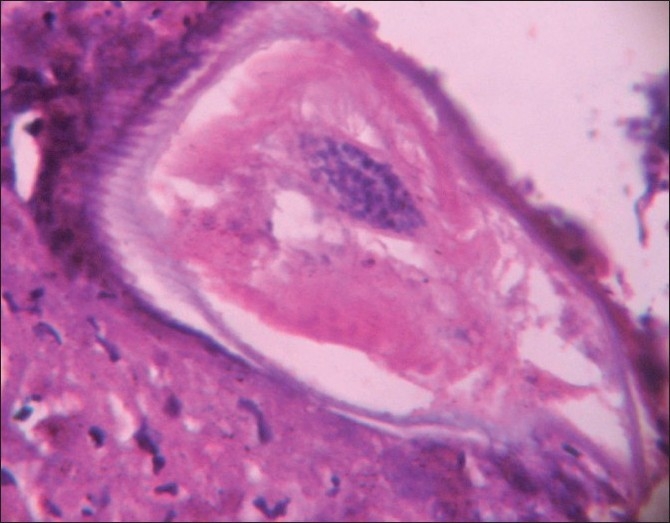
Cross section of Dirofilaria repens adult worm comprising of thick multilayered cuticle, transverse striations, and longitudinal wavy ridges (H and E, ×400)
Case 2
A 45-year-old male, presented with a slowly growing solitary firm swelling in the lateral side of neck since few weeks. Past history revealed his frequent visits to different parts of Kerala as a part of business work. On examination it was a firm subcutaneous swelling. His complete hemogram revealed eosinophilia and absolute eosinophil count of 0.95×109/l. As differential diagnosis, lipoma and schwannoma were considered. The lesion was excised and histopathology [Figure 3] showed features similar to case 1 with more dense collections of eosinophils, eosinophilic microabscess and Charcot Leyden crystals confirming D. repens.
Figure 3.
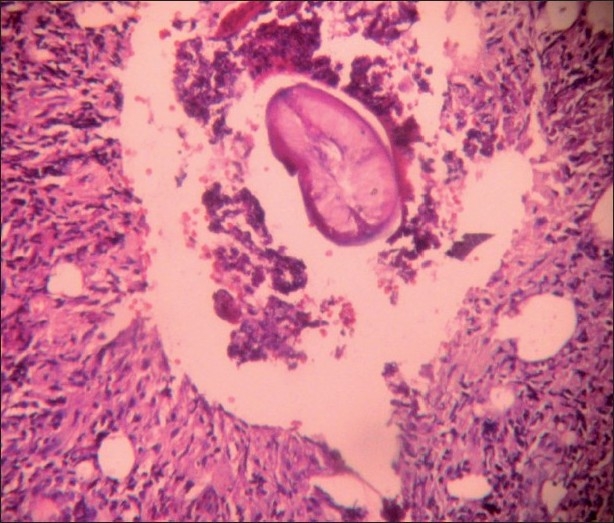
Histopathology of neck mass with the cross section of Dirofilaria and dense inflammatory background. (H and E, ×100)
DISCUSSION
The human dirofilariasis caused by D. repens, have been reported widely throughout Asia, Europe, and Africa with less reported cases in India.[4] The first reported case of human ocular dirofilariasis in India occurred in Kerala in 1976[7,9] and subcutaneous dirofilariasis caused by D. repens was recorded in 2004 in the same region.[7] The region Kerala is considered as endemic for dirofilariasis due to the climatic conditions and the presence of suitable vectors species.[1,8] Even though southern India is considered endemic for dirofilariasis,there are few case reports from the northern[5] or western parts[10] of india. Almost all human infections by D. repens are localized in the upper parts of the body, mostly in and around the eyes.[7] A review of the literature showed about 400 cases of subcutaneous dirofilariasis most of them reported from Southern and Eastern Europe, Asia, and Sri Lanka.[7,8,11]
D. repens is the most common causative agent of human dirofilariasis in India, however few cases caused by D. immitis have been reported.[8,10] Exact identification of the species may be possible after studying the fully matured worm. D. repens has a cuticle of 20 μm thickness, transverse striations, and large numbers of external longitudinal ridges. D. immitis can be differentiated from D. repens by the absence of longitudinal ridges and transverse striations.[7,11] In order to confirm the diagnosis of D. repens infection, DNA extraction followed by panfilarial polymerase chain reaction (PCR) may be performed.[11,12] In developing countries like India, owing to the low prevalence rate, PCR methods and standard antibody detecting tests are not available for the diagnosis of D. repens. Human dirofilariasis is detected many years after the initial infection, when the worm dies and is enveloped in a foreign body granuloma.[7] Patients usually present with single migratory nodule which may or may not be tender.[7] Both of our cases had nontender subcutaneous nodules. Surgical removal of the worm or the lesion is the treatment of choice. Most cases are diagnosed retrospectively, when the histopathological sections of biopsy or excision material are viewed.[7,8] There is no need for chemotherapy as microfilaraemia is extremely rare.[1,7,8] The few reported cases of meningoencephalitis secondary to D. repens microfilaraemia, were treated with the antihelminthic drug albendazole plus methylprednisolone and showed good response.[12] Our cases, had no evidence of microfilaraemia and after 1 year of follow up showed no evidence of recurrence. Human cases of dirofilariasis are most probably underreported because many of them remain undiagnosed or unpublished. Increased awareness of this infection among clinicians treating this condition, and development of the antibody screening system may improve the patient care and also increase the prevalence rate. Information is also lacking on which mosquito vectors are involved in transmission of D. repens in the area under study. In other geographic areas where human dirofilariasis is endemic, changes in climatic conditions (temperature, relative humidity, rainfall, rate of evaporation) favor the development of vector mosquitoes and the larval phase of the nematode in the vector. Medical awareness of infection risk is essential for a correct diagnosis, and the use of serologic analysis for D. repens somatic antigen merits further study as a diagnostic aid. Further monitoring of the situation in the endemic areas is needed to establish guidelines for preventive measures, including effective chemoprophylaxis in animals.[13] Dirofilariasis should be considered in the differential diagnosis of a single migratory or non- migratory subcutaneous swelling,especially if the patient is coming from an endemic area.[7,8]
CONCLUSION
Human infection with D. repens has been increasing in India and other parts of the world. Many of them remain undiagnosed or unpublished. Hence, there is need for increased awareness about this infection and diagnostic serological tests, which would improve the prevalence rate and patient care.
Acknowledgments
We kindly acknowledge Dr J H Makannavar, Senior Professor of Pathology for his valuable suggestion and guidance.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Sabu L, Devada K, Subramanian H. Dirofilariasis in dogs and humans in Kerala. Indian J Med Res. 2005;121:691–3. [PubMed] [Google Scholar]
- 2.Pampiglione S, Canestri Tritti G, Rivasi F. Human Dirofilariasis due to Dirofilaria (Nochtiella) repens: A review of world literature. Parassitologiath. 1995;37:149–93. [PubMed] [Google Scholar]
- 3.Dissanaike AS, Abeyewickreme W, Wijesundera MD, Weerasooriya MV, Ismail MM. Human dirofilariasis caused by Dirofilaria (Nochtiella) repens in Sri Lanka. Parassitologia. 1997;39:375–82. [PubMed] [Google Scholar]
- 4.Nadgir S, Tallur SS, Mangoli V, Halesh LH, Krishna BV. Subconjuntival dirofilariasis in India. Southeast Asian J Trop Med Public Health. 2001;32:244–6. [PubMed] [Google Scholar]
- 5.Gautam V, Rustagi IM, Singh S, Arora DR. Subconjunctival infection with Dirofilaria repens. Jpn J Infect Dis. 2002;55:47–8. [PubMed] [Google Scholar]
- 6.Sekhar HS, Srinivasa H, Batru BR, Mathai E, Shariff S, Macaden RS. Human ocular dirofilariasis in Kerala, Southern India. Indian J Pathol Microbiol. 2000;43:77–9. [PubMed] [Google Scholar]
- 7.Padmaja P, Kanagalakshmi, Samuel R, Kuruvilla PJ, Mathai E. Subcutaneous dirofilariasis in southern India: A case report. Ann Trop Med Parasitol. 2005;99:437–40. doi: 10.1179/36485905X36253. [DOI] [PubMed] [Google Scholar]
- 8.Singh R, Shwetha JV, Samantaray JC, Bando G. Dirofilariasis: rare case report. Indian J Med Microbiol. 2010;28:75–7. doi: 10.4103/0255-0857.58739. [DOI] [PubMed] [Google Scholar]
- 9.Joseph A, Thomas PG, Subramaniam KS. Conjunctivitis by Dirofilaria conjunctivae. Indian J Opthalmol. 1976;24:20–2. [PubMed] [Google Scholar]
- 10.Badhe BP, Sane SY. Human pulmonary dirofilariasis in India: A case report. J Trop Med Hyg. 1989;92:425–6. [PubMed] [Google Scholar]
- 11.Sathyan P, Manikandan P, Bhaskar M, Padma S, Singh G, Appalaraju B. Subtenons infection by Dirofilaria repens. Indian J Med Microbiol. 2006;24:61–2. doi: 10.4103/0255-0857.19899. [DOI] [PubMed] [Google Scholar]
- 12.Poppert S, Hodapp M, Krueger A, Hegasy G, Nieson WD, Kern WV, et al. Dirofilaria repens infection and concomitant meningoencephalitis. Emerg Infect Dis. 2009;15:1844–6. doi: 10.3201/eid1511.090936. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kramer LH, Vladimir V, Kartashev, Grandi G, Morchon R, Sergei AN, et al. Human subcutaneous dirofilariasis, Russia. Emerg Infect Dis. 2007;13:150–2. doi: 10.3201/eid1301.060920. [DOI] [PMC free article] [PubMed] [Google Scholar]


