Abstract
Purpose of review
This paper summarises the recent literature on the relation between cleaning exposures and respiratory health, in particular asthma, including reviews, epidemiological surveys, surveillance programmes and exposure studies. The authors also aimed to identify gaps in the current knowledge and to recommend future research on the topic.
Recent findings
A large international general population study showed an increased risk of new-onset asthma associated with cleaning work, with professional use of cleaning products, and with domestic use of cleaning sprays. Three surveillance studies confirm the recognition of occupational asthma cases among cleaners and among others who use cleaning products at work. Six workforce-based studies show that respiratory symptoms are partly work-related, and are associated with certain specific exposures including sprays, chlorine bleach and other disinfectants.
Summary
Recent studies have strengthened the evidence of asthma and other adverse respiratory effects in cleaning workers. Similar effects were seen in other settings where cleaning products are used such as healthcare professionals and homemakers. Both new-onset asthma and work-exacerbated asthma due to cleaning exposures may play a role. Exposure to cleaning sprays, chlorine bleach and other disinfectants may be particularly relevant. The predominant effect mechanisms remain largely unclear and may include both specific sensitisation and irritant-related features.
Keywords: Aerosols, Asthma, chemically induced, epidemiology, Detergents, adverse effects, Disinfectants, adverse effects, Homemaker Services, Humans, Irritants, adverse effects, Occupational Exposure, adverse effects
Keywords: Cleaning, cleaners, asthma, respiratory
INTRODUCTION
There is growing evidence that cleaners are at increased risk of asthma and other respiratory disorders. A systematic review published in this journal in 2006 [1] summarised the literature on this topic published in the period 2003 to 2005, and selected key articles published before 2003. The authors concluded that the evidence for an increased risk of asthma in cleaning workers was consistent and accumulating, and that a few specific occupational risk factors (products or tasks) had been suggested. However, they also noted that it was largely unclear which of the potentially important irritant and/or sensitising mechanisms play a predominant role.
The main aim of the present report is to concisely review the recent literature published since 2006 on the topic of respiratory health in cleaning workers. In addition, we wished to broaden the scope by including also relevant studies addressing more generally respiratory effects of cleaning products when used either at work in other occupations such as health care professionals, or in private households.
SEARCH STRATEGY
A Medline search was performed for articles using the key words (cleaning OR cleaners) AND (asthma OR respiratory) published in the period 2006 to 2009. We made a critical selection relevant for the topic, and added important references from the period 2006 to 2009 that were not identified by the Medline search. Finally, 21 papers published in international peer-reviewed journals were included: three reviews on occupational asthma [2–4], four papers from a population-based longitudinal survey [5–6,7*,8], three surveillance studies [9,10*,11], eight papers from six workforce-based studies [12–19], and three papers on the characterization of exposures in cleaners [20,21*,22].
REVIEWS ON OCCUPATIONAL ASTHMA
The proceedings of the Third Jack Pepys Workshop on Asthma in the Workplace [2] recognised a role of irritant exposures in asthma among cleaners. The relevance of accidental exposures was also noted, hypothesising that some cleaners may have had an initial accidental exposure and following that may have work-exacerbated asthma. A recent review of agents that can cause occupational asthma [3] included several cleaning agents, mostly disinfectants. Although the issue of multiple exposures in cleaning workers was stressed, the main focus was put on sensitising properties of cleaning agents and hence on asthma with a latency period. Nevertheless, it was recognised that many cleaning agents are respiratory irritants and could interact with sensitisers in the development of occupational asthma. Overall, authors considered that not much was known about the risk factors, exposure levels, clinical features, and pathogenetic mechanisms of asthma related to cleaning agents. A review focusing on mechanisms in occupational asthma considered only one form of irritant-induced occupational asthma: that without a latency period after acute exposures to high concentrations [4]. Cleaning agents associated with occupational asthma were classified as low molecular weight agents, inducing asthma following a non-IgE mediated mechanism.
POPULATION-BASED STUDIES
Epidemiological studies based on general population samples have several advantages over workforce-based studies. The most important are the possibility to evaluate similar exposures across occupations, better possibilities to control for health-related selection biases such as the Healthy Worker Effect, and the opportunity to assess the burden of occupational disease in the general population. The previous review [1] reported a relevant number of population-based studies that found higher prevalence rates of asthma or lower respiratory tract symptoms suggestive of asthma in current cleaning workers when compared to non-manual workers or to all other occupations. Interestingly, one of the studies also showed an increased risk of asthma in women who had left the cleaning profession, which was suggestive of an enduring effect after removal from exposure. Importantly, almost all of the reviewed epidemiological studies had a cross-sectional design, some of which following case-control approaches. Thus, the reported excess risks are likely to include both new-onset occupational asthma and work-exacerbated asthma. Evidence from longitudinal studies, indispensable to specifically address new-onset occupational asthma, was very limited. Only one population-based incident case-control study from Finland reported a non-significantly 42% increased risk of new-onset asthma in cleaning women as compared to professionals, clerks and administrative workers. Data for male cleaning workers were not reported.
We identified four recent papers from the longitudinal European Community Respiratory Health Survey (ECRHS II) that associated asthma with cleaning. Regarding occupation, Kogevinas and colleagues [5] reported a higher risk of new-onset asthma in 358 individuals that had been employed in cleaning and caretaking during the nine-year follow-up period as compared to 4,143 employed in professional, clerical or administrative jobs throughout during the follow-up (Relative Risk (RR) 1.7; 95% Confidence Interval (CI) 0.9–3.2). In addition, the authors applied an asthma-specific job exposure matrix (JEM) and the incidence of new-onset asthma for individuals with exposure to cleaning products across all occupations in the study was significantly higher than for those unexposed to any agent according to the JEM (RR 1.8; CI 1.0–3.2). An increased risk for incident asthma was also observed for the group of 291 nurses (RR 2.2; CI 1.3–4.0). A more specific analysis was reported in a separate paper using information from job-specific questionnaires that had been obtained for nurses in the ECRHS II interviews [6]. The highest risks of incident asthma were found among nurses who used ammonia, bleach and/or cleaning products in spray form at work. This large international study suggested that professional use of cleaning products in various occupations was related to new-onset asthma. It remained unclear to what extent such exposures also contributed to work-exacerbated asthma.
Using the same base population of the ECRHS II, the risk of new-onset asthma was also evaluated in relation to the use of household cleaning products among 3,503 adults who did the cleaning in their own homes and did not have asthma at baseline [7*]. Using three definitions of asthma, this study showed a significant 30% to 50% increased risk of incident asthma related to the use of products in spray-form at least once a week. This association was linked predominantly to the most commonly used air fresheners, glass cleaners, and furniture cleaning sprays, and the risk increased when frequency of use or number of different sprays increased. Among other products, not used in spray applications, weekly use of hypochlorite bleach was non-significantly associated with new-onset asthma (RR between 1.1 and 1.3). An additional cross-sectional analysis using the ECRHS II participants who did the cleaning in their homes showed that frequent use of bleach (that is, on four or more days per week) was associated with the prevalence of lower respiratory tract symptoms and possibly with bronchial hyperresponsiveness [8]. Perhaps paradoxically, this analysis also showed an inverse association of bleach use with the prevalence of atopic sensitisation to common environmental allergens, hay fever and allergic symptoms. The inverse association for atopic sensitisation was present for specific IgE to both indoor and outdoor allergens, was consistent in various subgroups including those without clinically apparent respiratory disease, and the effect was stronger when bleach was used more frequently. The authors hypothesised that this could be explained either by direct exposure to volatile chlorinated agents released during or shortly after bleach use, or indirectly due to a cleaner home environment.
SURVEILLANCE STUDIES
Registry reports of surveillance schemes are helpful in assessing the incidence of occupational diseases in a defined area in a certain time period, and to evaluate the causal agents. The previous review [1] included several occupational asthma surveillance studies from various countries that had reported cases of occupational asthma in cleaning workers, or related to professional use of cleaning products. We identified three new studies published in or after 2006 analysing cleaning workers or cleaning products using surveillance programmes.
A voluntary reporting system of occupational respiratory diseases in the autonomous region of Catalonia (Spain) showed 174 newly diagnosed cases of occupational asthma in the year 2002 (incidence 77 cases per million) accounting for 48% of all occupational respiratory diseases voluntarily reported [9]. For 15 cases (9%), cleaning products were suspected as being the causal agent. Interestingly, this surveillance system also notified 46 cases of acute inhalations (20 cases per million). Cleaning was the most frequently reported occupation (26%) being associated with acute inhalations. Follow-up on these cases could not be performed, and therefore it remained unclear how many of these cases developed chronic respiratory effects including Reactive Airways Dysfunction Syndrome (RADS).
A study from Alberta province (Canada) [10*] applied an interesting data linkage approach to estimate the extent and distribution of new-onset occupational asthma. The rationale was that using numbers of cases presenting for compensation typically underestimate the true incidence, since claims are not made for particularly less severe diseases, and in addition some important sectors are typically underrepresented. Workers’ Compensation Board claims for any reason in the period 1995 to 2004 were identified. Data were linked to physician billing data, and incident cases of asthma were identified as new onset adult asthma in the 12 months prior to a claim without asthma in the previous 3 years. Occupations were linked to the asthma-specific JEM mentioned earlier [5], and an incident case-referent analysis was performed. Exposure to low molecular weight cleaning products was associated with an increased risk of asthma in men (Odds Ratio (OR) 1.9; CI 1.3–2.7) but, however, not in women (OR 0.9; CI 0.8–1.1). No significantly increased risk for asthma in cleaning workers as such was reported.
The Sentinel Event Notification System for Occupational Risks (SENSOR) performed in four US states identified 2,995 cases of work-related asthma in the period 1993 to 2000, the majority classified as new-onset asthma. Educational services formed the third most frequently reported industry sector (9%) associated with work-related asthma. A specific analysis was performed for the 265 cases from the educational services industry [11]. Janitors, cleaners, and housekeepers accounted for 12% of the cases, with 84% classified as new-onset asthma. Across all occupations, cleaning products were reported as being the causal agents for 20% of all cases of work-related asthma. Most cleaning products were not specified, and among the specified products the most common were formaldehyde, graffiti remover, bleach, carpet cleaners and ammonia solution. This paper using SENSOR data added evidence for work-related asthma provided earlier regarding cleaning workers and cleaning products among health care workers, summarised in the previous review [1].
WORKFORCE-BASED STUDIES
Advantages of workforce-based studies over population-based studies are opportunities for more specific and less biased assessment of occupational exposure, and bigger numbers of individuals with specific exposures. We identified reports of workforce-based studies among cleaning workers and among other occupations that involve exposure to cleaning agents.
Cleaning workers
Obadia and co-workers [12] studied the prevalence of asthma and respiratory symptoms in 566 non-domestic cleaners and 587 other building workers from two union locals in Ontario province (Canada). Men were predominantly school cleaners, and the prevalence rate of physician-diagnosed asthma seemed to be higher than in male “other building workers” (OR 2.1; CI 0.9–4.8). However, when narrowing the definition to those with asthma onset after starting work, this association disappeared (OR 0.9; CI 0.4–2.3). Although no association for physician-diagnosed asthma was apparent in women, female cleaners were significantly more likely than other building workers to report any respiratory symptoms in the previous year (OR 2.6; CI 1.6–4.3). This was more pronounced for and work-related symptoms when defined as improving when away from work (OR 3.9; CI 2.1–7.4). The authors identified several specific tasks at risk for work-related symptoms among male cleaners, including waxing and wax stripping of floors, spot cleaning of carpets, oiling of furniture, cleaning tiles and cleaning grout. Another paper using the same study population reported that skin symptoms, particularly rash in the last year, were more common in cleaners, and that asthma and respiratory symptoms were more common among male cleaners with rash [13]. The authors concluded that there is a strong link between work-related symptoms of asthma and dermatitis among cleaners.
Massin and colleagues reported a study among 175 cleaning and disinfecting workers in the food industry, predominated by slaughterhouses [14]. Personal exposure levels of nitrogen trichloride and aldehydes were determined. The prevalence rates of chronic respiratory symptoms and asthma among the 175 exposed workers were not different from those in the control group comprising 70 non-exposed workers of small manufacturing plants. The prevalence of irritation symptoms (eye, nose, sore throat, dry cough) was significantly higher in exposed, particularly among those with the highest exposure levels or the longest exposure duration in the food industry. The prevalence of bronchial hyperresponsiveness to methacholine was non-significantly higher in exposed workers.
A cross-sectional study among 341 non-domestic cleaners employed by 32 cleaning service companies in Brazil included questionnaires, skin prick testing and pulmonary function tests [15]. Chlorine bleach was the most common agent related to both upper and lower airway symptoms. Work-related asthma or rhinitis increased monotonously with the number of years employed in cleaning. However, most of the tasks performed and products used showed similar frequencies for the workers with work-related asthma/rhinitis and those without symptoms.
A panel study was reported among 43 Spanish domestic cleaning women with asthma and/or chronic bronchitis [16]. Associations between specific daily cleaning exposures and respiratory symptoms and peak flow were evaluated. Lower respiratory tract symptoms were more common on working days, particularly when involving more than 8 hours of cleaning work. When taking into account both cleaning work in other people’s homes and cleaning their own home, it was found that the use of diluted bleach, degreasing sprays and air refreshing sprays were independently associated with a higher probability of having lower respiratory tract symptoms on the day the products were used. In addition, 11 out of 37 cases (30%) with adequate repeated peak flow data were identified as having occupational asthma when analysed using the Occupational Asthma System (OASYS) and/or reviewed by an expert. This study showed that a relevant proportion of cleaning workers with asthma could be diagnosed as having occupational asthma using internationally acknowledged methods, and suggested that occupational exposure to cleaning products can aggravate pre-existing obstructive lung disease.
Other occupations involving exposure to cleaning agents
Another study on short-term respiratory effects of cleaning exposures was done in US homemakers [17]. Associations between specific cleaning activities and the use of specific cleaning products and lower respiratory tract symptoms were evaluated in 25 female homemakers with asthma and 19 without asthma. Symptoms and peak flow were recorded daily within 30 minutes before and after home cleaning activities. Details of the cleaning tasks and products were recorded as well. The authors found that cleaning activities were related to short-term lower respiratory tract symptoms among asthmatic women, whereas no effects were apparent in non-asthmatic women. This could not be associated with specific cleaning exposures. In any case, results of this study are suggestive of exacerbations of in principle well-controlled asthma due to household cleaning work.
A study among 2,738 health care professionals from Texas [18] evaluated occupational risk factors for asthma in physicians, occupational therapists, nurses and respiratory therapists. After applying an industry-specific job exposure matrix, exposure to cleaning agents was associated with asthma. The prevalence rate of physician-diagnosed asthma with onset after entry into the health care profession was higher among workers exposed to agents used for instrument cleaning (OR 2.2; CI 1.3–3.7) and surface cleaners (OR 2.0; CI 1.2–3.4). In addition, the prevalence of respiratory symptoms consistent with bronchial hyperresponsiveness was higher among those with exposure to surface cleaners (OR 1.6; CI 1.2–2.1) and also associated with the report of a spill at work (OR 2.0; CI 1.3–3.2), the latter being suggestive of an acute inhalation to irritants. The prevalence of new-onset asthma was highest among the 448 nursing professionals, and a more detailed analysis within the latter subgroup highlighted the importance of exposure to cleaning and disinfecting products used for instrument and surface cleaning [19].
EXPOSURE STUDIES
Characterisation of exposure to cleaning chemicals in different occupational settings is important to understand determinants of exposure and hence to develop preventive workplace control measures, to contribute to the hypothesis generation of effect mechanisms, and to improve the quantification of exposure-response relationships in epidemiological studies. Apart from the study in the food industry mentioned earlier [14] we found reports of three studies in the period 2006–2009 that aimed at the characterisation of exposure to cleaning products.
Arif and co-workers [20] performed a qualitative study among 32 domestic and 47 industrial cleaning workers in the US. Domestic cleaners demonstrated significant skills deficit across each of these three themes as compared to industrial cleaners. Domestic cleaners reported more frequent exposure to respiratory irritants and sensitizers and also reported adverse respiratory symptoms as compared to industrial cleaners.
A detailed characterisation of exposures to cleaning products among US hospital cleaners was reported [21*]. Authors followed an integrated approach including workplace interviews, reviews of product Materials Safety Data Sheets and the scientific literature on adverse health effects to humans, reviews of physical/chemical properties of cleaning ingredients, and occupational hygiene observational analyses. They concluded that a combination of product evaluation and workplace exposure data is necessary to develop strategies for protecting workers from cleaning hazards. The conducted task based assessment allowed classification of cleaning tasks in different exposure categories (Figure 1), a strategy that can be employed by epidemiological investigations of the impact of cleaning on health.
Figure 1.
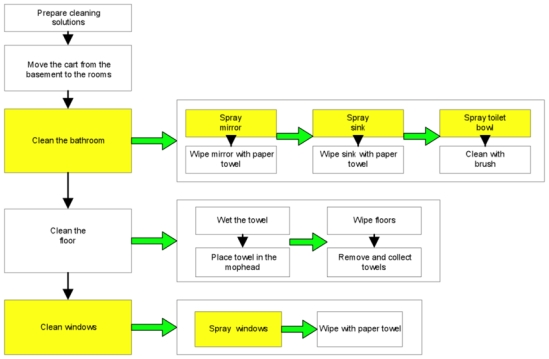
Process flow diagram of the tasks performed for patient room cleaning. The shaded boxes indicate cleaning tasks/steps with higher potential for inhalation exposure. Reproduced from [21*].
Finally, in an experimental study the airborne concentrations of glycol ethers (regulated toxic air contaminants) and terpenoids (including d-limonene which has sensitising properties) were measured during and after the application of five different cleaning products and air fresheners [22]. The authors found that the application of common cleaning products resulted in excessive exposures to potentially harmful volatile pollutants. Airborne levels of these chemical agents remained elevated for many hours after cleaning.
CONCLUSIONS
Studies reported in the last four years have strengthened the evidence of adverse respiratory effects, particularly asthma, in cleaning workers and otherwise in relation to the use of cleaning products (Table 1). The population at risk is particularly large; apart from cleaning workers many others are occupationally exposed to cleaning agents. This indicates a highly important public health issue, particularly when considering also the ubiquitous use of cleaning products in private homes. Cleaning-related asthma is a preventable disease and in order to develop prevention strategies it is indispensable to identify its specific risk factors and underlying mechanisms.
Table 1.
Summary of main findings on the relation between cleaning exposures and respiratory health from recent papers describing original studies
| Type and design of study | Study population | Main findings | Reference |
|---|---|---|---|
| Multi-centre population-based longitudinal study | General population samples from Europe, USA and Australia; including 358 cleaners, 291 nurses and 3501 homemakers. Years 1990–2003. |
|
5,6,7*,8 |
| Surveillance programme; voluntary notification of work-related respiratory diseases | 174 newly diagnosed cases of occupational asthma from Catalonia, Spain. Year 2002. |
|
9 |
| Data linkage of compensation claims and physician billing data | 12,554 new-onset asthma cases among 782,908 with claims in Alberta, Canada. Years 1995–2004. |
|
10* |
| Surveillance SENSOR | 265 educational service workers with work-related asthma from four USA states. Years 1993–2000. |
|
11 |
| Workforce-based cross-sectional study | 566 non-domestic cleaners and 587 other building workers from Ontario, Canada. |
|
12,13 |
| Workforce-based cross-sectional study | 175 cleaning and disinfecting workers in the French food industry and 70 non-exposed. | Risk of irritative symptoms increased with exposure (either intensity or duration). | 14 |
| Workforce-based cross-sectional study | 341 non-domestic cleaners employed in cleaning service companies from Brazil |
|
15 |
| Workforce-based; panel study | 43 Spanish domestic cleaners with asthma and/or chronic bronchitis | Lower respiratory tract symptoms were more common on working days, and independently associated with diluted bleach, degreasing sprays and air refreshing sprays
|
16 |
| Workforce-based; panel study | 25 homemakers with and 19 without asthma from USA |
|
17 |
| Workforce-based; cross-sectional study. | 2738 Health care professionals (448 nurses) from Texas, USA |
|
18,19 |
Both new-onset asthma and work-exacerbated asthma due to cleaning exposures may play a role, although more longitudinal surveys and specific studies in asthmatic populations are required. Both in domestic and non-domestic cleaners, the reviewed papers suggested a number of specific tasks and products that apparently increased the risk of asthma. The most important products that have been repeatedly reported include products in spray-form, chlorine bleach and other disinfectants. Many cleaning agents are respiratory irritants and some have sensitising properties. Relevant exposure levels to volatile compounds released from cleaning products have been reported to occur during common cleaning activities.
New studies should include a detailed exposure assessment and characterise effect mechanisms in relation to specific exposures. Both new-onset asthma, with and without latency periods, and work-exacerbated asthma should be considered. Rather than trying to answer the question whether the respiratory effects seen in cleaning workers or otherwise related to cleaning products are “real” or “true” (occupational) asthma, the authors judge it more relevant to characterise asthma phenotypes in order to help evaluating underlying effect mechanisms. The application of respiratory biomarkers and perhaps specific bronchial challenge testing can be helpful.
Acknowledgments
Part of the work reported in this review was supported by the Health Institute Carlos III/European Regional Development Fund (01-3058 and PI 06/1378), Afsset (Agence Française de Sécurité Sanitaire de l’Environnement et du Travail; EST-2009/1/15) and the Global Allergy and Asthma European Network (GA2LEN; Sixth EU Framework Programme for Research, FOOD-CT-2004-506378).
REFERENCES AND RECOMMENDED READING
* Papers of special interest
- 1.Jaakkola JJ, Jaakkola MS. Professional cleaning and asthma. Curr Opin Allergy Clin Immunol. 2006;6:85–90. doi: 10.1097/01.all.0000216849.64828.55. [DOI] [PubMed] [Google Scholar]
- 2.Tarlo SM, Malo JL. Third Jack Pepys Workshop on Asthma in the Workplace Participants. An official ATS proceedings: asthma in the workplace: the Third Jack Pepys Workshop on Asthma in the Workplace: answered and unanswered questions. Proc Am Thorac Soc. 2009;6:339–349. doi: 10.1513/pats.200810-119ST. [DOI] [PubMed] [Google Scholar]
- 3.Malo JL, Chan-Yeung M. Agents causing occupational asthma. J Allergy Clin Immunol. 2009;123:545–550. doi: 10.1016/j.jaci.2008.09.010. [DOI] [PubMed] [Google Scholar]
- 4.Maestrelli P, Boschetto P, Fabbri LM, Mapp CE. Mechanisms of occupational asthma. J Allergy Clin Immunol. 2009;123:531–542. doi: 10.1016/j.jaci.2009.01.057. [DOI] [PubMed] [Google Scholar]
- 5.Kogevinas M, Zock JP, Jarvis D, et al. Exposure to substances in the workplace and new-onset asthma: an International prospective population-based study (ECRHS-II) Lancet. 2007;370:336–341. doi: 10.1016/S0140-6736(07)61164-7. [DOI] [PubMed] [Google Scholar]
- 6.Mirabelli MC, Zock JP, Plana E, et al. Occupational risk factors for asthma among nurses and related healthcare professionals in an International study. Occup Environ Med. 2007;64:474–479. doi: 10.1136/oem.2006.031203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7*.Zock JP, Plana E, Jarvis D, et al. The use of household cleaning sprays and adult asthma: an international longitudinal study. Am J Respir Crit Care Med. 2007;176:735–741. doi: 10.1164/rccm.200612-1793OC. This study identified domestic use of cleaning sprays to be associated with new-onset asthma. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zock JP, Plana E, Antó JM, et al. Domestic use of hypochlorite bleach, atopic sensitization and respiratory symptoms in adults. J Allergy Clin Immunol. 2009;124:731–738.e1. doi: 10.1016/j.jaci.2009.06.007. [DOI] [PubMed] [Google Scholar]
- 9.Orriols R, Costa R, Albanell M, et al. Reported occupational respiratory diseases in Catalonia. Occup Environ Med. 2006;63:255–260. doi: 10.1136/oem.2005.022525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10*.Cherry N, Beach J, Burstyn I, et al. Data linkage to estimate the extent and distribution of occupational disease: new onset adult asthma in Alberta, Canada. Am J Ind Med. 2009;52:831–840. doi: 10.1002/ajim.20753. This study linked data from compensation claims and physician billing data. An increased risk of new-onset occupational asthma related to cleaning agents in men was reported. [DOI] [PubMed] [Google Scholar]
- 11.Mazurek JM, Filios M, Willis R, et al. Work-related asthma in the educational services industry: California, Massachusetts, Michigan, and New Jersey, 1993–2000. Am J Ind Med. 2008;51:47–59. doi: 10.1002/ajim.20539. [DOI] [PubMed] [Google Scholar]
- 12.Obadia M, Liss GM, Lou W, et al. Relationships between asthma and work exposures among non-domestic cleaners in Ontario. Am J Ind Med. 2009;52:716–723. doi: 10.1002/ajim.20730. [DOI] [PubMed] [Google Scholar]
- 13.Lynde CB, Obadia M, Liss GM, et al. Cutaneous and respiratory symptoms among professional cleaners. Occup Med (Lond) 2009;59:249–254. doi: 10.1093/occmed/kqp051. [DOI] [PubMed] [Google Scholar]
- 14.Massin N, Hecht G, Ambroise D, et al. Respiratory symptoms and bronchial responsiveness among cleaning and disinfecting workers in the food industry. Occup Environ Med. 2007;64:75–81. doi: 10.1136/oem.2005.026203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.de Fátima Maçãira E, Algranti E, Medina Coeli Mendonça E, Antônio Bussacos M. Rhinitis and asthma symptoms in non-domestic cleaners from the Sao Paulo metropolitan area, Brazil. Occup Environ Med. 2007;64:446–453. doi: 10.1136/oem.2006.032094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Medina-Ramón M, Zock JP, Kogevinas M, et al. Short-term respiratory effects of cleaning exposures in domestic cleaning women. Eur Respir J. 2006;27:1196–1203. doi: 10.1183/09031936.06.00085405. [DOI] [PubMed] [Google Scholar]
- 17.Bernstein JA, Brandt D, Rezvani M, et al. Evaluation of cleaning activities on respiratory symptoms in asthmatic female homemakers. Ann Allergy Asthma Immunol. 2009;102:41–46. doi: 10.1016/S1081-1206(10)60106-8. [DOI] [PubMed] [Google Scholar]
- 18.Delclos GL, Gimeno D, Arif AA, et al. Occupational risk factors and asthma among health care professionals. Am J Respir Crit Care Med. 2007;175:667–675. doi: 10.1164/rccm.200609-1331OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Arif AA, Delclos GL, Serra C. Occupational exposures and asthma among nursing professionals. Occup Environ Med. 2009;66:274–278. doi: 10.1136/oem.2008.042382. [DOI] [PubMed] [Google Scholar]
- 20.Arif AA, Hughes PC, Delclos GL. Occupational exposures among domestic and industrial professional cleaners. Occup Med (Lond) 2008;58:458–463. doi: 10.1093/occmed/kqn082. [DOI] [PubMed] [Google Scholar]
- 21*.Bello A, Quinn MM, Perry MJ, Milton DK. Characterization of occupational exposures to cleaning products used for common cleaning tasks--a pilot study of hospital cleaners. Environ Health. 2009;8:11. doi: 10.1186/1476-069X-8-11. This paper describes an integrated approach to characterise exposures to cleaning products, with an application in hospital cleaners. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Singer BC, Destaillats H, Hodgson AT, Nazaroff WW. Cleaning products and air fresheners: emissions and resulting concentrations of glycol ethers and terpenoids. Indoor Air. 2006;16:179–191. doi: 10.1111/j.1600-0668.2005.00414.x. [DOI] [PubMed] [Google Scholar]


