Abstract
Background
The decision to commit suicide may be impulsive, but lethal suicidal acts often involve planning and forethought. People who attempt suicide make disadvantageous decisions in other contexts, but nothing is known about the way they decide about the future. Can the willingness to postpone future gratification differentiate between individuals prone to serious, premeditated and less serious, unplanned suicidal acts?
Methods
Four groups of depressed participants aged 60+ made choices between smaller immediate and larger delayed monetary rewards: 15 who made high-lethality suicide attempts, 14 who made low-lethality suicide attempts, 12 who seriously contemplated suicide, and 42 people with depression but no history of suicidal thoughts. The reference group was 31 psychiatrically healthy elders.
Results
Individuals who had made low-lethality attempts displayed an exaggerated preference for immediate rewards compared to non-suicidal depressed and healthy controls. Those who had carried out high-lethality suicide attempts were more willing to delay future rewards, compared to low-lethality attempters. Better planned suicide attempts were also associated with willingness to wait for larger rewards. These effects were unchanged after accounting for education, global cognitive function, substance use disorders, psychotropic medications, and possible brain injury from attempts. Discount rates were correlated with having debt but were not significantly associated with income, hopelessness, depressive severity, premorbid IQ, age at first attempt, or choice of violent means.
Conclusions
While clinicians often focus on impulsivity in patients at risk for suicide, these data suggest that identifying biological characteristics and treatments for non-impulsive suicidal older people may be even more important.
Keywords: suicide, cognition, decision making, reward, depressive disorder, aged, time perception, executive function, choice behavior
Unlike the rates of cardiovascular disease, stroke, homicide, and automobile accidents, which in the US have all declined over the past decade, suicide rates have not (1). So far, suicidal behavior has defied efforts to develop neuroscience-based diagnostic tests and treatments. Inherited predisposition, genetic and epigenetic markers, neurochemical and neural circuitry alterations all point to a biological basis of suicidal behavior (2, 3). However, we lack useful knowledge about subgroups and the various pathways that lead to suicide. Suicidal behavior is very heterogeneous, as in the case of differences between attempted and completed suicide (4) or between individuals with single vs. multiple suicide attempts (5–7). This poorly understood heterogeneity frustrates attempts to characterize and target its biological substrates. For example, clinical observations suggest a distinction between impulsive and non-impulsive suicidal acts. Indeed, impulsive-aggressive traits are over-represented in suicide victims (8) and their families (9) and in suicide attempters (10). However, researchers have not been able to relate trait impulsivity to observable characteristics of suicidal behavior. Impulsive traits assessed through self-report do not seem to predict suicidal acts that are poorly planned or less determined (11, 12). Here, we propose a behavioral economic approach to distinguishing between impulsive and premeditated suicidal acts.
To gain insight into decision processes that lead to suicide, recent studies have examined the way suicidal individuals make decisions in other contexts, under risk and uncertainty (13, 14). However, nothing is known about a very important kind of decisions: those involving the future. Humans and animals generally work harder for immediate, compared to delayed rewards (“delay discounting”) (15). Two theories of neural mechanisms of delay discounting in humans have been proposed. According to the separate neural systems hypothesis, it depends on the balance of activity between frontolimbic reward circuitry and the frontal executive system involved in cognitive control (16, 17). The single system account relates delay discounting to the activity of a single network comprised of the ventral striatum, medial prefrontal and posterior cingulate cortex (18, 19). An exaggerated preference for immediate rewards has been previously related to impulsive traits and drug use (20). Perhaps surprisingly, this area has received minimal attention in mood disorders (21). In this framework, suicide can be viewed, in some cases, as an attempt to obtain immediate relief while foregoing all future rewards. We hypothesized that individuals who make less serious suicide attempts would show a preference for immediate rewards, while those who plan and carry out the most serious attempts would be more patient. We tested this hypothesis in people with late-life depression, a condition associated with serious and premeditated suicidal acts, by asking participants to make a series of choices between smaller immediate and larger delayed monetary rewards.
Methods and Materials
Study groups and characterization of suicidal behavior
To dissociate the effects of high-lethality and low-lethality suicide attempts from those of depression and suicidal ideation, we studied four groups of participants aged 60 and older with non-psychotic unipolar depression determined by SCID/DSMIV: 15 who made high-lethality suicide attempts, 14 who made low-lethality suicide attempts, 12 who seriously contemplated suicide (“ideators”), and 42 people with depression but no history of suicidal thoughts. All participants provided written informed consent. The University of Pittsburgh Institutional Review Board approved the study.
Suicide attempters had made a self-injurious act with the intent to die (22) AND presented with thoughts of suicide at the time of study enrollment. Suicide attempt history was verified by a psychiatrist (AYD or KSz), using all available information: participant’s report, medical records, information from the treatment team, and collateral information from family or friends. Significant discrepancies between these sources led to exclusion from the study. Medical seriousness of attempts was assessed using the Beck Lethality Scale (BLS) (23); for participants with multiple attempts, data for the highest-lethality attempt are presented. High-lethality attempts resulted in coma, need for resuscitation, unstable vital signs, penetrating wounds of abdomen or chest, third-degree burns, major bleeding, as defined by a score of ≥4 on the Beck Lethality Scale. Violent means – shooting, cutting, jumping, and hanging – were used in 3/14 low-lethality and 3/15 high-lethality suicide attempts; only one high-lethality attempt was by shooting. None of the attempts caused direct head injuries, however we assessed potential anoxic-ischemic or toxic brain injury, based on the BLS, medical records and the clinical interview. A psychiatrist (AYD or KSz) identified any attempts with a score of ≥4 on the BLS and any history of systemic hypotension >5 minutes or asphyxia or neurotoxic ingestion (e.g. polyatomic alcohols, methanol, or organic solvents); 3/15. For one individual it was impossible to completely rule out brain injury from a past attempt: we excluded her from the subsequent sensitivity analysis. In addition to lethality, we assessed suicidal intent associated with suicide attempts, using Beck’s Suicide Intent Scale, SIS (24). To assess whether the willingness to wait for larger rewards was associated with better planned suicide attempts, we used the planning subscale of the SIS (isolation, timing, precautions against discovery, not seeking help, final arrangements, preparation, and suicide note) (25). We also measured subjective lethal intent using the corresponding subscale of the SIS (25). Suicide attempters and suicide ideators presented with thoughts of suicide at the time of study enrollment. Suicide ideators had thoughts of suicide with a specific plan, serious enough to precipitate an inpatient admission or an increase in the level of outpatient care and no lifetime history of suicide attempt. Thus, these participants have seriously contemplated suicide and communicated this intention to their family or medical professionals. Participants with passive death wish, transient or ambiguous suicidal ideas were excluded from this group. Non-suicidal depressed elderly were included in the study to detect an association between delay discounting and suicidal behavior above and beyond effects of depression. These participants had no current or lifetime history of suicide attempts or suicidal ideation as established by clinical interview, review of medical records, SCID/DSMIV, and SSI (lifetime). Participants were excluded from this group if they had indirect self-destructive behaviors. Thirty-one control subjects were included as the reference group. They had to have no lifetime history of any psychiatric disorder as determined by SCID/DSMIV.
Cognitive and clinical characterization
Current global cognitive function was assessed with the Dementia Rating Scale (DRS), testing initiation/perseveration, attention, construction, conceptualization, and memory (26). Depression severity was measured with the 17-item Hamilton Rating Scale for Depression (HRSD) (27). Burden of physical illness was assessed with the Cumulative Illness Rating Scale adapted for Geriatrics (CIRS-G) (28). We obtained medication lists from pharmacy records. We measured the intensity of pharmacotherapy for the current episode of depression with the Antidepressant Treatment History Form (29). The ATHF score is based on antidepressant trial duration in addition to the dose and also reflects the use of augmenting agents (e.g. antipsychotics, lithium). In order to capture exposure to psychotropic medications not included in the ATHF score, we additionally assessed exposure to sedatives/hypnotics, drugs with anticholinergic activity, and opioid analgesics. Intra-class correlation coefficients measuring interrater reliability among our assessors were 0.95 for HRSD, 0.97 for CIRS-G, and 0.99 for the DRS. Income and debt items from the MacArthur Sociodemographic Questionnaire, reflecting real-life economic behaviors (30), were available on 34/114 participants. Wechsler Test of Adult Reading (WTAR; assessing premorbid IQ (31)), data were available for 64/114 participants. We used WTAR scores in a correlational analysis to test whether premorbid IQ was related to discount rates (32), possibly confounding group effects.
Inclusion/exclusion criteria and study procedures are described in detail in the Supplementary Material.
Delay discounting
To assess the preference for smaller immediate vs. larger delayed rewards, we used Kirby’s Monetary Choice Questionnaire (MCQ)(33). The MCQ presents 27 choices between delayed larger monetary rewards and smaller rewards available immediately. Discount rates are inferred using a Bayesian procedure as originally proposed by Kirby (33). The MCQ identifies discount rates for small ($25–$35), medium ($50–$60), and large ($75–$85) delayed-reward amounts; their geometric mean is the overall discount rate. Higher discount rates reflect a preference for immediate rewards. To capture low discount rates potentially seen in the elderly (34), we added 3 choices with very small differences between immediate and delayed rewards. One of the choices was later randomly selected, and the chosen immediate or delayed reward was delivered to the participant as a debit card. Discount rates on the MCQ correlate strongly with more comprehensive measures of delay discounting [r=0.82; (35)].
Statistical analysis
We used SPSS 18.0 (SPSS Inc., Chicago, IL) and MATLAB 7.6 (The MathWorks Inc., Natick, MA). All tests were two-sided. We first compared groups on demographic and clinical characteristics using ANOVA and chi-square tests. For these and all subsequent ANOVAs, we examined post-hoc contrasts using the Tukey HSD test. Discount rates were inferred using a Bayesian procedure and assuming hyperbolic discounting (Equation 1) as originally proposed by Kirby (33).
| Equation 1 |
where k is the discount rate. The overall discount rate was calculated as the geometric mean of discount rates for the three reward ranges. Discount rates were then natural log-transformed for normality. We examined group differences in the log-transformed discount rates (ln[k]) using ANOVA. We used ROC analyses to test how well ln(k) discriminates between high- and low-lethality attempters, seeking a cutoff with the best balance of sensitivity and specificity. To more intuitively represent discount rates, we calculated the delay that discounts the future reward by 50%, akin to its half-life (36). As can be seen from Equation 1, it is the inverse of k. Given the inherently non-linear distribution of Delay50 values, we tested group differences using the Kruskal-Wallis test. Our sensitivity analyses used log-transformed discount rates as the dependent variable and employed an ANOVA with education and global cognitive functioning as covariates and also ANOVAs excluding participants with lifetime substance use disorders, current substance use disorders, and those with possible brain injury from suicide attempts.
Results
Demographic, cognitive (Table 1) and clinical (Table 2) characteristics
Table 1.
Demographic and cognitive characteristics
| Controls (C) N=31 |
Non-Suicidal Depressed (D) N=42 |
Suicide ideators (I) N=12 |
Low-lethality suicide attempters (SA-L) N=14 |
High-lethality suicide attempters (SA-H) N=15 |
p | Post-hoc, Tukey HSD |
|
|---|---|---|---|---|---|---|---|
| Men, N (%) | 17 (54.8) | 15 (35.7) | 8 (66.7) | 5 (35.7) | 8 (53.3) | .22 | - |
| White, N (%) | 30 (96.8) | 35 (83.3) | 11 (91.7) | 10 (71.4) | 15 (100) | .21 | - |
| Age, years (SD) | 68.1 (5.8) | 70.3 (8.6) | 69.5 (8.7) | 66.1 (8.1) | 67.4 (7.1) | .38 | - |
| Years of Education, mean (SD) | 14.8 (3.2) | 14.3 (2.8) | 16.5 (2.6) | 12.6 (1.3) | 14.2 (3.3) | .016 | I>SA-L |
| Mini-mental status examination (N=106), mean (SD) | 28.5 (1.4) | 28.3 (1.6) | 27.8 (2.4) | 28.1 (1.9) | 27.6 (2.3) | .59 | - |
| Dementia rating scale (N=94), mean (SD) | 138.1 (2.7) | 133.3 (6.7) | 132.8 (9.4) | 135.0 (4.9) | 134.4 (5.2) | .021 | D<C |
Table 2.
Clinical characteristics
| Controls (C) N=31 |
Non-Suicidal Depressed (D) N=42 |
Suicide ideators (I) N=12 |
Low-lethality suicide attempters (SA-L) N=14 |
High-lethality suicide attempters (SA-H) N=15 |
p | Post-hoc, Tukey HSD |
|
|---|---|---|---|---|---|---|---|
| Lifetime substance use disorders, N (%) | - | 5 (11.9) | 1 (8.3) | 5 (35.7) | 3 (20) | .17 | - |
| Current substance use disorders, N (%) | - | 2 (4.8) | 1 (8.3) | 2 (14.3) | 3 (20) | .34 | - |
| Depressive Severity (HRS16), mean (SD) | 2.9 (2.0) | 13.5 (6.7) | 16.8 (8.1) | 16.4 (6.7) | 14.5 (6.6) | <.0001 | D=I=SA-L=SA-H>C |
| Burden of physical illness (Cumulative Illness Rating Scale adapted for Geriatrics) (N=105), mean (SD) | 7.2 (3.2) | 10.1 (3.8) | 7.4 (3.3) | 8.5 (2.7) | 6.67 (4.5) | .004 | D>C=SA-L |
| Intensity of Antidepressant Pharmacotherapy During Current Episode, Antidepressant Treatment History Form Score (N=93), mean (SD) | - | 1.9 (1.8) | 1.6 (2.4) | 3.1 (2.6) | 2.3 (2.2) | .40 | - |
| Receiving Sedatives/Hypnotics, N (%) | - | 17 (40.5) | 8 (66.7) | 5 (35.7) | 10 (66.7) | .14 | - |
| Receiving Anticholinergic Agents, N (%) | - | 11 (26.2) | 3 (25.0)) | 4 (28.6) | 3 (20.0) | .96 | - |
| Receiving Opioid Analgesics, N (%) | - | 9 (21.4) | 3 (25.0) | 2 (14.3) | 2 (13.3) | .82 | - |
| Scale for Suicidal Ideation, mean (SD) | - | - | 16.6 (7.5) | 18.6 (9.0) | 20.7 (9.2) | .49 | - |
| Age of first suicide attempt, mean (SD) | - | - | - | 49.8 (18.9) | 56.9 (19.6) | .33 | - |
| Age of highest-lethality suicide attempt, mean (SD) | - | - | - | 56.0 (19.2) | 63.4 (12.0) | .22 | - |
| Suicidal Intent Scale, mean (SD) | - | - | - | 14.5 (4.7) | 19.1 (4.2) | .032 | - |
| Planning subscale, Suicidal Intent Scale, mean (SD) | - | - | - | 5.0 (2.4) | 7.5 (3.4) | .014 | - |
The four groups were similar in race, gender, and MMSE scores (Table 1). Non-suicidal depressed participants had a higher burden of physical illness compared to high-lethality attempters (Table 2) and controls and displayed lower global cognitive function than controls (Table 1). Low-lethality attempters had a lower education than suicide ideators (Table 1). The three depressed groups did not differ significantly in the severity of depressive symptoms, psychotropic exposure, or in the prevalence of lifetime or current substance use disorders (Table 2). High-lethality attempters reported higher suicidal intent; 10/15 high-lethality attempters vs. 5/14 low-lethality attempters had made their first attempt after age 60 (χ2=2.8, p=.096).
Discounting of future monetary rewards and suicidal behavior
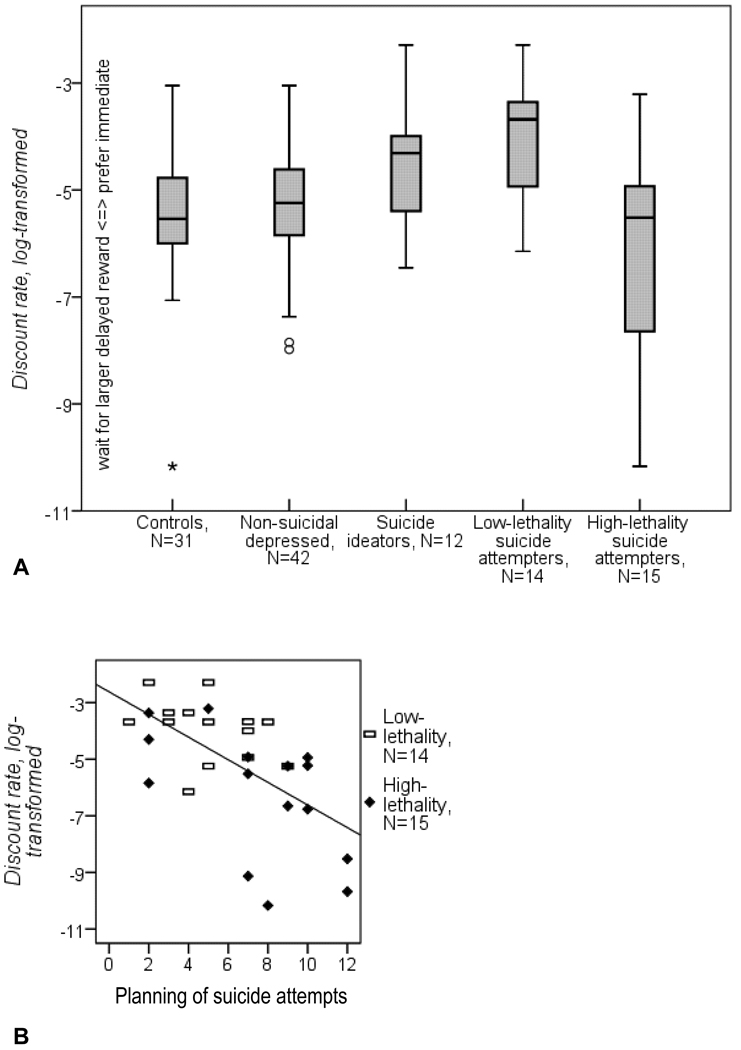
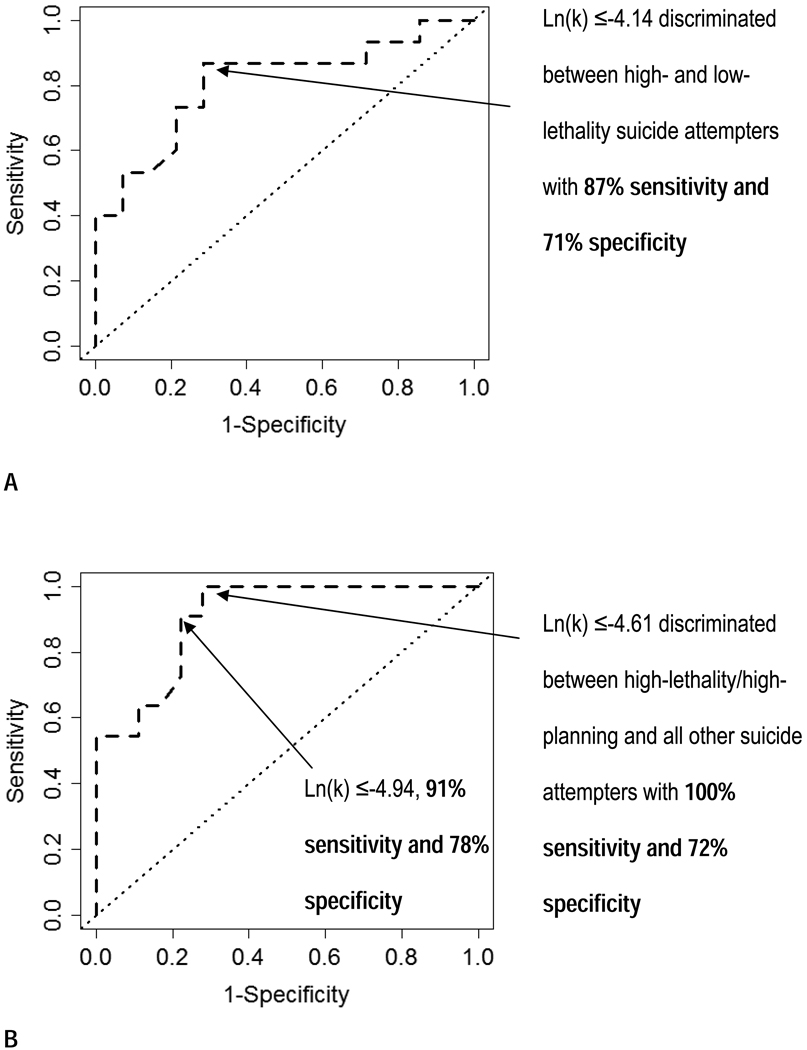
High-lethality attempters were more willing to delay future monetary rewards, compared to low-lethality attempters and suicide ideators (Fig. 1A). Moreover, higher levels of attempt planning were associated with a willingness to delay future rewards (Fig. 1B). In contrast, an exaggerated preference for immediate rather than larger delayed rewards was observed only in those who had either contemplated suicide or made low-lethality attempts (Fig. 1A), compared to the two control groups and to those who had made high-lethality attempts. The discount rate (ln[k] ≤-4.14) discriminated between high- and low-lethality suicide attempters with 87% sensitivity and 71% specificity (AUC=.81, Fig. 2a). In non-psychiatric controls, a delay of 282 days (geometric mean) decreased the subjective value of a future reward by half, compared to 211 days in non-suicidal depressed, 90 days in suicide ideators, 52 days in low-lethality attempters and 508 days, in high-lethality attempters (Kruskal-Wallis test: asymptotic p=.001). These effects were unchanged after accounting for education, global cognitive function, use of psychoactive substances, exposure to psychotropic medications, and possible brain injury from suicide attempts (see Supplementary Material).
Figure 1. Discounting of future rewards and suicidal behavior.
A. Low-lethality suicide attempters and suicide ideators showed the strongest preference for immediate rewards, followed by the two non-suicidal comparison groups. In contrast, high-lethality suicide attempters were more willing to wait for larger rewards (F[4,109]=5.9, p<.001, effect size: η2=0.18; Tukey HSD: low-lethality attempters> high-lethality attempters =depressed=controls; ideators> high-lethality attempters=controls).
B. Willingness to wait for larger rewards was associated with suicide attempts that were better planned (r=.60, p=0.001)
Figure 2. Discount rates discriminate subgroups of attempters: ROC analyses.
A. High- vs. low-lethality attempters. Area under the curve (AUC): .81. B. Post-hoc analysis: high-lethality/high-planning vs. all other attempters. AUC: .91.
Post-hoc analyses: low discount rates in high-lethality/high-planning attempters
Planning partly accounted for the heterogeneity in discount rates among high-lethality attempters evident in Fig. 1. In a post-hoc analysis, we examined delay discounting among the most determined attempters who had engaged in extensive planning and inflicted serious self-harm, arguably leaving no part of their suicidal act to chance. These 11 attempters with both high lethality (BLS≥4) and high planning (median split on the SIS planning subscale) displayed the lowest discount rates, below those of depressed controls (F(4,109)=9.5, p<.001, η2=0.26, high-lethality/high-planning attempters<non-suicidal depressed<other attempters=suicide ideators; other attempters>controls). Within suicide attempters, the model contrasting high-lethality/high-planning and all other attempts accounted for 50% (unadjusted) of the variance in discount rates vs. 31% (unadjusted) for the one contrasting high-lethality and low-lethality attempters. As two independent factors, lethality (F[1,25]=7.2, p=.013) and planning (F[1,25]=6.1, p=.020) were each related to discount rates, but did not explain more variance (51%, unadjusted). Ln(k) ≤-4.61 discriminated between high-lethality/high-planning and all other suicide attempters with 100% sensitivity and 72% specificity (AUC=.91, Fig. 2b).
Dimensions of suicidal behavior – lethality, planning, subjective intent, choice of violent means – as predictors of discount rates
When the four dimensions of suicidal behavior were examined in a single model, only lethality (F[1,23]=8.8, p=.007, η2=.28) and planning (F[1,23]=8.1, p=.009, η2=.26) were inversely related to discount rates, while subjective lethal intent (F[1,23]=2.9, p=.10, η2=.11) and choice of violent means (F[1,23]<0.1, p=.91, η2<.01) were not.
Exploratory analyses: debt, income, premorbid IQ, hopelessness, depressive severity, age at first suicide attempt, and impulsive approach to social problems
An exploratory analysis linking the preference for immediate rewards to real-life economic behaviors revealed that it was related to having debt (r=.36, p=.04), but not to income (r=−.05, p=.79). Premorbid IQ was not related to discount rates in this sample (r=−.09, p=.49). In suicide attempters, it was not related to hopelessness (r=.10, p=.61), severity of depression (r=−.14, p=.46), or age at first suicide attempt (r=.−28, p=.14). The score on the Impulsive/Careless subscale of the Social Problem Solving Questionnaire, which captures a narrow, hurried, and inadequate approach to social problems seen in some suicide attempters (37), was also not correlated with discount rates (r=.06, p=.63).
Discussion
Discounting of future monetary rewards discriminated between high- and low-lethality suicidal acts in depressed older adults and was inversely related to attempt planning. Our findings suggest that, in the context of depression and the stresses of old age (loss, disability, pain), at least two different pathways can lead to attempted suicide. In the first, impulsive individuals react to stressors with poorly planned and less serious suicidal acts. This behavior can be thought of as a failure of flexible cognitive control when integrating input from various modalities (reward/punishment magnitude, time, internal state)(32). It is conceivable that some parts of the distributed network involved in this integration – dorsolateral and ventrolateral prefrontal, anterior and posterior cingulate, posterior parietal cortex, and basal ganglia (16, 18, 38) – are altered in impulsive suicide attempters. Delay discounting may be a promising target for interventions aiming to prevent suicidal behavior in this group by reducing impulsivity: it is easily measured, can be studied in animals, and its neural underpinnings are increasingly well understood. Interventions aimed at enhancing cognitive control over choice behavior such as theta burst transcranial magnetic stimulation of the dorsolateral prefrontal cortex (39), stimulants (40), working memory training (41), and prospection (42) may reduce discount rates.
In the second, more ominous, scenario, people who carefully consider their future, plan and carry out serious suicidal acts. Low impulsivity by itself cannot credibly account for this behavior. However, our results resonate with findings of the association between obsessive-compulsive traits and suicide (43, 44), harking back to the cognitive rigidity theory (45). In addition to explaining these findings, a theory of cognitive substrates of serious, premeditated suicidal behavior will need to also account for impaired reward/punishment-based learning (13, 46) and broader cognitive dyscontrol (46, 47) observed in high-lethality attempters. This literature along with our clinical observations leads us to speculate that disruptions in high-order processes such as representation of complex action/reinforcement contingencies and hypothesis generation may account for the persistent investment in the suicidal plan as the only solution. In any case, several orthogonal neurocognitive vulnerabilities are likely to contribute independently to suicidal behavior and will need to be differentially targeted by treatment.
Impulsivity and suicidal behavior across the lifespan
The association of low discount rates with serious, premeditated suicide attempts in old age sheds new light on findings that impulsive traits are associated with completed suicide in younger but not in older people (8, 48) and uncovers one of the possible reasons for the high lethality of late-life suicidal behavior (49). Here, one may also draw a parallel between the willingness to wait for larger rewards and the trait of high conscientiousness, found to distinguish older suicide victims from suicide attempters (50).
Delay discounting in depression
Neither the presence of late-life depression nor its severity affected discount rates in our study, in contrast to an earlier finding of increased delay discounting in mid-life depression (21). We see two possible reasons for this discrepancy. First, Takahashi and colleagues did not report on suicidal behavior in their sample, and thus the group difference found in that study may have been predominantly driven by individuals with suicidal ideation and/or history of impulsive attempts. Second, it is possible that aging moderates the effect of depression on delay discounting (34).
Strengths and limitations
The five-group design allowed us to examine a range of late-life suicidal behavior, while controlling for effects of depression. Our study also benefited from careful characterization of suicidal behavior, clinical, and cognitive characteristics. Importantly, we were able to control for medication exposure and possible brain injury from suicide attempts – issues that often plague case-control studies of attempted suicide. The case-control design and small group sizes constitute the main limitations of our study. With respect to generalizability, our sample did not include, perhaps inevitably, suicidal elderly with severe cognitive impairment and psychotic depression – important antecedents of late-life suicide. Further, our finding of the lack of association between the choice of violent means and discount rates should be interpreted with caution. The caveat here is that the most important violent method – shooting – is censored in our sample, being mostly fatal.
In summary, behavioral impulsivity indexed by delay discounting relates to observable aspects of suicidal behavior: lethality and planning. Groups of suicidal individuals with high and low impulsivity may need to be considered separately in future biological studies of suicidal behavior and will likely require different therapeutic interventions.
Supplementary Material
Acknowledgments
This work was supported by NIMH grants K23 MH086620, K23 MH070471, P30MH52247, and T32 MH016804, Center for Injury Research and Control/Centers for Disease Control, the American Foundation for Suicide Prevention, the John A. Hartford Foundation, and the UPMC Endowment in Geriatric Psychiatry.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Financial disclosures
Dr. Sahakian has served as a consultant to Boehringer-Ingelheim, Cambridge Cognition, GlaxoSmithKline, Eli Lilly, Novartis, and Shire. Dr. Reynolds has received pharmaceutical supplies for his National Institutes of Health (NIH)–sponsored work from Forest Laboratories, Pfizer, Bristol-Myers Squibb, Wyeth, and Eli Lilly. Dr. Clark has served as a consultant to Cambridge Cognition. Dr. Forman was employed as a Staff Physician, Behavioral Health Service, Department of Verterans Affairs Medical Center, Pittsburgh, PA during the conduct of this study. The study contents do not represent the views of the Department of Veteran Affairs or the United States Government. All other authors have no biomedical financial interests or potential conflicts of interest.
References
- 1.Centers for Disease Control and Prevention; National Center for Injury Prevention and Control. Web-based Injury Statistics Query and Reporting System (WISQARS) www.cdc.gov/ncipc/wisqars.
- 2.van Heeringen C, Bijttebier S, Godfrin K. Suicidal brains: A review of functional and structural brain studies in association with suicidal behaviour. Neuroscience & Biobehavioral Reviews. doi: 10.1016/j.neubiorev.2010.08.007. In Press, Corrected Proof. [DOI] [PubMed] [Google Scholar]
- 3.Ernst C, Mechawar N, Turecki G. Suicide neurobiology. Prog Neurobiol. 2009;89:315–333. doi: 10.1016/j.pneurobio.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 4.Beautrais AL. Suicides and serious suicide attempts: two populations or one? Psychol Med. 2001;31:837–845. doi: 10.1017/s0033291701003889. [DOI] [PubMed] [Google Scholar]
- 5.Jeglic EL, Sharp IR, Chapman JE, Brown GK, Beck AT. History of family suicide behaviors and negative problem solving in multiple suicide attempters. Arch Suicide Res. 2005;9:135–146. doi: 10.1080/13811110590903981. [DOI] [PubMed] [Google Scholar]
- 6.Pagura J, Cox BJ, Sareen J, Enns MW. Factors associated with multiple versus single episode suicide attempts in the 1990–1992 and 2001–2003 United States national comorbidity surveys. J Nerv Ment Dis. 2008;196:806–813. doi: 10.1097/NMD.0b013e31818b6a77. [DOI] [PubMed] [Google Scholar]
- 7.Talbot NL, Duberstein PR, Cox C, Denning D, Conwell Y. Preliminary report on childhood sexual abuse, suicidal ideation, and suicide attempts among middle-aged and older depressed women. Am J Geriatr Psychiatry. 2004;12:536–538. doi: 10.1176/appi.ajgp.12.5.536. [DOI] [PubMed] [Google Scholar]
- 8.Dumais A, Lesage AD, Alda M, Rouleau G, Dumont M, Chawky N, et al. Risk factors for suicide completion in major depression: a case-control study of impulsive and aggressive behaviors in men. Am J Psychiatry. 2005;162:2116–2124. doi: 10.1176/appi.ajp.162.11.2116. [DOI] [PubMed] [Google Scholar]
- 9.McGirr A, Alda M, Seguin M, Cabot S, Lesage A, Turecki G. Familial aggregation of suicide explained by cluster B traits: a three-group family study of suicide controlling for major depressive disorder. Am J Psychiatry. 2009;166:1124–1134. doi: 10.1176/appi.ajp.2009.08111744. [DOI] [PubMed] [Google Scholar]
- 10.Beautrais AL, Joyce PR, Mulder RT. Access to firearms and the risk of suicide: a case control study. Australian & New Zealand Journal of Psychiatry. 1996;30:741–748. doi: 10.3109/00048679609065040. [see comment] [DOI] [PubMed] [Google Scholar]
- 11.Baca–Garcia E, Diaz–Sastre C, García Resa E, Blasco H, Braquehais Conesa D, Oquendo MA, et al. Suicide attempts and impulsivity. European Archives of Psychiatry and Clinical Neuroscience. 2005;255:152–156. doi: 10.1007/s00406-004-0549-3. [DOI] [PubMed] [Google Scholar]
- 12.Witte TK, Merrill KA, Stellrecht NE, Bernert RA, Hollar DL, Schatschneider C, et al. "Impulsive" youth suicide attempters are not necessarily all that impulsive. J Affect Disord. 2008;107:107–116. doi: 10.1016/j.jad.2007.08.010. [DOI] [PubMed] [Google Scholar]
- 13.Jollant F, Bellivier F, Leboyer M, Astruc B, Torres S, Verdier R, et al. Impaired decision making in suicide attempters. American Journal of Psychiatry. 2005;162:304–310. doi: 10.1176/appi.ajp.162.2.304. [DOI] [PubMed] [Google Scholar]
- 14.Dombrovski AY, Clark L, Siegle GJ, Butters MA, Ichikawa N, Sahakian BJ, et al. Reward/Punishment reversal learning in older suicide attempters. Am J Psychiatry. 2010;167:699–707. doi: 10.1176/appi.ajp.2009.09030407. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ainslie G. Impulse control in pigeons. Journal of the Experimental Analysis of Behavior. 1974;21:485–489. doi: 10.1901/jeab.1974.21-485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.McClure SM, Laibson DI, Loewenstein G, Cohen JD. Separate neural systems value immediate and delayed monetary rewards. Science. 2004;306:503–507. doi: 10.1126/science.1100907. [DOI] [PubMed] [Google Scholar]
- 17.McClure SM, Ericson KM, Laibson DI, Loewenstein G, Cohen JD. Time discounting for primary rewards. J Neurosci. 2007;27:5796–5804. doi: 10.1523/JNEUROSCI.4246-06.2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kable JW, Glimcher PW. The neural correlates of subjective value during intertemporal choice. Nat Neurosci. 2007;10:1625–1633. doi: 10.1038/nn2007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Kable JW, Glimcher PW. An "as soon as possible" effect in human intertemporal decision making: behavioral evidence and neural mechanisms. J Neurophysiol. 2010;103:2513–2531. doi: 10.1152/jn.00177.2009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Reynolds B. A review of delay-discounting research with humans: relations to drug use and gambling. Behav Pharmacol. 2006;17:651–667. doi: 10.1097/FBP.0b013e3280115f99. [DOI] [PubMed] [Google Scholar]
- 21.Takahashi T, Oono H, Inoue T, Boku S, Kako Y, Kitaichi Y, et al. Depressive patients are more impulsive and inconsistent in intertemporal choice behavior for monetary gain and loss than healthy subjects--an analysis based on Tsallis' statistics. Neuro Endocrinol Lett. 2008;29:351–358. [PubMed] [Google Scholar]
- 22.O'Carroll PW, Berman AL, Maris RW, Moscicki EK, Tanney BL, Silverman MM, et al. Beyond the Tower of Babel: a nomenclature for suicidology. Suicide Life Threat Behav. 1996;26:237–252. [PubMed] [Google Scholar]
- 23.Beck AT, Beck R, et al. Classification of suicidal behaviors: I. Quantifying intent and medical lethality. American Jounal of Psychiatry. 1975;132:285–287. doi: 10.1176/ajp.132.3.285. [DOI] [PubMed] [Google Scholar]
- 24.Beck AT, Shuyler D, Herman I. Development of suicidal intent scales. In: Beck AT, Resnik HLP, Lettieri DJ, editors. The prediction of suicide. Bowie, MD: Charles Press; 1974. pp. 45–56. [Google Scholar]
- 25.Mieczkowski TA, Sweeney JA, Haas GL, Junker BW, Brown RP, Mann JJ. Factor composition of the Suicide Intent Scale. Suicide Life Threat Behav. 1993;23:37–45. [PubMed] [Google Scholar]
- 26.Mattis S. Psychological Assessment Resources. Odessa, FL: 1988. Dementia Rating Scale (DRS) [Google Scholar]
- 27.Hamilton M. A rating scale for depression. J Neurol Neurosurg Psychiatry. 1960;23:56–62. doi: 10.1136/jnnp.23.1.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Miller MD, Paradis CF, Houck PR, Mazumdar S, Stack JA, Rifai AH, et al. Rating chronic medical illness burden in geropsychiatric practice and research: application of the Cumulative Illness Rating Scale. Psychiatry Res. 1992;41:237–248. doi: 10.1016/0165-1781(92)90005-n. [DOI] [PubMed] [Google Scholar]
- 29.Sackeim HA. The definition and meaning of treatment-resistant depression. J Clin Psychiatry. 2001;62 Suppl 16:10–17. [PubMed] [Google Scholar]
- 30.MacArthur Network on SES and Health. MacArthur Sociodemographic Questionnaire. http://www.macses.ucsf.edu/research/socialenviron/sociodemographic.php.
- 31.Wechsler D. Wechsler Test of Adult Reading. San Antonio, Texas: The Psychological Corporation; 2001. [Google Scholar]
- 32.Shamosh NA, Deyoung CG, Green AE, Reis DL, Johnson MR, Conway AR, et al. Individual differences in delay discounting: relation to intelligence, working memory, and anterior prefrontal cortex. Psychol Sci. 2008;19:904–911. doi: 10.1111/j.1467-9280.2008.02175.x. [DOI] [PubMed] [Google Scholar]
- 33.Kirby KN, Petry NM, Bickel WK. Heroin addicts have higher discount rates for delayed rewards than non-drug-using controls. J Exp Psychol Gen. 1999;128:78–87. doi: 10.1037//0096-3445.128.1.78. [DOI] [PubMed] [Google Scholar]
- 34.Green L, Myerson J, Ostaszewski P. Discounting of delayed rewards across the life span: age differences in individual discounting functions. Behavioural Processes. 1999;46:89–96. doi: 10.1016/S0376-6357(99)00021-2. [DOI] [PubMed] [Google Scholar]
- 35.Epstein LH, Richards JB, Saad FG, Paluch RA, Roemmich JN, Lerman C. Comparison between two measures of delay discounting in smokers. Exp Clin Psychopharmacol. 2003;11:131–138. doi: 10.1037/1064-1297.11.2.131. [DOI] [PubMed] [Google Scholar]
- 36.Kirby KN, Marakovic NN. Delay-discounting probabilistic rewards: Rates decrease as amounts increase. Psychonomic Bulletin & Review. 1996;3:100–104. doi: 10.3758/BF03210748. [DOI] [PubMed] [Google Scholar]
- 37.Gibbs LM, Dombrovski AY, Morse J, Siegle GJ, Houck PR, Szanto K. When the solution is part of the problem: problem solving in elderly suicide attempters. Int J Geriatr Psychiatry. 2009;24:1396–1404. doi: 10.1002/gps.2276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ballard K, Knutson B. Dissociable neural representations of future reward magnitude and delay during temporal discounting. Neuroimage. 2009;45:143–150. doi: 10.1016/j.neuroimage.2008.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Cho SS, Ko JH, Pellecchia G, Van Eimeren T, Cilia R, Strafella AP. Continuous theta burst stimulation of right dorsolateral prefrontal cortex induces changes in impulsivity level. Brain Stimul. 2010;3:170–176. doi: 10.1016/j.brs.2009.10.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.de Wit H, Enggasser JL, Richards JB. Acute administration of d-amphetamine decreases impulsivity in healthy volunteers. Neuropsychopharmacology. 2002;27:813–825. doi: 10.1016/S0893-133X(02)00343-3. [DOI] [PubMed] [Google Scholar]
- 41.Bickel WK, Yi R, Landes RD, Hill PF, Baxter C. Remember the Future: Working Memory Training Decreases Delay Discounting Among Stimulant Addicts. Biological Psychiatry. doi: 10.1016/j.biopsych.2010.08.017. In Press, Corrected Proof. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Peters J, Buchel C. Episodic future thinking reduces reward delay discounting through an enhancement of prefrontal-mediotemporal interactions. Neuron. 2010;66:138–148. doi: 10.1016/j.neuron.2010.03.026. [DOI] [PubMed] [Google Scholar]
- 43.Diaconu G, Turecki G. Obsessive-compulsive personality disorder and suicidal behavior: evidence for a positive association in a sample of depressed patients. J Clin Psychiatry. 2009;70:1551–1556. doi: 10.4088/JCP.08m04636. [DOI] [PubMed] [Google Scholar]
- 44.Harwood D, Hawton K, Hope T, Jacoby R. Psychiatric disorder and personality factors associated with suicide in older people: a descriptive and casecontrol study. Int J Geriatr Psychiatry. 2001;16:155–165. doi: 10.1002/1099-1166(200102)16:2<155::aid-gps289>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 45.Neuringer C. Rigid Thinking in Suicidal Individuals. J Consult Psychol. 1964;28:54–58. doi: 10.1037/h0045809. [DOI] [PubMed] [Google Scholar]
- 46.Keilp JG, Sackeim HA, Brodsky BS, Oquendo MA, Malone KM, Mann JJ. Neuropsychological dysfunction in depressed suicide attempters. American Journal of Psychiatry. 2001;158:735–741. doi: 10.1176/appi.ajp.158.5.735. [DOI] [PubMed] [Google Scholar]
- 47.Keilp JG, Oquendo MA, Stanley BH, Burke AK, Cooper TB, Malone KM, et al. Future Suicide Attempt and Responses to Serotonergic Challenge. Neuropsychopharmacology. 2008 doi: 10.1038/npp.2008.28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.McGirr A, Renaud J, Bureau A, Seguin M, Lesage A, Turecki G. Impulsive-aggressive behaviours and completed suicide across the life cycle: a predisposition for younger age of suicide. Psychol Med. 2008;38:407–417. doi: 10.1017/S0033291707001419. [DOI] [PubMed] [Google Scholar]
- 49.De Leo D, Padoani W, Scocco P, Lie D, Bille-Brahe U, Arensman E. Attempted and completed suicide in older subjects: results from the WHO/EURO Multicentre Study of Suicidal Behaviour. Int J Geriatr Psychiatry. 2001;16:300–310. doi: 10.1002/gps.337. [DOI] [PubMed] [Google Scholar]
- 50.Useda JD, Duberstein PR, Conner KR, Beckman A, Franus N, Tu X, et al. Personality differences in attempted suicide versus suicide in adults 50 years of age or older. J Consult Clin Psychol. 2007;75:126–133. doi: 10.1037/0022-006X.75.1.126. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.