Abstract
In type 2 diabetes mellitus, glucose homeostasis is tightly maintained through insulin secretion and insulin sensitivity. Therefore, finding an accurate method to assess insulin secretion and sensitivity using clinically available data would enhance the quality of diabetic medical care. In an effort to find such a method, we developed a computational approach to derive indices of these factors using a 2-h oral glucose tolerance test (OGTT). To evaluate our method, clinical data from subjects who received an OGTT and a glucose clamp test were examined. Our insulin secretion index was significantly correlated with an analogous index obtained from a hyperglycemic clamp test (r = 0.90, n = 46, p < 0.001). Our insulin sensitivity index sensitivity was also significantly correlated with an analogous index obtained from a hyperinsulinemic-euglycemic clamp test (r = 0.56, n = 79, p < 0.001). These results suggest that our method can potentially provide an accurate and convenient tool toward improving the management of diabetes in clinical practice by assessing insulin secretion and insulin sensitivity.
Keywords: Insulin secretion, Insulin sensitivity, Type 2 diabetes, Mathematical model, OGTT, Clinical use
Introduction
Insulin secretion and insulin sensitivity play a crucial role in glucose homeostasis; hence, assessing these factors in the care of type 2 diabetes (T2D) is important. The deregulation of these factors, which results in insufficient insulin secretion and activity, leads to hyperglycemia [1]; therefore, insulin secretion and insulin sensitivity are targeted by therapies for the treatment of diabetes [2].
Many mathematical models have been proposed for the assessment of insulin secretion and insulin sensitivity [3] by analyzing glucose tolerance tests such as the intravenous glucose tolerance test (IVGTT) and the oral glucose tolerance test (OGTT). Among these approaches, the minimal model proposed by Bergman et al. [4], which analyzes an IVGTT to assess insulin sensitivity, is one of the most notable. To introduce this concept into more general practice, several other models that use an OGTT have been reported. For example, mathematical models to analyze 11 blood samples obtained during a 5-h OGTT have been proposed and validated by comparison with direct measurement methods. The second-phase (or static) insulin secretion index proposed by Toffolo et al. [5] has been validated using a glucose clamp method [6], and the insulin sensitivity index proposed by Dalla Man et al. [7] has been validated using a glucose tracer method [8].
Modeling techniques that rely on data from a more convenient OGTT protocol, while maintaining reasonable assessment accuracy, would have a greater chance of application in clinical settings [9]. In particular, test results from 2-h OGTTs would be beneficial because the 2-h glucose level during an OGTT has been used as one of the diagnostic criteria for diabetes by the World Health Organization (WHO) [10].
The purpose of this study was to provide an accurate method for assessing insulin secretion and insulin sensitivity in T2D from clinically available data. For this purpose, we developed a computational method to assess these factors using only four blood samples obtained during a 2-h OGTT. The method is based on mathematical modeling combined with extrapolation and interpolation methods. Our indices for measuring insulin secretion and insulin sensitivity using OGTTs were compared with analogous indices obtained using a glucose clamp technique [11] in Japanese subjects with varying degrees of glucose tolerance.
Methods
Mathematical modeling
We considered plasma glucose and insulin levels to be the two major variables for this analysis; therefore, our mathematical model uses these variables only.
Oral glucose is absorbed from the intestines and passes through the liver before entering the systemic circulation. The liver functions as a buffer that keeps the glucose level stable by suppressing splanchnic glucose output (SGO) to the circulatory system. Therefore, to construct a model for interpreting OGTT results, a description of liver function is required.
The challenge in constructing our OGTT model was to develop a parametric description of SGO that reflects liver function. To describe SGO, a new function was introduced in our model. We adapted well-validated and reported models for the other aspects of functions.
Model to derive the insulin sensitivity index
Intravenously administered glucose circulates throughout the body immediately after ingestion. However, orally administered glucose is absorbed from the intestines and first passes through the liver before entering the systemic circulation. This first-pass effect of the liver must be considered in a model that assesses insulin sensitivity using OGTTs. For this reason, SGO was incorporated into our model. A function, R ΔSGO, that represents the varying rate of SGO was introduced and coupled with the classical minimal model, which describes glucose kinetics without SGO and is applicable to IVGTT studies [4]. The general formulation is described as follows:
 |
where G (mg dl−1) is the plasma glucose concentration, I (μU ml−1) is the plasma insulin concentration, X (min−1) is a variable in a remote insulin compartment where insulin is active in accelerating glucose disappearance, R ΔSGO (mg dl−1 min−1) is the varying SGO rate after an oral glucose load, and p G1 (min−1), p G2 (min−1), and p G3 (μU−1 ml min−2) are rate parameters. A subscript in parentheses represents a value at a time after the oral glucose load, and a zero subscript (e.g., I (0) and G (0)) represents a value at time 0. By defining insulin sensitivity as the quantitative influence of insulin on increasing the disappearance of glucose, the insulin sensitivity index is deductively given by p G3/p G2. The explicit definition of X, the parameters, and the derivation of the index are found in reference [4].
In healthy subjects, SGO is maintained within a low range by a prompt increase in glucose uptake and a suppression of glucose production. In T2D, some of these functions are disordered, and these dysfunctions contribute to hyperglycemia [12–16]. It is known that insulin is one of the key factors responsible for the hepatic functions of glucose uptake and suppression; however, there are other key factors involved, such as the portal signal (the difference in glucose concentration between the portal vein and the hepatic artery), whose regulatory mechanisms have not yet been clearly defined [12–16]. As was mentioned, the present requirement is not to describe the details of hepatic glucose regulation but to describe SGO. After that is done, we can model R ΔSGO to satisfy the following relation between the state of hepatic function and SGO. In T2D (in which there is dysfunction in hepatic glucose regulation), the increase in the SGO rate is assumed to be larger because the increase in hepatic glucose uptake and suppression of hepatic glucose production are smaller than in healthy subjects. Thus, we assumed that the maximum value for SGO is larger, and that peak SGO occurs earlier in T2D. Most of the oral glucose absorbed from the intestines appears in the plasma within 2 or 3 h after administration [16]. For this reason, SGO returns to basal levels regardless of the state of hepatic glucose function (i.e., R ΔSGO converges to within a small and narrow range after 2 h). We modeled R ΔSGO to satisfy the above requirements for peak value, peak time, and convergence of SGO. R ΔSGO is defined by the following equation:
 |
k W (kg−1 min−1 mg−1 dl) is a constant, W (kg) is the weight, the parameter α (min) is the scale parameter, the parameter β (dimensionless) is the shape parameter, and f w (min−1) is the Weibull density function [17]. In pharmacokinetics, this density function is widely used to describe drug absorption following oral administration. As long as the two parameters α and β are positive, the area under the glucose absorption curve (AUC) will increase exponentially with time and asymptotically approach 1 as time approaches infinity. To satisfy the assumptions about SGO, f w is multiplied by the inverse of p G4 and p G5 in the expression for R ΔSGO. The expression thus defined satisfies the assumptions and can describe a wide variety of SGO functions (Figs. 1, 2).
Fig. 1.
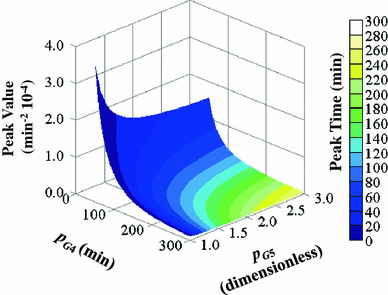
Peak values and peak time of 
Fig. 2.
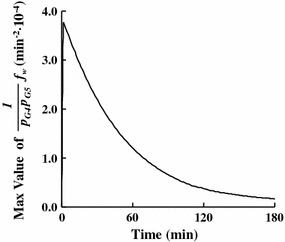
Max values of  The ranges of the parameters are from 50 to 300 (min) for p
G4 and from 1 to 3 (dimensionless) for p
G5
The ranges of the parameters are from 50 to 300 (min) for p
G4 and from 1 to 3 (dimensionless) for p
G5
Model to derive the insulin secretion index
Pancreatic insulin secretion (R I) can be described as the sum of two components: dynamic insulin secretion (R I1) and static insulin secretion (R I2). This sum is based on a previously reported OGTT minimal model [5]. The rate of change in plasma insulin concentration (dI/dt) is represented by the sum of R I, and the insulin circulation rate is calculated from a single-compartment model with a rate parameter p I1 (min−1) for insulin disappearance,
 |
 |
R I1 (μU ml−1 min−1) represents the secretion of rapidly releasable insulin stored in β-cells in response to elevations in the glucose level, according to the following equation:
 |
where the parameter p I2 (μU ml−1 mg−1 dl) describes the sensitivity of dynamic insulin secretion by the β-cells.
R I2 (μU ml−1 min−1) represents the secretion of newly recruited insulin in response to an elevated glucose level, according to the following equation (with R Ib = 0):
 |
The parameter p I4 (μU ml−1 mg−1 dl min−1) describes the sensitivity of static insulin secretion by β-cells to an elevated glucose level with a time constant parameter p I3 (min).
R
I is always non-negative, and when 

Clinical data collection
To evaluate our insulin secretion index, we retrospectively studied 46 Japanese subjects who had received an OGTT and a hyperglycemic clamp (HGC) within 1 week of each other. The subjects had the following characteristics: 33 male, 13 female; 50.4 ± 12.0 (mean ± SD) years old; body mass index (BMI) 26.2 ± 6.1 kg m−2; and 9 with normal glucose tolerance (NGT), 5 with impaired glucose tolerance (IGT), and 32 with T2D. To evaluate our insulin sensitivity index, we retrospectively studied 82 Japanese subjects who had received an OGTT and a hyperinsulinemic-euglycemic clamp (HIC) within 1 week of each other. These subjects had the following characteristics: 79 subjects after exclusions; 57 male, 22 female; 53.1 ± 13.4 years old; BMI 25.6 ± 5.1 kg m−2; and 10 with NGT, 11 with IGT, and 58 with T2D. To assess insulin sensitivity in all areas other than the liver in the HIC, the insulin infusion rate was adjusted to achieve a serum insulin concentration of 100 μU ml−1; because of the possibility of insufficient inhibition of hepatic glucose production, we eliminated 3 cases with a steady-state insulin concentration under 50 μU ml−1 during the HIC [12]. Clinical and metabolic characteristics are summarized in Table 1. All of these clinical tests were performed at the Osaka University Graduate School of Medicine (46 cases) or the Kobe University Graduate School of Medicine (36 cases).
Table 1.
Characteristics of the subjects
| Subjects used in the evaluation of insulin secretion | Subjects used in the evaluation of insulin sensitivity | |||||||
|---|---|---|---|---|---|---|---|---|
| All | NGT | IGT | T2D | All | NGT | IGT | T2D | |
| n | 46 | 9 | 5 | 32 | 79 | 10 | 11 | 58 |
| Age (years old) | 50.4 ± 12.0 | 45.8 ± 14.3 | 46.4 ± 9.1 | 52.4 ± 11.5 | 53.1 ± 13.4 | 47.8 ± 15.0 | 49.7 ± 14.2 | 54.7 ± 12.9 |
| Sex (male/female) | 33/13 | 8/1 | 3/2 | 22/10 | 57/22 | 9/1 | 8/3 | 40/18 |
| BMI (kg m−2) | 26.2 ± 6.1 | 28.7 ± 8.6 | 26.0 ± 5.8 | 25.5 ± 5.3 | 25.6 ± 5.1 | 28.0 ± 8.4 | 26.3 ± 4.8 | 25.1 ± 4.3 |
| G (0) (mg dl−1) | 113.7 ± 25.1 | 83.9 ± 8.1 | 93.0 ± 13.9 | 125.4 ± 20.1 | 112.6 ± 21.6 | 84.4 ± 7.8 | 98.2 ± 13.8 | 120.1 ± 18.9 |
| G (30) (mg dl−1) | 205.7 ± 54.0 | 138.8 ± 29.8 | 179.6 ± 35.2 | 228.7 ± 43.5 | 202.9 ± 46.7 | 143.8 ± 32.3 | 188.0 ± 49.8 | 216.0 ± 39.5 |
| G (60) (mg dl−1) | 258.8 ± 78.0 | 157.2 ± 43.3 | 191.4 ± 21.1 | 297.9 ± 54.5 | 253.7 ± 64.8 | 157.5 ± 40.9 | 213.9 ± 35.8 | 277.8 ± 52.3 |
| G (120) (mg dl−1) | 254.8 ± 105.8 | 103.4 ± 19.0 | 154.2 ± 14.2 | 313.0 ± 65.9 | 254.4 ± 90.6 | 105.5 ± 19.0 | 162.1 ± 22.6 | 297.6 ± 60.4 |
| I (0) (μU ml−1) | 6.8 ± 6.6 | 11.5 ± 12.7 | 6.0 ± 2.5 | 5.7 ± 3.8 | 6.3 ± 5.8 | 10.7 ± 12.2 | 5.9 ± 4.3 | 5.6 ± 3.8 |
| I (30) (μU ml−1) | 35.1 ± 51.1 | 94.0 ± 89.6 | 35.5 ± 27.6 | 18.5 ± 17.9 | 28.7 ± 40.9 | 91.4 ± 84.9 | 29.5 ± 24.1 | 17.8 ± 15.5 |
| I (60) (μU ml−1) | 43.7 ± 50.5 | 110.0 ± 75.8 | 46.3 ± 23.3 | 24.7 ± 22.2 | 37.2 ± 41.1 | 104.2 ± 73.8 | 40.2 ± 24.4 | 25.1 ± 20.1 |
| I (120) (μU ml−1) | 44.0 ± 39.7 | 79.0 ± 61.9 | 56.3 ± 32.1 | 32.2 ± 25.3 | 41.1 ± 33.6 | 75.0 ± 59.7 | 44.2 ± 30.0 | 34.7 ± 24.1 |
| SSIHGC (μU ml−1) | 24.4 ± 24.8 | 56.4 ± 37.8 | 27.8 ± 9.0 | 14.9 ± 10.9 | ||||
| GIR/SSIHIC (mg kg−1 min−1 μU−1 ml) | 0.064 ± 0.034 | 0.074 ± 0.046 | 0.081 ± 0.032 | 0.059 ± 0.030 | 0.063 ± 0.032 | 0.072 ± 0.044 | 0.079 ± 0.037 | 0.059 ± 0.027 |
The G and I represent glucose and insulin concentrations during the OGTT, respectively. A subscript in parentheses represents a value at a time (min) after the oral glucose load. The SSIHGC and SSIHIC represent steady-state insulin concentrations during the HGC and the HIC, respectively. The GIR represents the steady-state glucose infusion rate during the HIC
The clinical protocol was approved by the ethics committee of each institution, and written informed consent was obtained from all subjects.
For the OGTTs, the standard WHO procedures were followed [10]. In brief, after a 12-h overnight fast, 75 g of glucose was given orally. Blood samples were collected at 0, 30, 60, and 120 min after the ingestion of the glucose, and the plasma glucose and serum insulin concentrations were measured.
For the glucose clamp methods, after a 12-h overnight fast, and before the start of the HGC or HIC, an artificial pancreas was used. An intravenous line was inserted into an antecubital vein for glucose and insulin administration. A second intravenous line was inserted into a vein in the contralateral hand for blood collection. During the clamp, blood samples were collected at 1- to 10-min intervals, and plasma glucose and serum insulin concentrations were measured.
For the HGC, exogenous glucose was infused intravenously by automatically adjusting the infusion rate to attain a plasma glucose concentration of 200 mg dl−1 for 90 min. All of the HGCs were performed at Osaka University.
For the HIC, the infusion rate of regular insulin was fixed at 1.1 mU kg−1min−1 to attain a serum insulin concentration of 100 μU ml−1, and exogenous glucose was infused to maintain a plasma glucose concentration of 90 mg dl−1 for at least 90 min.
The plasma glucose concentrations were determined using the glucose oxidase method. The serum insulin concentrations were determined using a sandwich enzyme immunoassay system. Spherelight Insulin (Sanyo Chemical Industries Ltd., Japan) was used at the Osaka University Graduate School of Medicine for insulin measurement. E-test Tosoh II (IRI) (Tosoh Co., Japan) was used at the Kobe University Graduate School of Medicine. An artificial endocrine pancreas (STG-22; Nikkiso Co., Japan) was used for the glucose clamp studies. The tested values were properly calibrated by each facility.
Individual parameter estimation from OGTT data
To estimate the parameters in the OGTT model, the reference values for the model input were extrapolated and interpolated from the observed glucose and insulin values. The glucose and insulin values at 300 min were assumed to have returned to the baseline levels, based on results reported from 5-h OGTTs [9, 18]. The values at 180 min were extrapolated from those at 0, 30, 60, and 120 min using a support vector machine [19] and following a previously reported procedure [20]. For this interpolation, a piecewise cubic Hermite interpolation [21, 22] was used as one of the interpolation methods. This method generates a curve which passes through the input values and does not overshoot between them. The parameters related to insulin secretion (p I) were estimated by minimizing the residual sum of squares of the insulin level between the reference and the model. The parameters related to glucose metabolism (p G) were estimated by minimizing the residual sum of glucose levels between the reference and the model. The parameter sets of p I and p G were independently estimated. The dG/dt and dI/dt were calculated by the interpolated functions. A brute-force algorithm was used to estimate them. This parameter estimation did not require a specific optimization algorithm, and comparable parameters can be obtained using other approaches, such as a genetic algorithm.
The parameters estimated for the individual cases were p G3, p G4, p G5, p I2, p I3, and p I4. The ranges for the estimated parameters were from 0.02 to 40 (μU−1 ml min−2 10−6) for p G3, from 50 to 300 (min) for p G4, from 1 to 3 (dimensionless) for p G5, from 0 to 80 (μU ml−1 mg−1 dl) for p I2, from 1 to 300 (min) for p I3, and from 0 to 600 (μU ml−1 mg−1 dl min−1) for p I4.
The other parameters were fixed to the mean population values found in the literature. The constant k W used in the R ΔSGO equation was set using the results of a direct SGO measurement that utilized a glucose tracer approach during an OGTT. The values and sources were as follows: p G1 = 0.014 (min−1) [7, 23], p G2 = 0.012 (min−1) [8], p I1 = 0.19 (min−1) [24], and k W = 2.0 (kg−1 mg−1 dl min−1 10−7) [16].
The parameters estimated for the individual cases were selected on the basis of their usefulness for assessing the pathophysiology underlying T2D. Other parameters that were fixed as constants in the model can have individual variation, which could have affected the results of the OGTT. However, we focused on the selected parameters in the present study.
Derivation and evaluation of clinical indices from our method
The steady-state serum insulin concentration during the HGC (SSIHGC) was used as an estimate of the second-phase insulin secretion in response to elevated glucose. The steady-state glucose infusion rate during the HIC (GIR) reflects insulin sensitivity mainly in peripheral tissues because hepatic glucose production is almost completely suppressed at the high insulin concentration used during the test [11]. In general, the actual steady-state glucose concentrations (SSG) and steady-state insulin concentrations (SSI) are different in each patient, although the target concentrations are set in the glucose clamp tests. The SSGHGC, SSGHIC, and SSIHIC in this study were 201.7 ± 14.0 mg dl−1, 92.5 ± 17.4 mg dl−1, and 112.4 ± 36.1 μU ml−1, respectively. Because the variation in SSIHIC was not small and directly affected the estimate of insulin sensitivity, the GIR revised by the SSI was used as the estimate of the sensitivity.
The parameter p I4 of the mathematical model was used as an estimate of second-phase insulin secretion in response to elevated glucose. During a state of the HGC, the dI/dt, dG/dt, dR I/dt, dR I1/dt, and dR I2/dt become zero. By applying these conditions to our model for the insulin sensitivity index, p I4 is described by the following equation
 |
During the HGC, the G − G (0) was assumed to be constant and the p I4 was proportional to the R I. By doing this, we could understand that the p I4 had an analogous meaning to the SSIHGC. In this study, the p G2 was fixed, and p G3/p G2 was proportional to the p G3. Therefore, the parameter p G3 was used as an estimate of the insulin sensitivity of peripheral tissues.
Linear correlation analyses were performed to quantify the strengths of associations between two numeric variables. Data are expressed as mean ± standard deviations (SD).
Results and discussion
Our OGTT-derived index for the second-phase of insulin secretion was significantly correlated with the steady-state insulin concentration during the HGC (r = 0.90, p < 0.001, Fig. 3a). Our insulin sensitivity index was significantly correlated with the steady-state glucose infusion rate revised by the insulin concentration (GIR/SSIHIC) during the HIC (r = 0.56, p < 0.001, Fig. 3b).
Fig. 3.
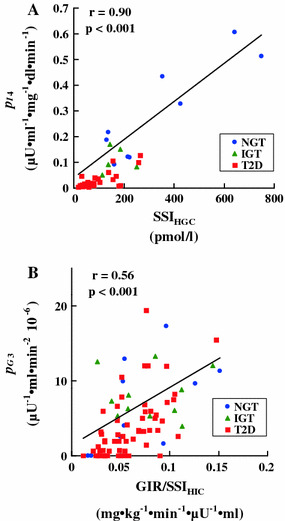
Relationship between our indices derived from the OGTT and analogous indices obtained using a glucose clamp. a Insulin secretion during second-phase insulin secretion. b Insulin sensitivity
The average glucose and insulin concentrations during the OGTTs that served as inputs to the mathematical models are shown in Fig. 4. The ability of the mathematical models to reproduce the input data was shown using weighted residuals and the results are shown in Fig. 5. To obtain the weighted residuals, the residuals between the results of the model and the input data were divided by the input values.
Fig. 4.
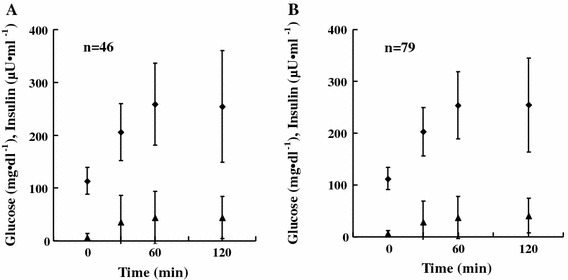
Plasma glucose and insulin during OGTTs. a Subjects used in the evaluation of insulin secretion. b Subjects used in the evaluation of insulin sensitivity
Fig. 5.
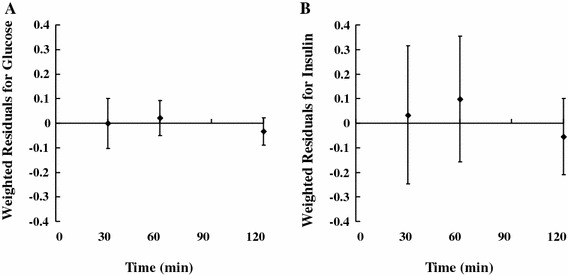
Weighted residuals for the subjects used in the evaluation of insulin sensitivity (n = 79). a Glucose. b Insulin
These results suggest that our method can potentially provide an accurate and convenient tool to improve the management of diabetes in clinical practice by assessing insulin secretion and insulin sensitivity. Our indices based on 2-h OGTTs showed good correlation with the analogous indices obtained from glucose clamp methods. Assessing these factors using a 2-h OGTT is advantageous because the 2-h OGTT is widely used for the diagnosis of diabetes under the WHO criteria, which makes this method easier to implement in a clinical setting. We compared the estimated accuracy of our method with that of other previously reported methods [25, 26] that can be used to assess these factors using data obtained from a 2-h OGTT. On the basis of the present data, our method has a higher correlation coefficient with the glucose clamp than the other approaches (Table 2). Characteristics of these indices in the subjects are summarized in Table 3.
Table 2.
Correlation coefficients of the OGTT- and clamp-derived insulin secretion and insulin sensitivity indices [25, 26]
| All | T2D | |
|---|---|---|
| SSIHGC | ||
| p 14 | 0.90 | 0.74 |
| p 14 * | 0.83 | 0.65 |
| HOMA-β | 0.67 | 0.56 |
| II index | 0.77 | 0.53 |
| Insulin0-120 (AUC) | 0.80 | 0.64 |
| GIR/SSIHIC | ||
| p G3 | 0.56 | 0.60 |
| p G3 * | 0.51 | 0.52 |
| HOMA-R | 0.42 | 0.29 |
| QUICKI | 0.44 | 0.36 |
| Matsuda index | 0.32 | 0.30 |
| OGIS120 | 0.41 | 0.22 |
The p I4 * and p G3 * were obtained without pre-processing the OGTT data. To derive an index of the OGIS120, glucose and insulin concentrations at 90 min during the OGTT are necessary in addition to the present input (4 blood samples during the 2-h OGTT) [26]. Here, interpolated G (90) and I (90) were used for the derivation of the indices
Table 3.
Characteristics of the OGTT-derived insulin secretion and insulin sensitivity indices of the subjects [25, 26]
| Subjects used in the evaluation of insulin secretion | Subjects used in the evaluation of insulin sensitivity | |||||||
|---|---|---|---|---|---|---|---|---|
| All | NGT | IGT | T2D | All | NGT | IGT | T2D | |
| n | 46 | 9 | 5 | 32 | 79 | 10 | 11 | 58 |
| HOMA-β (mg dl−1 μU−1 ml) | 89 ± 155 | 261 ± 292 | 78 ± 22 | 42 ± 47 | 72 ± 123 | 240 ± 283 | 65 ± 42 | 44 ± 46 |
| HOMA-R (mg dl−1 μU ml−1) | 1.82 ± 1.58 | 2.41 ± 2.90 | 1.43 ± 0.79 | 1.72 ± 1.12 | 1.69 ± 1.41 | 2.26 ± 2.77 | 1.47 ± 1.14 | 1.63 ± 1.11 |
| II index (mg−1 dl μU ml−1) | 0.44 ± 0.83 | 1.60 ± 1.36 | 0.32 ± 0.28 | 0.14 ± 0.18 | 0.33 ± 0.66 | 1.51 ± 1.32 | 0.26 ± 0.22 | 0.14 ± 0.16 |
| Insulin0-120 (AUC) (μU ml−1) | 37.0 ± 40.2 | 85.9 ± 63.7 | 41.1 ± 18.2 | 22.6 ± 18.6 | 32.2 ± 32.3 | 82.0 ± 61.3 | 34.3 ± 17.4 | 23.2 ± 16.3 |
| QUICKI (arbitrary unit) | 0.367 ± 0.040 | 0.367 ± 0.057 | 0.372 ± 0.036 | 0.366 ± 0.037 | 0.371 ± 0.040 | 0.370 ± 0.054 | 0.379 ± 0.044 | 0.369 ± 0.037 |
| Matsuda index (mg−1 dl μU ml−1) | 6.91 ± 4.58 | 5.88 ± 4.22 | 5.80 ± 1.65 | 7.38 ± 4.97 | 7.09 ± 4.16 | 5.92 ± 3.98 | 7.16 ± 3.69 | 7.28 ± 4.31 |
| OGIS120 (ml min−1 m−2) | 369 ± 59 | 422 ± 63 | 418 ± 45 | 346 ± 45 | 372 ± 55 | 424 ± 60 | 415 ± 40 | 355 ± 47 |
| p I4 (μU ml−1 mg−1 dl min−1) | 0.089 ± 0.134 | 0.291 ± 0.189 | 0.109 ± 0.049 | 0.029 ± 0.031 | 0.070 ± 0.106 | 0.275 ± 0.185 | 0.083 ± 0.047 | 0.032 ± 0.029 |
| p G3 (μU−1 ml min−2 10−6) | 4.95 ± 5.06 | 6.58 ± 6.32 | 6.70 ± 2.01 | 4.22 ± 4.95 | 5.13 ± 5.09 | 7.65 ± 5.44 | 3.84 ± 3.13 | 4.29 ± 5.01 |
In a previous study [26], the reproducibility of clinical indices was assessed with duplicate OGTT data from the same subjects. The resulting correlation was reported to be r < 0.90. This means that the upper bound of correlation coefficients between surrogate indices and the glucose clamp should be below 0.90. In this context, the present coefficient of 0.90 between the SSIHGC and p I4 might be too high. Both in all subjects and subjects with T2D (Table 2), our method’s data showed coefficients superior to those from the other methods, which is an interesting fact regardless of any discussion about absolute coefficient values.
The use of mathematical modeling may be one reason why our method showed better estimation accuracy than the other methods. Multiple factors contribute simultaneously to the regulation of glucose metabolism; therefore, time-dependent dynamics are important to fully understand the metabolism process. Mathematical modeling using differential equations is suitable for this type of system because it can describe the dynamics of a system consisting of multiple factors.
The pre-processing of the OGTT data may be another reason for the better estimation accuracy of our method. In general, the estimation accuracy of a model is enhanced by using a large amount of input data. However, we limited the directly available data to four samples from the 2-h OGTT to enhance the applicability of our method. Then, we assumed that the information lost by limiting the samples used could be partially recovered by considering the following characteristics of glucose and insulin dynamics: glucose and insulin concentrations change continuously after the start of the test, the derivative of the change in these concentrations becomes smaller over time, and values at 300 min return to the basal level in most cases [9, 17]. Next, the data were converted to continuous 5-h OGTT data using extrapolation and interpolation, as described in the parameter estimation section (Fig. 6). Although clear statistical significance cannot be obtained with the present number of cases, the validity of our assumption was supported by the estimation accuracy being improved by this pre-processing to some extent (Table 1).
Fig. 6.
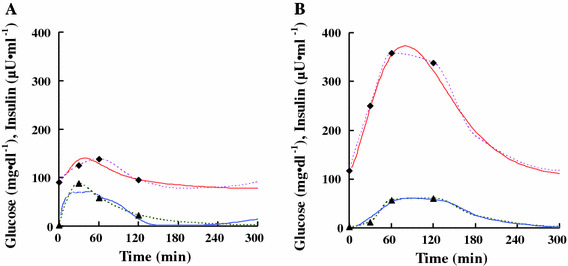
Examples of pre-processed and parameter-derived OGTTs. Squares and triangles represent glucose and insulin concentrations, respectively. Dotted lines represent extrapolated and interpolated data. Solid lines represent glucose and insulin concentrations calculated by the estimated parameters. a NGT, b T2D
Correlation coefficients between the GIR/SSIHIC and the HOMA-R, QUICKI, and Matsuda indices may seem to be smaller than those indicated in previous reports [27], but these coefficients in this study are not exceptionally small. For instance, correlation coefficients between the glucose clamp and the HOMA-R have been heterogeneous, ranging from strong [27] to weak [26]. There is a report which showed similar coefficients to those in this study [26]. These HOMA-R, QUICKI, and Matsuda indices are based on the concept that the higher the glucose and insulin concentrations are, the lower the insulin sensitivity will be. However, this concept may not be valid for some classes of diabetics who have high glucose concentrations and low insulin concentrations. In those patients, it is not obvious that higher insulin concentrations indicate lower insulin sensitivity. Because the average insulin secretion concentrations of the subjects were relatively low (Table 1), this might be a potential reason for the small correlation coefficients in this study’s indices.
It should be noted that absolute values of the correlation coefficients between the OGTT-derived and clamp-derived indices can often fluctuate and depend on cohorts because clinical characteristics of the cohorts used for evaluation can vary greatly. Therefore, there may be differences between the cohorts but each coefficient can contain essentially the similar clinical significance.
We assumed that the rate of hepatic insulin extraction was constant and that renal function was normal in building the model. The model requires insulin secretion to assess insulin sensitivity using insulin-dependent changes in glucose concentrations. Therefore, our method may have limitations for those subjects with hepatic dysfunction, renal impairment, or severe β-cell dysfunction.
The assessment of insulin secretion and insulin sensitivity is of great importance in selecting an optimal diabetic treatment strategy. The onset and progression of T2D is strongly correlated with dysfunction of these factors [1]. Most of the agents currently used to treat hyperglycemia can be broadly classified according to their improvement of one of these factors [2]. For this reason, it is important to identify the factor that is the underlying cause of the hyperglycemia so that a targeted therapy can be used. Therefore, the assessment of these factors becomes important. In support of this idea, a previous study compared the relationship between pathologic characterization based on the SSIHGC and GIR and successful therapy that achieved a well-controlled blood glucose level [28]. In that study, the average SSIHGC and GIR of patients successfully treated with sulfonylurea (glibenclamide) or an insulin sensitizer (pioglitazone) were compared. The SSIHGC and GIR in the group successfully treated with sulfonylurea were lower than those in the group treated with the insulin sensitizer, suggesting that, for a given therapy to be successful, the medication should target the underlying cause of the diabetes. This result demonstrates the importance of the quantitative assessment of β-cell function and insulin sensitivity for the selection of a suitable treatment for each patient.
In this study, we have shown that our method is accurate and potentially applicable in clinical practice for assessing the diabetic status of an individual patient. One of our goals is to apply this method to the daily clinical practice of general practitioners as a tool to determine the optimal treatment regimen, as do experienced diabetologists. Although our method showed better correlation coefficients of the reference values than those obtained by the other methods, the clinical significance of this improvement is now in question. To validate its clinical significance, we next plan to evaluate our method with additional clinical data that measures the efficacy of various medications used to treat hyperglycemia.
Acknowledgments
We would like to thank K. Kishi and K. Asano (Sysmex Corporation, Japan) for their helpful advice and encouragement.
Open Access
This article is distributed under the terms of the Creative Commons Attribution Noncommercial License which permits any noncommercial use, distribution, and reproduction in any medium, provided the original author(s) and source are credited.
Footnotes
M. Seike and T. Saitou contributed equally to this study.
References
- 1.Kahn SE. The relative contributions of insulin resistance and beta-cell dysfunction to the pathophysiology of type 2 diabetes. Diabetologia. 2003;46:3–19. doi: 10.1007/s00125-003-1190-9. [DOI] [PubMed] [Google Scholar]
- 2.Fowler MJ. Diabetes treatment, part 2: oral agents for glycemic management. Clin Diabetes. 2007;25:131–134. doi: 10.2337/diaclin.25.4.131. [DOI] [Google Scholar]
- 3.Mari A. Mathematical modeling in glucose metabolism and insulin secretion. Assessment of nutritional status and analytical methods. Curr Opin Clin Nutr Metab Care. 2002;5(5):495–501. doi: 10.1097/00075197-200209000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Bergman R, Ider Y, Bowden C, Cobelli C. Quantitative estimation of insulin sensitivity. Am J Physiol. 1979;236(6):E667–E676. doi: 10.1152/ajpendo.1979.236.6.E667. [DOI] [PubMed] [Google Scholar]
- 5.Toffolo G, Breda E, Cavaghan M, Ehrmann D, Polonsky K, Cobelli C. Quantitative indexes of beta-cell function during graded up&down glucose infusion from C-peptide minimal models. Am J Physiol Endocrinol Metab. 2001;280:E2–E10. doi: 10.1152/ajpendo.2001.280.1.E2. [DOI] [PubMed] [Google Scholar]
- 6.Steil G, Hwu C, Janowski R, Hariri F, Jinagouda S, Darwin C, Tadros S, Rebrin K, Saad M. Evaluation of insulin sensitivity and β-cell function indexes obtained from minimal model analysis of a meal tolerance test. Diabetes. 2004;53:1201–1207. doi: 10.2337/diabetes.53.5.1201. [DOI] [PubMed] [Google Scholar]
- 7.Dalla Man C, Caumo A, Cobelli C. The oral glucose minimal model: estimation of insulin sensitivity from a meal test. IEEE Trans Biomed Eng. 2002;49(5):419–429. doi: 10.1109/10.995680. [DOI] [PubMed] [Google Scholar]
- 8.Dalla Man C, Caumo A, Basu R, Rizza R, Toffolo G, Cobelli C. Minimal model estimation of glucose absorption and insulin sensitivity from oral test: validation with a tracer method. Am J Physiol Endocrinol Metab. 2004;287:E637–E643. doi: 10.1152/ajpendo.00319.2003. [DOI] [PubMed] [Google Scholar]
- 9.Dalla Man C, Campioni M, Polonsky KS, Basu R, Rizza RA. Two-hour seven-sample oral glucose tolerance test and meal protocol: minimal model assessment of β-cell responsivity and insulin sensitivity in nondiabetic individuals. Diabetes. 2005;54:3265–3273. doi: 10.2337/diabetes.54.11.3265. [DOI] [PubMed] [Google Scholar]
- 10.Alberti KGMM, Zimmet PZ. Definition, diagnosis and classification of diabetes mellitus and its complications. Part. 1: diagnosis and classification of diabetes mellitus. Provisional report of a WHO Consultation. Diabetes Med. 1998;15:539–553. doi: 10.1002/(SICI)1096-9136(199807)15:7<539::AID-DIA668>3.0.CO;2-S. [DOI] [PubMed] [Google Scholar]
- 11.DeFronzo R, Tobin J, Andres R. Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol. 1979;237(3):E214–E233. doi: 10.1152/ajpendo.1979.237.3.E214. [DOI] [PubMed] [Google Scholar]
- 12.Campbell PJ, Mandarino LJ, Gerich JE. Quantification of the relative impairment in actions of insulin on hepatic glucose production and peripheral glucose uptake in non-insulin-dependent diabetes mellitus. Metabolism. 1988;37(1):15–21. doi: 10.1016/0026-0495(88)90023-6. [DOI] [PubMed] [Google Scholar]
- 13.Tamura Y, Niwa M, Uchino H, Uchida T, Kawamori R. Postprandial hyperglycemia and impaired hepatic glucose uptake in type 2 diabetes. Int Diabetes Monit. 2002;14(2):1–6. [Google Scholar]
- 14.Ludvik B, Nolan J, Roberts A, Baloga J, Joyce M, Bell J, Olefsky J. Evidence for decreased splanchnic glucose uptake after oral glucose administration in non-insulin-dependent diabetes mellitus. J Clin Invest. 1997;100:2354–2361. doi: 10.1172/JCI119775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ishida T, Hosokawa H, Kawanishi K, Irino S (1987) The differential role of liver and peripheral tissue on glucose metabolism. In: Shigeta Y, Lebovitz H, Gerich J, Malaisse W (eds) Proceedings of the 4th Japan–Korea symposium on diabetes mellitus: best approach to the ideal therapy of diabetes mellitus. Elsevier, Amsterdam, pp 297–300
- 16.Mitrakou A, Kelley D, Veneman T, Jenssen T, Pangburn T, Reilly J, Gerich J. Contribution of abnormal muscle and liver glucose metabolism to postprandial hyperglycemia in NIDDM. Diabetes. 1990;39:1381–1390. doi: 10.2337/diabetes.39.11.1381. [DOI] [PubMed] [Google Scholar]
- 17.Dressman JB, Reppas C, editors. Oral drug absorption: prediction and assessment. 2. London: Informa Healthcare; 2010. [Google Scholar]
- 18.Bock G, Dalla Man C, Campioni M, Chittilapilly E, Basu R, Toffolo G, Cobelli C, Rizza R. Pathogenesis of pre-diabetes: mechanisms of fasting and postprandial hyperglycemia in people with impaired fasting glucose and/or impaired glucose tolerance. Diabetes. 2006;55:3536–3549. doi: 10.2337/db06-0319. [DOI] [PubMed] [Google Scholar]
- 19.Vapnik V, Golowich S, Smola AJ (1997) A support vector method for function approximation, regression estimation, and signal processing. In: Mozer MC, Jordan MI, Petsche T (eds) Advances in neural information processing systems: proceedings of the 1996 conference on neural information processing systems, vol 9. MIT Press, Cambridge, pp 281–287
- 20.Lu J, Seike M, Liu W, Wu P, Wang L, Wu Y, Naito Y, Nakajima H, Kouchi Y. Extrapolation of clinical data from an oral glucose tolerance test using a support vector machine. World Acad Sci Eng Technol. 2009;53:1271–1274. [Google Scholar]
- 21.Fritsch FN, Carlson RE. Monotone piecewise cubic interpolation. SIAM J Numer Anal. 1980;17:238–246. doi: 10.1137/0717021. [DOI] [Google Scholar]
- 22.Kahaner D, Moler C, Nash S. Numerical methods and software. Englewood Cliffs: Prentice-Hall; 1989. [Google Scholar]
- 23.Carson ER, Cobelli C, Finkelstein L. The mathematical modeling of metabolic and endocrine systems. New York: Wiley; 1983. [Google Scholar]
- 24.Toffolo G, Campioni M, Basu R, Rizza RA, Cobelli C. A minimal model of insulin secretion and kinetics to assess hepatic insulin extraction. Am J Physiol Endocrinol Metab. 2006;290:E169–E176. doi: 10.1152/ajpendo.00473.2004. [DOI] [PubMed] [Google Scholar]
- 25.Pacini G, Mari A. Methods for clinical assessment of insulin sensitivity and β-cell function. Best Pract Res Clin Endocrinol Metab. 2003;17(3):305–322. doi: 10.1016/S1521-690X(03)00042-3. [DOI] [PubMed] [Google Scholar]
- 26.Mari A, Ludvik B, Pacini G, Nolan JJ, Murphy E. A model-based method for assessing insulin sensitivity from the oral glucose tolerance test. Diabetes Care. 2001;24:539–548. doi: 10.2337/diacare.24.3.539. [DOI] [PubMed] [Google Scholar]
- 27.Bonora E, Targher G, Alberiche M, Bonadonna RC, Saggiani F, Zenere MB, Monauni T, Muggeo M. Homeostasis model assessment closely mirrors the glucose clamp technique in the assessment of insulin sensitivity: studies in subjects with various degrees of glucose tolerance and insulin sensitivity. Diabetes Care. 2000;23:57–63. doi: 10.2337/diacare.23.1.57. [DOI] [PubMed] [Google Scholar]
- 28.Gorogawa S, Kaneto H, Matsuhisa M, Ohtoshi K, Kawamori D, Hazama Y, Yoshiuchi K, Yamasaki Y. Possible novel index determined by the glucose clamp test for selection of a suitable therapy for each type 2 diabetic patient. Diabetes Res Clin Pract. 2005;69(1):1–4. doi: 10.1016/j.diabres.2004.10.006. [DOI] [PubMed] [Google Scholar]


