Abstract
Background
The associations between adiposity and metabolic risk factors have been suggested to vary across ethnicities. Studies in Caucasians have shown that after adjusting for waist circumference and body mass index (BMI), a larger hip circumference may be protective for metabolic risk factors. To our knowledge, these associations have never been examined in a Chinese population.
Methods
Baseline (1987–1988) and follow-up (1993–1994) data were from the People's Republic of China Study (n = 1,144 men, n = 1,776 women). Logistic models were stratified by sex and adjusted for age, smoking, center, and education. Incidence differences (ID) comparing the sex specific 85th percentile to the 15th percentile of hip circumference were computed for elevated blood pressure, blood glucose and triglycerides, low high-density lipoprotein cholesterol (HDL-C), and multiple metabolic abnormalities (three or more of the aforementioned).
Results
In models adjusted for waist circumference and BMI, the ID [95% confidence interval (CI)] per 1,000 persons associated with a 12-cm larger hip were −132 (−237, −26) for low HDL-C; −85 (−138, −31) for elevated triglycerides; and −49 (−83, −4) for multiple metabolic abnormalities. In males, a larger hip circumference was not associated with a reduction of incident risk factors, although the ID tended to be negative.
Conclusions
In Chinese women, greater mass in the lower trunk region was inversely associated with incident high triglycerides, low HDL-C, and multiple metabolic abnormalities when adjusted for general and central adiposity. This association was not detected in men. Additional research is needed to better understand the mechanisms by which fat at different depots results in differential risk.
Introduction
Specific fat depots may be more closely related to metabolic risk than overall adiposity.1 Many studies have used the ratio of waist and hip circumferences as a means of capturing aspects of body shape that are poorly detected by body mass index (BMI). Nevertheless, the waist-to-hip ratio does not differentiate the independent effects of hip and waist circumferences, and the ratio measure does not account for possible nonlinear associations between the two anthropometrics.2,3
Although waist and hip circumferences are crude measures of adipose tissue distribution, the circumference measures show a high association with the size of the respective fat depots,4–6 and they are clinically practical due to the low risk of assessment to patients, low cost, and ease of collection. Waist circumference is an indicator of the amount of visceral and subcutaneous adiposity around the abdomen, while hip circumference assesses skeletal frame size and adipose and muscle mass in the buttock and thigh regions (gluteofemoral).7,8 In mutually adjusted models, waist circumference has been shown to correlate with abdominal visceral and subcutaneous adiposity and hip circumference was inversely correlated with those depots but positively correlated with leg fat mass.8 Visceral and subcutaneous adipocytes have different lipolytic activities because visceral fat is associated with adverse cardiovascular risk factors and is more metabolically active compared with adipocytes in subcutaneous fat.6
In contrast to a large waist circumference at a given overall body size, a large hip circumference has been suggested to be less associated with risk of disease and even potentially protective. After adjustment for one another and for BMI, waist and hip circumferences have been shown to have independent and opposite associations with cardiovascular risk factors, coronary heart disease (CHD), cardiovascular disease (CVD), and mortality.6,9–23 Studies examining components of hip and waist circumferences, specifically, leg and trunk fat, and leg lean mass, using dual-energy X-ray absorptiometry (DXA) or computed tomography (CT) have found positive associations of trunk fat and inverse associations of thigh or leg fat with insulin resistance, dyslipidemia, diabetes, and other metabolic risk factors. These associations have been observed in black, white, and Japanese populations.8,22,24–27
To our knowledge, no studies have evaluated the association of hip circumference, independent of waist circumference or BMI, with cardiovascular risk factors in a Chinese population. It is well established that adiposity is associated with metabolic risk. Because Chinese have greater adiposity at the same level of BMI compared to non-Asian populations and experience metabolic abnormalities at low levels of adiposity,28–30 it is uncertain whether an inverse association of hip circumference with metabolic risk factors would be observed in a Chinese population. Our goal was to explore whether a larger hip circumference, when controlling for waist circumference or BMI, would be associated with a lower incidence of metabolic risk factors in a Chinese cohort from Guangzhou, China.
Materials and Methods
Study population
Data were from the community-based People's Republic of China (PRC) Study.31 Waist and hip circumferences were collected from subjects living in urban and rural areas of Guangzhou, China (southern). Baseline and follow-up examinations were in 1987–1988 and 1993–1994, respectively. Participants were aged 28–69 years at baseline.
Of the n = 3,019 eligible subjects, participants were excluded if missing anthropometric data at baseline (n = 52) or follow up (n = 15), missing education at baseline (n = 1), self-report of cancer (n = 13), or CHD (n = 18). Following these exclusions, 1,144 men and 1,776 women were included in the analyses. For each of the incident outcomes examined, prevalent cases of the condition were excluded. This study was approved by the Institutional Review Board (IRB) at each field center, and the analysis was approved by the University of North Carolina at Chapel Hill (UNC-CH) IRB on research involving human subjects.
Measurements
Protocols and training manuals for measurements and the review, processing, and analyses of data were administered by the Collaborative Studies Coordinating Center at UNC-CH. Data were collected in examination centers by trained personnel. Participants wore light clothing without shoes during collection of anthropometric data. Height was measured to the nearest centimeter (cm) and weight to the nearest kilogram (kg). BMI was calculated [weight (kg)/height (m)2]. Circumferences of the waist and hip were measured to the nearest 0.1 cm. Waist circumference was measured by passing the tape measure through the midpoint between the superior iliac crest and the lowest rib. Hip circumference was measured at the maximum protrusion.
Subjects were instructed to fast 12 h prior to the examination. Glucose assays were performed on an Abbott autoanalyzer. Serum glucose was measured by the hexokinase/glucose-6-phosphate dehydrogenase method. High-density lipoprotein cholesterol (HDL-C) and triglycerides (TG) were measured according to protocols by the Lipid Standardization Program of the U.S. National Heart, Lung and Blood Institute (NHLBI) and Centers for Disease Control (CDC). Serum TG was determined with use of an enzymic reagent from Abbott Laboratories. Serum HDL-C was measured using the Boehringer Mannheim Diagnostics high-performance enzymic reagent calibrated with precise standards on the Abbott analyzer after precipitation of other lipid fractions with dextran sulfate. To ensure quality control, random samples were analyzed by the CDC.
Blood pressure was measured three times at each visit using a random zero mercury sphygmomanometer on the right arm with the participant seated. The average of the last two measurements was used in the analyses. Participants self-reported use of antihypertension medications in the previous 2 weeks.
Definition of outcomes
Outcomes were dichotomized based on criteria from the Adult Treatment Panel III (ATP III) of the National Cholesterol Education Program (NCEP) for metabolic syndrome.32 Components of the metabolic syndrome were defined as: (1) HDL-C <1.03 mmol/L in males or <1.29 mmol/L in females, (2) triglycerides ≥1.7 mmol/L, (3) fasting blood glucose ≥5.6 mmol/L or self-reported diabetes, and (4) blood pressure ≥130/85 mmHg or self-report of current antihypertensive medication use. The fifth criterion of the metabolic syndrome is a large waist circumference. Because waist circumference was included as a covariate in our models, we did not model it as an outcome. Instead we assessed a clustering of risk factors similar to the ATP III metabolic syndrome definition but exclusive of waist circumference, which we termed “multiple metabolic abnormalities” and defined as the presence of at least three of the four aforementioned ATP III outcomes examined.
Statistical analyses
Models were stratified by gender because of the well-known differences in body shape between men and women.33 Dichotomous outcomes were coded as 0 (no disease) or 1 (incident disease). All models include the covariates field center (urban or rural), age (years), and highest education level attained (less than senior middle school, senior middle school, more than senior middle school). For all outcomes, the covariates for smoking, alcohol, menopausal status, and physical activity were examined but were not included because associations were small, not statistically significant (p < 0.05), and did not influence the coefficients associated with variables of interest.
Quadratic terms were tested to assess nonlinear associations of BMI, waist circumference, hip circumference, and age with metabolic risk factors. Most quadratic terms were not significant at p < 0.05, except for age,2 which improved model fit significantly in women. Interactions between hip circumference and age as well as hip circumference and BMI were assessed for each outcome using the Wald test with one degree of freedom, and none were significant at p < 0.05. The adjusted incidence at the sex-specific 15th percentile of hip circumference and the incidence differences (ID) comparing the sex-specific 85th percentile to the 15th percentile of hip circumference were computed. ID estimates were obtained from logistic regression models, and 95% confidence intervals (CI) were calculated using the delta method by the prvalue command in Stata 10.0.34,35 The incidence and ID were also modeled with adjustment for additional anthropometric measures (waist circumference and BMI). The ID was standardized to the mean covariate values for continuous variables and to the most prevalent education level (<senior middle school) and center (rural).
Results
The distribution of most demographic characteristics was similar between the sexes, except for alcohol and smoking status (Table 1). A small percentage of women consumed alcohol (15.1%) or smoked (3.0%), whereas men were much more likely to drink (59.4%) or smoke (66.1%). The majority of subjects were normal weight or underweight and did not have abdominal obesity according to standard World Health Organization (WHO) BMI definitions and Asian central obesity cut points of ≥90 cm in males and ≥80 cm in females (Table 1). In this sample, the Pearson correlation coefficients for waist circumference, hip circumference, and BMI were high and ranged from 0.76 to 0.83 in men and 0.79 to 0.87 in women. Despite the high correlations, collinearity of anthropometric measures, evaluated using a variance inflation factor (VIF) were all less than 5.0, well below the criterion for indication of 10.0.
Table 1.
Baseline Characteristics Among Chinese Women and Men, the People's Republic of China Study (1987–1988)
| Variables | Women (n = 1,776) | Men (n = 1,144) |
|---|---|---|
| Age (years), mean (SD) | 44.8 (8.0) | 45.1 (8.3) |
| Body mass index (kg/m2), mean (SD) | 21.0 (2.8) | 20.6 (2.5) |
| Body mass index category (%) | ||
| <18.5 kg/m2 | 18.2 | 18.9 |
| 18.5 to <23.0 kg/m2 | 62.6 | 65.4 |
| 23.0 to <25.0 kg/m2 | 10.8 | 10.1 |
| 25.0 to <27.5 kg/m2 | 5.9 | 4.3 |
| 27.5 to <30.0 kg/m2 | 1.7 | 1.1 |
| 30.0 to <32.5 kg/m2 | 0.5 | 0.4 |
| ≥32.5 kg/m2 | 0 | 0 |
| Waist circumference (cm), mean (SD) | 70.5 (7.8) | 73.2 (7.6) |
| Central obesitya (%) | 13.4 | 3.4 |
| Hip circumference (cm), mean (SD) | 88.1 (6.3) | 87.4 (5.4) |
| Hip circumference, 15th percentile (cm) | 82.0 | 82.0 |
| Hip circumference, 85th percentile (cm) | 94.0 | 93.0 |
| Current cigarette or leaf smokers (%) | 3.0 | 66.1 |
| Current drinkers (%) | 15.1 | 59.4 |
| Exercise | ||
| No | 83.8 | 79.6 |
| Occasionally | 4.5 | 5.4 |
| Regularly | 8.6 | 13.5 |
| Educational attainment (%) | ||
| <Senior middle school | 82.2 | 79.0 |
| Senior middle school | 14.6 | 17.6 |
| >Senior middle school | 3.2 | 3.4 |
| Center (rural) (%) | 56.6 | 59.7 |
| Systolic blood pressure (mmHg), mean (SD) | 112.1 (15.8) | 113.3 (14.8) |
| Diastolic blood pressure (mmHg), mean (SD) | 72.0 (9.5) | 73.6 (9.9) |
| Glucose (mmol/L), mean (SD) | 4.4 (1.1) | 4.1 (0.9) |
| HDL-C (mmol/L), mean (SD) | 1.4 (0.3) | 1.4 (0.4) |
| Triglycerides (mmol/L), mean (SD) | 1.3 (1.0) | 1.3 (1.1) |
According to the World Health Organization (WHO) guidelines for Asians, central obesity is defined as a waist circumference ≥ 90 cm in males and ≥ 80 cm in females.
SD, standard deviation; HDL-C, high-density lipoprotein cholesterol.
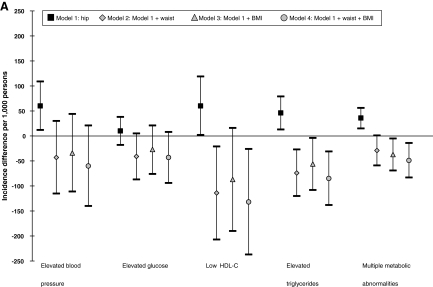
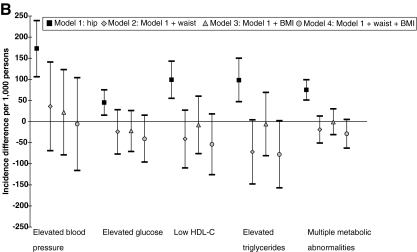
The unadjusted baseline prevalence and 6-year incidence for each outcome as well as markers of adiposity are shown in Table 2. In both women and men, multiple metabolic abnormalities and elevated blood glucose were the least prevalent outcomes (<10%); however, the crude prevalence and incidence levels were higher, between 10% and 34%, for elevated blood pressure, low HDL-C, and elevated triglycerides. The adjusted incidences of metabolic risk factors at the 15th percentile of hip circumference are shown in Table 3 and the incidence difference (between the 85th and 15th percentile of hip circumference (a difference of 11 cm in males and 12 cm in females) per 1,000 persons are shown in Fig. 1, A and B. Hip circumference was positively associated with incident outcomes when it was the only anthropometric measure included in the model (model 1). When adjusted for waist circumference (model 2) or BMI (model 3), the ID tended to be null or negative, suggesting hip circumference may be neutral or inversely associated with incident metabolic risk factors when accounting for general or central adiposity. In women (Fig. 1A), with adjustment for waist circumference, a larger hip circumference was associated with a significant decrease in incidence (95% CI) per 1,000 persons for high triglycerides −74 (−120, −27) and low HDL-C −114 (−207, −21); and when adjusting for BMI, hip circumference was associated with a significant decrease in incidence per 1,000 persons for high triglycerides −56 (−108, −4) and multiple metabolic abnormalities −37 (−69, −5). In males (Fig. 1B), ID estimates for models 2 and 3 tended to be null or negative.
Table 2.
Crude Baseline Prevalence and 6-Year Incidence of Adiposity and Metabolic Abnormalities Among Chinese Women and Men
| |
Women |
Men |
||
|---|---|---|---|---|
| Prevalence % | Incidence % | Prevalence % | Incidence % | |
| Elevated BMI (≥25 kg/m2) | 9.7 | 6.7 | 5.7 | 7.0 |
| Central obesitya (waist circumference ≥80 cm in women and ≥90 cm in men) | 13.4 | 11.2 | 3.4 | 4.1 |
| Elevated blood pressure (≥130/85 mmHg or medication) | 15.2 | 23.6 | 17.2 | 30.2 |
| Elevated glucose (≥5.6 mmol/L) | 9.6 | 13.1 | 7.5 | 8.6 |
| Low HDL-C (<1.29 mmol/L in women; <1.03 mmol/L in men) | 34.3 | 32.8 | 15.0 | 13.3 |
| Elevated triglycerides (≥1.7 mmol/L) | 23.9 | 11.1 | 22.1 | 15.8 |
| Multiple metabolic abnormalities (≥3 of the above criteria) | 5.0 | 8.8 | 2.4 | 6.1 |
According to the World Health Organization (WHO) guidelines for Asians and the IOTF metabolic syndrome definition for Chinese.
BMI, body mass index; HDL-C, high-density lipoprotein cholesterol; IOTF, International Obesity Task Force.
Table 3.
Incidence of Metabolic Abnormalities per 1,000 Persons (95% CI) at the 15th Percentilea of Hip
| |
Model 1 |
Model 2 |
Model 3 |
Model 4 |
|---|---|---|---|---|
| Risk at the 15th percentile of hipa(95% CI) | Model 1b | (Model 1b + waist) | (Model 1b + BMI) | (Model 1b + waist + BMI) |
| Women | ||||
| Elevated blood pressure (≥130/85 mmHg or antihypertensive medication use) | 191 (161, 220) | 237 (194, 281) | 233 (188, 278) | 246 (198, 294) |
| Elevated glucose (≥5.6 mmol/L) | 96 (75, 117) | 122 (90, 155) | 115 (82, 147) | 123 (88, 158) |
| Low HDL-C (<1.29 mmol/L) | 295 (257, 334) | 380 (323, 437) | 366 (306, 427) | 389 (326, 453) |
| Elevated triglycerides (≥1.7 mmol/L) | 75 (56, 95) | 128 (92, 163) | 120 (84, 156) | 135 (95, 176) |
| Multiple metabolic abnormalities (≥3 of the above criteria) | 42 (29, 55) | 70 (46, 93) | 74 (49, 100) | 81 (53, 110) |
| Men | ||||
| Elevated blood pressure (≥130/85 mmHg or antihypertensive medication use) | 220 (183, 258) | 274 (219, 328) | 279 (225, 333) | 292 (233, 350) |
| Elevated glucose (≥5.6 mmol/L) | 56 (37, 75) | 86 (51, 121) | 84 (52, 117) | 95 (56, 134) |
| Low HDL-C (<1.03 mmol/L) | 87 (63, 110) | 138 (95, 180) | 124 (85, 162) | 144 (99, 190) |
| Elevated triglycerides (≥1.7 mmol/L) | 112 (84, 141) | 179 (129, 228) | 150 (107, 193) | 182 (130, 234) |
| Multiple metabolic abnormalities (≥3 of the above criteria) | 21 (11, 31) | 47 (24, 71) | 40 (20, 59) | 53 (26, 80) |
The 15th percentile of hip is 82 cm in men and in women.
Model 1 includes hip, age, smoking, center, and education. For women, this model also includes age.2
CI, confidence interval; BMI, body mass index; HDL-C, high-density lipoprotein cholesterol.
FIG. 1.
(A) Incidence difference [95% confidence interval (CI)] per 1,000 persons for metabolic abnormalities at the 15th versus 85th percentile of hip circumference in women. All models were adjusted for baseline age, age2, education level, smoking status, and field center. Multiple metabolic abnormalities were defined as the presence of three or more metabolic abnormalities [elevated blood pressure, elevated glucose, low high-density lipoprotein cholesterol (HDL-C) and elevated triglycerides]. The 15th and 85th percentiles of hip were 82 cm and 94 cm, respectively. (B) Incidence difference (95% CI) per 1,000 persons for metabolic abnormalities at the 15th versus 85th percentile of hip circumference in men. All models were adjusted for baseline age, education level, smoking status, and field center. Multiple metabolic abnormalities were defined as the presence of three or more metabolic abnormalities (elevated blood pressure, elevated glucose, low HDL-C, and elevated triglycerides). The 15th and 85th percentiles of hip were 82 cm and 93 cm, respectively.
Model 4 included hip and was adjusted for both waist circumference and BMI. In women, the ID (95% CI) per 1,000 persons was −85 (−138, −31) for incident high triglycerides, −132 (−237, −26) for low HDL-C and −49 (−83, −14) for multiple metabolic abnormalities. For blood pressure and glucose, estimates were negative but confidence intervals included zero. In men, point estimates for all the outcomes examined were negative and the confidence intervals included zero.
Additional sex-stratified regression models were run to examine the association of hip circumference with incident hypertension and diabetes. Results suggest a larger hip circumference was not associated with a greater incidence of diabetes or hypertension.
Discussion
In this prospective study, hip circumference was positively associated with incident metabolic risk factors in Chinese men and women. After adjustment for waist circumference and BMI, women with a larger hip circumference had a lower risk of incident elevated TGs, low HDL-C, and multiple metabolic abnormalities, and null associations were found for elevated blood pressure and elevated glucose. In men, after adjustment for waist circumference or waist circumference and BMI, the association of hip circumference with glucose, lipid levels, and multiple metabolic abnormalities was inverse, but not statistically significant. Weaker inverse associations in men are consistent with other studies, many of which found stronger evidence of an inverse association of hip circumference with adverse outcomes in women10,16,18,20,36 This differential may be due to gender differences in hip girth, body composition, and/or fat distribution. Although the gender differences in hip circumference are smaller in Chinese compared to Caucasians, gender differences in body shape and fat distribution persist.37 In this cohort, the difference in hip circumference between women and men was less than 1 cm, whereas most studies in Caucasian populations have shown gender differences in hip circumference between 1 and 6 cm.8,12,15 We explored whether gender differences were related to differences in height, but when height was added to the models, the estimates remained essentially unchanged.
The participants in our study were leaner than populations examined in previous studies of hip circumference, yet associations between hip circumference and metabolic risk factors were observed. Here the mean BMI among Chinese was 20.6 kg/m2 in men and 21.0 kg/m2 in women, and fewer than 6% of men and 10% of women had a BMI of 25 kg/m2 and above, whereas in most studies the mean BMI was ≥25 kg/m2.9,11–15,17,21,36,38 A recent study36 that reported an inverse association of hip circumference with incident diabetes and CHD included data from American whites and blacks in whom the mean value for hip circumference within the lowest quintile of hip circumference (92.7 cm) was larger than our overall population mean for hip circumference (87.8 cm). The sex-specific mean value of hip circumference in our population was also smaller than means reported in previously published studies.9,11–15,17,21,36,38
We know of six studies that have used a cross-sectional design to examine the association of hip circumference with metabolic syndrome or its component risk factors (blood pressure, lipids, and glucose).10,12,13,16,21,22,38 Two of these studies were conducted among Australians.13,21 Dixon et al.21 examined obese Australian women and used receiver operating characteristic (ROC) curves to identify the values of hip and waist circumferences associated with the highest sum of sensitivity and specificity for the presence of metabolic syndrome. They then tested the odds of metabolic syndrome above versus below that cutoff. The investigators found a small hip circumference (below the cutoff of 115 cm) was associated with greater odds of the metabolic syndrome [odds ratio (OR) (95% CI): 12.3 (3.0, 51.0)] compared to a large hip circumference (above the cutoff of 115 cm). The Australian Diabetes, Obesity and Lifestyle study,13 a nationally representative study among 11,247 participants aged 25 and older, found that the OR (95% CI) associated with a 1 standard deviation (SD) increase in hip circumference (7.6 cm in men and 11.1 cm in women) was 0.55 (0.41, 0.73) in men and 0.42 (0.27, 0.65) in women for diabetes; 0.58 (0.50, 0.67) in men and 0.37 (0.30, 0.45) in women for dyslipidemia; and 0.80 (0.69, 0.93) in men and 0.88 (0.70, 1.11) in women for hypertension.
The Quebec Family Study examined the association of hip circumference with metabolic risk factors by modeling hip circumference as a continuous variable.12 Models were adjusted for age, BMI, and waist circumference. In men, a 1-cm increase in hip circumference was associated with higher levels of HDL-C [mean ± SD 0.008 ± 0.004 mmol/L] and lower levels of triglycerides (−0.039 ± 0.011 mmol/L) and glucose (−0.039 ± 0.018 mmol/L). Associations were positive, but not significant, for blood pressure. In women, only the association of a 1-cm increase in hip circumference with triglycerides (−0.017 ± 0.006 mmol/L) was significant. Associations were inverse, but not significant, for blood pressure.
Two papers summarized results from a cross-sectional study of Caucasians in Tehran, Iran.10,16 Quintiles of hip circumference were used to predict the OR for ATP III metabolic syndrome components among 5,720 women10 and 4,040 men16 aged 18–74. In women, the adjusted OR comparing the largest versus smallest hip circumference quintile was inversely associated with all components of the metabolic syndrome, and in men this was true for all outcomes except elevated blood pressure.
A cross-sectional study that examined the association of hip circumference with metabolic risk factors in non-Caucasians included Melanesians, Micronesians, Indians, and Creoles from Mauritius, Rodrigues, Papua New Guinea, and Nauru.38 In all four ethnic groups, a 1 SD larger hip circumference (6.9–11.8 cm in men and 9.7–13.6 cm in women) was associated with lower glucose and TG levels in both sexes and higher HDL-C levels in women only, after adjustment for waist circumference, BMI, and age. Inverse associations with blood pressure were not significant.
To our knowledge the only other study of hip circumference that included a large East Asian sample used anthropometry and DXA to examine the cross-sectional association of hip circumference and depots of lean and fat mass with cardiovascular risk factors.22 Participants included Japanese men (n = 1,249) and women (n = 3,007) aged 20–79 years. A 1-cm increase in hip circumference was associated with a decrease in the odds—OR (95% CI) for males and for females) of hypertension [0.92 (0.87, 0.98) and 0.94 (0.91, 0.98)], low HDL-C [0.91 (0.84, 0.98) and 0.88 (0.81, 0.95)], hypertriglyceridemia [0.91 (0.87, 0.96) and 0.97 (0.93, 1.01)], dyslipidemia [0.92 (0.87, 0.96) and 0.96 (0.93, 0.98)], and diabetes [0.88 (0.79, 0.97) and 0.90 (0.84, 0.98)]—when controlling for BMI and waist circumference. Further examination of cardiovascular risk factors with measures of body composition suggested a positive association of trunk fat mass and a negative association of leg fat mass with hypertension, hypertriglyceridemia, dyslipidemia, and diabetes in men. In women, greater trunk fat mass and lower leg fat mass were significantly and positively associated with these outcomes as well as for hypercholesterolemia and low HDL-C.
The six cross-sectional studies presented above support the inverse association of a larger hip circumference with metabolic risk factors when controlling for waist circumference or BMI. The reduction in risk was generally moderate with ORs typically in the range of 0.9–0.4 for a 1 SD increase in hip circumference or for comparison of the highest to lowest quartile or quintile of hip circumference. Similar to our study of incidence, the majority of these studies of prevalence12,13,16,38 found weaker associations of hip circumference with blood pressure, compared to the association with other metabolic risk factors. Hypertension is a multigenic disease that varies in etiology39,40; therefore, it is possible that only a subset of individuals with hypertension have elevated blood pressure as a result of mechanisms related to fat distribution.
To our knowledge, our study is the first to examine the prospective association of hip circumference with all metabolic syndrome components. Longitudinal studies examining the associations with hip circumference have focused on CHD, CVD, diabetes, or mortality as outcome measures and none included an East Asian sample. We know of six studies that have examined longitudinal associations with hip circumference,11,14,15,17,23,36 all of which support an inverse association of a larger hip circumference with incident CHD, CVD, diabetes, and mortality when controlling for central or general adiposity.
Overall, results from both cross-sectional and longitudinal studies support an inverse association of a larger hip circumference with glucose, lipids, and health outcomes (CHD, CVD, mortality) and perhaps a weak association with blood pressure when accounting for general or central adiposity. Although the causal mechanisms between fat depots and risk factors are not certain, it has been suggested that inflammatory markers and insulin resistance may play an intermediary role in the link between adipose tissue and metabolic risk1,41,42 Adipose tissue in the gluteofemoral region may serve an important role in the removal of nonesterified fatty acids (NEFA) from the circulation.43,44 This activity could protect the liver, pancreas, and skeletal muscle from exposure and accumulation of NEFA and thereby limit the development of insulin resistance. Thigh subcutaneous fat has also been correlated with greater insulin sensitivity.45 More research is needed to better understand the underlying mechanisms in various populations.
This is the first longitudinal study to indicate an inverse association of a large hip circumference with incident metabolic outcomes in a Chinese population. This population was unusually lean by Western standards, indicating that high levels of adiposity are not required for an inverse association of hip circumference to be detected. It is well established that excess adiposity is associated with a greater risk for the metabolic syndrome. However, the distribution of the adiposity appears to be indicative of risk. The authors acknowledge the identification of a statistical association does not prove causation, and the underlying mechanisms for the inverse association cannot be discerned based on our study. Strengths of this work include the quality control of the data collection, longitudinal design, and use of measured anthropometry. This study is limited in that we did not have more discriminative measures of body composition such as DXA or CT scans; the sample was from one city in southern China during 1987–1994, and the prevalence of obesity has increased since this time. Further examination of hip circumference with metabolic abnormalities may help clarify the underlying pathology and differences observed across body weight categories and gender. Additional research on Chinese populations that incorporates subjects who are overweight and obese and includes additional measures of trunk and leg fat and leg lean mass may provide insight into the mechanistic role of regional adiposity on metabolic risk factors.
Acknowledgments
This work was supported by the Carolina Program for Health and Aging Research (CPHAR) of the University of North Carolina Institute on Aging (2T32AG000272-06A2), the General Clinical Research Centers program of the Division of Research Resources (RR00046), the National Institutes of Health (R01 DK069678), and the National Institute of Diabetes and Digestive and Kidney Diseases (P30DK056350-05S2).
Author Disclosure Statement
For all authors, no competing financial interests exist.
References
- 1.Westphal SA. Obesity, abdominal obesity, and insulin resistance. Clin Cornerstone. 2008;9:23–29. doi: 10.1016/s1098-3597(08)60025-3. discussion 30–21. [DOI] [PubMed] [Google Scholar]
- 2.Seidell JC. Kahn HS. Williamson DF. Lissner L. Valdez R. Report from a Centers for Disease Control and Prevention Workshop on use of adult anthropometry for public health and primary health care. Am J Clin Nutr. 2001;73:123–126. doi: 10.1093/ajcn/73.1.123. [DOI] [PubMed] [Google Scholar]
- 3.Allison DB. Paultre F. Goran MI. Poehlman ET. Heymsfield SB. Statistical considerations regarding the use of ratios to adjust data. Int J Obes Relat Metab Disord. 1995;19:644–652. [PubMed] [Google Scholar]
- 4.Jiang C. Lei SF. Liu MY. Xiao SM. Chen XD. Deng FY. Xu H. Tan LJ. Yang YJ. Wang YB. Sun X. Guo YF. Guo JJ. Zhu XZ. Deng HW. Evaluating the correlation and prediction of trunk fat mass with five anthropometric indices in Chinese females aged 20–40 years. Nutr Metab Cardiovasc Dis. 2007;17:676–683. doi: 10.1016/j.numecd.2006.04.007. [DOI] [PubMed] [Google Scholar]
- 5.Xiao SM. Lei SF. Chen XD. Liu MY. Jian WX. Xu H. Tan LJ. Deng FY. Yang YJ. Wang YB. Sun X. Jiang C. Guo YF. Guo JJ. Li YN. Jiang H. Zhu XZ. Deng HW. Correlation and prediction of trunk fat mass with four anthropometric indices in Chinese males. Br J Nutr. 2006;96:949–955. doi: 10.1017/bjn20061820. [DOI] [PubMed] [Google Scholar]
- 6.Snijder MB. Dekker JM. Visser M. Bouter LM. Stehouwer CD. Yudkin JS. Heine RJ. Nijpels G. Seidell JC Hoorn Study. Trunk fat and leg fat have independent and opposite associations with fasting and postload glucose levels: the Hoorn study. Diabetes Care. 2004;27:372–377. doi: 10.2337/diacare.27.2.372. [DOI] [PubMed] [Google Scholar]
- 7.Molarius A. Seidell JC. Selection of anthropometric indicators for classification of abdominal fatness—a critical review. Int J Obes Relat Metab Disord. 1998;22:719–727. doi: 10.1038/sj.ijo.0800660. [DOI] [PubMed] [Google Scholar]
- 8.Rocha PM. Barata JT. Teixeira PJ. Ross R. Sardinha LB. Independent and opposite associations of hip and waist circumference with metabolic syndrome components and with inflammatory and atherothrombotic risk factors in overweight and obese women. Metabolism. 2008;57:1315–1322. doi: 10.1016/j.metabol.2008.01.003. [DOI] [PubMed] [Google Scholar]
- 9.Snijder MB. Dekker JM. Visser M. Yudkin JS. Stehouwer CDA. Bouter LM. Hewine RJ. Nijpels G. Seidell JC. Larger thigh and hip circumferences are associated with better glucose tolerance: The Hoorn study. Obes Res. 2003;11:104–111. doi: 10.1038/oby.2003.18. [DOI] [PubMed] [Google Scholar]
- 10.Esmaillzadeh A. Mirmiran P. Moeini SH. Azizi F. Larger hip circumference independently contributed to reduced metabolic risks in Tehranian adult women. Int J Cardiol. 2006;108:338–345. doi: 10.1016/j.ijcard.2005.05.019. [DOI] [PubMed] [Google Scholar]
- 11.Heitmann BL. Frederiksen P. Lissner L. Hip circumference and cardiovascular morbidity and mortality in men and women. Obes Res. 2004;12:482–487. doi: 10.1038/oby.2004.54. [DOI] [PubMed] [Google Scholar]
- 12.Seidell JC. Perusse L. Despres JP. Bouchard C. Waist and hip circumferences have independent and opposite effects on cardiovascular disease risk factors: The Quebec Family Study. Am J Clin Nutr. 2001;74:315–321. doi: 10.1093/ajcn/74.3.315. [DOI] [PubMed] [Google Scholar]
- 13.Snijder MB. Zimmet PZ. Visser M. Dekker JM. Seidell JC. Shaw JE. Independent and opposite associations of waist and hip circumferences with diabetes, hypertension and dyslipidemia: The AusDiab Study. Int J Obes Relat Metab Disord. 2004;28:402–409. doi: 10.1038/sj.ijo.0802567. [DOI] [PubMed] [Google Scholar]
- 14.Lissner L. Bjorkelund C. Heitmann BL. Seidell JC. Bengtsson C. Larger hip circumference independently predicts health and longevity in a Swedish female cohort. Obes Res. 2001;9:644–646. doi: 10.1038/oby.2001.85. [DOI] [PubMed] [Google Scholar]
- 15.Snijder MB. Dekker JM. Visser M. Bouter LM. Stehouwer CDA. Kostense PJ. Yudkin JS. Heine RJ. Nijpels G. Seidell JC. Associations of hip and thigh circumferences independent of waist circumference with the incidence of type 2 diabetes: the Hoorn Study. Am J Clin Nutr. 2003;77:1192–1197. doi: 10.1093/ajcn/77.5.1192. [DOI] [PubMed] [Google Scholar]
- 16.Esmaillzadeh A. Mirmiran P. Azadbakht L. Amiri P. Azizi F. Independent and inverse association of hip circumference with metabolic risk factors in Tehranian adult men. Prev Med. 2006;42:354–357. doi: 10.1016/j.ypmed.2005.12.009. [DOI] [PubMed] [Google Scholar]
- 17.Bigaard J. Frederiksen K. Tjonneland A. Thomsen BL. Overvad K. Heitmann BL. Sorensen TIA. Waist and hip circumferences and all-cause mortality: usefulness of the waist-to-hip ratio? Int J Obes Relat Metab Disord. 2004;28:741–747. doi: 10.1038/sj.ijo.0802635. [DOI] [PubMed] [Google Scholar]
- 18.Canoy D. Wareham N. Luben R. Welch A. Bingham S. Day N. Khae KT. Serum lipid concentration in relation to anthropometric indices of central and peripheral fat distribution in 20,021 British men and women: results from the EPIC-Norfolk population-based cohort study. Atherosclerosis. 2006;189:420–427. doi: 10.1016/j.atherosclerosis.2005.12.027. [DOI] [PubMed] [Google Scholar]
- 19.Canoy D. Luben R. Welch A. Bingham S. Wareham N. Day N. Khaw KT. Fat distribution, body mass index and blood pressure in 22,090 men and women in the Norfolk cohort of the European Prospective Investigation into Cancer and Nutrition (EPIC-Norfolk) study. J Hypertens. 2004;22:2067–2074. doi: 10.1097/00004872-200411000-00007. [DOI] [PubMed] [Google Scholar]
- 20.Benetou V. Bamia C. Trichopoulos D. Trichopoulou A. Associations of anthropometric characteristics with blood cholesterol fractions among adults. The Greek EPIC study. Eur J Clin Nutr. 2006;60:942–948. doi: 10.1038/sj.ejcn.1602403. [DOI] [PubMed] [Google Scholar]
- 21.Dixon JB. Strauss BJ. Laurie C. O'Brien PE. Smaller hip circumference is associated with dyslipidemia and the metabolic syndrome in obese women. Obes Surg. 2007;17:770–777. doi: 10.1007/s11695-007-9142-y. [DOI] [PubMed] [Google Scholar]
- 22.Sakai Y. Ito H. Egami Y. Ohoto N. Hijii C. Yanagawa M. Satoh S. Jingu S. Favourable association of leg fat with cardiovascular risk factors. J Intern Med. 2005;257:194–200. doi: 10.1111/j.1365-2796.2004.01432.x. [DOI] [PubMed] [Google Scholar]
- 23.Canoy D. Boekholdt SM. Wareham N. Luben R. Welch A. Bingham S. Buchan I. Day N. Khaw KT. Body fat distribution and risk of coronary heart disease in men and women in the European Prospective Investigation Into Cancer and Nutrition in Norfolk cohort: A population-based prospective study. Circulation. 2007;116:2933–2943. doi: 10.1161/CIRCULATIONAHA.106.673756. [DOI] [PubMed] [Google Scholar]
- 24.Goodpaster BH. Krishnaswami S. Harris TB. Katsiaras A. Kritchevsky SB. Simonsick EM. Nevitt M. Holvoet P. Newman AB. Obesity, regional body fat distribution, and the metabolic syndrome in older men and women. Arch Intern Med. 2005;165:777–783. doi: 10.1001/archinte.165.7.777. [DOI] [PubMed] [Google Scholar]
- 25.Snijder MB. Visser M. Dekker JM. Goodpaster BH. Harris TB. Kritchevsky SB. De Rekeneire N. Kanaya AM. Newman AB. Tylavsky FA. Seidell JC Health ABC Study. Low subcutaneous thigh fat is a risk factor for unfavourable glucose and lipid levels, independently of high abdominal fat. The Health ABC Study. Diabetologia. 2005;48:301–308. doi: 10.1007/s00125-004-1637-7. [DOI] [PubMed] [Google Scholar]
- 26.Wiklund P. Toss F. Weinehall L. Hallmans G. Franks PW. Nordstrom A. Nordstrom P. Abdominal and gynoid fat mass are associated with cardiovascular risk factors in men and women. J Clin Endocrinol Metab. 2008;93:4360–4366. doi: 10.1210/jc.2008-0804. [DOI] [PubMed] [Google Scholar]
- 27.Aasen G. Fagertun H. Tonstad S. Halse J. Leg fat mass as measured by dual X-ray absorptiometry (DXA) impacts insulin resistance differently in obese women versus men. Scand J Clin Lab Invest. 2009;69:181–189. doi: 10.1080/00365510802464641. [DOI] [PubMed] [Google Scholar]
- 28.Chen CM. Overview of obesity in Mainland China. Obes Rev. 2008;9(Suppl 1):14–21. doi: 10.1111/j.1467-789X.2007.00433.x. [DOI] [PubMed] [Google Scholar]
- 29.Stevens J. Truesdale KP. Katz EG. Cai J. Impact of body mass index on incident hypertension and diabetes in Chinese Asians, American Whites, and American Blacks: The People's Republic of China Study and the Atherosclerosis Risk in Communities Study. Am J Epidemiol. 2008;167:1365–1374. doi: 10.1093/aje/kwn060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Wang J. Thornton JC. Russell M. Burastero S. Heymsfield S. Pierson RN., Jr Asians have lower body mass index (BMI) but higher percent body fat than do whites: comparisons of anthropometric measurements. Am J Clin Nutr. 1994;60:23–28. doi: 10.1093/ajcn/60.1.23. [DOI] [PubMed] [Google Scholar]
- 31.An epidemiological study of cardiovascular and cardiopulmonary disease risk factors in four populations in the People's Republic of China. Baseline report from the P.R.C.-U.S.A. Collaborative Study. People's Republic of China—United States Cardiovascular and Cardiopulmonary Epidemiology Research Group. Circulation. 1992;85:1083–1096. doi: 10.1161/01.cir.85.3.1083. [DOI] [PubMed] [Google Scholar]
- 32.Grundy SM. Brewer HB., Jr Cleeman JI. Smith SC., Jr Lenfant C. Definition of metabolic syndrome: Report of the National Heart, Lung, and Blood Institute/American Heart Association conference on scientific issues related to definition. Circulation. 2004;109:433–438. doi: 10.1161/01.CIR.0000111245.75752.C6. [DOI] [PubMed] [Google Scholar]
- 33.Stevens J. Katz EG. Huxley RR. Associations between gender, age and waist circumference. Eur J Clin Nutr. 2010;64:6–15. doi: 10.1038/ejcn.2009.101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Xu J. Long JS. Confidence intervals for predicted outcomes in regression models for categorical outcomes. 2005. http://www.indiana.edu/∼jslsoc/stata/spostci/xulong-prvalue-23aug2005.pdf/ http://www.indiana.edu/∼jslsoc/stata/spostci/xulong-prvalue-23aug2005.pdf/
- 35.Xu J. Long JS. Using the Delta Method to Construct Confidence Intervals for Predicted Probabilities, Rates, and Discrete Changes. 2005. http://www.indiana.edu/∼jslsoc/stata/spostci/spost_deltaci.pdf/ http://www.indiana.edu/∼jslsoc/stata/spostci/spost_deltaci.pdf/
- 36.Parker ED. Pereira MA. Stevens J. Folsom AR. Association of hip circumference with incident diabetes and coronary heart disease: the Atherosclerosis Risk in Communities study. Am J Epidemiol. 2009;169:837–847. doi: 10.1093/aje/kwn395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jiang CQ. Lam TH. Lin JM. Yue XJ. Cheng KK. Tomlinson B. Wong KS. Cheung BM. Thomas GN. An overview of the Guangzhou Biobank Cohort Study-Cardiovascular Disease Subcohort (GBCS-CVD): A platform for multidisciplinary collaboration. J Hum Hypertens. 2010;24:139–150. doi: 10.1038/jhh.2009.52. [DOI] [PubMed] [Google Scholar]
- 38.Snijder MB. Zimmet PZ. Visser M. Dekker JM. Seidell JC. Shaw JE. Independent association of hip circumference with metabolic profile in different ethnic groups. Obes Res. 2004;12:1370–1374. doi: 10.1038/oby.2004.173. [DOI] [PubMed] [Google Scholar]
- 39.Williams RR. Hunt SC. Hasstedt SJ. Hopkins PN. Wu LL. Berry TD. Stults BM. Barlow GK. Schumacher MC. Lifton RP, et al. Multigenic human hypertension: evidence for subtypes and hope for haplotypes. J Hypertens Suppl. 1990;8:S39–S46. [PubMed] [Google Scholar]
- 40.Doris PA. Hypertension genetics, single nucleotide polymorphisms, and the common disease: Common variant hypothesis. Hypertension. 2002;39(2 Pt 2):323–331. doi: 10.1161/hy0202.104087. [DOI] [PubMed] [Google Scholar]
- 41.Cannon CP. Obesity-related cardiometabolic complications. Clin Cornerstone. 2008;9:11–19. doi: 10.1016/s1098-3597(08)60024-1. discussion 20–12. [DOI] [PubMed] [Google Scholar]
- 42.Manolopoulos KN. Karpe F. Frayn KN. Gluteofemoral body fat as a determinant of metabolic health. Int J Obes (Lond) 2010;34:949–959. doi: 10.1038/ijo.2009.286. [DOI] [PubMed] [Google Scholar]
- 43.Frayn KN. Adipose tissue as a buffer for daily lipid flux. Diabetologia. 2002;45:1201–1210. doi: 10.1007/s00125-002-0873-y. [DOI] [PubMed] [Google Scholar]
- 44.Bobbioni-Harsch E. Pataky Z. Makoundou V. Kozakova M. Dekker J. Golay A. Fat distribution influences the cardio-metabolic profile in a clinically healthy European population. Eur J Clin Invest. 2009;39:1055–1064. doi: 10.1111/j.1365-2362.2009.02211.x. [DOI] [PubMed] [Google Scholar]
- 45.Goodpaster BH. Thaete FL. Simoneau JA. Kelley DE. Subcutaneous abdominal fat and thigh muscle composition predict insulin sensitivity independently of visceral fat. Diabetes. 1997;46:1579–1585. doi: 10.2337/diacare.46.10.1579. [DOI] [PubMed] [Google Scholar]